Abstract
Cardiovascular disease has always been the most serious public health problem in China. Although many studies have found that the risk of death caused by cardiovascular disease is related to air pollutants, the existing results are still inconsistent. The aim of this study was to investigate the effects of air pollutants on the risk of daily cardiovascular deaths in Hefei, China. Daily data on cardiovascular deaths, daily air pollutants, and meteorological factors from 2007 to 2016 were collected in this study. A time-series study design using a distributed lag nonlinear model was employed to evaluate the association between air pollutants and cardiovascular deaths. First, a single air pollutant model was established based on the minimum value of Akaike information criterion (AIC), and the single day lag effects and multi-day lag effects were discussed separately. Then, two-pollutant models were fitted. Subgroup analyses were conducted by gender (male and female), age (< 65 age and ≥ 65 age), and disease type (ischemic heart disease and cerebral vascular disease). There were 34,500 cases of cardiovascular deaths during the period 2007–2016, and the average concentrations of air pollutants (PM10, SO2, NO2, PM2.5, CO, O3) were 106.11, 20.34, 30.49, 72.59, 958.7, and 67.88 μg/m3, respectively. An increase of interquartile range (IQR) in PM10, SO2, NO2, PM2.5, CO, and O3 were associated with an increase of 4.34% (95%CI 1.54~7.23%) at lag 0–6, 5.79% (95%CI 2.43~9.27%) at lag 0–5, 4.47% (95%CI 1.64~7.37%) at lag 0–5, 3.14% (95%CI 0.03~6.36%) at lag 0–4, 3.11% (95%CI 0.21~6.10%) at lag 0–3, and 8.17% (95%CI 1.89~14.84%) at lag 0–5 in cardiovascular deaths, respectively. Females, older group (≥ 65 years) and deaths from cerebral vascular disease were more vulnerable to air pollution than males, younger individuals (< 65 years) and deaths from ischemic heart disease. Our results suggest that air pollution increased the risk of cardiovascular deaths in Hefei. These findings can provide evidence for effective air quality interventions in Hefei.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is the leading cause of death in the world (Venkatesan 2016). As estimated by the World Health Organization (WHO), 17.7 million people died of CVD in 2015, accounting for 45% of the world’s nonaccidental deaths, and 82% of these CVD deaths occurred in low and middle-income countries (Butler 2011). With the development of economy and the aggravation of population aging, CVD has posed the greatest health burden to the healthcare system of China. In addition, the prevalence and mortality of CVD will continue to rise in the next 10 years (Chen et al. 2017).
CVD is a multi-factorial disorder induced by interaction of heredity, circumstance, and behavior. Smoking and air pollution are the major risk factors of CVD (Gakidou et al. 2017). With the rapid development of industrialization and urbanization, the air quality of China has deteriorated seriously over the past few years. In 2016, air pollution was the fourth-highest risk factor of global burden of disease, leading to approximately 1.58 million deaths and 32.28 million DALYs (Gakidou et al. 2017). The decrease of air pollutant concentration and the improvement in personal protection can prevent CVD effectively, thereby reducing the health and economic burden of CVD.
Previous studies have suggested that air pollution is more associated with lung and respiratory diseases, such as pneumonia (Jiang et al. 2018; Nhung et al. 2017) and asthma (Guo et al. 2018). However, growing number of studies have shown that there is a link between short-term exposure to air pollution and CVD in China (Dehbi et al. 2017; Feng et al. 2019; Liu et al. 2019; Wu et al. 2019; Ye et al. 2016). Dehbi et al. (2017) used a cohort analysis of two large follow-up years in the UK and found that CVD deaths increased with increasing PM10, PM2.5, and SO2. Liu et al. (2019) assessed the association between air pollutants and CVD mortality in Shenyang, China, from 2013 to 2016, and observed that the increments in PM2.5, PM10, SO2, NO2, CO, and O3 were associated with an increase of CVD mortality. Wu et al. (2019) examined the effects of atmospheric particulate matter on CVD deaths due to different causes in Lanzhou, during 2014–2015, and found that elevated concentrations of PM2.5, PMC, and PM10 had different effects on CVD deaths due to different causes. Ye et al. (2016) reported that for every 10 μg/m3 increase in PM2.5 and PM10, coronary heart disease increased by 0.74% and 0.23% in Shanghai. Feng et al. (2019) explored the relationship between PM10 and CVD emergency department admissions in Beijing between January 2013 and December 2013 and found that for a 10 μg/m3 increment of PM10, the total CVD emergency department admissions increased by 0.29%.
These different studies have demonstrated that air pollutants have a detrimental effect on the occurrence or exacerbation of CVD, but most prior studies were conducted in large cities. The effect of air pollutants on health varied across different regions (Chen et al. 2013; Dong et al. 2013). Hefei is a city with frequent haze events occurring, and its air quality exceeds the national secondary concentration limit every year (Zhang et al. 2017a). Therefore, it is essential to conduct study on the effects of air pollution on residents’ health in Hefei.
This time-series analysis aimed to estimate the association of short-term exposure to air pollution and deaths due to CVD in Hefei during 2007–2016. Stratified analyses by age, gender, and disease type were conducted to identify the vulnerable subgroups.
Materials and methods
Study Area
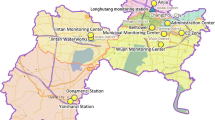
Hefei (30° 57′–32° 32′ north, 116° 41′–117° 58′ ) is the capital of Anhui province, and it has a subtropical monsoon humid climate with obvious monsoons. Hefei has a total area of 11,445 km2. By the end of 2016, the population of Hefei is 7.87 million, of which 2.59 million are registered residents. Hefei has 4 districts, 4 counties, and 1 county-level city. The cardiovascular death population included in this study was only the registered population in Hefei urban area (Yaohai, Luyang, Shushan, and Baohe districts). The cardiovascular death data of the surrounding suburbs such as Changfeng County, Feidong County, and Feixi County were not obtained, and the air quality monitoring stations in Hefei City were located in the urban area. The level of air pollutants in the suburbs was quite different from that in the urban area, so it was not included in the study.
Air pollution and meteorology data
The daily data on air pollutants, including PM10, NO2, PM2.5, CO, SO2, and O3, were provided by the Hefei Environmental Monitoring Center. Daily air pollutant values were calculated by averaging the 24-h values. The data were originally collected from 10 air quality monitoring stations. The daily meteorological factors of Hefei from 2007to 2016 were obtained from the China Meteorological Data Network (http://data.cma.gov.cn/).
Cardiovascular death data collection
We obtained the 2007–2016 resident death data from the Hefei Municipal Center for Disease Control and extracted the CVD deaths data using the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10). Specifically, data on cardiovascular disease (I00–I99), ischemic heart disease (I20–I25), and cerebral vascular disease (I60–I69) were extracted. In order to identify the subgroups vulnerable to air pollutants, we conducted stratified analyses by gender (male and female), age (< 65 years old and ≥ 65 years old), and disease type (ischemic heart disease and cerebral vascular disease) (Zhu et al. 2017).
Statistical analysis
Daily CVD deaths, air pollutants, and meteorological factors were described as mean standard deviation (SD) and quartiles. Spearman rank correlation analysis was conducted to estimate the relationships between air pollutants and meteorological factors. A time-series analysis approach in DLNM was applied to estimate the association between ambient air pollution and CVD deaths. Studies have shown that daily CVD deaths are consistent with the Poisson distribution, and the number of daily deaths may be excessively discrete (Lu et al. 2015; Maji et al. 2017). Therefore, the quasi-Poisson distribution was adopted in the DLNM model in our study (Lu et al. 2015; Yang et al. 2016a; Zhu et al. 2017).
We use cubic spline functions to control the confounding effects of long-term trends, seasons, day of the week, and public holiday, and meteorological factors (average temperature, average pressure, relative humidity, wind speed, and precipitation) were sequentially included in the model; the Akaike information criterion (AIC) (Gasparrini et al. 2010) was used to measure the goodness of fit of the model, and the minimum AIC value is expressed as the preferred model. Finally, the model of the average temperature and relative humidity is introduced. The basic model of this study is as follows:
where t is the time observed (days); Yt is the dependent variable, number of CVD deaths at t day; μt is the expected mean of Yt; α is the constant of model; ns is the natural cubic spline function; Timet is the time variable, day t, used to control the long-term trend and seasonality of time; df is the degree of freedom; DOWt is the day of the week effect; Tempt is the average temperature on day t; and RHt is the average relative humidity of the day t. According to previous research experience, the mean temperature and relative humidity degrees were both set to 4 (Li et al. 2015), the maximum lag days of average temperature and relative humidity were 27 (Guo et al. 2011) days and the current day (Luo et al. 2018), respectively, the degree of freedom of the time variable in the model is selected as 7 df/year (Yang et al. 2016b). A single-contaminant model was established to assess the impact of single air pollutants on CVD deaths in residents. The single pollutant model is shown as follows:
where Xt,l1 represents pollutant concentrations at day t (PM10, PM2.5, NO2, SO2, CO, and O3), λ is the coefficient of the matrix, and l1 is the maximum number of days of lag in air pollutants. COVs denotes all the confounders in the core model (1). We examined the associations with different lag structures from the current day (lag 0) up to 7 days before (lag 7). We also estimated the cumulative effect of air pollution with distributed lag models (defined as lag 0–1, lag 0–2,…, lag 0–7). According to the Akaike information criterion (AIC) (Li et al. 2015), the df for air pollutants lag days was specified to be 5.
Based on the single pollutant model, a multiple-pollutant model was constructed to assess the stability of each air pollutant’s impact on CVD deaths. Optimal lag day for each contaminant in the single-contaminant model were fixed, then we added additional air pollutants for adjustment. Considering the collinearity between air pollutants, PM10 and PM2.5 do not appear in the model simultaneously (see Supplementary material 1). We used nonparametric tests to compare whether the effect of air pollution on CVD deaths were significantly different by gender (male and female), age (< 65 years and ≥ 65 years), and different types of CVD (ischemic heart disease and cerebral vascular disease), and the effects of air pollutant concentration on CVD deaths in subgroups were analyzed. Sensitivity analysis were conducted by varying dfs for time (6,8,9), temperature and relative humidity (3,5,6) to examine the robustness of the results in our study.
Time-series analysis was performed using the “dlnm” and “splines” software packages in R3.3.3. The results were expressed as excess risk (ER) and 95% CI, where ER = (RR − 1) × 100% (Zhang et al. 2017b), that mean with per interquartile range (IQR) increase in air pollutant. The results were shown by the excess relative risk [(relative risk − 1) × 100%] with their 95% confidence intervals (95%CI) associated with per interquartile range (IQR) increase in air pollutant (Lu et al. 2015; Tao et al. 2014), percentage change in risk of CVD deaths, P value < 0.05 was considered to be statistically significant.
Results
Description of data
The geographical location of Hefei and the distribution of air monitoring stations are shown in Fig. 1. Table 1 summarizes the basic statistics of CVD deaths, air pollutants, and meteorological factor in Hefei from 2007 to 2016. During the study period, a total of 34,500 deaths caused by CVD were involved, of which 18,774 (54.41%) and 15,726 (45.59%) were male and female; 5222 (14.92%) and 29,278 (84.86%) were < 65 age and ≥ 65 age. There were 10,837 (31.41%) deaths caused by ischemic heart disease and 14,382 (41.69%) deaths caused by cerebral vascular disease. For air pollutants, the daily average concentrations of PM10, SO2, and NO2 were 106.11, 20.34, and 30.49 μg/m3 (2007–2016); the average daily concentrations of PM2.5, CO, and O3 were 72.59, 958.7, and 67.88 μg/m3 (2013–2016). The IQR of PM10, SO2, NO2, PM2.5, CO, and O3 were 64.4, 14.3, 15.8, 46.2, 400, and 50.1 μg/m3, respectively. The average daily temperature is 16.73 °C, and the average relative humidity is 74.43%.
Time-series analysis
The time-series plot showed the daily mutations of air pollutant concentrations and CVD deaths during the study period (Fig. 2). CVD deaths showed seasonal changes during the study, CVD deaths in winter (In December of that year to February of the next year) is significantly higher than in summer (June–August), and CVD deaths is increasing year by year. The PM10, SO2, and PM2.5 daily concentration generally have been declining year by year, and NO2, CO, and O3 showed an upward trend year by year. But all of them had similar characteristics of periodic fluctuation, the seasonal pattern of PM10, SO2, PM2.5, NO2, CO, and O3 showed low concentration in summer and autumn and high concentration in winter and spring.
Spearman’s correlation analysis and exposure-response relationships
Table 2 describes the correlation between meteorological factors and air pollutants. There was a high correlation between PM2.5 and PM10 (r = 0.804), and PM10 was moderately correlated with other air pollutants and weather factors. There is a positive correlation (P < 0.05) between PM10 and PM2.5, SO2, NO2, and CO, while it is negatively correlated with O3, temperature, and relative humidity (P < 0.05); PM2.5 is positively correlated with NO2, SO2, and CO, negatively correlated with O3, temperature, and relative humidity (P < 0.05); NO2, SO2, and CO related analysis result is in accord with the result of PM2.5 and PM10 analysis (see Table 2). It is recommend that full consideration shall be given to the confounding effect of meteorological factor in the research on the influences of air pollutions on the deaths caused by CVD, and multi-pollutant model shall be employed to control the influences of other pollutants.
Figure 3 illustrates the exposure-response relationships between six air pollutants at the current day and the relative risk of CVD deaths. We can also find that the curves associated with PM10, SO2, NO2, PM2.5, and CO presented similar linear trends, which indicated that the higher concentration of air pollutants might cause a significant increase in CVD deaths, and O3 curve tended to be not associated with CVD deaths.
Exposure response relationships between six air pollutants and CVD deaths. The x-axis represented the concentration of air pollutants (μg/m3) at the current day, the y-axis indicated log relative risk of CVD deaths. The imaginary lines were the 95%Cl. All models were adjusted for time, temperature, relative humidity, weekend, and holiday
Analysis of the DLNM
Single pollutant model analysis
Three-dimensional plot of relative risks (RRs) of CVD deaths along air pollutions and lag 0~lag 7 days are shown in Fig. 4. The distributed lag surface reveals that CVD deaths risk increased with an increase in PM10, SO2, NO2, PM2.5, CO, and O3. We presented the associations of PM10, SO2, NO2, PM2.5, CO, and O3 with CVD deaths over different lag days in Table 3. For the single-day lag effects, the greatest impact on the risk of CVD deaths with per IQR increment in PM10 were found at lag 0 with 1.64% (95%CI 0.46~2.83%), SO2 at lag 2 with 1.45% (95%CI 0.72~2.18%), NO2 at lag 1 with 1.04% (95%CI 0.27~1.55%), PM2.5 at lag 1 with 0.84% (95%CI 0.04~1.65%), CO at lag 0 with 1.66% (95%CI 0.04~3.31%), and O3 at lag 2 with 1.83% (95%CI 0.51~3.18%). In terms of multi-day lag effects, the strongest effects of PM10, SO2, NO2, PM2.5, CO, and O3 on CVD deaths were 4.34% (95%CI 1.54~7.23%) at lag 0–6, 5.79% (95%CI 2.43~9.27%) at lag 0–5, 4.47% (95%CI 1.64~7.37%) at lag 0–5, 3.14% (95%CI 0.03~6.36%) at lag 0–4, 3.11% (95%CI 0.21~6.10%) at lag 0–3, and 8.17% (95%CI 1.89~14.84%) at lag 0–5, respectively.
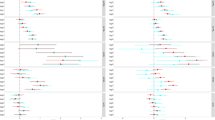
Subgroup analysis
It was found that air pollutants have significant effects on CVD deaths in male and female (Z = 13.539, P = 0.000), < 64 ages and ≥ 65 ages (Z = 70.201, P = 0.000), ischemic heart disease, and cerebral vascular disease (Z = 19.278, P = 0.000). The percent change of overall CVD deaths with per IQR increment in single pollutants by gender and age are shown in Fig. 5 and Supplementary Tables S1–S2. PM10, SO2, and NO2 both increased the risk of CVD deaths in male and female. The strongest effects of PM10, SO2, and NO2 on male CVD deaths were 4.76% (95%CI 0.49~7.20%) at lag 0–7, 5.69% (95%CI 1.23~10.34%) at lag 0–5, and 3.46% (95%CI 0.00~7.04%) at lag 0–4; the strongest effects of PM10, SO2, and NO2 on female CVD deaths were 5.37% (95%CI 1.60~9.27%) at lag 0–5, 5.97% (95%CI 1.11~11.06%) at lag 0–5, and 5.65% (95%CI 1.55~9.92%) at lag 0–5. However, PM2.5, CO, and O3 have been found to exhibit sex selective effect; this study did not find significant statistical significance between PM2.5, CO, and O3 and CVD deaths in male, but female was just the opposite; the strongest effects of PM2.5, CO, and O3 on female CVD deaths were 5.06% (95%CI 0.03~10.34%) at lag 0–5, 5.63% (95%CI 1.30~10.14%) at lag 0–3, and 15.40% (95%CI 5.67~26.03%) at lag 0–5, which means females suffered more from the adverse effects of air pollutants. For age subgroups, pollutants also exhibit age-selective effects, and only SO2, NO2, and PM2.5 increased the risk of CVD deaths on age < 65 years group; the strongest effects of SO2, NO2, and PM2.5 on age < 65 years group CVD deaths were 8.62% (95%CI 0.18~17.78%) at lag 0–5, 5.94% (95%CI 0.13~12.08%) at lag 0–2, and 15.18% (95%CI 2.31~29.66%) at lag 0–7. The strongest effects of PM10, SO2, NO2, CO, and O3 on age ≥ 65 years group CVD deaths were 4.45% (95%CI 1.00~8.01%) at lag 0–7, 5.97% (95%CI 1.11~11.06%) at lag 0–5, 4.32% (95%CI 1.31~7.42%) at lag 0–5, 5.09% (95%CI 0.25~10.17%) at lag 0–3, and 8.06 (95%CI 1.38~15.19%) at lag 0–5; elderly groups (aged 65+) suffered more from the adverse effects of air pollutants. Grouped according to different types of CVD such as ischemic heart disease and cerebral vascular disease, it was found that there was only statistical significance between O3 and ischemic heart disease; the strongest effects were 13.08% (95%CI 1.97~25.39%) at lag 0–5. Cerebral vascular disease was mainly affected by PM10, SO2, and NO2; the strongest effects of PM10, SO2, and NO2 on cerebral vascular disease were 6.25% (95%CI 1.31~11.43%) at lag 0–7, 5.68% (95%CI 0.55%~11.07%) at lag 0–5, and 6.34% (95%CI 1.93~10.95%) at lag 0–5 (Table 4).
Multi-pollutant model analysis
After determining the optimal lag for each pollutant in a single pollutant model, we added additional contaminants to adjustment. The percent increase and 95%CI for CVD deaths associated with per IQR increment of air pollutants in multi-pollutant models are presented in Table 5. The results of the air pollutants in the two pollutants were lower than those of the single pollutant model, and only the effects of SO2 and O3 on CVD deaths were more stable (P < 0.05). The fitting results of other pollutants PM10, NO2, PM2.5, and CO in the multi-pollutant model were not statistically significant (P > 0.05).
Sensitivity analysis
In the range of (6,8,9), the change of df/year has no significant effect on the connection of air pollution with CVD deaths (Supplementary Fig. S1). In addition, we obtained similar results when modifying df (3,5,6) for the mean temperature and relative humidity (Supplementary Figs. S2–S3).
Discussion
In this study, the DLNM was utilized to analyze the relationship between air pollutants and CVD from 2007 to 2016 in Hefei. The results showed that PM10, SO2, NO2, PM2.5, CO, and O3 had significant adverse effects on overall CVD and its subtypes, including ischemic heart disease and cerebral vascular disease. Subgroup analysis showed that females were more sensitive to the effects of PM10, SO2, NO2, PM2.5, CO, and O3 than males, and regarding gender, residents aged ≥ 65 years were more susceptible to the effects of PM10, CO, and O3 than residents < 65 years old, but < 65 years old were more susceptible to the effects of SO2, NO2, and PM2.5 than aged ≥ 65 years. Our results may be relevant for the prevention and treatment of CVD and provide constructive advice for controlling air pollution in Hefei, China.
The exceeded days of PM10, SO2, NO2, PM2.5, CO, and O3 (based on the first-class concentration limit of China’s “Environmental Air Quality Standards” (GB3095-2012)) were 87.72%, 3.18%, 0.68%, 84.87%, 0.07%, and 2.33%, respectively. PM10, PM2.5, and SO2 were the major pollutants in Hefei. Hefei Air Quality ranks 48th out of 74 cities, and the average concentration of PM10, SO2, NO2, PM2.5, CO, and O3 was ranked 38th, 38th, 32th, 71th, 37th, and 36th, respectively. Studies have shown that particulate matter (PM10, PM2.5) mainly comes from various industrial production, construction, and road dust. SO2 is mainly derived from the combustion of coal oil and the exhaust of motor vehicles. Therefore, it was of great meaning and emergency to predict the risk of CVD caused by air pollution in Hefei. We concluded that with per IQR increase in PM10, CVD deaths were significantly increased by 1.64% (95%CI 0.46~2.83%) at lag 0 in single-day lags and 4.34% (95%CI 1.54~7.23%) at lag 0–6 in multi-day lags. Our results are similar to previous studies, Zahra Soleimani et al. (2019). Exploring the relationship between air pollution and hospitalization rates for CVD, they observed a 1.08% increase in CVD hospitalization for every 10 μg/m3 increase in PM10. Zhang et al. (2017b) concluded that with per 10 μg/m3 increases in PM10, CVD mortality was significantly increased by 1.012% (1.011–1.013) at lag 1 day. However, we found no statistical association between PM10 CVD deaths in a study in Wuhan. The inconsistent results may be due to the concentration of PM10 in different regions and demographic differences.
For SO2, we concluded that with per IQR increase in SO2, CVD deaths and cerebral vascular disease were significantly increased by 1.45% (95%CI 0.72~2.18%) at lag 2 and 1.61% (95%CI 0.54~2.69%) at lag 1 in single day, and the effects in multi-day lags were greater than single-day lags, which were consistent with most previous studies. In Beijing, the relative risks (95%CI) of per 10 mg/m3 increased to SO2 were 1.008 (0.999–1.018) on cardiovascular emergency room admissions (Ma et al. 2017). Dong et al. studied the effects of air pollution on CVD morbidity in three cities in Northeast China, and it was found that for every 20 μg/m3 increase in SO2 concentration, CVD rate increased by 1.14% (Dong et al. 2013). The acute effects of SO2 on population death in the atmosphere of six cities in China, we can find that the effect of SO2 on CVD death is different, but they all have an obvious correlation (Zeng et al. 2015).
This study found that the concentrations of NO2 and O3 were increasing year by year, and O3 had the greatest adverse effect on CVD deaths; we concluded that with per IQR increase in O3, CVD was significantly increased by 1.83% (95%CI 0.51~3.18%) at lag 3 in single-day lags and 8.17% (95%CI 1.89~14.84%) at lag 0–5 in multi-day lags. Different from other studies (Huang et al. 2018; Yang et al. 2018), of the six air pollutants in this study, only O3 has an effect on ischemic heart disease. We found that with per IQR increase in NO2 at lag 0–5 days, it could lead to a 1.04% (95%CI 0.27~1.55%) and 1.61% (95%CI 0.54~2.69%) increment in CVD deaths and cerebral vascular disease. Our finding was also consistent with other previous studies (Huang et al. 2018; Yang et al. 2018). NO2 and O3 can inhibit the activity of enzymes, affect the metabolism of lipoproteins, induce systemic inflammatory reactions, and cause CVD diseases (Faridi et al. 2018). Our study showed that SO2+NO2 and O3+CO still have significant effects on CVD deaths in the two-pollutant models; this suggests that SO2, NO2, O3, and CO were powerful predictors of CVD deaths in Hefei, China. In other multi-pollution models, we did not find that the combined effect of pollutants has an effect on CVD deaths, probably due to the strong correlation between pollutants, affecting their death effects on CVD.
Consistent with previous studies (Garcia et al. 2016; Zhu et al. 2017), females were more susceptible to the effects of PM10, SO2, NO2, PM2.5, CO, and O3 than males. Although this relationship is not evident, some biological and abiotic factors can explain this phenomenon (Bennett et al. 1996; Eaker et al. 1993); first, in anatomy, females have smaller respiratory tract diameters, so females have higher airway responses and particulate deposition effects than males. For the age subgroup, the study showed that residents ≥ 65 years old were more sensitive to PM10, CO, and O3 than residents < 65 years old; the results of SO2, NO2, and PM2.5 were exactly the opposite. This may be explained by differences in exposure to air pollutants among residents of different ages, and it is more common in older people with chronic diseases (Roth et al. 2017).
In this study, there are several advantages: first, this study had a longer time span than similar studies in the past (generally 2–5 years), the time span of this study reached 10 years, can reveal the long-term exposure effects of air pollutants, and compared to previous studies, the types of air pollutants in our study are more comprehensive, and it is a good response to the effects of air pollutants on CVD deaths, so the results were more reliable and accurate. Second, this study used a distributed-lag nonlinear model to quantitatively analyze the effects of air pollutants on CVD in residents, and the model is more active than the generalized additive model. Third, the study compared different genders, ages, and the effects of air pollutants on different types of CVD deaths in the same population; sensitive populations were identified, and more favorable targeted preventive and control measures were proposed. Fourth, as we mentioned above, Hefei is the representative area for the combined pollution of coal smoke and motor vehicle exhaust in the central cities. This study will help us better understand the impact of air pollution on CVD deaths in a coal smoke and motor vehicle exhaust polluted region. Of course, this study also has some shortcomings. First, as with other similar studies, air pollutant concentration data and meteorological data are obtained from fixed detection sites, which could not represent total exposure to population, underestimate the health effects of air pollution. Second, due to the lack of data on indoor air pollutants, indoor air pollution is not considered in this study, which may also affect population exposure levels and overestimate the link between ambient air pollutants and death. Finally, this study only involves Hefei; the results of the study should be cautious when extrapolated. However, from the point of view of big data analysis, although there are some shortcomings, the research results still have some persuasion.
Conclusions
In summary, we evaluated the effects of ambient air pollutants on CVD deaths during 2007–2016 in Hefei. Through the DLNM of time-series analysis, we observed positive associations between PM10, SO2, NO2, PM2.5, CO, and O3 concentration at different lag days and CVD deaths. NO2 and SO2 were the largest two risk pollutants of CVD deaths in Hefei. Females and elderly for CVD were more vulnerable to air pollution. In consequence, some effective measures should be taken to strengthen the management of the ambient air pollutants, and to enhance the protection of the high-risk population from air pollutants.
References
Bennett WD, Zeman KL, Kim C (1996) Variability of fine particle deposition in healthy adults: effect of age and gende. Am J Respir Crit Care Med 153:1641–1647
Butler D (2011) UN targets top killers. Nature 477:260–261
Chen R et al (2013) Seasonal variation in the acute effect of particulate air pollution on mortality in the China Air Pollution and Health Effects Study (CAPES). Sci Total Environ 450-451:259–265
Chen WW, Gao RL, Liu LS, Zhu ML, Wang W, Wang YJ, Wu ZS, Li HJ, Gu DF, Yang YJ, Zheng Z, Jiang LX, Hu SS (2017) China cardiovascular diseases report 2015: a summary. J Geriatr Cardiol 14:1–10
Dehbi HM, Blangiardo M, Gulliver J, Fecht D, de Hoogh K, al-Kanaani Z, Tillin T, Hardy R, Chaturvedi N, Hansell AL (2017) Air pollution and cardiovascular mortality with over 25years follow-up: A combined analysis of two British cohorts. Environ Int 99:275–281
Dong G-H et al (2013) Associations between ambient air pollution and prevalence of stroke and cardiovascular diseases in 33 Chinese communities. Atmos Environ 77:968–973
Eaker ED, Chesebro JH, Sacks FM, Wenger NK, Whisnant JP, Winston M (1993) Cardiovascular disease in women. Circulation 88:1999–2009
Faridi S, Shamsipour M, Krzyzanowski M, Künzli N, Amini H, Azimi F, Malkawi M, Momeniha F, Gholampour A, Hassanvand MS, Naddafi K (2018) Long-term trends and health impact of PM2.5 and O3 in Tehran, Iran, 2006-2015. Environ Int 114:37–49
Feng W, Li H, Wang S, van Halm-Lutterodt N, An J, Liu Y, Liu M, Wang X, Guo X (2019) Short-term PM10 and emergency department admissions for selective cardiovascular and respiratory diseases in Beijing, China. Sci Total Environ 657:213–221
Gakidou E et al (2017) Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017(390):1345–1422
Garcia M et al (2016) Cardiovascular disease in women: clinical perspectives. Circ Res 118:1273–1293
Gasparrini A, Armstrong B, Kenward MG (2010) Distributed lag non-linear models. Stat Med 29:2224–2234
Guo Y, Barnett AG, Pan X, Yu W, Tong S (2011) The impact of temperature on mortality in Tianjin, China: a case-crossover design with a distributed lag nonlinear model. Environ Health Perspect 119:1719–1725
Guo H, Huang S, Chen M (2018) Air pollutants and asthma patient visits: Indication of source influence. Sci Total Environ 625:355–362
Huang J et al (2018) The burden of ischemic heart disease related to ambient air pollution exposure in a coastal city in South China. Environ Res 164:255–261
Jiang W et al (2018) Outdoor particulate air pollution and indoor renovation associated with childhood pneumonia in China. Atmos Environ 174:76–81
Li L, Lin GZ, Liu HZ, Guo Y, Ou CQ, Chen PY (2015) Can the Air Pollution Index be used to communicate the health risks of air pollution? Environ Pollut 205:153–160
Liu M et al (2019). Population susceptibility differences and effects of air pollution on cardiovascular mortality: epidemiological evidence from a time-series study. Environ Sci Pollut Res Int 26:15943-15952
Lu F, Zhou L, Xu Y, Zheng T, Guo Y, Wellenius GA, Bassig BA, Chen X, Wang H, Zheng X (2015) Short-term effects of air pollution on daily mortality and years of life lost in Nanjing, China. Sci Total Environ 536:123–129
Luo L et al (2018). Short-Term Effects of Ambient Air Pollution on Hospitalization for Respiratory Disease in Taiyuan, China: A Time-Series Analysis. Int J Environ Res Public Health 15:1-14
Ma Y, Zhao Y, Yang S, Zhou J, Xin J, Wang S, Yang D (2017) Short-term effects of ambient air pollution on emergency room admissions due to cardiovascular causes in Beijing, China. Environ Pollut 230:974–980
Maji S, Ahmed S, Siddiqui WA, Ghosh S (2017) Short term effects of criteria air pollutants on daily mortality in Delhi, India. Atmos Environ 150:210–219
Nhung NTT et al (2017) Short-term association between ambient air pollution and pneumonia in children: A systematic review and meta-analysis of time-series and case-crossover studies. Environ Pollut 230:1000–1008
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, Ahmed M, Aksut B, Alam T, Alam K, Alla F, Alvis-Guzman N, Amrock S, Ansari H, Ärnlöv J, Asayesh H, Atey TM, Avila-Burgos L, Awasthi A, Banerjee A, Barac A, Bärnighausen T, Barregard L, Bedi N, Belay Ketema E, Bennett D, Berhe G, Bhutta Z, Bitew S, Carapetis J, Carrero JJ, Malta DC, Castañeda-Orjuela CA, Castillo-Rivas J, Catalá-López F, Choi JY, Christensen H, Cirillo M, Cooper L Jr, Criqui M, Cundiff D, Damasceno A, Dandona L, Dandona R, Davletov K, Dharmaratne S, Dorairaj P, Dubey M, Ehrenkranz R, el Sayed Zaki M, Faraon EJA, Esteghamati A, Farid T, Farvid M, Feigin V, Ding EL, Fowkes G, Gebrehiwot T, Gillum R, Gold A, Gona P, Gupta R, Habtewold TD, Hafezi-Nejad N, Hailu T, Hailu GB, Hankey G, Hassen HY, Abate KH, Havmoeller R, Hay SI, Horino M, Hotez PJ, Jacobsen K, James S, Javanbakht M, Jeemon P, John D, Jonas J, Kalkonde Y, Karimkhani C, Kasaeian A, Khader Y, Khan A, Khang YH, Khera S, Khoja AT, Khubchandani J, Kim D, Kolte D, Kosen S, Krohn KJ, Kumar GA, Kwan GF, Lal DK, Larsson A, Linn S, Lopez A, Lotufo PA, el Razek HMA, Malekzadeh R, Mazidi M, Meier T, Meles KG, Mensah G, Meretoja A, Mezgebe H, Miller T, Mirrakhimov E, Mohammed S, Moran AE, Musa KI, Narula J, Neal B, Ngalesoni F, Nguyen G, Obermeyer CM, Owolabi M, Patton G, Pedro J, Qato D, Qorbani M, Rahimi K, Rai RK, Rawaf S, Ribeiro A, Safiri S, Salomon JA, Santos I, Santric Milicevic M, Sartorius B, Schutte A, Sepanlou S, Shaikh MA, Shin MJ, Shishehbor M, Shore H, Silva DAS, Sobngwi E, Stranges S, Swaminathan S, Tabarés-Seisdedos R, Tadele Atnafu N, Tesfay F, Thakur JS, Thrift A, Topor-Madry R, Truelsen T, Tyrovolas S, Ukwaja KN, Uthman O, Vasankari T, Vlassov V, Vollset SE, Wakayo T, Watkins D, Weintraub R, Werdecker A, Westerman R, Wiysonge CS, Wolfe C, Workicho A, Xu G, Yano Y, Yip P, Yonemoto N, Younis M, Yu C, Vos T, Naghavi M, Murray C (2017) Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J Am Coll Cardiol 70:1–25
Soleimani Z et al (2019) Short-term effects of ambient air pollution and cardiovascular events in Shiraz, Iran, 2009 to 2015. Environ Sci Pollut Res Int 26(7):6359–6367
Tao Y et al (2014) Air pollution and hospital admissions for respiratory diseases in Lanzhou, China. Environ Pollut 185:196–201
Venkatesan P (2016) WHO report: air pollution is a major threat to health. Lancet Respir Med 4:351
Wu T et al (2019). Association between particulate matter air pollution and cardiovascular disease mortality in Lanzhou, China. Environ Sci Pollut Res Int 26:15262-15272
Yang HC, Chang SH, Lu R, Liou DM (2016a) The effect of particulate matter size on cardiovascular health in Taipei Basin, Taiwan. Comput Methods Prog Biomed 137:261–268
Yang J, Yin P, Zhou M, Ou CQ, Li M, Li J, Liu X, Gao J, Liu Y, Qin R, Xu L, Huang C, Liu Q (2016b) The burden of stroke mortality attributable to cold and hot ambient temperatures: Epidemiological evidence from China. Environ Int 92-93:232–238
Yang Y, Tang R, Qiu H, Lai PC, Wong P, Thach TQ, Allen R, Brauer M, Tian L, Barratt B (2018) Long term exposure to air pollution and mortality in an elderly cohort in Hong Kong. Environ Int 117:99–106
Ye X et al (2016) Acute effects of particulate air pollution on the incidence of coronary heart disease in Shanghai, China. PLoS One 11:e0151119
Zeng Q et al (2015) Acute effects of SO2 and NO2 on mortality in the six cities of China. Zhonghua Yu Fang Yi Xue Za Zhi 49:1085–1091
Zhang C, Ding R, Xiao C, Xu Y, Cheng H, Zhu F, Lei R, di D, Zhao Q, Cao J (2017a) Association between air pollution and cardiovascular mortality in Hefei, China: A time-series analysis. Environ Pollut 229:790–797
Zhang Y, Peng M, Yu C, Zhang L (2017b) Burden of mortality and years of life lost due to ambient PM10 pollution in Wuhan, China. Environ Pollut 230:1073–1080
Zhu J, Zhang X, Zhang X, Dong M, Wu J, Dong Y, Chen R, Ding X, Huang C, Zhang Q, Zhou W (2017) The burden of ambient air pollution on years of life lost in Wuxi, China, 2012-2015: a time-series study using a distributed lag non-linear model. Environ Pollut 224:689–697
Acknowledgments
Appreciation is to all the staff members at the Hefei City Center for Disease Control and Prevention, China for the data collection.
Funding
This study was supported by the National Air Pollution Impact on Population Health Monitoring Project (National Health Office Disease Control Letter [2015] No. 397) and Anhui University Student Innovation and Entrepreneurship Training Program Project (0311011105).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Responsible editor: Philippe Garrigues
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• The risk of CVD deaths increased with the rising in air pollutant concentrations.
• Females were more vulnerable to air pollution exposure as compared to males which were similar to comparison of ages ≥ 65 and < 65 ages.
• The ER of cerebral vascular disease was significantly correlated with the concentration of PM10, SO2, and NO2, where as ischemic heart disease was only determined by O3.
Electronic supplementary material
ESM 1
(DOCX 194 kb)
Rights and permissions
About this article
Cite this article
Xu, J., Geng, W., Geng, X. et al. Study on the association between ambient air pollution and daily cardiovascular death in Hefei, China. Environ Sci Pollut Res 27, 547–561 (2020). https://doi.org/10.1007/s11356-019-06867-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-019-06867-4