Abstract
Most studies of short-term exposure to ambient air pollution and cerebrovascular diseases focused on specific stroke-related outcomes, and results were inconsistent due to data unavailability and limited sample size. It is unclear yet how ambient air pollution contributes to the total cardiovascular mortality in central China. Daily deaths from cerebrovascular diseases were obtained from the Disease Surveillance Point System (DSPs) of Wuhan Center for Disease Control and Prevention during the period from 2013 to 2019. Air pollution data were obtained from Wuhan Ecology and Environment Institute from 10 national air quality monitoring stations, including average daily PM2.5, PM10, SO2, NO2, and O3. Average daily temperature and relative humidity were obtained from Wuhan Meteorological Bureau. We performed a Poisson regression in generalized additive models (GAM) to examine the association between ambient air pollution and cerebrovascular disease mortality. We observed a total of 84,811 deaths from cerebrovascular diseases from 1 January 2013 to 31 December 2019 in Wuhan. Short-term exposure to PM2.5, PM10, SO2, and NO2 was positively associated with daily deaths from cerebrovascular diseases, and no significant association was found for O3. The largest effect on cerebrovascular disease mortality was found at lag0 for PM2.5 (ERR: 0.927, 95% CI: 0.749–1.105 per 10 μg/m3) and lag1 for PM10 (ERR: 0.627, 95% CI: 0.493–0.761 per 10 μg/m3), SO2 (ERR: 2.518, 95% CI: 1.914, 3.122 per 10 μg/m3), and NO2 (ERR: 1.090, 95% CI: 0.822–1.358 per 10 μg/m3). The trends across lags were statistically significant. The stratified analysis demonstrated that females were more susceptible to SO2 and NO2, while elder individuals aged above 65 years old, compared with younger people, suffered more from air pollution, especially from SO2. Short-term exposure to PM2.5, PM10, SO2, and NO2 were significantly associated with a higher risk of cerebrovascular disease mortality, and elder females seemed to suffer more from air pollution. Further research is required to reveal the underlying mechanisms.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cerebrovascular disease, including a range of conditions that affect the flow of blood through the brain, is highly prevalent in older people and remaining a leading cause of death throughout the world (Truelsen et al. 2000; Feigin et al. 2017). Scientific evidence has shown that air pollution and cerebrovascular diseases are positively related, which could be mediated through direct and indirect effects of exposure to air pollutants on vascular tone, endothelial function, thrombosis, and myocardial ischemia (Brook et al. 2002; Lucking et al. 2008; Lundbäck et al. 2009; Mills et al. 2011). According to the GBD (Global Burden of Disease) report, 12.8% of DALYs for stroke in China were attributable to air pollution in 2017 (Yin et al. 2020). Globally, air pollution was the sixth cause of stroke death from 1990 to 2017 and accounted for 28.1% of DALYs for stroke from environmental factors exposure (air pollution, Pb) (Avan et al. 2019).
A few studies have explored associations between air pollution and cerebrovascular-related outcomes. A meta-analysis with a total of 6.2 million events across 28 countries from 94 studies reported that stroke hospitalization or stroke mortality was positively associated with a short-term increase in concentrations of PM2.5 (RR: 1.011, 95% CI: 1.011–1.012 per 10 μg/m3), PM10 (RR: 1.003, 95% CI: 1.002–1.004 per 10 μg/m3), SO2 (RR: 1.019, 95% CI: 1.011–1.027 per 10 ppb), NO2 (RR: 1.014, 95% CI: 1.009–1.019 per 10 ppb), and O3 (RR: 1.011, 95% CI: 1.011–1.012 per 10 μg/m3) (Shah et al. 2015). More recently, a time-series study in Mexico City showed an increase of 10 μg/m3 in PM2.5 was associated with increased cerebrovascular mortality by 3.43% (95% CI: 0.10–6.28) for lag days 0 to 1, and stronger effects were identified among people over 65 years old (Gutiérrez-Avila et al. 2017). However, results were inconsistent in countries of low-level exposure. Two prospective studies in Sweden and Spain showed no significant associations between long-term exposure to particulate matters and incident stroke events (Ljungman et al. 2019; Vivanco-Hidalgo et al. 2019). In a US study conducted in 2019, short-term exposure to NO2 (OR: 1.24, 95% CI: 1.01–1.52 per interquartile) was found to increase the risk of hemorrhagic stroke, whereas no substantial association was observed for PM2.5, PM10, NO2, and SO2 with a risk of total stroke in post-menopausal women (Sun et al. 2019).
As the largest and most populous city in central China, health effects of air pollution in Wuhan are worth studying. However, most previous studies focused on specific stroke-related health outcomes, and it is not clear yet how air pollution affects the total cerebrovascular disease mortality in Wuhan. Besides, data in previous studies were mostly collected from hospitals (Xiang et al. 2013; Wang et al. 2019; Qi et al. 2020), which may lead to a lack of representativeness and selection bias. In this study, we obtained integral and accurate Wuhan death records directly from the Disease Surveillance Point System (DSPs) and employed generalized additive models (GAM) to explore the association between short-term exposure to air pollution and cerebrovascular disease mortality in Wuhan, China during 2013–2019. This study may have important implications for the risk assessment and prevention of cerebrovascular disease and provide certain epidemiological evidence for policy-makers to curb ambient air pollution in Wuhan.
Materials and methods
Data collection
Cerebrovascular disease mortality data were collected from Disease Surveillance Point System (DSPs) of Wuhan Center for Disease Control and Prevention from 1 January 2013 to 31 December 2019. All death cases are from local residents registered in Wuhan Hukou System. We obtained individual death registration records for cerebrovascular diseases (International Classification of Diseases, 10th revision—ICD10: I60-I69) including death date, age group, gender, and death reason. And then we created a dataset including the daily counts of deaths from cerebrovascular disease chronologically for this period.
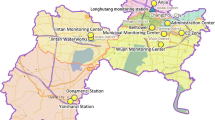
Air pollution data were obtained from 10 national air quality monitoring stations in Wuhan operated by the Wuhan Ecology and Environment Bureau. The average concentration of air pollutants measured in these monitoring stations was used as a proxy for daily exposure to air pollution in Wuhan. We included five air pollutants in our analysis, including average daily PM2.5 (mass of particles with aerodynamic diameter < 2.5 μm), PM10 (mass of particles with aerodynamic diameter < 10 μm), SO2 (sulfur dioxide), NO2 (nitrogen dioxide), and O3 (ground-level ozone) from 1 January 2013 to 31 December 2019. Meteorological data, including average daily temperature and relative humidity, were obtained from Wuhan Meteorological Administration.
The study was approved by the ethics committee of the Wuhan Centers for Disease Control and Prevention. Since the data was analyzed at an aggregate level with no individual information involved, informed consent from the participants was waived for this study.
Statistical analysis
A time-series study design was used to evaluate the association between air pollution and cerebrovascular disease mortality. We first created a time-series dataset including the daily deaths from cerebrovascular disease, day of the week (DOW), the concentration of air pollutants, average daily temperature, and humidity for the period from 1 January 2013 to 31 December 2019 before statistical analysis. Daily deaths from cerebrovascular disease, air pollutants, and meteorological factors were described as mean, standard deviation (SD), and quartiles. Spearman correlation was conducted to explore the relationship between pollutant concentrations and meteorological factors.
A generalized additive regression model (GAM), based on Poisson distribution, was used in performing a time series on daily counts of deaths from cerebrovascular disease and air pollution. The model is as follows:
where E(Yt) is the estimated daily counts of deaths from cerebrovascular diseases at day t; α is the intercept of the model; Zt represents the concentration of each air pollutant on day t, μg/m3; β is the log of relative risk in daily deaths from cerebrovascular disease based on an increase of 10 μg/m3 in air pollutant concentrations; DOW was included as an indicator variable to adjust the weekends. ns is the natural cubic smoothing function for the nonlinear variables such as temperature, humidity, and calendar time, which was applied to control multi-annual and seasonal trends, as well as the meteorological factors; Degrees of freedom (df) was selected by referring to previous literature; In the final model, we defined 7 df per year for time trends, 6 and 3 df per year for temperature and relative humidity respectively (Peng et al. 2006; Zanobetti and Schwartz 2009; Chen et al. 2010).
PM2.5, PM10, SO2, NO2, and O3 were incorporated into the model separately to evaluate the relationship between daily deaths from cerebrovascular disease and each air pollutant. Due to the potential delayed effects of air pollution on cerebrovascular diseases (Shang et al. 2013), we constructed both single-day lag models including lag0–lag5 and multi-day lag models from lag 0–1 to lag 0–5 to explore the adverse effect of air pollutants on developing cerebrovascular diseases at different lag days in this study. We also performed multi-pollutant models to explore the possible confounding effects from the presence of co-pollutants. Furthermore, we tested for potential effect modification by performing additional analysis stratified by gender (males, females) and age group (< 65, ≥ 65).
The effect of each air pollutant on the risk of cerebrovascular disease mortality was reported as excess relative risk (ERR) with 95% confidence intervals (CI). All data sorting and statistical analysis were performed using Excel 2019 and R (version 3.3.3) packages “mgcv” and “nlme”. Results with a 2-sided and p value < 0.05 were statistically significant.
Results
A total of 84,811 cerebrovascular disease deaths were collected from 1 January 2013 to 31 December 2019 in Wuhan. Among all subjects, 53.3% were males, and 83% were 65 years or older (Table 1). During the 7-year period of our study, mean ± SD exposure to air pollution was 64.05 ± 46.29 μg/m3, 95.86 ± 56.09 μg/m3, 15.73 ± 14.37 μg/m3, 54.51 ± 30.49 μg/m3, and 87.21 ± 48.99 μg/m3 for PM2.5, PM10, SO2, NO2, and O3, respectively. Daily mean temperature was 17.18 ± 9.26 °C and relative humidity was 79.07 ± 10.33% (Table 2). According to Pearson’s correlation analysis, most air pollutants were highly correlated with each other except O3 and moderately or poorly correlated with temperature and relative humidity (Table 3).
Table 4 shows the results of the single-pollutant model for exposure to air pollution at different lag days, expressed as ERRs with 10 μg/m3 increments in five air pollutants. When adjusting for average daily temperature, relative humidity, and weekend, as expected, we observed a positive association between PM2.5, PM10, SO2, NO2, and cerebrovascular disease mortality. For single-day effects, the largest positive percent changes of daily deaths from cerebrovascular disease with a 10 μg/m3 increment in pollutant concentration were found at lag0 for PM2.5 (ERR: 0.927%, 95% CI: 0.749–1.105) and at lag1 for PM10 (ERR: 0.627%, 95% CI: 0.493–0.761), SO2 (ERR: 2.518%, 95% CI: 1.914–3.122), and NO2 (ERR: 1.090%, 95% CI: 0.822–1.358), respectively. The effect values gradually reduced with the lag days increasing. In terms of multi-day lags, the strongest effects of PM2.5, PM10, SO2, and NO2 on cerebrovascular mortality were 0.995% (95% CI: 0.774, 1.216) at lag 0–3 days, 0.792% (95% CI: 0.629, 0.954), 2.961% (95% CI: 2.239, 3.683), and 1.151% (95% CI: 0.844, 1.459) at lag 0–2 days, respectively. The effect values in multi-day lags were larger than those single-day lags. Besides, the effects of SO2 on cerebrovascular mortality at all lags were the greatest while the associations were similar among PM2.5, PM10, SO2, and NO2. The evidence of an association between exposure to O3 and mortality due to cerebrovascular diseases was uncertain. (Table 3)
Results of stratified analysis by gender and age group are shown in Fig. 1. Generally, the effects of air pollutants on cerebrovascular disease mortality are similar between different genders, but the effect of SO2 and NO2 is significantly greater in females than males among most lag days. Consistent with the single pollutant model, SO2 has the maximum impact on both males and females among all pollutants. The effect was significantly greater among elders over 65 years old. In contrast, the effect of PM2.5 on young people was similar to or slightly higher than that on the elders. It is noted that among all pollutants, SO2 has the greatest effect on the elderly, and no significant effect was found of O3 on cerebrovascular disease mortality of both two gender groups.
Figure 2 illustrates the Exposure-Response (E-R) relationship between the concentration of air pollutants at lag0 and the relative risks of daily deaths. Generally, the curves of five pollutants presented positive trends, which indicated that the higher concentration of air pollutants might cause a mortality increase. The E-R curve of PM2.5 was S-shaped, first rose sharply towards the peak concentration at about 50 μg/m3, and then slowly increased. The E-R curves of PM10 and O3 grew steadily at low concentrations and then became flat for the concentrations ≥ 100 μg/m3. The almost linear E-R curves of SO2 and NO2 showed a steady trend of continuous growth, indicating that the risk of cerebrovascular mortality ascended steadily as the pollutant concentration increases
Discussion
In our study, based on integral and accurate death records directly from the Disease Surveillance Point System (DSPs) from 2013 to 2017, we have explored the association between cerebrovascular disease mortality and short-term exposure to multiple air pollutants in Wuhan, China. We concluded that after adjusting for temperature, relative humidity, and weekend effect, ambient air pollution was positively associated with the daily deaths from cerebrovascular diseases. We found a stronger association for SO2 and no significant association for O3. In single-pollutant models, the largest effect was found at lag0 for PM2.5 and lag1 for PM10, SO2, NO2. The effect values gradually reduced with the lag days increasing, and the trends across lags were statistically significant. Stratified analysis demonstrated that females were more vulnerable to SO2 and NO2, and compared with younger people, elders over 65 years old suffered more from air pollution, especially from SO2. This study may have important implications for the risk assessment and prevention of cerebrovascular diseases and provides certain epidemiological evidence for policy-makers to curb ambient air pollution in Wuhan, China.
Our results suggest that short-term exposure to PM2.5, PM10, SO2, and NO2 was positively associated with an increased risk of cerebrovascular disease mortality, which is consistent with many previous studies (Zhang et al. 2017; Leepe et al. 2019; Wu et al. 2019). In our single-pollutant models, the adverse effects of PM2.5 on cerebrovascular disease mortality reached peaks at lag0 and PM10, SO2, and NO2 at lag1 in single-day lags. Likewise, these time-lag effects of air pollution on cerebrovascular-related outcomes have also been discussed before, and we found that the effect was greater at short-term lag days, mostly at lag 0 and lag 1 in some Asia studies. A similar study conducted in Taipei showed that PM2.5 and PM10 lagged 3 days; O3 lagged 0 days were significantly associated with increased emergency admissions for cerebrovascular diseases by 2.1% (95% CI: 1.005–1.037), 3% (95% CI: 1.011–1.037), and 3.1% (95% CI: 1.010–1.056), respectively (Chan et al. 2006); a time-series study conducted in Thailand found that PM10 and NO2 have largest effects on total cardiovascular admissions at lag1 with an increase of 0.73% (95% CI: 0.15–1.32), 1.28 (95% CI: 0.65–1.91) while SO2 at lag0 (Phosri et al. 2019). A multicity study of short-term effects of air pollution on mortality conducted in Asia also showed that the average lag 0–1 days usually generated the highest excess risk of cardiovascular mortality in most cities concluded in this study (Wong et al. 2008). This finding is crucial to take timely measures to effectively prevent air pollution and protect the population’s health.
This study also showed that SO2 was the major air pollutant affecting the cerebrovascular mortality among all the five pollutants included in this study and no significant association was found for O3. The results of some previous studies are consistent with our findings (Ren et al. 2017; Zhang et al. 2017; Nhung et al. 2020). A nationwide time-series analysis conducted in China observed that an increment of 1.37% (95% CI: 1.05–1.70) in daily hospital admissions for ischemic stroke was significantly associated with per 10-μg/m3 increase in SO2 (mean SO2 concentration was 27.9 μg/m3) (Tian et al. 2018), which is slightly lower than the estimates of 2.52% in our study. According to a previous meta-analysis, the risks of cardiovascular disease mortality were reduced at higher PM2·5 concentrations (Vodonos et al. 2018), and it is uncertain whether a similar pattern of effect also exists in SO2 which needs further research.
Stratified analysis showed that elder females seemed to suffer more risk of cerebrovascular disease mortality from ambient air pollution. Consistent with previous studies (Shah et al. 2015; Hystad et al. 2020), we found higher vulnerability to air pollution among elderly individuals, especially to SO2. Although the mechanism still remains unclear, according to early research results, older age was the main contributor to cerebrovascular diseases (Kelly-Hayes et al. 2003). Also, the larger risk estimates in elder populations might be associated with differences in the distribution of our research subjects with a majority of older people aged above 65 years old. We also concluded that females were more vulnerable to ambient exposure to SO2 and NO2. A latest prospective cohort study across 21 high-income, middle-income, and low-income countries have reported similar results of gender difference in ambient air pollution on cardiovascular disease mortality (Hystad et al. 2020). However, an ecological time-series study in northern Thailand showed that PM10 exposure was positivity associated with cerebrovascular disease visits with an incidence rate ratio of 1.025% (95% CI: 1.004–1.046) while the relationship for females was insignificant (Mueller et al. 2020). The reasons for our gender-specific findings are unclear and need further investigation. We suggest that more research should focus on the physiological characteristics of different genders to further explain and examine this difference. Given the difference in the population susceptibility to SO2, effective public health prevention policies can be made to reduce the burden of cerebrovascular diseases.
Explanation of the trend of E-R relationships is important for public health development, especially for those sensitive populations that could be protected by limiting ambient air pollutants below threshold levels (Song et al. 2019). In this study, the typical S-shaped curve for PM2.5 tends to hit a plateau at high concentrations. This may be a consequence of the “harvesting effect” that susceptible populations might have already developed symptoms and visited clinics before air pollutant concentration reached a reasonably high level (Chen et al. 2017). That might also explain the linear E-R curve of PM10 and O3, where the daily deaths for cerebrovascular diseases grew significantly slower or even dropped at high concentrations. Specially, we observed a threshold relationship between O3 and cerebrovascular mortality whose curve remained flat and then rose rapidly after the concentration was above 100 μg/m3, which is quite close to the threshold limits for O3 according to WHO Air Quality Guidelines (AQG-global update 2005).
Several studies have explored city-level difference in the relationships between air pollution and cardiovascular-related outcomes in China. According to a national time series analysis (Yin et al. 2017), we found that the PM10 concentration (54.3 μg/m3) in Wuhan ranked 10th among 38 major cities in China, and the maximum likelihood estimates (percentage) (lag = 0) in Wuhan of 10 μg/m3 on total mortality for deaths due to cardiorespiratory diseases were slightly higher than the pooled results. Although the mechanical explanation of adverse effects of air pollution on cerebrovascular mortality remains unclear, several pathways including oxidative stress, systemic inflammation, thrombosis, and vascular endothelial dysfunction have been stated (Huang et al. 2017; Dong et al. 2018; Tian et al. 2018; Yang et al. 2020). Vascular function injury might be central to mechanisms for air pollution-related stroke, which could lead to raised blood pressure and plasma viscosity (Münzel et al. 2018; Chen et al. 2019). It has been shown that exposure to ambient air pollution was associated with increased thrombosis and vascular endothelial dysfunction by provoking oxidative stress and releasing systemic inflammatory cytokines (Rich et al. 2012). Besides, evidence also suggested that exposure to air pollution can lead to dysfunction of the autonomic system, which has been found as the major pathway that could result in air pollution-related adverse cerebrovascular outcomes (Wu et al. 2010).
Our study has several limitations. First, as an inherent limitation of ecological studies, we used the average concentration of air pollutants measured in ten air monitoring stations in Wuhan as a proxy to represent the individual exposure, which may cause misclassification of exposure and ignores the spatial impact of air pollution on cerebrovascular mortality (Winzar 2015). Second, due to data unavailability, we cannot adjust other personal-level risk factors related to cerebrovascular diseases like tobacco use, physical activity, and diet habits (Stafoggia et al. 2014). Third, the detailed information about age was not accessible, so the pooled estimation may bias the effects of air pollutants on specific age groups. Future studies could split the population into more multiple age subgroups to further explore the effect modification of age on the relationship between air pollution and cerebrovascular mortality. Fourth, we cannot rule out the non-relevant death records due to poor physical condition or other reasons than air pollution. Fifth, meteorological exposure assessment may not be comprehensive enough due to data unavailability. More studies are needed to warrant the reliability and generalization of our study.
Conclusions
In our study, based on 7-year death records in Wuhan, we found that exposure to PM2.5, PM10, SO2, and NO2 was positively associated with a higher risk of adverse cerebrovascular events, especially for elder females. Our findings could provide epidemiological evidence for risk assessment of air pollution on cerebrovascular mortality, which may have important implications for policy-makers to curb and prevent ambient air pollution in Wuhan, China.
Availability of data and materials
The data on air pollution and meteorological factors can be obtained from the National Air Pollution Monitoring System (http://www.cnemc.cn) and the China Meteorological Data Sharing Service System (https://data.cma.cn). The data on cerebrovascular disease mortality are available from the corresponding author upon reasonable request.
References
Avan A, Digaleh H, Di Napoli M et al (2019) Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: an ecological analysis from the Global Burden of Disease Study 2017. BMC Med 17:191. https://doi.org/10.1186/s12916-019-1397-3
Brook RD, Brook JR, Urch B, Vincent R, Rajagopalan S, Silverman F (2002) Inhalation of fine particulate air pollution and ozone causes acute arterial vasoconstriction in healthy adults. Circulation 105:1534–1536. https://doi.org/10.1161/01.CIR.0000013838.94747.64
Chan CC, Chuang KJ, Chien LC, Chen WJ, Chang WT (2006) Urban air pollution and emergency admissions for cerebrovascular diseases in Taipei, Taiwan. Eur Heart J 27:1238–1244. https://doi.org/10.1093/eurheartj/ehi835
Chen R, Chu C, Tan J, Cao J, Song W, Xu X, Jiang C, Ma W, Yang C, Chen B, Gui Y, Kan H (2010) Ambient air pollution and hospital admission in Shanghai, China. J Hazard Mater 181:234–240. https://doi.org/10.1016/j.jhazmat.2010.05.002
Chen R, Yin P, Meng X, Liu C, Wang L, Xu X, Ross JA, Tse LA, Zhao Z, Kan H, Zhou M (2017) Fine particulate air pollution and daily mortality: a nationwide analysis in 272 Chinese cities. Am J Respir Crit Care Med 196:73–81. https://doi.org/10.1164/rccm.201609-1862OC
Chen G, Wang A, Li S, Zhao X, Wang Y, Li H, Meng X, Knibbs LD, Bell ML, Abramson MJ, Wang Y, Guo Y (2019) Long-term exposure to air pollution and survival after ischemic stroke: the China national stroke registry cohort. Stroke 50:563–570. https://doi.org/10.1161/STROKEAHA.118.023264
Dong H, Yu Y, Yao S, Lu Y, Chen Z, Li G, Yao Y, Yao X, Wang SL, Zhang Z (2018) Acute effects of air pollution on ischaemic stroke onset and deaths: a time-series study in Changzhou, China. BMJ Open 8:1–8. https://doi.org/10.1136/bmjopen-2017-020425
Feigin VL, Norrving B, Mensah GA (2017) Global burden of stroke. Circ Res 120:439–448. https://doi.org/10.1161/CIRCRESAHA.116.308413
Gutiérrez-Avila I, Rojas-Bracho L, Riojas-Rodríguez H, Kloog I, Rothenberg SJ (2017) Cardiovascular and cerebrovascular mortality associated with acute exposure to PM2.5 in Mexico City. Stroke 49(7):1734–1736. https://doi.org/10.1161/STROKEAHA.118.021034
Huang F, Luo Y, Tan P et al (2017) Gaseous air pollution and the risk for stroke admissions: a case-crossover study in Beijing, China. Int J Environ Res Public Health 14. https://doi.org/10.3390/ijerph14020189
Hystad P, Larkin A, Rangarajan S, AlHabib KF, Avezum Á, Calik KBT, Chifamba J, Dans A, Diaz R, du Plessis JL, Gupta R, Iqbal R, Khatib R, Kelishadi R, Lanas F, Liu Z, Lopez-Jaramillo P, Nair S, Poirier P, Rahman O, Rosengren A, Swidan H, Tse LA, Wei L, Wielgosz A, Yeates K, Yusoff K, Zatoński T, Burnett R, Yusuf S, Brauer M (2020) Associations of outdoor fine particulate air pollution and cardiovascular disease in 157 436 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet Planet Heal 4:e235–e245. https://doi.org/10.1016/S2542-5196(20)30103-0
Kelly-Hayes M, Beiser A, Kase CS, Scaramucci A, D’Agostino RB, Wolf PA (2003) The influence of gender and age on disability following ischemic stroke: the Framingham study. J Stroke Cerebrovasc Dis 12:119–126. https://doi.org/10.1016/S1052-3057(03)00042-9
Leepe KA, Li M, Fang X, Hiyoshi A, Cao Y (2019) Acute effect of daily fine particulate matter pollution on cerebrovascular mortality in Shanghai, China: a population-based time series study. Environ Sci Pollut Res 26:25491–25499. https://doi.org/10.1007/s11356-019-05689-8
Ljungman PLS, Andersson N, Stockfelt L, Andersson EM, Nilsson Sommar J, Eneroth K, Gidhagen L, Johansson C, Lager A, Leander K, Molnar P, Pedersen NL, Rizzuto D, Rosengren A, Segersson D, Wennberg P, Barregard L, Forsberg B, Sallsten G, Bellander T, Pershagen G (2019) Long-term exposure to particulate air pollution, black carbon, and their source components in relation to ischemic heart disease and stroke. Environ Health Perspect 127:1–11. https://doi.org/10.1289/EHP4757
Lucking AJ, Lundback M, Mills NL, Faratian D, Barath SL, Pourazar J, Cassee FR, Donaldson K, Boon NA, Badimon JJ, Sandstrom T, Blomberg A, Newby DE (2008) Diesel exhaust inhalation increases thrombus formation in man. Eur Heart J 29:3043–3051. https://doi.org/10.1093/eurheartj/ehn464
Lundbäck M, Mills NL, Lucking A, Barath S, Donaldson K, Newby DE, Sandström T, Blomberg A (2009) Experimental exposure to diesel exhaust increases arterial stiffness in man. Part Fibre Toxicol 6:1–6. https://doi.org/10.1186/1743-8977-6-7
Mills NL, Miller MR, Lucking AJ, Beveridge J, Flint L, Boere AJF, Fokkens PH, Boon NA, Sandstrom T, Blomberg A, Duffin R, Donaldson K, Hadoke PWF, Cassee FR, Newby DE (2011) Combustion-derived nanoparticulate induces the adverse vascular effects of diesel exhaust inhalation. Eur Heart J 32:2660–2671. https://doi.org/10.1093/eurheartj/ehr195
Mueller W, Loh M, Vardoulakis S, Johnston HJ, Steinle S, Precha N, Kliengchuay W, Tantrakarnapa K, Cherrie JW (2020) Ambient particulate matter and biomass burning: an ecological time series study of respiratory and cardiovascular hospital visits in northern Thailand. Environ Heal A Glob Access Sci Source 19:1–12. https://doi.org/10.1186/s12940-020-00629-3
Münzel T, Gori T, Al-Kindi S et al (2018) Effects of gaseous and solid constituents of air pollution on endothelial function. Eur Heart J 39:3543–3550. https://doi.org/10.1093/eurheartj/ehy481
Nhung NTT, Schindler C, Chau NQ, Hanh PT, Hoang LT, Dien TM, Thanh NTN, Künzli N (2020) Exposure to air pollution and risk of hospitalization for cardiovascular diseases amongst Vietnamese adults: case-crossover study. Sci Total Environ 703:134637. https://doi.org/10.1016/j.scitotenv.2019.134637
Peng RD, Dominici F, Louis TA (2006) Model choice in time series studies of air pollution and mortality. J R Stat Soc Ser A Stat Soc 169:179–203. https://doi.org/10.1111/j.1467-985X.2006.00410.x
Phosri A, Ueda K, Ling V et al (2019) Effects of ambient air pollution on daily hospital admissions for respiratory and cardiovascular diseases in Bangkok, Thailand. Sci Total Environ 651:1144–1153. https://doi.org/10.1016/j.scitotenv.2018.09.183
Qi X, Wang Z, Guo X et al (2020) Short-term effects of outdoor air pollution on acute ischaemic stroke occurrence: a case-crossover study in Tianjin, China. Occup Environ Med 1–6. https://doi.org/10.1136/oemed-2019-106301
Ren M, Li N, Wang Z, Liu Y, Chen X, Chu Y, Li X, Zhu Z, Tian L, Xiang H (2017) The short-term effects of air pollutants on respiratory disease mortality in Wuhan, China: comparison of time-series and case-crossover analyses. Sci Rep 7:1–9. https://doi.org/10.1038/srep40482
Rich DQ, Kipen HM, Huang W, Wang G, Wang Y, Zhu P, Ohman-Strickland P, Hu M, Philipp C, Diehl SR, Lu SE, Tong J, Gong J, Thomas D, Zhu T, Zhang J(J) (2012) Association between changes in air pollution levels during the Beijing olympics and biomarkers of inflammation and thrombosis in healthy young adults. JAMA - J Am Med Assoc 307:2068–2078. https://doi.org/10.1001/jama.2012.3488
Shah ASV, Lee KK, McAllister DA et al (2015) Short term exposure to air pollution and stroke: Systematic review and meta-analysis. BMJ 350. https://doi.org/10.1136/BMJ.h1295
Shang Y, Sun Z, Cao J, Wang X, Zhong L, Bi X, Li H, Liu W, Zhu T, Huang W (2013) Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ Int 54:100–111. https://doi.org/10.1016/j.envint.2013.01.010
Song J, Lu M, Lu J, Chao L, An Z, Liu Y, Xu D, Wu W (2019) Acute effect of ambient air pollution on hospitalization in patients with hypertension: a time-series study in Shijiazhuang, China. Ecotoxicol Environ Saf 170:286–292. https://doi.org/10.1016/j.ecoenv.2018.11.125
Stafoggia M, Cesaroni G, Peters A, Andersen ZJ, Badaloni C, Beelen R, Caracciolo B, Cyrys J, de Faire U, de Hoogh K, Eriksen KT, Fratiglioni L, Galassi C, Gigante B, Havulinna AS, Hennig F, Hilding A, Hoek G, Hoffmann B, Houthuijs D, Korek M, Lanki T, Leander K, Magnusson PK, Meisinger C, Migliore E, Overvad K, Östenson CG, Pedersen NL, Pekkanen J, Penell J, Pershagen G, Pundt N, Pyko A, Raaschou-Nielsen O, Ranzi A, Ricceri F, Sacerdote C, Swart WJR, Turunen AW, Vineis P, Weimar C, Weinmayr G, Wolf K, Brunekreef B, Forastiere F (2014) Long-term exposure to ambient air pollution and incidence of cerebrovascular events: results from 11 European cohorts within the ESCAPE project. Environ Health Perspect 122:919–925. https://doi.org/10.1289/ehp.1307301
Sun S, Stewart JD, Eliot MN, Yanosky JD, Liao D, Tinker LF, Eaton CB, Whitsel EA, Wellenius GA (2019) Short-term exposure to air pollution and incidence of stroke in the Women’s Health Initiative. Environ Int 132:105065. https://doi.org/10.1016/j.envint.2019.105065
Tian Y, Liu H, Zhao Z, Xiang X, Li M, Juan J, Song J, Cao Y, Wang X, Chen L, Wei C, Hu Y, Gao P (2018) Association between ambient air pollution and daily hospital admissions for ischemic stroke: a nationwide time-series analysis. PLoS Med 15:1–16. https://doi.org/10.1371/journal.pmed.1002668
Truelsen T, Begg S, Mathers C (2000) The Global Burden of Cerebrovascular Disease. WHO. https://www.who.int/healthinfo/statistics/bod_cerebrovasculardiseasestroke.pdf
Vivanco-Hidalgo RM, Avellaneda-Gómez C, Dadvand P, Cirach M, Ois Á, Gómez González A, Rodriguez-Campello A, de Ceballos P, Basagaña X, Zabalza A, Cuadrado-Godia E, Sunyer J, Roquer J, Wellenius GA (2019) Association of residential air pollution, noise, and greenspace with initial ischemic stroke severity. Environ Res 179:108725. https://doi.org/10.1016/j.envres.2019.108725
Vodonos A, Awad YA, Schwartz J (2018) The concentration-response between long-term PM 2.5 exposure and mortality: a meta-regression approach. Environ Res 166:677–689. https://doi.org/10.1016/j.envres.2018.06.021
Wang W, Liu C, Ying Z, Lei X, Wang C, Huo J, Zhao Q, Zhang Y, Duan Y, Chen R, Fu Q, Zhang H, Kan H (2019) Particulate air pollution and ischemic stroke hospitalization: how the associations vary by constituents in Shanghai, China. Sci Total Environ 695:133780. https://doi.org/10.1016/j.scitotenv.2019.133780
Winzar H (2015) The ecological fallacy: how to spot one and tips on how to use one to your advantage. Australas Mark J 23:86–92. https://doi.org/10.1016/j.ausmj.2014.12.002
Wong CM, Vichit-Vadakan N, Kan H, Qian Z (2008) Public health and air pollution in Asia (PAPA): a multicity study of short-term effects of air pollution on mortality. Environ Health Perspect 116:1195–1202. https://doi.org/10.1289/ehp.11257
Wu S, Deng F, Niu J, Huang Q, Liu Y, Guo X (2010) Association of heart rate variability in taxi drivers with marked changes in particulate air pollution in Beijing in 2008. Environ Health Perspect 118:87–91. https://doi.org/10.1289/ehp.0900818
Wu T, Ma Y, Wu X et al (2019) Association between particulate matter air pollution and cardiovascular disease mortality in Lanzhou, China. Environ Sci Pollut Res 15262–15272. https://doi.org/10.1007/s11356-019-04742-w
Xiang H, Mertz KJ, Arena VC, Brink LL, Xu X, Bi Y, Talbott EO (2013) Estimation of short-term effects of air pollution on stroke hospital admissions in Wuhan, China. PLoS One 8:1–5. https://doi.org/10.1371/journal.pone.0061168
Yang BY, Fan S, Thiering E, Seissler J, Nowak D, Dong GH, Heinrich J (2020) Ambient air pollution and diabetes: a systematic review and meta-analysis. Environ Res 180:108817. https://doi.org/10.1016/j.envres.2019.108817
Yin P, He G, Fan M, Chiu KY, Fan M, Liu C, Xue A, Liu T, Pan Y, Mu Q, Zhou M (2017) Particulate air pollution and mortality in 38 of China’s largest cities: time series analysis. BMJ 356:1–12. https://doi.org/10.1136/bmj.j667
Yin P, Brauer M, Cohen AJ, Wang H, Li J, Burnett RT, Stanaway JD, Causey K, Larson S, Godwin W, Frostad J, Marks A, Wang L, Zhou M, Murray CJL (2020) The effect of air pollution on deaths, disease burden, and life expectancy across China and its provinces, 1990–2017: an analysis for the Global Burden of Disease Study 2017. Lancet Planet Heal 5196:1–13. https://doi.org/10.1016/s2542-5196(20)30161-3
Zanobetti A, Schwartz J (2009) The effect of fine and coarse particulate air pollution on mortality: a national analysis. Environ Health Perspect 117:898–903. https://doi.org/10.1289/ehp.0800108
Zhang C, Ding R, Xiao C, Xu Y, Cheng H, Zhu F, Lei R, di D, Zhao Q, Cao J (2017) Association between air pollution and cardiovascular mortality in Hefei, China: a time-series analysis. Environ Pollut 229:790–797. https://doi.org/10.1016/j.envpol.2017.06.022
Funding
This research was funded by Basic Applied Research Project of Wuhan Science and Technology Bureau, grant number 2015061701011631.
Author information
Authors and Affiliations
Contributions
Conceptualization: Yaqiong Yan, Jie Gong, and Hao Xiang
Data curation: Niannian Yang;
Funding acquisition: Yaqiong Yan, and Hao Xiang;
Methodology: Yan Guo;
Software: Xi Chen;
Supervision: Hao Xiang, and Jie Gong;
Validation: Juan Dai
Writing—original draft: Chuangxin Wu;
Writing—review and editing: Yuanyuan Zhao.
All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
The study was approved by the ethics committee of the Wuhan Centers for Disease Control and Prevention. Since the data was analyzed at an aggregate level with no individual information involved, informed consent from the participants was waived for this study.
Consent for publication
Not applicable
Additional information
Responsible editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Yan, Y., Chen, X., Guo, Y. et al. Ambient air pollution and cerebrovascular disease mortality: an ecological time-series study based on 7-year death records in central China. Environ Sci Pollut Res 28, 27299–27307 (2021). https://doi.org/10.1007/s11356-021-12474-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-12474-z