Abstract
Neuroinflammation limits tissue damage in response to pathogens or injury and promotes repair. There are two stages of inflammation, initiation and resolution. P2X receptors are gaining attention in relation to immunology and inflammation. The P2X7 receptor in particular appears to be an essential immunomodulatory receptor, although P2X1 and P2X4 receptors also appear to be involved. ATP released from damaged or infected cells causes inflammation by release of inflammatory cytokines via P2X7 receptors and acts as a danger signal by occupying upregulated P2X receptors on immune cells to increase immune responses. The purinergic involvement in inflammation is being explored for the development of novel therapeutic strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
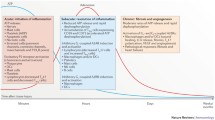
Inflammation involves a complex haemostatic mechanism that enables the body to detect and fight foreign antigens and restore tissue integrity. ATP serves as an acute ‘danger signal’ and behaves as a mediator of inflammation and immunity [1, 2]. Purinergic signalling contributes to the fine tuning of inflammation and immune responses in such a way that the danger to the host is eliminated efficiently with minimal damage to healthy tissues [3]. Brain inflammation occurs following responses to insults, such as bacterial and viral infection, stroke, traumatic injury, and neurodegenerative disorders. During the course of inflammation, there is upregulation of P2X purinoceptors located on immune cells (neutrophils, eosinophils, monocytes, macrophages, mast cells, and lymphocytes). ATP release from injured cells enhances the inflammatory response through increased synthesis of prostaglandin E2 (PGE2) [4] via P2X7 receptors [5]. P2X receptor involvement in inflammation also occurs in irritable bowel syndrome [6, 7], lung injury and fibrosis [8, 9], systemic inflammation [10], arthritis [11], fever [12], and rhinosinusitis [13]. Purinergic signalling in different inflammatory cells involves purinoceptor responses in immune cells (see [14]). Microglia are immune cells in the central nervous system (CNS) [15]. They mediate neuroinflammatory responses to insult in response to a variety of triggers, including toxic metabolites and autoimmunity by detection of pathogens [16]. In addition to microglia, astrocytes as well as perivascular monocytes and macrophages invading to sites of insult from the circulation promote neuroinflammation [17]. Neuronal activity also contributes to inflammation [18]. Activation of P2X7 receptors promotes neuroinflammation by causing the release of inflammatory cytokines, such as interleukin (IL)-1β and tumour necrosis factor-α [19–21]. P2X3 receptors are upregulated in the colonic mucosa of humans with inflammatory bowel disease [22]. There is increased release of ATP from endothelial cells during acute inflammation [23]. ATP triggers cytokine release from inflammatory cells, acts as a chemotactic factor and, after breakdown by ectoenzymes to adenosine, is a potent immunosuppressant [24, 25]. ATP may reach a concentration of several hundred micromoles within the interstitium of inflamed tissues [26, 27]. P2X receptors play a central role in inflammation, particularly the P2X7 receptor. P2X1 receptors [28, 29] and P2X4 receptors [30] probably also play a role in inflammation and immunity (Fig. 1).
Release of extracellular adenosine triphosphate (ATP) and adenosine diphosphate (ADP) and activation of ATP (P2) receptors during inflammation. During inflammatory conditions that occur in vascular thrombosis, hypoxia, ischemia, inflammatory bowel disease, and acute lung injury, multiple cell types release nucleotides, typically in the form of ATP or ADP, from the intracellular compartment into the extracellular space. The release of nucleotides includes release of ATP from necrotic cells, pannexin-hemichannel-dependent release of ATP during apoptosis, and release of ATP through connexin hemichannels from activated inflammatory cells such as polymorphonuclear granulocytes (neutrophils). In addition, release of extracellular ATP has been shown to occur through vesicular exocytosis or connexin hemichannels from endothelial and urothelial cells, osteoblasts, and astrocytes, as well as nerves (not shown). An additional source of extracellular nucleotides in inflammatory conditions is provided by activated platelets, which release ATP and ADP through the release of granules and exocytosis. In the extracellular space, these nucleotides function as signalling molecules that can activate P2Y receptors (G protein-coupled receptors) or P2X receptors (ligand-gated ion channels). Examples of nucleotide-receptor signalling in inflammatory conditions include P2Y6- or P2X7-receptor signalling, which mediates vascular inflammation, and P2Y1-, P2X1-, and P2Y12-receptor signalling, which mediate platelet activation. Activation of P2 receptors of the P2Y2 and P2X7 family that are expressed on dendritic cells is thought to play a role in promoting lung inflammation in chronic lung diseases such as asthma (reproduced from [9], with permission from the Massachusetts Medical Society)
Multiple inflammatory mediators, including cytokines, chemokines, and prostaglandins, are elevated in the cerebrospinal fluid and in post-mortem brain tissues of patients with a history of neuroinflammatory conditions, as well as neurodegenerative diseases [31]. P2X receptors are involved in immune-related neuroinflammatory dysfunctions, including ischaemia and neurodegenerative diseases (see [32]).
Activation of an inflammasome, a protein complex consisting of caspase-1, apoptosis-associated speck-like protein, and nod-like receptor proteins (NLRP1 or NLRP3) [33] expressed in myeloid immune precursor cells is involved. NLRP inflammasomes are activated by the recognition of pathogens-associated molecular patterns or damage-associated molecular patterns (DAMPs) [34]. Inflammasomes are involved in P2X7 receptor coupling to IL-1β release [19].
ATP release occurs from damaged cells at the site of injury and from activated immune cells, glial cells, and endothelial cells. ATP release in vivo has also been shown in response to contact allergens [35], irradiation, allograft rejection [36], and intraperitoneal lipopolysaccharide administration [4], as well as mechanical distortion [37, 38]. ATP released during viral infection is an important inflammatory regulator that activates the inflammasome pathway and regulates inflammatory responses [39]. P2X4 receptors were claimed to influence inflammasome activation after spinal cord injury [40]. The secretion of ATP by bacteria infected macrophages leads to activation of P2X7 receptors [41]. Prevention of cell death or ATP release through p38 or AKT activation interfered with inflammasome activation and IL-1β production. Overexpression of P2X7 receptors was reported in the intestinal mucosa of Crohn’s (inflammatory) disease patients [42].
Reviews focussing on nucleotide signalling during inflammation are available [14, 43–47].
Inflammation and P2X receptors
Changes in P2X receptor subtype expression in neuroinflammatory conditions in various in vitro and in vivo models have been reported. P2X4 receptors are associated with an early inflammatory mediator, PGE2 [30]. P2X4 receptors, similar to P2X7, form a large conductance pore on the cell membrane, facilitating ion efflux and subsequent inflammasome activation [5]. The P2X4 receptor may act as an initial trigger, while the P2X7 receptor, in concert with pannexin 1, may amplify the signal [47]. The P2X4 receptor contribution to PGE2 release in mice is of minor relevance when compared to that of P2X7 receptors [4].
Of the seven P2X subtypes, the P2X7 receptor is the most important for involvement in mediating neuroinflammation [20]. Activation of P2X7 receptors results in DAMP, initiating neuroinflammatory cascades [5]. Further, the formation of the P2X7 receptor pore appears to be necessary for activating the inflammasome [48]. The P2X7 receptor is one of the most potent plasma membrane receptors responsible for the release of inflammatory cytokines of the IL-1 family, IL2, IL6, and IL18 [45, 49, 50]. P2X7 receptor activation is a strong stimulus for IL-18 as well as Il-1β [51, 52] and IL-1α secretion [53]. Microglia are the main source of IL-1β release, but it has also been claimed that IL-1β release from neurons is important [40]. IL-2 synthesis in lymphocytes requires functional P2X receptors [54], probably P2X7 [55, 56]. P2X7 receptors also mediate biglycan-stimulated IL-1β release from mouse macrophages [57]. A P2X7 receptor-P2X4 receptor interaction in the process of IL-1β and IL-18 release has been identified in bone marrow-derived dendritic cells [58]. Smoking contributes to the pro-inflammatory status of perivascular visceral adipose tissue by enhancing the expression and activity of the P2X7 receptor-inflammasome complex [59]. Stimulation of P2X7 receptors drives release of both exosomes and microvesicles from several different cell types relevant to inflammation.
P2X7 receptors are expressed on glial and immune cells of monocyte-macrophage origin and on presynaptic terminals on neurons, with the highest levels on microglia [60–63]. P2X7 receptors, acting via different pathways, play a major role in the promotion as well as in the suppression of inflammation in different pathophysiological conditions ([64, 65] and see [46]). P2X7 receptors mediate transforming growth factor β secretion. P2X7 receptor activation also releases a potent immunosuppressive agent, HLA-G [66, 67] and vascular endothelial growth factor, another major player in inflammation [68]. Another function of P2X7 receptors in inflammation is the activation of transcription factors such as NFkB and NFAT [69, 70]. P2X7 receptor activation opens a cation-specific channel activating several pathways, including the inflammasome, leading to the stress-activated protein kinase pathway that results in apoptosis, and the mitogen-activated protein kinase pathway. Ectonucleotidases control P2X7 receptor function, including the resolution as well as the initial phases of inflammation (see [71]). [11C]-A-740003, a P2X7 receptor antagonist, has been used as a novel tracer of neuroinflammation [72].
P2X7 receptors trigger the activation of the NLRP3 inflammasome, the main intracellular complex involved in the transduction of danger signals and in the initiation of inflammation [73]. The role of the NLRP3 inflammasome in pro-IL-1β processing and pyroptosis places the P2X7 receptor at the centre of cytokine immunology. Since the discovery of the inflammasome [33], whether activation by pathogen- and damage-associated molecular patterns requires a direct, physical, interaction with the scaffold NLR inflammasome proteins has been discussed. Ca2+ might be a suitable second messenger responsible for inflammasome activation [39], and this would be consistent with the role of the P2X7 receptor as a trigger of the NLRP3 inflammasome since P2X7 receptor opening drives a large Ca2+ influx from the extracellular space.
ATP, the extracellular messenger of cellular injury, accumulates to hundred micromolar levels at sites of injury and inflammation [26, 27]. In the presence of inflammation or stress, there is a fast increase of extracellular ATP to near millimolar levels quickly mediating stimulation of pro-inflammatory pathways [74]. Some P2X7 receptor polymorphisms appear to protect against infection, but others increase the risk of developing chronic inflammatory diseases [75].
Immune cells and inflammation
The participation of P2X receptors in inflammation and immunity is gaining attention probably because of the role played by P2X7 receptors in IL-1β processing and release. All immune cells, whether of the myeloid or lymphoid lineage, express at least one P2X receptor subtype, and many express all seven subtypes [2, 45, 76–81]. Mononuclear phagocytes are the inflammatory cell type where P2X receptor expression has been best characterized [82]. Monocyte/macrophage and myeloid dendritic cells express P2X1, P2X4, and P2X7 receptors [45]. P2X5 receptors are expressed by T lymphocytes. The function of P2X5 receptors in inflammation is not clear. Neutrophils and eosinophils express P2X1, P2X4, and P2X7 receptors, although the level of expression is different in the quiescent or activated state [83–85]. P2X1, P2X4, and P2X7 receptors are expressed on T and B lymphocytes and natural killer cells [45]. ATP released by tissue damage, acts as a danger signal by acting on P2 receptors on immune cells to stimulate the immune response [86]. P2 receptors are present on immune cells and their expression is modulated by inflammatory cytokines [87]. P2X receptors have been implicated in the participation of the immune system in inflammatory pain [88, 89]. P2X1, P2X4, P2X7, and perhaps P2X3 receptors are expressed by mast cells [90, 91]. Mast cells were the cell type in which the properties of the P2X7 receptor were initially observed and characterized by Cockcroft and Gomperts [92]. P2X receptor expression is also present on microglia, both in vitro and in vivo, particularly P2X4 and P2X7 receptors [93, 94]. P2X receptors on mast cells are involved in the pathogenesis of chronic airway allergic inflammation [91].
Inflammatory pain
P2X7 receptors are involved in inflammatory pain [95–99]. There is reduced inflammation-induced hyperalgesia in rats following treatment with oxidized ATP, a P2X7 receptor antagonist [100]. P2X7 receptors play a transductional role in the development of inflammatory pain [101].
A review includes a discussion of the role of P2X3 receptors in inflammatory pain [102]. During the inflammatory process in peripheral tissue, neither prostaglandins nor sympathetic amines can sensitize primary afferent neurons by themselves; they depend on previous neuronal P2X3 receptor activation [103]. Spontaneous and evoked responses of spinal nociceptive neurons are attenuated by P2X3 receptor antagonism in inflamed rats [104]. Data has been presented to indicate that antagonism of spinal P2X3/P2X2/3 receptors regulates an indirect activation of the opioid system to alleviate inflammatory hyperalgesia [105]. P2X4 receptors probably also participate because of their involvement in neuropathic pain [106, 107], which is relevant for inflammation. Mice lacking P2X4 receptors show impaired inflammasome activation [40] and do not develop pain hypersensitivity in response to inflammatory agents, and this is paralleled by a complete absence of PGE2 in inflammatory exudates [30]. There is also a suggestion that P2X4 receptors might modulate P2X7 receptor activity [56]. P2X7 receptor antagonists reduce inflammatory pain in rats [100, 108–110]. Chronic inflammatory pain was abolished in P2X7 receptor knockout mice [95]. Central sensitization of nociceptive neurons in medullary dorsal horn of rats involves P2X7 receptors [111]. P2X7 receptor antagonism of chronic pain is likely mediated through immuno-neural interactions that affect the release of inflammatory cytokines [112]. Inflammatory pain involved in dressing changes of burn patients was relieved by puerarin, an isoflavonoid derived from a Chinese herb [113]. The effects were correlated with the decreased expression of P2X7 receptor mRNA and protein in peripheral blood mononuclear cells in burn patients.
Pathology and inflammation
Purinergic contributions to neuroinflammation in relation to disorders of the CNS are being explored. Pathological neuroinflammation, promoting apoptosis and necrosis, and influencing the synaptic and intrinsic membrane properties of neurons contributes to CNS pathologies [114]. A role for neuroinflammation occurs in neurodegenerative diseases, such as Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, amyotrophic lateral sclerosis, Huntington’s disease, stroke, and epilepsy [115]. Neuroinflammation is also a pathological factor in psychiatric mood disorders [116, 117]. The NLRP3 inflammasome is a central mediator of systemic inflammation and a link between psychological stress and the emergence of depression and other psychiatric illnesses [118] and ATP, accumulated following insult, induces NLRP-mediated IL-1β processing [93]. Epidemiological and gene-linking studies have implicated P2X7 in a host of CNS diseases [119, 120]. Neuroimmunological changes occur in psychiatric disorders, including major depressive disorder, bipolar disorder, obsessive compulsive disorder, and schizophrenia. Chronic inflammation associated with diabetes, obesity, or autoimmune diseases increases the risk of psychiatric disorders (see [47]). These disorders are characterized by chronic, low grade, or intermittent inflammation, in contrast to neurodegenerative diseases, where there is acute inflammation in the brain parenchyma. Schizophrenia is considered to be a neurodevelopmental disorder, and foetal neuroinflammation, resulting from maternal infection, is implicated [116]. Enhanced levels of pro-inflammatory cytokines in the brain and enhanced microglial activation occur in foetal neuroinflammation, leading to abnormal brain maturation.
Associations between susceptibility or resistance to parasites and bacteria and loss- or gain-of-function polymorphisms in the P2X7 receptor indicate that it is important in infectious disease [121]. ATP activation of the NLRP3 inflammasome protects mice against bacterial infection [122]. The P2X7 receptor plays a role in acute and chronic stages of infection as well as a ‘danger signal’ in the initial stages of inflammation (see [71]).
Therapeutic potential
Purinergic-based therapies may be useful to halt excessive inflammation and promote repair of neuroinflammatory disorders [4, 80, 123, 124].
P2X7 receptor antagonists are promising targets for anti-inflammatory therapy [125, 126], including inflammation in the CNS [11, 95, 100, 127, 128]. In view of its potent pro-inflammatory effect, the analgesic activity of P2X7 receptor blockers is of interest for therapeutic implications [99]. Blockade of P2X7 receptors reduced nociception in animal models of chronic inflammatory pain [96, 125, 129–132]. Relief of inflammatory pain was produced by the P2X7 receptor antagonist, oxidized ATP, in arthritic rats [11]. Blockade by the selective P2X7 receptor antagonist, A-839977, was lost in IL-1αβ knockout mice [133].
P2X3 receptor antagonists have also been suggested to be a therapeutic target for pain therapy [134]. Application of apyrase to CD39-deficient mice prior to ischaemia reduced infarct volumes and neutrophil counts [135, 136]. Kinase inhibitors have been recommended for the treatment of inflammatory and autoimmune disorders, such as rheumatoid arthritis, psoriasis, organ transplantation, and autoimmune diseases [137, 138].
Activation of the purinergic pathway may be implicated in transplantation-related injuries. Following transplantation, ATP, the pro-inflammatory danger signal, is released from damaged cells to promote proliferation of immune cells, T cell activation, and inflammation. Targeting purinoceptors may promote immunosuppression and reduce inflammation. The ectonucleotidases, CD39 and CD73, hydrolyze ATP to the anti-inflammatory mediator adenosine, which suppresses pro-inflammatory cytokine production leading to improved graft survival. The mechanisms of action of several immunosuppressive drugs, such as calcineurin and mTOR inhibitors, involve purinergic signalling. Targeting the purinergic signalling pathway by increasing ectonucleotidase activity and/or boosting short term adenosine-mediated immunosuppression have potential in preventing allograft vascular injury, ameliorating rejection, and promoting tolerance.
Conclusion
P2X receptors mediate the responses to ATP, one of the most ancient evolutionary extracellular messengers (see [139]). ATP is an intracellular molecule, so its release is suited to signal cell distress or injury. This ‘danger signal role’ of ATP became more and more relevant in multicellular animals. P2X receptors play important roles in pathophysiology (see [140, 141]) and P2X7 receptors, in particular, are vitally involved in inflammation.
References
Di Virgilio F, Ferrara N, Idzko M, Panther E, Norgauer J, La Sala A, Girolomoni G (2003) Extracellular ATP, receptors and inflammation. Drug Dev Res 59:171–174
Di Virgilio F, Boeynaems JM, Robson SC (2009) Extracellular nucleotides as negative modulators of immunity. Curr Opin Pharmacol 9:507–513
Bours MJ, Swennen EL, Di Virgilio F, Cronstein BN, Dagnelie PC (2006) Adenosine 5’-triphosphate and adenosine as endogenous signaling molecules in immunity and inflammation. Pharmacol Ther 112:358–404
Barberà-Cremades M, Baroja-Mazo A, Gomez AI, Machado F, Di Virgilio F, Pelegrín P (2012) P2X7 receptor-stimulation causes fever via PGE2 and IL-1β release. FASEB J 26:2951–2962
Fiebich BL, Akter S, Akundi RS (2014) The two-hit hypothesis for neuroinflammation: role of exogenous ATP in modulating inflammation in the brain. Front Cell Neurosci 8:260
De Man JG, Seerden TC, De Winter BY, Van Marck EA, Herman AG, Pelckmans PA (2003) Alteration of the purinergic modulation of enteric neurotransmission in the mouse ileum during chronic intestinal inflammation. Br J Pharmacol 139:172–184
Kurashima Y, Kiyono H, Kunisawa J (2015) Pathophysiological role of extracellular purinergic mediators in the control of intestinal inflammation. Mediators Inflamm 2015:427125
Riteau N, Gasse P, Fauconnier L, Gombault A, Couegnat M, Fick L, Kanellopoulos J, Quesniaux VF, Marchand-Adam S, Crestani B, Ryffel B, Couillin I (2010) Extracellular ATP is a danger signal activating P2X7 receptor in lung inflammation and fibrosis. Am J Respir Crit Care Med 182:774–783
Eltzschig HK, Sitkovsky MV, Robson SC (2012) Purinergic signaling during inflammation. N Engl J Med 367:2322–2333
Cauwels A, Rogge E, Vandendriessche B, Shiva S, Brouckaert P (2014) Extracellular ATP drives systemic inflammation, tissue damage and mortality. Cell Death Dis 5:e1102
Dell’Antonio G, Quattrini A, Dal Cin E, Fulgenzi A, Ferrero ME (2002) Antinociceptive effect of a new P2Z/P2X7 antagonist, oxidized ATP, in arthritic rats. Neurosci Lett 327:87–90
Gourine AV, Dale N, Gourine VN, Spyer KM (2004) Fever in systemic inflammation: roles of purines. Front Biosci 9:1011–1022
Kim IS, Rhee CS, Lee JH, Heo JH, Park J, Lee CH (2007) Effects of purinergic stimulation on ciliary beat frequency and chloride secretion in sinusitis. Laryngoscope 117:1677–1682
Jacob F, Pérez Novo C, Bachert C, Van CK (2013) Purinergic signaling in inflammatory cells: P2 receptor expression, functional effects, and modulation of inflammatory responses. Purinergic Signal 9:285–306
Streit WJ, Mrak RE, Griffin WS (2004) Microglia and neuroinflammation: a pathological perspective. J Neuroinflammation 1:14
Gendelman HE (2002) Neural immunity: friend or foe? J Neurovirol 8:474–479
Yamasaki R, Lu H, Butovsky O, Ohno N, Rietsch AM, Cialic R, Wu PM, Doykan CE, Lin J, Cotleur AC, Kidd G, Zorlu MM, Sun N, Hu W, Liu L, Lee JC, Taylor SE, Uehlein L, Dixon D, Gu J, Floruta CM, Zhu M, Charo IF, Weiner HL, Ransohoff RM (2014) Differential roles of microglia and monocytes in the inflamed central nervous system. J Exp Med 211:1533–1549
Xanthos DN, Sandkuhler J (2014) Neurogenic neuroinflammation: inflammatory CNS reactions in response to neuronal activity. Nat Rev Neurosci 15:43–53
Di Virgilio F (2007) Liaisons dangereuses: P2X7 and the inflammasome. Trends Pharmacol Sci 28:465–472
Lister MF, Sharkey J, Sawatzky DA, Hodgkiss JP, Davidson DJ, Rossi AG, Finlayson K (2007) The role of the purinergic P2X7 receptor in inflammation. J Inflamm (Lond) 4:5
Tschopp J, Schroder K (2010) NLRP3 inflammasome activation: the convergence of multiple signalling pathways on ROS production? Nat Rev Immunol 10:210–215
Yiangou Y, Facer P, Baecker PA, Ford AP, Knowles CH, Chan CL, Williams NS, Anand P (2001) ATP-gated ion channel P2X3 is increased in human inflammatory bowel disease. Neurogastroenterol Motil 13:365–369
Bodin P, Burnstock G (1998) Increased release of ATP from endothelial cells during acute inflammation. Inflamm Res 47:351–354
Hasko G, Linden J, Cronstein B, Pacher P (2008) Adenosine receptors: therapeutic aspects for inflammatory and immune diseases. Nat Rev Drug Discov 7:759–770
Rayah A, Kanellopoulos JM, Di Virgilio F (2012) P2 receptors and immunity. Microbes Infect 14:1254–1262
Pellegatti P, Raffaghello L, Bianchi G, Piccardi F, Pistoia V, Di Virgilio F (2008) Increased level of extracellular ATP at tumor sites: in vivo imaging with plasma membrane luciferase. PLoS One 3:e2599
Falzoni S, Donvito G, Di Virgilio F (2013) Detecting adenosine triphosphate in the pericellular space. Interface Focus 3:20120101
Chvatchko Y, Valera S, Aubry JP, Renno T, Buell G, Bonnefoy JY (1996) The involvement of an ATP-gated ion channel, P2X1, in thymocyte apoptosis. Immunity 5:275–283
Woehrle T, Yip L, Elkhal A, Sumi Y, Chen Y, Yao Y, Insel PA, Junger WG (2010) Pannexin-1 hemichannel-mediated ATP release together with P2X1 and P2X4 receptors regulate T-cell activation at the immune synapse. Blood 116:3475–3484
Ulmann L, Hirbec H, Rassendren F (2010) P2X4 receptors mediate PGE2 release by tissue-resident macrophages and initiate inflammatory pain. EMBO J 29:2290–2300
Chakraborty S, Kaushik DK, Gupta M, Basu A (2010) Inflammasome signaling at the heart of central nervous system pathology. J Neurosci Res 88:1615–1631
Apolloni S, Montilli C, Finocchi P, Amadio S (2009) Membrane compartments and purinergic signalling: P2X receptors in neurodegenerative and neuroinflammatory events. FEBS J 276:354–364
Martinon F, Burns K, Tschopp J (2002) The inflammasome: a molecular platform triggering activation of inflammatory caspases and processing of proIL-beta. Mol Cell 10:417–426
Bernier LP (2012) Purinergic regulation of inflammasome activation after central nervous system injury. J Gen Physiol 140:571–575
Weber FC, Esser PR, Müller T, Ganesan J, Pellegatti P, Simon MM, Zeiser R, Idzko M, Jakob T, Martin SF (2010) Lack of the purinergic receptor P2X7 results in resistance to contact hypersensitivity. J Exp Med 207:2609–2619
Wilhelm K, Ganesan J, Muller T, Durr C, Grimm M, Beilhack A, Krempl CD, Sorichter S, Gerlach UV, Juttner E, Zerweck A, Gartner F, Pellegatti P, Di Virgilio F, Ferrari D, Kambham N, Fisch P, Finke J, Idzko M, Zeiser R (2010) Graft-versus-host disease is enhanced by extracellular ATP activating P2X7R. Nat Med 16:1434–1438
Burnstock G (1999) Release of vasoactive substances from endothelial cells by shear stress and purinergic mechanosensory transduction. J Anat 194:335–342
Bodin P, Burnstock G (2001) Purinergic signalling: ATP release. Neurochem Res 26:959–969
Lee BH, Hwang DM, Palaniyar N, Grinstein S, Philpott DJ, Hu J (2012) Activation of P2X7 receptor by ATP plays an important role in regulating inflammatory responses during acute viral infection. PLoS One 7:e35812
de Rivero Vaccari JP, Bastien D, Yurcisin G, Pineau I, Dietrich WD, De Koninck Y, Keane RW, Lacroix S (2012) P2X4 receptors influence inflammasome activation after spinal cord injury. J Neurosci 32:3058–3066
Ali SR, Timmer AM, Bilgrami S, Park EJ, Eckmann L, Nizet V, Karin M (2011) Anthrax toxin induces macrophage death by p38 MAPK inhibition but leads to inflammasome activation via ATP leakage. Immunity 35:34–44
Neves AR, Castelo-Branco MT, Figliuolo VR, Bernardazzi C, Buongusto F, Yoshimoto A, Nanini HF, Coutinho CM, Carneiro AJ, Coutinho-Silva R, de Souza HS (2014) Overexpression of ATP-activated P2X7 receptors in the intestinal mucosa is implicated in the pathogenesis of Crohn’s disease. Inflamm Bowel Dis 20:444–457
Di Virgilio F, Falzoni S, Mutini C, Sanz JM, Chiozzi P (1998) Purinergic P2X7 receptor: a pivotal role in inflammation and immunomodulation. Drug Dev Res 45:207–213
Bours MJ, Dagnelie PC, Giuliani AL, Wesselius A, Di Virgilio F (2011) P2 receptors and extracellular ATP: a novel homeostatic pathway in inflammation. Front Biosci (Schol Ed) 3:1443–1456
Idzko M, Ferrari D, Eltzschig HK (2014) Nucleotide signalling during inflammation. Nature 509:310–317
Di Virgilio F (2015) P2X receptors and inflammation. Curr Med Chem 22:866–877
Beamer E, Gölöncsér F, Horváth G, Bekö K, Otrokocsi L, Koványi B, Sperlágh B (2015) Purinergic mechanisms in neuroinflammation: an update from molecules to behavior. Neuropharmacology In Press
Monif M, Reid CA, Powell KL, Smart ML, Williams DA (2009) The P2X7 receptor drives microglial activation and proliferation: a trophic role for P2X7R pore. J Neurosci 29:3781–3791
Solini A, Chiozzi P, Morelli A, Fellin R, Di Virgilio F (1999) Human primary fibroblasts in vitro express a purinergic P2X7 receptor coupled to ion fluxes, microvesicle formation and IL-6 release. J Cell Sci 112:297–305
Ferrari D, Pizzirani C, Adinolfi E, Lemoli RM, Curti A, Idzko M, Panther E, Di Virgilio F (2006) The P2X7 receptor: a key player in IL-1 processing and release. J Immunol 176:3877–3883
Perregaux DG, McNiff P, Laliberte R, Conklyn M, Gabel CA (2000) ATP acts as an agonist to promote stimulus-induced secretion of IL-1β and IL-18 in human blood. J Immunol 165:4615–4623
Mehta VB, Hart J, Wewers MD (2001) ATP-stimulated release of interleukin (IL)-1β and IL-18 requires priming by lipopolysaccharide and is independent of caspase-1 cleavage. J Biol Chem 276:3820–3826
Pelegrin P, Barroso-Gutierrez C, Surprenant A (2008) P2X7 receptor differentially couples to distinct release pathways for IL-1β in mouse macrophage. J Immunol 180:7147–7157
Yip L, Woehrle T, Corriden R, Hirsh M, Chen Y, Inoue Y, Ferrari V, Insel PA, Junger WG (2009) Autocrine regulation of T-cell activation by ATP release and P2X7 receptors. FASEB J 23:1685–1693
Newbolt A, Stoop R, Virginio C, Surprenant A, North RA, Buell G, Rassendren F (1998) Membrane topology of an ATP-gated ion channel (P2X receptor). J Biol Chem 273:15177–15182
Antonio LS, Stewart AP, Xu XJ, Varanda WA, Murrell-Lagnado RD, Edwardson JM (2011) P2X4 receptors interact with both P2X2 and P2X7 receptors in the form of homotrimers. Br J Pharmacol 163:1069–1077
Babelova A, Moreth K, Tsalastra-Greul W, Zeng-Brouwers J, Eickelberg O, Young MF, Bruckner P, Pfeilschifter J, Schaefer RM, Grone HJ, Schaefer L (2009) Biglycan, a danger signal that activates the NLRP3 inflammasome via toll-like and P2X receptors. J Biol Chem 284:24035–24048
Sakaki H, Tsukimoto M, Harada H, Moriyama Y, Kojima S (2013) Autocrine regulation of macrophage activation via exocytosis of ATP and activation of P2Y11 receptor. PLoS One 8:e59778
Rossi C, Santini E, Chiarugi M, Salvati A, Comassi M, Vitolo E, Madec S, Solini A (2014) The complex P2X7 receptor/inflammasome in perivascular fat tissue of heavy smokers. Eur J Clin Invest 44:295–302
Choi HB, Ryu JK, Kim SU, McLarnon JG (2007) Modulation of the purinergic P2X7 receptor attenuates lipopolysaccharide-mediated microglial activation and neuronal damage in inflamed brain. J Neurosci 27:4957–4968
Matute C, Torre I, Pérez-Cerdá F, Pérez-Samartín A, Alberdi E, Etxebarria E, Arranz AM, Ravid R, Rodríguez-Antiguedad A, Sánchez-Gómez M, Domercq M (2007) P2X7 receptor blockade prevents ATP excitotoxicity in oligodendrocytes and ameliorates experimental autoimmune encephalomyelitis. J Neurosci 27:9525–9533
Skaper SD, Debetto P, Giusti P (2010) The P2X7 purinergic receptor: from physiology to neurological disorders. FASEB J 24:337–345
Weisman GA, Camden JM, Peterson TS, Ajit D, Woods LT, Erb L (2012) P2 receptors for extracellular nucleotides in the central nervous system: role of P2X7 and P2Y2 receptor interactions in neuroinflammation. Mol Neurobiol 46:96–113
Solle M, Labasi J, Perregaux DG, Stam E, Petrushova N, Koller BH, Griffiths RJ, Gabel CA (2001) Altered cytokine production in mice lacking P2X7 receptors. J Biol Chem 276:125–132
Labasi JM, Petrushova N, Donovan C, McCurdy S, Lira P, Payette MM, Brissette W, Wicks JR, Audoly L, Gabel CA (2002) Absence of the P2X7 receptor alters leukocyte function and attenuates an inflammatory response. J Immunol 168:6436–6445
Rizzo R, Ferrari D, Melchiorri L, Stignani M, Gulinelli S, Baricordi OR, Di Virgilio F (2009) Extracellular ATP acting at the P2X7 receptor inhibits secretion of soluble HLA-G from human monocytes. J Immunol 183:4302–4311
Rizzo R, Bortolotti D, Bolzani S, Fainardi E (2014) HLA-G molecules in autoimmune diseases and infections. Front Immunol 5:592
Adinolfi E, Raffaghello L, Giuliani AL, Cavazzini L, Capece M, Chiozzi P, Bianchi G, Kroemer G, Pistoia V, Di Virgilio F (2012) Expression of P2X7 receptor increases in vivo tumor growth. Cancer Res 72:2957–2969
Ferrari D, Chiozzi P, Falzoni S, dal Susino M, Melchiorri L, Baricordi OR, Di Virgilio F (1997) Extracellular ATP triggers IL-1β release by activating the purinergic P2Z receptor of human macrophages. J Immunol 159:1451–1458
Ferrari D, Stroh C, Schulze-Osthoff K (1999) P2X7/P2Z purinoreceptor-mediated activation of transcription factor NFAT in microglial cells. J Biol Chem 274:13205–13210
Morandini AC, Savio LE, Coutinho-Silva R (2014) The role of P2X7 receptor in infectious inflammatory diseases and the influence of ectonucleotidases. Biomed J 37:169–177
Janssen B, Vugts DJ, Funke U, Spaans A, Schuit RC, Kooijman E, Rongen M, Perk LR, Lammertsma AA, Windhorst AD (2014) Synthesis and initial preclinical evaluation of the P2X7 receptor antagonist [11C]A-740003 as a novel tracer of neuroinflammation. J Labelled Comp Radiopharm 57:509–516
Lopez-Castejon G, Pelegrin P (2012) Current status of inflammasome blockers as anti-inflammatory drugs. Expert Opin Investig Drugs 21:995–1007
North RA (2002) Molecular physiology of P2X receptors. Physiol Rev 82:1013–1067
Caseley EA, Muench SP, Roger S, Mao HJ, Baldwin SA, Jiang LH (2014) Non-synonymous single nucleotide polymorphisms in the P2X receptor genes: association with diseases, impact on receptor functions and potential use as diagnosis biomarkers. Int J Mol Sci 15:13344–13371
Haag F, Adriouch S, Brass A, Jung C, Möller S, Scheuplein F, Bannas P, Seman M, Koch-Nolte F (2007) Extracellular NAD and ATP: partners in immune cell modulation. Purinergic Signal 3:71–81
Myrtek D, Idzko M (2007) Chemotactic activity of extracellular nucleotideson human immune cells. Purinergic Signal 3:5–11
Martinon F (2008) Detection of immune danger signals by NALP3. J Leukoc Biol 83:507–511
Wewers MD, Sarkar A (2009) P2X7 receptor and macrophage function. Purinergic Signal 5:189–195
Ferrero ME (2011) Purinoceptors in inflammation: potential as anti-inflammatory therapeutic targets. Front Biosci (Landmark Ed) 16:2172–2186
Junger WG (2011) Immune cell regulation by autocrine purinergic signalling. Nat Rev Immunol 11:201–212
Di Virgilio F, Chiozzi P, Ferrari D, Falzoni S, Sanz JM, Morelli A, Torboli M, Bolognesi G, Baricordi OR (2001) Nucleotide receptors: an emerging family of regulatory molecules in blood cells. Blood 97:587–600
Koshi R, Coutinho-Silva R, Cascabulho CM, Henrique-Pons A, Knight GE, Loesch A, Burnstock G (2005) Presence of the P2X7 purinergic receptor on immune cells that invade the rat endometrium during oestrus. J Reprod Immunol 66:127–140
Ferrari D, Idzko M, Dichmann S, Purlis D, Virchow C, Norgauer J, Chiozzi P, Di Virgilio F, Luttmann W (2000) P2 purinergic receptors of human eosinophils: characterization and coupling to oxygen radical production. FEBS Lett 486:217–224
Lucattelli M, Cicko S, Muller T, Lommatzsch M, De Cunto G, Cardini S, Sundas W, Grimm M, Zeiser R, Durk T, Zissel G, Sorichter S, Ferrari D, Di Virgilio F, Virchow JC, Lungarella G, Idzko M (2011) P2X7 receptor signaling in the pathogenesis of smoke-induced lung inflammation and emphysema. Am J Respir Cell Mol Biol 44:423–429
Vitiello L, Gorini S, Rosano G, La Sala A (2012) Immunoregulation through extracellular nucleotides. Blood 120:511–518
Di Virgilio F, Ferrari D, Chiozzi P, Falzoni S, Sanz JM, dal Susino M, Mutini C, Hanau S, Baricordi OR (1996) Purinoceptor function in the immune system. Drug Dev Res 39:319–329
Marchand F, Perretti M, McMahon SB (2005) Role of the immune system in chronic pain. Nat Rev Neurosci 6:521–532
Moalem G, Tracey DJ (2006) Immune and inflammatory mechanisms in neuropathic pain. Brain Res Rev 51:240–264
Wareham K, Vial C, Wykes RC, Bradding P, Seward EP (2009) Functional evidence for the expression of P2X1, P2X4 and P2X7 receptors in human lung mast cells. Br J Pharmacol 157:1215–1224
Bulanova E, Bulfone-Paus S (2010) P2 receptor-mediated signaling in mast cell biology. Purinergic Signal 6:3–17
Cockcroft S, Gomperts BD (1980) The ATP4- receptor of rat mast cells. Biochem J 188:789–798
Burnstock G (2008) Purinergic signalling and disorders of the central nervous system. Nat Rev Drug Disc 7:575–590
Inoue K (2008) Purinergic systems in microglia. Cell Mol Life Sci 65:3074–3080
Chessell IP, Hatcher JP, Bountra C, Michel AD, Hughes JP, Green P, Egerton J, Murfin M, Richardson J, Peck WL, Grahames CB, Casula MA, Yiangou Y, Birch R, Anand P, Buell GN (2005) Disruption of the P2X7 purinoceptor gene abolishes chronic inflammatory and neuropathic pain. Pain 114:386–396
Hughes JP, Hatcher JP, Chessell IP (2007) The role of P2X7 in pain and inflammation. Purinergic Signal 3:163–169
Chu YX, Zhang Y, Zhang YQ, Zhao ZQ (2010) Involvement of microglial P2X7 receptors and downstream signaling pathways in long-term potentiation of spinal nociceptive responses. Brain Behav Immun 24:1176–1189
Alves LA, Bezerra RJ, Faria RX, Ferreira LG, da Silva FV (2013) Physiological roles and potential therapeutic applications of the P2X7 receptor in inflammation and pain. Molecules 18:10953–10972
Burnstock G (2013) Purinergic mechanisms and pain—an update. Eur J Pharmacol 716:24–40
Dell’Antonio G, Quattrini A, Cin ED, Fulgenzi A, Ferrero ME (2002) Relief of inflammatory pain in rats by local use of the selective P2X7 ATP receptor inhibitor, oxidized ATP. Arthritis Rheum 46:3378–3385
Clark AK, Staniland AA, Marchand F, Kaan TK, McMahon SB, Malcangio M (2010) P2X7-dependent release of interleukin-1β and nociception in the spinal cord following lipopolysaccharide. J Neurosci 30:573–582
Wirkner K, Sperlágh B, Illes P (2007) P2X3 receptor involvement in pain states. Mol Neurobiol 36:165–183
Prado FC, Araldi D, Vieira AS, Oliveira-Fusaro MC, Tambeli CH, Parada CA (2013) Neuronal P2X3 receptor activation is essential to the hyperalgesia induced by prostaglandins and sympathomimetic amines released during inflammation. Neuropharmacology 67:252–258
Xu J, Chu KL, Brederson JD, Jarvis MF, McGaraughty S (2012) Spontaneous firing and evoked responses of spinal nociceptive neurons are attenuated by blockade of P2X3 and P2X2/3 receptors in inflamed rats. J Neurosci Res 90:1597–1606
McGaraughty S, Honore P, Wismer CT, Mikusa J, Zhu CZ, McDonald HA, Bianchi B, Faltynek CR, Jarvis MF (2005) Endogenous opioid mechanisms partially mediate P2X3/P2X2/3-related antinociception in rat models of inflammatory and chemogenic pain but not neuropathic pain. Br J Pharmacol 146:180–188
Tsuda M, Shigemoto-Mogami Y, Koizumi S, Mizokoshi A, Kohsaka S, Salter MW, Inoue K (2003) P2X4 receptors induced in spinal microglia gate tactile allodynia after nerve injury. Nature 424:778–783
Beggs S, Trang T, Salter MW (2012) P2X4R+ microglia drive neuropathic pain. Nat Neurosci 15:1068–1073
Honore P, Donnelly-Roberts D, Namovic MT, Hsieh G, Zhu CZ, Mikusa JP, Hernandez G, Zhong C, Gauvin DM, Chandran P, Harris R, Medrano AP, Carroll W, Marsh K, Sullivan JP, Faltynek CR, Jarvis MF (2006) A-740003 [N-(1-{[(cyanoimino)(5-quinolinylamino) methyl]amino}-2,2-dimethylpropyl)-2-(3,4-dimethoxyphenyl)acetamide], a novel and selective P2X7 receptor antagonist, dose-dependently reduces neuropathic pain in the rat. J Pharmacol Exp Ther 319:1376–1385
King BF (2007) Novel P2X7 receptor antagonists ease the pain. Br J Pharmacol 151:565–567
Teixeira JM, Oliveira MC, Parada CA, Tambeli CH (2010) Peripheral mechanisms underlying the essential role of P2X7 receptors in the development of inflammatory hyperalgesia. Eur J Pharmacol 644:55–60
Itoh K, Chiang CY, Li Z, Lee JC, Dostrovsky JO, Sessle BJ (2011) Central sensitization of nociceptive neurons in rat medullary dorsal horn involves purinergic P2X7 receptors. Neuroscience 192:721–731
McGaraughty S, Chu KL, Namovic MT, Donnelly-Roberts DL, Harris RR, Zhang XF, Shieh CC, Wismer CT, Zhu CZ, Gauvin DM, Fabiyi AC, Honore P, Gregg RJ, Kort ME, Nelson DW, Carroll WA, Marsh K, Faltynek CR, Jarvis MF (2007) P2X7-related modulation of pathological nociception in rats. Neuroscience 146:1817–1828
Zhang J, Li X, Gao Y, Guo G, Xu C, Li G, Liu S, Huang A, Tu G, Peng H, Qiu S, Fan B, Zhu Q, Yu S, Zheng C, Liang S (2013) Effects of puerarin on the inflammatory role of burn-related procedural pain mediated by P2X7 receptors. Burns 39:610–618
Yirmiya R, Goshen I (2011) Immune modulation of learning, memory, neural plasticity and neurogenesis. Brain Behav Immun 25:181–213
Frank-Cannon TC, Alto LT, McAlpine FE, Tansey MG (2009) Does neuroinflammation fan the flame in neurodegenerative diseases? Mol Neurodegener 4:47
Meyer U (2013) Developmental neuroinflammation and schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 42:20–34
Najjar S, Pearlman DM, Alper K, Najjar A, Devinsky O (2013) Neuroinflammation and psychiatric illness. J Neuroinflammation 10:43
Iwata M, Ota KT, Duman RS (2013) The inflammasome: pathways linking psychological stress, depression, and systemic illnesses. Brain Behav Immun 31:105–114
Hansen T, Jakobsen KD, Fenger M, Nielsen J, Krane K, Fink-Jensen A, Lublin H, Ullum H, Timm S, Wang AG, Jorgensen NR, Werge T (2008) Variation in the purinergic P2RX7 receptor gene and schizophrenia. Schizophr Res 104:146–152
Ursu D, Ebert P, Langron E, Ruble C, Munsie L, Zou W, Fijal B, Qian YW, McNearney TA, Mogg A, Grubisha O, Merchant K, Sher E (2014) Gain and loss of function of P2X7 receptors: mechanisms, pharmacology and relevance to diabetic neuropathic pain. Mol Pain 10:37
Miller CM, Boulter NR, Fuller SJ, Zakrzewski AM, Lees MP, Saunders BM, Wiley JS, Smith NC (2011) The role of the P2X7 receptor in infectious diseases. PLoS Pathog 7:e1002212
Xiang Y, Wang X, Yan C, Gao Q, Li SA, Liu J, Zhou K, Guo X, Lee W, Zhang Y (2013) Adenosine-5’-triphosphate (ATP) protects mice against bacterial infection by activation of the NLRP3 inflammasome. PLoS One 8:e63759
Fumagalli M, Lecca D, Abbracchio MP (2011) Role of purinergic signalling in neuro-immune cells and adult neural progenitors. Front Biosci (Landmark Ed) 16:2326–2341
Ochoa-Cortes F, Liñán-Rico A, Jacobson KA, Christofi FL (2014) Potential for developing purinergic drugs for gastrointestinal diseases. Inflamm Bowel Dis 20:1259–1287
Sorge RE, Trang T, Dorfman R, Smith SB, Beggs S, Ritchie J, Austin JS, Zaykin DV, Vander MH, Costigan M, Herbert TA, Yarkoni-Abitbul M, Tichauer D, Livneh J, Gershon E, Zheng M, Tan K, John SL, Slade GD, Jordan J, Woolf CJ, Peltz G, Maixner W, Diatchenko L, Seltzer Z, Salter MW, Mogil JS (2012) Genetically determined P2X7 receptor pore formation regulates variability in chronic pain sensitivity. Nat Med 18:595–599
Mehta N, Kaur M, Singh M, Chand S, Vyas B, Silakari P, Bahia MS, Silakari O (2014) Purinergic receptor P2X7: a novel target for anti-inflammatory therapy. Bioorg Med Chem 22:54–88
Friedle SA, Curet MA, Watters JJ (2010) Recent patents on novel P2X7 receptor antagonists and their potential for reducing central nervous system inflammation. Recent Pat CNS Drug Discov 5:35–45
Takenouchi T, Sekiyama K, Sekigawa A, Fujita M, Waragai M, Sugama S, Iwamaru Y, Kitani H, Hashimoto M (2010) P2X7 receptor signaling pathway as a therapeutic target for neurodegenerative diseases. Arch Immunol Ther Exp (Warsz ) 58:91–96
Donnelly-Roberts DL, Jarvis MF (2007) Discovery of P2X7 receptor-selective antagonists offers new insights into P2X7 receptor function and indicates a role in chronic pain states. Br J Pharmacol 151:571–579
Donnelly-Roberts D, McGaraughty S, Shieh CC, Honore P, Jarvis MF (2008) Painful purinergic receptors. J Pharmacol Exp Ther 324:409–415
Carroll WA, Donnelly-Roberts D, Jarvis MF (2009) Selective P2X7 receptor antagonists for chronic inflammation and pain. Purinergic Signal 5:63–73
Brumfield S, Matasi JJ, Tulshian D, Czarniecki M, Greenlee W, Garlisi C, Qiu H, Devito K, Chen SC, Sun Y, Bertorelli R, Ansell J, Geiss W, Le VD, Martin GS, Vellekoop SA, Haber J, Allard ML (2011) Synthesis and SAR development of novel P2X7 receptor antagonists for the treatment of pain: part 2. Bioorg Med Chem Lett 21:7287–7290
Honore P, Donnelly-Roberts D, Namovic M, Zhong C, Wade C, Chandran P, Zhu C, Carroll W, Perez-Medrano A, Iwakura Y, Jarvis MF (2009) The antihyperalgesic activity of a selective P2X7 receptor antagonist, A-839977, is lost in IL-1αβ knockout mice. Behav Brain Res 204:77–81
Wang C, Gu Y, Li GW, Huang LY (2007) A critical role of the cAMP sensor Epac in switching protein kinase signalling in prostaglandin E2-induced potentiation of P2X3 receptor currents in inflamed rats. J Physiol 584:191–203
Hyman MC, Petrovic-Djergovic D, Visovatti SH, Liao H, Yanamadala S, Bouïs D, Su EJ, Lawrence DA, Broekman MJ, Marcus AJ, Pinsky DJ (2009) Self-regulation of inflammatory cell trafficking in mice by the leukocyte surface apyrase CD39. J Clin Invest 119:1136–1149
Rhett JM, Fann SA, Yost MJ (2014) Purinergic signaling in early inflammatory events of the foreign body response: modulating extracellular ATP as an enabling technology for engineered implants and tissues. Tissue Eng Part B Rev 20:392–402
Bhagwat SS (2007) MAP kinase inhibitors in inflammation and autoimmune disorders. In: Macor JE (ed) Annual Reports in Medicinal Chemistry, Volume 42. Academic Press, Amsterdam, pp 265–278
Bhagwat SS (2009) Kinase inhibitors for the treatment of inflammatory and autoimmune disorders. Purinergic Signal 5:107–115
Burnstock G, Verkhratsky A (2009) Evolutionary origins of the purinergic signalling system. Acta Physiologica 195:415–447
Burnstock G (2006) Pathophysiology and therapeutic potential of purinergic signaling. Pharmacol Rev 58:58–86
Burnstock G (2007) Physiology and pathophysiology of purinergic neurotransmission. Physiol Rev 87:659–797
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burnstock, G. P2X ion channel receptors and inflammation. Purinergic Signalling 12, 59–67 (2016). https://doi.org/10.1007/s11302-015-9493-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-015-9493-0