Abstract
Background
Previous studies addressing the question of whether continuous positive airway pressure (CPAP) could improve the insulin resistance and glucose control in patients with obstructive sleep apnea (OSA) have led to conflicting results. Therefore, we conducted the meta-analysis to evaluate the effects of CPAP on glycemic control and insulin resistance in OSA patients.
Methods
We searched PubMed, HighWire Press, Ovid Medline (R), Cochrane library, and EMBASE before December 2011 on original English language studies. The meta-analysis was conducted using Review Manager Version 5.
Results
The summary estimate for mean difference of homeostasis model assessment insulin resistance (HOMA) from 12 non-diabetic studies was −0.55 (95 % CI, −0.91 to −0.20; P = 0.002). When compared with fasting blood glucose at baseline, 3 to 24 weeks of CPAP treatment did not improve glycemic control in non-diabetic subjects (−0.12; 95 % CI, −0.3 to 0.06; P = 0.20), as well as in diabetic subjects (−0.71; 95 % CI, −2.24 to 0.83; P = 0.37). There were no intervention-related changes in body mass index.
Conclusions
Our analysis showed that CPAP significantly improved insulin resistance in non-diabetic patients with moderate to severe OSA, while no significant change in body mass index was detected. Compared with fasting blood glucose at baseline, there was no change in glycemic control with CPAP. Further large-scale, randomized, and controlled studies are needed to evaluate the longer treatment and its possible effects on weight loss and glycemic homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a common disorder characterized by recurrent episodes of partial or complete obstruction of the upper airway during sleep, leading to intermittent hypoxia and sleep fragmentation. It is estimated that 24 % of men and 9 % of women in the middle-aged individuals meet the minimal diagnostic criteria for OSA (≥5 apnea–hypopnea events per hour of sleep) [1]. Accumulating evidence implicates that OSA may be associated with insulin resistance, glucose intolerance, and metabolic syndrome, but independent of obesity. Obesity, specifically central obesity, is very common in patients with OSA who may gain weight more easily than the equally obese without OSA [2].
The primary treatment for OSA is continuous positive airway pressure (CPAP), which benefits the patients by maintaining upper airway patency. Previous studies addressing the question of whether CPAP could improve the insulin resistance and glucose control in these OSA patients have led to conflicting results. Some investigations demonstrate that adherence to CPAP treatment plays an important role in ameliorating insulin resistance or glucose intolerance, without significant changes in body weight [3–5]. However, other studies reported that the relationship between insulin resistance and OSA was entirely dependent on body mass and failed to show any improvement with CPAP therapy [6, 7].
To update the state of knowledge in this area, we conducted a meta-analysis of the effects of continuous positive airway pressure on glycemic control and insulin resistance in patients with OSA. Given the potential role of obesity in the prevalence of insulin resistance or glucose intolerance, we also evaluated the changes of body mass index (BMI) before and after CPAP intervention.
Methods
Literature search
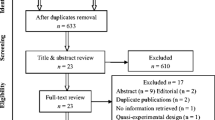
We searched PubMed, HighWire Press, Ovid Medline (R), Cochrane library, and EMBASE before December 2011 on original English language studies, using the following search terms: “sleep disordered breathing” or “obstructive sleep apnea” and “CPAP” and “insulin resistance”. Although other methods had been developed and validated to evaluate insulin resistance, such as quantitative insulin sensitivity check index and fasting plasma glucose-to-insulin ratio, homeostasis model assessment insulin resistance (HOMA-IR) calculated by a mathematical model (fasting insulin (microunits per milliliter) × fasting glucose (millimoles per liter)/22.5), correlates well with the glucose disposal rate derived from the hyperinsulinemic euglycemic clamp [8, 9] and is universally used in non-diabetic populations [10, 11]. After review the titles and abstracts of retrieved articles, 390 duplicate and unrelated searches were first removed; then, 40 were identified for additional scrutiny. Further exclusions (23 papers) were made through perusal of full texts and two studies were subsequently excluded from the meta-analysis. Finally, 15 were eligible for the meta-analysis.
Selection criteria
Studies that met the following criteria were included: (1) prospective observational studies; (2)the study populations were limited to adults with newly diagnosed moderate to severe OSA receiving CPAP therapy; (3) duration of CPAP intervention was >2 weeks; (4) HOMA-IR, fasting glucose, and BMI were measured before and after CPAP. All the selected articles were independently reviewed by two investigators (DY and HY) to determine whether they could be included in this meta-analysis.
Data collection and analysis
The longitudinal data extracted from each paper included first author, year of publication, study design, sample size, mean age, mean BMI, AHI, duration of CPAP intervention, adherence with CPAP, fasting glucose, and HOMA-IR before and after therapy. The articles with overlapping data sets or the same study subjects were excluded.
The meta-analysis was conducted using Review Manager Version 5. Estimates of summary statistics on BMI, fasting glucose, and HOMA-IR in humans at baseline and post-treatment of CPAP, were calculated as mean differences (MD) and corresponding 95 % confidence intervals (95 % CI). To calculate pooled results, studies were weighted by inverse variance method with a random-effects or a fixed-effects model. The I 2 index and corresponding 95 % CI were used to summarize variability of outcomes derived from heterogeneity between the trials [12, 13]. If I 2 is <50 %, a fixed-effects model was used; otherwise, the random-effects model was adopted. All the papers that resulted in significant heterogeneity of the studies in the meta-analysis were removed from the meta-analysis. Potential publication bias was observed using a funnel plot.
Results
Study characteristics
A total of 430 papers that fitted our criteria for inclusion were retrieved from PubMed, HighWire Press, Ovid Medline (R), and EMBASE before December 2011. Three hundred ninety papers were excluded because they were duplicate articles or otherwise did not meet our inclusion criteria, or requisite data were not available. Thus, 40 were identified for additional scrutiny. Of the 40 studies, 23 papers were subsequently dropped from the review after further exclusions were made through review of full texts, and two studies (Garcia et al. [14] and Henley et al. [15]) were excluded from the meta-analysis for significant heterogeneity or too much weight (>60 %) on the meta-analyses of fasting blood glucose, HOMA-IR, and BMI. Finally, 15 were eligible for the meta-analysis (Table 1).
Quantitative synthesis
Meta-analysis of fasting blood glucose in OSA with CPAP
Eleven of the 15 studies reviewed in this section were qualified for inclusion. Of these 11studies, 9 studies provided glycemic data for non-diabetic OSA while 2 studies for those with diabetes. The analysis showed that compared with fasting blood glucose at baseline, 3 to 24 weeks of CPAP treatment did not improve glycemic control in non-diabetic subjects (−0.12; 95 % CI, −0.3 to 0.06; P = 0.20; Fig. 1). For diabetic subjects, there was also no change in glycemic control with CPAP (−0.71; 95 % CI, −2.24 to 0.83; P = 0.37) and insufficient data could be extracted to make conclusive statement.
Meta-analysis of effects of CPAP on HOMA-IR
To estimate the pooled mean difference of HOMA-IR from 12 non-diabetic studies, a meta-analysis was performed. No significant heterogeneity was observed among these studies (I 2 = 28, P > 0.10).The summary estimate for mean HOMA-IR difference was −0.55 (95 % CI, −0.91to −0.20; P = 0.002; Fig. 2). That is to say, CPAP therapy led to an improvement in non-diabetic HOMR-IR of 0.55 points lower than pre-treatment. As for diabetic subjects, West et al. reported that CPAP might have a trend in decrease of mean HOMA-IR value in comparison with pre-CPAP (−1.5; 95 % CI, −3.39 to o.39).
Meta-analysis of BMI for OSA with CPAP
There were no intervention-related changes in BMI in six non-diabetic studies (0.22, 95 % CI, −0.96 to 1.40, P = 0.72) and two diabetic studies (−0.03, 95 % CI, −2.84 to 2.78, P = 0.98; Fig. 3).
No evidence of publication biases was observed in the graphed funnel plots of the above meta-analysis.
Discussion
In our meta-analysis, therapeutic CPAP in non-diabetic subjects with moderate to severe OSA resulted in a significant decrease in HOMA-IR. However, there was no intervention-related reduction in BMI. The analysis also indicated that compared with fasting blood glucose at baseline, 3 to 24 weeks of CPAP treatment did not have different effects on glucose levels.
This meta-analysis has a number of strengths that increase confidence to our findings. Firstly, after removing the individual high heterogeneity, there was no significant evidence of heterogeneity across the studies. Secondly, we constructed a funnel plot that did not suggest a substantial effect of publication bias. Thirdly, the compliance of CPAP use, AHI, and other baseline characteristics were comparable among studies.
Nevertheless, the review also has several limitations. Firstly, small sample population with overweight to obese may limit the generalizability of the results. So, additional large scale, different demography, and randomized controlled trials are needed to confirm these results. Secondly, the use of only English language papers only may cause some publication biases. Thirdly, the duration of CPAP therapy, ranging from 3 to 24 weeks, may be relatively shorter, which could not exert ameliorative effects on weight loss and glycemic homeostasis. Further studies are required to evaluate longer treatment and its possible effects.
Despite of these limitations, our data showed that insulin resistance could be improved after CPAP treatment without significant alteration of BMI and thereby indirectly demonstrated that OSA may induce insulin resistance independent of obesity [3–5]. It is well-established that insulin resistance is essential to the development of multiple metabolic disorders, including prediabetes or type 2 diabetes and lipid abnormalities, which are known to increase cardiovascular risk. Several population-based prospective studies demonstrated that insulin resistance was significantly related to coronary heart disease and stroke [16, 17]. Furthermore, the Insulin Resistance Atherosclerosis Study showed insulin resistance was positively associated with intimal medial thickness of the carotid artery [18]. Therefore, the earlier the CPAP is instituted as a treatment for moderate to severe OSA, the greater it will bring the benefits to cardiovascular protection.
HOMA-IR is regarded as a simple, inexpensive, and reliable surrogate measure of insulin resistance [19], predicting both diabetes and cardiovascular disease outcomes in many epidemiological studies [11, 20–22]. In the Women’s Health Initiative Observational Study [22], with a median follow-up period of 5.9 years, the estimated relative risk of diabetes per SD increment in HOMA-IR were 3.40 (2.95–3.92), adjusting for matching factors and diabetes risk factors. Additionally, prospective data from the Verona Diabetes Complications Study [21] showed that a 1-unit increase in HOMA-IR value was associated with an odds ratio for incident CVD of 1.56, after a mean follow-up of 4.5 years. Thus, in our meta-analysis, the measured change of HOMA-IR index (−0.55) might have beneficial effects not only on risk of diabetes but also on prevalence of CVD in patients with type 2 diabetes.
For the evaluation of fasting blood glucose, the result indicated that 3 to 24 weeks of CPAP treatment did not improve glycemic control in non-diabetic subjects compared with pre-CPAP. Possible reason may be explained by the reported increase in plasma growth hormone during CPAP treatment [23, 24]. Growth hormone causes strong lipolytic effect, increase in the supply of free fatty acids, decrease in glucose utilization by skeletal muscles and thus leads to hyperglycemia [25].
In conclusion, CPAP significantly improves insulin resistance in non-diabetic patients with moderate to severe OSA, without significant changes in BMI. Compared with fasting blood glucose at baseline, there was no change in glycemic control with CPAP. Further large-scale, randomized, and controlled studies are needed to evaluate the longer treatment and its possible effects on weight loss and glycemic homeostasis.
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Phillips BG, Hisel TM, Kato M, Pesek CA, Dyken ME, Narkiewicz K, Somers VK (1999) Recent weight gain in patients with newly diagnosed obstructive sleep apnea. J Hypertens 17:1297–1300
Ip MS, Lam B, Ng MM, Lam WK, Tsang KW, Lam KS (2002) Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med 165:670–676
Punjabi NM, Ahmed MM, Polotsky VY, Beamer BA, O'Donnell CP (2003) Sleep-disordered breathing, glucose intolerance, and insulin resistance. Respir Physiol Neurobiol 136:167–178
Harsch IA, Hahn EG, Konturek PC (2005) Insulin resistance and other metabolic aspects of the obstructive sleep apnea syndrome. Med Sci Monit: Int Med J Exp Clin Res 11:RA70–RA75
Saarelainen S, Lahtela J, Kallonen E (1997) Effect of nasal CPAP treatment on insulin sensitivity and plasma leptin. J Sleep Res 6:146–147
Smurra M, Philip P, Taillard J, Guilleminault C, Bioulac B, Gin H (2001) CPAP treatment does not affect glucose-insulin metabolism in sleep apneic patients. Sleep Med 2:207–213
Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, Monauni T, Muggeo M (2000) Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care 23:57–63
Katsuki A, Sumida Y, Gabazza EC, Murashima S, Furuta M, Araki-Sasaki R, Hori Y, Yano Y, Adachi Y (2001) Homeostasis model assessment is a reliable indicator of insulin resistance during follow-up of patients with type 2 diabetes. Diabetes Care 24:362–365
Hermans MP, Levy JC, Morris RJ, Turner RC (1999) Comparison of tests of beta-cell function across a range of glucose tolerance from normal to diabetes. Diabetes 48:1779–1786
Haffner SM, Kennedy E, Gonzalez C, Stern MP, Miettinen H (1996) A prospective analysis of the HOMA model. The Mexico City Diabetes Study. Diabetes Care 19:1138–1141
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Garcia JM, Sharafkhaneh H, Hirshkowitz M, Elkhatib R, Sharafkhaneh A (2011) Weight and metabolic effects of CPAP in obstructive sleep apnea patients with obesity. Respir Res 12:80
Henley DE, Buchanan F, Gibson R, Douthwaite JA, Wood SA, Woltersdorf WW, Catterall JR, Lightman SL (2009) Plasma apelin levels in obstructive sleep apnea and the effect of continuous positive airway pressure therapy. J Endocrinol 203:181–188
Lempiainen P, Mykkanen L, Pyorala K, Laakso M, Kuusisto J (1999) Insulin resistance syndrome predicts coronary heart disease events in elderly nondiabetic men. Circulation 100:123–128
Pyorala M, Miettinen H, Halonen P, Laakso M, Pyorala K (2000) Insulin resistance syndrome predicts the risk of coronary heart disease and stroke in healthy middle-aged men: the 22-year follow-up results of the Helsinki Policemen Study. Arterioscler Thromb Vasc Biol 20:538–544
Howard G, O'Leary DH, Zaccaro D, Haffner S, Rewers M, Hamman R, Selby JV, Saad MF, Savage P, Bergman R (1996) Insulin sensitivity and atherosclerosis. The Insulin Resistance Atherosclerosis Study (IRAS) Investigators. Circulation 93:1809–1817
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Li CL, Tsai ST, Chou P (2003) Relative role of insulin resistance and beta-cell dysfunction in the progression to type 2 diabetes—The Kinmen Study. Diabetes Res Clin Pract 59:225–232
Bonora E, Formentini G, Calcaterra F, Lombardi S, Marini F, Zenari L, Saggiani F, Poli M, Perbellini S, Raffaelli A, Cacciatori V, Santi L, Targher G, Bonadonna R, Muggeo M (2002) HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects: prospective data from the Verona Diabetes Complications Study. Diabetes Care 25:1135–1141
Song Y, Manson JE, Tinker L, Howard BV, Kuller LH, Nathan L, Rifai N, Liu S (2007) Insulin sensitivity and insulin secretion determined by homeostasis model assessment and risk of diabetes in a multiethnic cohort of women: the Women's Health Initiative Observational Study. Diabetes Care 30:1747–1752
Saini J, Krieger J, Brandenberger G, Wittersheim G, Simon C, Follenius M (1993) Continuous positive airway pressure treatment. Effects on growth hormone, insulin and glucose profiles in obstructive sleep apnea patients. Horm Metab Res = Hormon Stoffwechselforschung = Horm Metab 25:375–381
Cooper BG, White JE, Ashworth LA, Alberti KG, Gibson GJ (1995) Hormonal and metabolic profiles in subjects with obstructive sleep apnea syndrome and the acute effects of nasal continuous positive airway pressure (CPAP) treatment. Sleep 18:172–179
Randle PJ, Garland PB, Hales CN, Newsholme EA (1963) The glucose fatty-acid cycle. Its role in insulin sensitivity and the metabolic disturbances of diabetes mellitus. Lancet 1:785–789
Barceló A, Barbé F, de la Peña M, Martinez P, Soriano JB, Piérola J, Agustí AG (2008) Insulin resistance and daytime sleepiness in patients with sleep apnoea. Thorax 63:946–950
Carneiro G, Togeiro SM, Ribeiro-Filho FF, Truksinas E, Ribeiro AB, Zanella MT, Tufik S (2009) Continuous positive airway pressure therapy improves hypoadiponectinemia in severe obese men with obstructive sleep apnea without changes in insulin resistance. Metab Syndr Relat Disord 7:537–542
Chung S, Yoon IY, Lee CH, Kim JW (2011) The effects of nasal continuous positive airway pressure on vascular functions and serum cardiovascular risk factors in obstructive sleep apnea syndrome. Sleep Breathing = Schlaf Atmung 15:71–76
Cuhadaroglu C, Utkusavas A, Ozturk L, Salman S, Ece T (2009) Effects of nasal CPAP treatment on insulin resistance, lipid profile, and plasma leptin in sleep apnea. Lung 187:75–81
Dawson A, Abel SL, Loving RT, Dailey G, Shadan FF, Cronin JW, Kripke DF, Kline LE (2008) CPAP therapy of obstructive sleep apnea in type 2 diabetics improves glycemic control during sleep. J Clin Sleep Med: JCSM: Off Publ Am Acad Sleep Med 4:538–542
de Lima AM, Franco CM, de Castro CM, Bezerra Ade A, Ataide L Jr, Halpern A (2010) Effects of nasal continuous positive airway pressure treatment on oxidative stress and adiponectin levels in obese patients with obstructive sleep apnea. Respir Int Rev Thorac Dis 79:370–376
Dorkova Z, Petrasova D, Molcanyiova A, Popovnakova M, Tkacova R (2008) Effects of continuous positive airway pressure on cardiovascular risk profile in patients with severe obstructive sleep apnea and metabolic syndrome. Chest 134:686–692
Lindberg E, Berne C, Elmasry A, Hedner J, Janson C (2006) CPAP treatment of a population-based sample—what are the benefits and the treatment compliance? Sleep Med 7:553–560
Murri M, Alcazar-Ramirez J, Garrido-Sanchez L et al (2009) Oxidative stress and metabolic changes after continuous positive airway pressure treatment according to previous metabolic disorders in sleep apnea-hypopnea syndrome patients. Transl Res: J Lab Clin Med 154:111–121
Nena E, Steiropoulos P, Tzouvelekis A, Tsara V, Hatzizisi O, Kyriazis G, Froudarakis M, Trakada G, Papanas N, Bouros D (2010) Reduction of serum retinol-binding protein-4 levels in nondiabetic obstructive sleep apnea patients under continuous positive airway pressure treatment. Respir Int Rev Thorac Dis 80:517–523
Nguyen PK, Katikireddy CK, McConnell MV, Kushida C, Yang PC (2010) Nasal continuous positive airway pressure improves myocardial perfusion reserve and endothelial-dependent vasodilation in patients with obstructive sleep apnea. J Cardiovasc Magn Reson: Off J Soc Cardiovasc Magn Reson 12:50
Patruno V, Aiolfi S, Costantino G, Murgia R, Selmi C, Malliani A, Montano N (2007) Fixed and autoadjusting continuous positive airway pressure treatments are not similar in reducing cardiovascular risk factors in patients with obstructive sleep apnea. Chest 131:1393–1399
Steiropoulos P, Papanas N, Nena E, Tsara V, Fitili C, Tzouvelekis A, Christaki P, Maltezos E, Bouros D (2009) Markers of glycemic control and insulin resistance in non-diabetic patients with obstructive sleep apnea hypopnea syndrome: does adherence to CPAP treatment improve glycemic control? Sleep Med 10:887–891
Trenell MI, Ward JA, Yee BJ, Phillips CL, Kemp GJ, Grunstein RR, Thompson CH (2007) Influence of constant positive airway pressure therapy on lipid storage, muscle metabolism and insulin action in obese patients with severe obstructive sleep apnoea syndrome. Diabetes Obes Metab 9:679–687
West SD, Nicoll DJ, Wallace TM, Matthews DR, Stradling JR (2007) Effect of CPAP on insulin resistance and HbA1c in men with obstructive sleep apnoea and type 2 diabetes. Thorax 62:969–974
Declaration of interest
The authors have no relevant interest to declare. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, D., Liu, Z., Yang, H. et al. Effects of continuous positive airway pressure on glycemic control and insulin resistance in patients with obstructive sleep apnea: a meta-analysis. Sleep Breath 17, 33–38 (2013). https://doi.org/10.1007/s11325-012-0680-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-012-0680-8