Abstract
Purpose
Few studies exist comparing the effect of different lower urinary tract dysfunctions (LUTDs) on anti-incontinence surgery. This study investigates the long-term therapeutic outcome of a suburethral sling procedure among women with stress urinary incontinence (SUI) and different LUTDs.
Methods
This study retrospectively reviewed 401 women treated with a suburethral sling for SUI. Following baseline videourodynamic findings, the patients were divided into pure SUI or SUI with concomitant LUTD (mixed detrusor overactivity and SUI, low detrusor contractility and SUI, and presence of bladder outlet obstruction and SUI) groups. The primary endpoint was the SUI-free-specific survival rate. A successful outcome was defined as the absence of any SUI event. The secondary endpoints included postoperative complications, surgical revision rate, and changes in videourodynamic parameters.
Results
At a mean follow-up of 5.1 (standard deviation: 5.4, range 0.1–24.1) years, the median cumulative duration of SUI-free survival was 15.4 years and 15.9 years in the pure SUI and SUI and concomitant LUTD subgroup, respectively, without significant difference between the groups. No between-group difference in postoperative complications was also noted. The cumulative incidences of the overall reoperation rate were 15.3%, 11.6%, 30.9%, and 7.3% in the pure SUI, detrusor overactivity, low detrusor contractility, and bladder outlet obstruction subgroups, respectively, with a significant difference between the groups (p = 0.006).
Conclusions
Women who underwent suburethral sling surgery for SUI treatment had comparable long-term success rates regardless of baseline LUTD. However, those with low detrusor contractility may experience less favorable results in terms of higher reoperation rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) is characterized by an inadvertent loss of urine that occurs when the intra-abdominal pressure increases, overcoming the urethral sphincter pressure. SUI negatively impacts social and working life and is associated with poor mental health [1].
The initial SUI treatment should be conservative, which includes weight loss, urinary containment, pelvic floor muscle training, vaginal estrogen therapy, duloxetine, and pulsed electromagnetic field stimulation [2, 3]. In cases that have failed nonsurgical management, surgical interventions, including bulking procedures, suburethral sling, autologous fascial pubovaginal sling, and colposuspension, may be considered [4]. Among the surgical options, suburethral sling had been considered the first-line option for SUI treatment based on its efficacy until July 2018 when National Health Service England announced the halt of its use due to growing concerns regarding mesh-related problems [5].
Patients with SUI can be classified as complicated based on the presentation of previous surgery for SUI, history of pelvic surgery or radiotherapy, presence of genitourinary prolapse, presence of voiding symptoms, and presence of neurogenic lower urinary tract dysfunction (LUTD). On the contrary, patients who do not fulfill the criteria for the complicated designation are classified as having uncomplicated SUI [2, 6]. Compared with pure SUI, patients with detrusor dysfunction or bladder outlet obstruction tend to show poorer treatment results [7,8,9]. Accordingly, urodynamic testing is often performed before surgical treatment of SUI in women suggested to have complicated SUI or in whom the subtype is unclear [10].
However, few studies have compared the long-term therapeutic effect of different LUTDs on anti-incontinence surgery. Therefore, this study aimed to investigate the treatment outcome of a suburethral sling procedure by dividing prognostic factors based on the presence of associated LUTD in women with SUI after a long-term follow-up.
Materials and methods
Patient enrollment and selection
This study was approved by the Institutional Review Board (IRB) and Ethics Committee of the Buddhist Tzu Chi General Hospital, Hualien, Taiwan (IRB: 109-005-B). Informed consent was waived because of the retrospective nature of this study. Consecutive women who had undergone a suburethral sling procedure for stress-predominant urinary incontinence at the Buddhist Tzu Chi General Hospital, Hualien, from September 1997 to March 2019, were recruited. All baseline characteristics, preoperative videourodynamic study (VUDS) parameters, operative reports, and postoperative clinical manifestations and complications were reviewed carefully through the electronic medical records.
To compare the long-term treatment outcomes and durability of suburethral sling procedures in different LUTDs, patients who did not receive preoperative VUDS and who had no return visit data from the analyses were excluded. To avoid confounding variables, patients who were proven to have pelvic organ prolapse and had received concomitant repair surgeries were also excluded. Otherwise, no other exclusion criteria were set to avoid selection bias and more closely mimic a real-world setting.
Suburethral sling procedure
All retropubic suburethral sling procedures in this study were performed by a single surgeon (Kuo HC) using a standardized procedure under spinal anesthesia. Briefly, a 2-cm-wide self-fashioned polypropylene mesh was placed below the mid-urethra through a subcutaneous tunnel at about the middle portion of the urethra of the anterior vaginal wall. The bilateral ends of the mesh were further pulled through the retropubic space up to the bilateral lower abdominal incision wounds, and the exact sling position and tension were adjusted following preoperative VUDS findings [11]. This technique has been used by the authors for over two decades, and the results were proven to be satisfactory and comparable with the commonly used commercial slings [12].
VUDS for LUTD
All of the selected patients had undergone VUDS and abdominal leak point pressure (ALPP) measurements before the surgery. Most of them were encouraged to receive repeat examinations to evaluate their voiding condition after the sling operation, at intervals of 3–6 months. All descriptions, terminology, and the practice of VUDS were performed following the standard procedure and the recommendations of the International Continence Society [13].
The urodynamic parameters recorded during the VUDS included ALPP, cystometric bladder capacity, maximum flow rate (Qmax), voided volume (Vol), postvoid residual volume, and detrusor pressure at Qmax (Pdet.Qmax). The female Bladder Outlet Obstruction Index (BOOIf; defined as Pdet.Qmax–2.2 × Qmax) [14], corrected Qmax (cQmax; defined as Qmax/Vol1/2), and voiding efficiency (defined as voided volume divided by cystometric bladder capacity) were calculated from the measured parameters.
Detrusor overactivity (DO) is characterized as involuntary detrusor contractions during the filling phase, whereas detrusor underactivity (DU) is defined as a reduction in strength and/or duration of contraction that results in prolonged and/or incomplete bladder emptying within a normal period [13]. Detrusor hyperactivity with impaired contractile function is defined as involuntary detrusor contraction during the filling phase, with low detrusor contractility in the voiding phase and a voiding efficiency of < 50% [15]. Bladder outlet obstruction is the presence of sustained detrusor contraction and radiographic evidence of obstruction at the bladder neck as bladder neck dysfunction and at the urethra as dysfunctional voiding [16, 17].
Patient grouping
The enrolled patients were categorized into subgroups based on their preoperative VUDS findings into the pure SUI (with a stable bladder), SUI and concomitant LUTD groups. Women who had concomitant LUTD were further divided into three subgroups: (1) mixed urodynamic DO and SUI; (2) low detrusor contractility, including detrusor hyperactivity with impaired contractile function, DU, and SUI; and (3) presence of bladder outlet obstruction, such as bladder neck dysfunction, dysfunctional voiding, and SUI (Fig. 1).
Outcome measurements
The primary endpoint of this study was SUI-free survival. A successful outcome was defined as the absence of any stress-specific urinary incontinence event assessed by both subjective and objective reports during the patients’ return visits. In contrast, an unsuccessful outcome was defined as the documentation of any SUI event. Secondary endpoints included patient-reported outcomes (e.g., postoperative complications), surgeon-reported outcomes (e.g., surgical revision type, reason, and rate), and changes in VUDS parameters. The prediction factors for successful treatment outcomes were also evaluated.
Statistical analysis
Continuous variables were expressed as means with standard deviations (SDs) and medians with interquartile range; categorical variables were presented as frequency (percentage). The analysis of variance was used to compare the between-group differences in continuous variables and the Chi-square test for categorical between-group differences. A post hoc analysis of variables was also performed among the different subgroups. Survival analysis was estimated using the Kaplan–Meier curve, and between-group differences in survival were discriminated using the log-rank test. Univariable and multivariable logistic regression models were used to predict factors associated with successful outcomes. For all analyses, two-sided p-values of < 0.05 were considered to be statistically significant. Data analyses were performed using SPSS version 25.0 (IBM Corp., Armonk, NY, USA).
Results
Baseline demographics
This analysis retrieved 401 women who received a suburethral sling procedure from September 1997 to March 2019. The mean patient age was 60.1 (SD: 11.7; range 20–89) years old, and the mean duration of follow-up was 5.1 (SD: 5.4; range 0.1–24.1) years. According to the preoperative VUDS findings, pure SUI was diagnosed in 236 (58.9%) patients and SUI and concomitant LUTD was diagnosed in 165 (41.1%) patients. Among patients with SUI and concomitant LUTD, 69 (17.2%), 55 (13.7%), and 41 (10.2%) had DO, low detrusor contractility, and bladder outlet obstruction, respectively (Fig. 1). Supplementary Table S1 summarizes the baseline demographics and clinical characteristics of the study groups, including age, body mass index, parity, vaginal delivery, operation history for hysterectomy, and menopausal status.
SUI-free survival
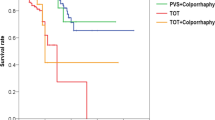
The median cumulative duration of SUI-free survival was 15.4 [interquartile range (IQR), 11.4–19.4] years in the pure SUI subgroup and 15.9 (IQR, 4.4–could not be estimated) years in the SUI and concomitant LUTD subgroups, respectively. No significant difference in the survival rate was found between the pure SUI and the SUI and concomitant SUI subgroups (p = 0.372; Fig. 2a). The consecutive survival rates at 3, 6, 9, 12, 15, 18, 21, and 24 years are listed in Fig. 2a, and no significant differences in any of the time points were also noted. On subgroup analysis, the survival rates among the subgroups of stable bladder, DO, low detrusor contractility, or bladder outlet obstruction were also not significant (p = 0.553; Fig. 2b).
Kaplan–Meier plot of stress urinary incontinence-free survival after suburethral sling procedures. A In the pure SUI and SUI and concomitant LUTD subgroups; B subgroup analysis by lower urinary tract function. LUTD, lower urinary tract dysfunction; NE, could not be estimated; NR, not reached; SUI, stress urinary incontinence
Patient-reported outcomes: postoperative complications
Table 1 lists the postoperative complications of the studied patients, and the distribution between de novo lower urinary tract symptoms (LUTS) and non-LUTS was not statistically significant (p = 0.604). Most complications comprise de novo urgency in LUTS and surgical wound pain in non-LUTS. Most (77.4%) cases were treated with oral medication at outpatient clinics. After adjusting these complications using the Clavien–Dindo system, the between-group difference was not statistically significant (p = 0.920).
Surgeon-reported outcomes: reoperation type, reason, and rate
The cumulative overall incidence rates of reoperation were 15.3%, 11.6%, 30.9%, and 7.3% in the stable bladder, DO, low detrusor contractility, and bladder outlet obstruction subgroups, respectively, with a significant difference between the groups (p = 0.006; Table 1). Post hoc analysis showed a significantly higher rate of any reoperation in the low detrusor contractility subgroup compared with the other groups, including stable bladder, DO, and bladder outlet obstruction subgroups (p-values were 0.007, 0.008, and 0.005, respectively). Among the entire study population, the reoperation rate for repeat suburethral sling for recurrent SUI was 7.7% at a mean of 8.8 years after the initial surgery. Likewise, a significantly greater proportion of patients in the low detrusor contractility subgroup received repeat suburethral sling procedures as compared with the stable bladder and DO subgroups (p-values were 0.013 and 0.030, respectively), but the difference was not statistically significant when compared with the bladder outlet obstruction subgroup (p = 0.051).
Surgeon-reported outcomes: changes in urodynamic parameters
Table 2 shows the urodynamic parameters at baseline and after suburethral sling surgery as well as the changes between the two time points in the current cohort disaggregated by these four SUI subgroups. Women with a stable bladder exhibited significant changes in all parameters postoperatively, although the similar results were not observed in the other subgroups. ALPP increased after the suburethral sling procedure in all SUI subgroups but showed no significant between-group difference. A significantly mild decrease in voiding efficiency was noted in the pure SUI and DO subgroups, but the other subgroups showed no change. Compared with patients with DO and bladder outlet obstruction, those with a stable bladder and low detrusor contractility had a significantly increased postoperative Pdet.Qmax (p-values were 0.003 and 0.007, respectively). The postoperative BOOIf was significantly higher in patients with a stable bladder and low detrusor contractility (p < 0.001 and p = 0.042, respectively) when compared with baseline. In addition, the changes of BOOIf in women with a stable bladder were significantly greater in women with bladder outlet obstruction (p = 0.018) on post hoc analysis.
Prediction of long-term SUI-free survival
Univariable and multivariable logistic regression models were performed to evaluate the association between the potential confounding variables and SUI-free survival after suburethral sling procedures (Supplementary Table S2). Although a correlation between postvoid residual volume and treatment outcome was suggested in the univariable logistic regression analysis (p = 0.037), the multivariable models demonstrated that Pdet.Qmax was the only significant independent factor for the SUI-specified result (p = 0.038). A greater baseline ALPP and the presence of different LUTDs failed to predict the treatment outcome. Otherwise, no statistically significant interactions were found between each of the covariates and SUI-free survival.
Discussion
It is believed that this is the first comparative study to comprehensively demonstrate the difference in long-term therapeutic outcomes of the suburethral sling between women with pure SUI, detrusor dysfunction and SUI, and bladder outlet obstruction and SUI. The results of the present study revealed no significant difference in continent-specific survival between women with SUI with or without concomitant LUTD after a long-term follow-up period. In addition, no significant difference was found in postoperative complications. However, women with SUI and low detrusor contractility showed poorer suburethral sling outcomes in terms of higher overall reoperation rate and reoperation for recurrent SUI when compared with the other subgroups.
Early in 2007, women with DU were found to have a significantly higher SUI recurrence rate than women with DO and normal detrusor function after suburethral sling surgery [8]. However, later in 2018, no significant difference in the rate of continence among these subgroups was reported during long-term follow-up [18]. This may be because of the improvements made in the surgical technique to handle the difficulty in balancing the tension between adequate urethral suspension and the ability to void after surgery, especially in patients with inadequate detrusor contractility. In addition, Franca et al. [17] found no significant difference in both the subjective or objective continence rates in women with undercontractility bladder and normal contractility bladder after suburethral sling surgery. However, both de novo voiding dysfunction and the reoperation rate for treating bladder outlet obstruction were higher in the undercontractility subgroup than in the normal contractility subgroup [19]. The results herein were consistent with a previous study in 2019 [16] and also agree with the report by Franca et al. [17] in that no significant difference in the long-term continence rate was found between women with low bladder contractility and the other subgroups. Moreover, women with low detrusor contractility had the least favorable surgical outcomes in terms of the long-term reoperation rate.
The role of urodynamics in the evaluation of SUI before anti-incontinence surgery has been long debated because office evaluation is noninferior to urodynamic testing before surgery in women with uncomplicated stress-predominant urinary incontinence [20]. Although some evidence in relevant literature reports has shown no better outcomes, urodynamic tests were found to change clinical decision-making [21]. The urodynamic results were found to be valuable for modifying therapeutic strategies and assisting in the selection of the optimum sling tension and position in patients with complicated SUI [11]. To achieve better anti-incontinence results and ensure we do not overlook potential complicated SUI patient, we encourage most of our patients to undergo VUDS before the surgery. This may be one of the possible reasons for the comparable SUI-free outcomes between women with pure SUI and those with SUI and concomitant LUTDs.
De novo overactive bladder (OAB), including both dry and wet, remain the two most common postoperative complications in each group, ranging from 17.1 to 24.6% in the bladder outlet obstruction and stable bladder group, respectively, regardless of the lower urinary tract (LUT) function in the current study. In a review of the literature, the incidence of de novo OAB ranged from 5 to 22% and was believed to be one of the most troublesome complications after anti-incontinence surgery for SUI [22]. Possible reasons for the wide range of the reported incidence are the difference in measuring tools, definitions used, surgical types and techniques, and follow-up duration [23]. Svenningsen et al. [24] reported a significant increase in de novo urge incontinence from 4.1% at 6–12 months after retropubic suburethral sling to 14.9% at 10-year follow-up. The formation of fibrotic tissue around the mesh or mesh erosion may be a possible explanation for the late onset of OAB symptoms. In addition, the effect of physiological change of aging after long-term follow-up may also play an important role [23].
This study found that patients with SUI and low detrusor contractility had the highest reoperation rates, including the rate of repeat suburethral sling (18.2%) and a relatively high rate of urethrolysis (10.9%). A less suburethral sling tension was intentionally adjusted to avoid postoperative difficulty in urination or urinary retention. However, because urethral resistance will decrease with aging, these patients will develop recurrent SUI several years later and require a second suburethral sling to resume urinary continence. In contrast, some women with low detrusor contractility cannot overcome the increase of urethral resistance (although it is mild) by the sling; therefore, they require urethrolysis to resume effective voiding.
Increased urethral resistance after a suburethral sling may help achieve long-term dryness. In a study of 655 women with SUI who were randomized to either Burch colposuspension or autologous fascia pubovaginal sling, a significant increase in postoperative Pdet.Qmax and slightly larger BOOIf values were found in patients who achieved successful outcomes than in those who were considered failures [25]. On the contrary, different points of view were taken from the data of the current study. In the present study, the multivariable logistic regression model indicated that patients with a higher baseline Pdet.Qmax, which is not only an indicator for higher detrusor pressure but also indirect evidence of higher urethral resistance, may offer a better long-term SUI-free survival rate after suburethral sling procedure. However, the odds ratio (1.060; confidence interval, 1.003–1.119) was too small to make predictions in clinical practice. ALPP reflects the passive urethral resistance to the increase in abdominal pressure and was also found to increase after suburethral sling in all SUI subgroups in this study, indicating an effective increase in urethral resistance after surgery. However, the urethral sphincter muscle tone will decrease with aging; therefore, a higher ALPP cannot predict the long-term success of suburethral sling surgery.
Except for patients in the bladder outlet obstruction subgroup, most of the women in the current study met the criteria suggesting increased urethral resistance based on the changes in urodynamic parameters. However, despite the contrary change in the postoperative increased Qmax and decreased BOOIf in women with SUI and concomitant bladder outlet obstruction, the presence of underlying bladder outlet obstruction did not have an apparent negative impact on the continence rate. This may be because those women had already been treated for outlet dysfunction before undergoing anti-incontinence surgery. Therefore, treatment for bladder outlet obstruction was not considered to be correlated with an adverse result after suburethral sling surgery.
In comparison with other studies regarding how LUTD may affect the efficacy of the suburethral sling, the current study had a longer follow-up period, and detailed baseline LUT function data following the preoperative VUDS were available for each of the studied patients in the current study. Four different types of LUT function from diverse aspects, including the cumulative continence-free survival, postoperative complications, reoperation rates, and changes in urodynamic parameters, were also simultaneously compared. In addition, a single surgeon performed the suburethral sling surgery in the studied patients using a standardized procedure, which may have also lowered the heterogenicity of the procedure itself.
Although this study revealed the long-term success rates did not differ between pure SUI and complicated SUI patients after anti-incontinence surgery, this study does not conclude that urodynamic study is useless in the management’s decision making for SUI. With the aid of preoperative urodynamic study, the treatment outcome of SUI had been influenced by the urodynamic findings before surgery and adjusting the sling tension during surgery.
Conclusion
The results in this study show that women with SUI who received suburethral sling had a comparable long-term continence-specific success rate, regardless of their baseline LUT functions. However, women with SUI and concomitant low detrusor contractility may yield a relatively less favorable treatment outcome in terms of higher reoperation rates. A higher baseline Pdet.Qmax in VUDS might suggest a better long-term SUI-free survival after the suburethral sling procedure.
Availability of data and materials
To protect patient privacy and to comply with relevant regulations, identified data are unavailable. Data will be made available upon request from qualified researchers with appropriate ethics board approvals and relevant data use agreements.
References
Hunskaar S, Burgio K, Diokno A, Herzog AR, Hjälmås K, Lapitan MC (2003) Epidemiology and natural history of urinary incontinence in women. Urology 62(4 Suppl 1):16–23. https://doi.org/10.1016/s0090-4295(03)00755-6
Nambiar AK, Arlandis S, Bø K, Cobussen-Boekhorst H, Costantini E, de Heide M, Farag F, Groen J, Karavitakis M, Lapitan MC, Manso M, Arteaga SM, Riogh ANA, O’Connor E, Omar MI, Peyronnet B, Phé V, Sakalis VI, Sihra N, Tzelves L, van Poelgeest-Pomfret ML, van den Bos TWL, van der Vaart H, Harding CK (2022) European association of urology guidelines on the diagnosis and management of female non-neurogenic lower urinary tract symptoms. Part 1: diagnostics, overactive bladder, stress urinary incontinence, and mixed urinary incontinence. Eur Urol. https://doi.org/10.1016/j.eururo.2022.01.045
Esmaeili S, Madani A, Chafjiri F, Madani Z, Leili E (2022) Efficacy and safety of pulsed electromagnetic field (PEMF) stimulation in the treatment of urinary symptoms in women with urinary incontinence. Urol Sci 33(4):170. https://doi.org/10.4103/uros.uros_123_21
Daugirdas SP, Markossian T, Mueller ER, Durazo-Arvizu R, Cao G, Kramer H (2020) Urinary incontinence and chronic conditions in the US population age 50 years and older. Int Urogynecol J 31(5):1013–1020. https://doi.org/10.1007/s00192-019-04137-y
Obloza A, Rai J, Teo R (2018) Surgical treatment of stress urinary incontinence in women. Obstet Gynaecol Reprod Med 28(11–12):339–346. https://doi.org/10.1016/j.ogrm.2018.11.004
Medina CA, Costantini E, Petri E, Mourad S, Singla A, Rodríguez-Colorado S, Ortiz OC, Doumouchtsis SK (2017) Evaluation and surgery for stress urinary incontinence: a FIGO working group report. Neurourol Urodyn 36(2):518–528. https://doi.org/10.1002/nau.22960
Richter HE, Diokno A, Kenton K, Norton P, Albo M, Kraus S, Moalli P, Chai TC, Zimmern P, Litman H, Tennstedt S (2008) Predictors of treatment failure 24 months after surgery for stress urinary incontinence. J Urol 179(3):1024–1030. https://doi.org/10.1016/j.juro.2007.10.074
Kuo HC (2007) Effect of detrusor function on the therapeutic outcome of a suburethral sling procedure using a polypropylene sling for stress urinary incontinence in women. Scand J Urol Nephrol 41(2):138–143. https://doi.org/10.1080/00365590600918121
Kim SJ, Choi HW, Cho HJ, Hwang TK, Kim JC (2010) The influence of preoperative bladder outlet obstruction on continence and satisfaction in patients with stress urinary incontinence after midurethral sling. Int Neurourol J 14(4):267–271. https://doi.org/10.5213/inj.2010.14.4.267
NICE Guidance—Urinary Incontinence and Pelvic Organ Prolapse in Women: Management: © NICE (2019) Urinary incontinence and pelvic organ prolapse in women: management (2019). BJU Int 123(5):777–803. https://doi.org/10.1111/bju.14763
Kuo HC (2001) Anatomical and functional results of pubovaginal sling procedure using polypropylene mesh for the treatment of stress urinary incontinence. J Urol 166(1):152–157
Kuo HC (2005) Long-term surgical results of pubovaginal sling procedure using polypropylene mesh in the treatment of stress urinary incontinence. Urol Int 74(2):147–152. https://doi.org/10.1159/000083286
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A (2003) The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 61(1):37–49. https://doi.org/10.1016/s0090-4295(02)02243-4
Solomon E, Yasmin H, Duffy M, Rashid T, Akinluyi E, Greenwell TJ (2018) Developing and validating a new nomogram for diagnosing bladder outlet obstruction in women. Neurourol Urodyn 37(1):368–378. https://doi.org/10.1002/nau.23307
Resnick NM, Yalla SV (1987) Detrusor hyperactivity with impaired contractile function. An unrecognized but common cause of incontinence in elderly patients. JAMA 257(22):3076–3081. https://doi.org/10.1001/jama.257.22.3076
Nitti VW, Tu LM, Gitlin J (1999) Diagnosing bladder outlet obstruction in women. J Urol 161(5):1535–1540
Kuo H-C (2021) Videourodynamic precision diagnosis and treatment of lower urinary tract symptoms in women. Urol Sci 32(3):94. https://doi.org/10.4103/uros.uros_46_21
Ong HL, Kuo HC (2019) Bladder dysfunction does not affect long-term success rate of the retropubic suburethral sling procedure in women with stress urinary incontinence. Low Urin Tract Symptoms 11(2):O168–O173. https://doi.org/10.1111/luts.12244
Natale F, Illiano E, Zucchi A, Balzarro M, La Penna C, Costantini E (2019) Transobturator mid-urethral sling in females with stress urinary incontinence and detrusor underactivity: effect on voiding phase. Int Urogynecol J 30(9):1519–1525. https://doi.org/10.1007/s00192-019-03871-7
Nager CW, Brubaker L, Litman HJ, Zyczynski HM, Varner RE, Amundsen C, Sirls LT, Norton PA, Arisco AM, Chai TC, Zimmern P, Barber MD, Dandreo KJ, Menefee SA, Kenton K, Lowder J, Richter HE, Khandwala S, Nygaard I, Kraus SR, Johnson HW, Lemack GE, Mihova M, Albo ME, Mueller E, Sutkin G, Wilson TS, Hsu Y, Rozanski TA, Rickey LM, Rahn D, Tennstedt S, Kusek JW, Gormley EA (2012) A randomized trial of urodynamic testing before stress-incontinence surgery. N Engl J Med 366(21):1987–1997. https://doi.org/10.1056/NEJMoa1113595
Clement KD, Lapitan MC, Omar MI, Glazener CM (2013) Urodynamic studies for management of urinary incontinence in children and adults. Cochrane Datab Syst Rev 2013(10):Cd003195. https://doi.org/10.1002/14651858.CD003195.pub3
Pergialiotis V, Mudiaga Z, Perrea DN, Doumouchtsis SK (2017) De novo overactive bladder following midurethral sling procedures: a systematic review of the literature and meta-analysis. Int Urogynecol J 28(11):1631–1638. https://doi.org/10.1007/s00192-017-3417-1
Marcelissen T, Van Kerrebroeck P (2018) Overactive bladder symptoms after midurethral sling surgery in women: risk factors and management. Neurourol Urodyn 37(1):83–88. https://doi.org/10.1002/nau.23328
Svenningsen R, Staff AC, Schiøtz HA, Western K, Sandvik L, Kulseng-Hanssen S (2014) Risk factors for long-term failure of the retropubic tension-free vaginal tape procedure. Neurourol Urodyn 33(7):1140–1146. https://doi.org/10.1002/nau.22466
Kraus SR, Lemack GE, Sirls LT, Chai TC, Brubaker L, Albo M, Leng WW, Lloyd LK, Norton P, Litman HJ, Urinary Incontinence Treatment N (2011) Urodynamic changes associated with successful stress urinary incontinence surgery: Is a little tension a good thing? Urology 78(6):1257–1262. https://doi.org/10.1016/j.urology.2011.07.1413
Acknowledgements
We thank our colleagues at the Department of Urology, Hualien Tzu Chi Hospital for their advice and comments. Further, we are grateful to all the staffs who helped in data collection.
Funding
All authors declare that no support, financial or otherwise, has been received from any organization that may have an interest in the submitted work.
Author information
Authors and Affiliations
Contributions
Conceptualization, H-CK; methodology, P-JL; validation, P-JL and H-CK; formal analysis, P-JL; investigation, P-JL; resources, H-CK; writing—original draft preparation, P-JL; writing—review and editing, H-CK; visualization, P-JL; supervision, H-CK; project administration, H-CK. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board and Ethics Committee of the Buddhist Tzu Chi General Hospital, Hualien, Taiwan (IRB: 109-005-B, January/08/2020).
Informed consent
Informed consent was waived because of the retrospective nature of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, PJ., Kuo, HC. Low detrusor contractility has a less favorable outcome of anti-incontinence surgery for women with stress urinary incontinence. Int Urol Nephrol 55, 2789–2798 (2023). https://doi.org/10.1007/s11255-023-03725-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03725-8