Abstract
Introduction and hypothesis
De novo overactive bladder (OAB) is a known complication of midurethral sling surgery for the treatment of stress urinary incontinence. To date, differences in the incidence of de novo OAB following the use of different types of midurethral sling remain relatively unknown. The purpose of the present systematic review was to evaluate this incidence and summarize current evidence.
Methods
We systematically searched the literature using the MEDLINE, Embase, Scopus, ClinicalTrials.gov, LILACS and Cochrane Central Register of Controlled Trials databases as well as the grey literature and references from the electronically retrieved articles. For comparisons of proportions, we used the chi-squared test. All reported analyses were designed as two-tailed. Statistical significance was set at p < 0.05.
Results
Finally, 32 studies were included in this systematic review, with a total of 3,139 patients who had undergone midurethral sling procedures that included transobturator tapes (TOT), retropubic tapes (TVT) or single-incision tapes (mini-slings). The overall incidence of de novo OAB was 11.5% in nonrandomized studies (280 women) and 6.4% in randomized studies (50 women). In relation to the type of midurethral sling, the incidence of de novo OAB was 9.7% for mini-slings, 11.2% for TVT-O, 8.7% for TOT and 9.8% for TVTs. The chi-squared test did not reveal significant differences (p = 0.58).
Conclusions
Current evidence suggests that the overall incidence of de novo OAB following midurethral sling procedures is approximately 9%. There is not enough evidence to support differences in the effects of the different types of sling with regard to this particular postoperative complication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The joint terminology report of the International Urogynecological Association (IUGA) and the International Continence Society (ICS) defines overactive bladder (OAB) as “urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence, in the absence of urinary tract infection (UTI) or other obvious pathology” [1]. Infection or other pathological conditions (such as bladder tumours, stones or outlet obstruction) should be excluded. Detrusor overactivity refers to a pattern of bladder muscle contractions that are observed during urodynamic investigations.
The most common risk factors for developing OAB are increasing age and body mass index, smoking, menopause, pelvic organ prolapse and pre-existing stress urinary incontinence. Prolapse surgery and continence surgery have also been shown to affect OAB incidence. Prolapse repair resulted in improvement in OAB symptoms in over 80% of the patients in a study that evaluated the influence of prolapse stage on the resolution of urgency symptoms and urgency incontinence after prolapse correction [2]. OAB has a direct impact on the patients’ quality of life (QoL). Women with OAB report significantly decreased health-related QoL and high levels of anxiety and depression, and are more likely to seek treatment for nocturia, frequency and urgency [3]. OAB also seems to affect sleep, general health perception, coping capacity and severity of urinary problems [4].
OAB is common in patients with urinary incontinence. Its aetiology is unclear; however, it is often associated with excessive contractile activity of the detrusor muscle. Surgery in patients with mixed urinary incontinence has been shown to improve the urge component of the incontinence, but not as much as the improvement in the stress component [5]. De novo OAB in patients with no previous findings of urgency incontinence has been seen following placement of a midurethral sling. This poses a significant problem as women with previous stress incontinence and surgery have already suffered a significant impact on their QoL, and therefore having a bothersome lower urinary tract symptom replaced by another one following surgery is something that should ideally be avoided or at least quantified in terms of its prevalence to assist preoperative counselling. To date, it remains unclear whether different types of sling are associated with different outcomes. The purpose of the present systematic review is to summarize current evidence on the specific outcome of de novo OAB following stress incontinence surgery and possibly provide directions for clinical practice and future research.
Materials and methods
Study design
The present study was designed according to the PRISMA guidelines [6]. Eligibility criteria were predetermined by the authors. No language or date restrictions were applied during the literature search. All prospective and retrospective observational studies which investigated the incidence of de novo OAB after insertion of a midurethral sling were considered as eligible for inclusion. The definition of OAB was based on the definitions used by the authors of the different studies. Case reports, reviews and animal studies were excluded. Articles that failed to report information on de novo OAB after these surgical procedures were excluded, along with those that dealt only with urinary incontinence after surgical procedures and those that included patients having bladder neck surgery for urinary incontinence. Studies that enrolled patients with symptoms of mixed urinary incontinence preoperatively and those that included patients who had undergone simultaneous surgery for pelvic organ prolapse (including vaginal hysterectomy, colporrhaphy and vaginal mesh procedure) were also excluded to avoid bias due to unmasking of pre-existing urgency after improvement of stress urinary symptoms. Whenever data from a particular study sample appeared in more than one publication, the article with the most complete follow-up data was used. Stratification for follow-up was not predesigned and was therefore not performed as it was anticipated that the studies would have different lengths of follow-up. No language restrictions were applied. Any discrepancies between the authors during data collection were resolved by the consensus of all authors.
Literature search and data collection
We systematically searched the literature using the MEDLINE (1966–2016), Embase (1947–2016), Scopus (2004–2016), ClinicalTrials.gov (2008–2016), LILACS (1982–2016), and Cochrane Central Register of Controlled Trials (CENTRAL) databases as well as the grey literature and the references from the electronically retrieved articles.
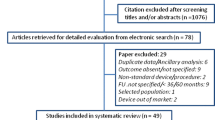
Specifically MEDLINE, Scopus, and ClinicalTrials.gov were searched using the keywords “TOT”, “TVT”, “TVT-O”, “TVT-S”, “TVT-secure”, “sling surgery” and “(anti)incontinence surgery” in combination with “overactive bladder”. Embase was searched using the keywords TOT”, “TVT”, “TVT-O”, “TVT-S”, “TVT-secure” and “sling surgery” in combination with “overactive bladder”, the CENTRAL database was searched using the keyword “overactive bladder”, and the LILACS database was searched using the term “de novo overactive bladder”. The search strategy is summarized in Fig. 1.
Quality assessment
The methodological quality of all the included studies was assessed using the Oxford Level of Evidence criteria and the GRADE list [7]. The randomized trials were evaluated using the modified Jadad score, which briefly assesses the description of studies as randomized along with details of the randomization, the description of studies as double-blind and the details of the double blinding procedure, information on withdrawals and allocation concealment (Fig. 2) [8].
Statistical analysis
The chi-squared and Fisher’s exact tests were used to compare proportions. All reported analyses were designed as two-tailed. Statistical significance was set at p < 0.05. The SPSS version 22.0 was used for the analyses (IBM Corp., Armonk, NY).
Meta-analysis
Meta-analysis of proportions was undertaken and a separate subgroup analysis according to the type of sling used was performed using MedCalc® (MedCalc Software, Ostend, Belgium). The heterogeneity among the studies was assessed using the chi-squared and the I 2-statistic tests. Statistical significance was set at p < 0.05 for the analysis of heterogeneity. Pooled odds ratios and 95% confidence intervals (CI) for all primary and secondary outcomes were calculated using both the Mantel-Haenszel fixed effects and the DerSimonian-Laird random effects models. Specifically, for all analyses, the results from fixed effects model are presented when both the chi-squared and I 2-statistic tests indicated no heterogeneity among the studies. When statistically significant heterogeneity was present, the results were analysed using the random effects model.
Results
Excluded studies
Five randomized trials were excluded because they reported the presence of de novo OAB among patients with urinary incontinence and vaginal prolapse, corrected either with simple colporrhaphy or with the use of synthetic mesh [9,10,11,12,13]. Ten nonrandomized studies were also excluded for the same reason [14,15,16,17,18,19,20,21,22,23]. Another study was excluded because it included patients with pre-existing OAB [24].
Included studies
Finally, 32 studies were included in this systematic review, with a total of 3,139 patients who had undergone midurethral sling procedures including transobturator tapes (TOT), retropubic tapes (TVT) or single-incision tapes (mini-slings) [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55]. The data from these studies were tabulated in two structured tables. Table 1 shows the details of the randomized controlled trials and Table 2 shows the details of the nonrandomized studies.
The overall incidence of de novo OAB was 11.5% in the nonrandomized studies (280 women) and 6.4% in the randomized studies (50 women) (p = 0.024). In relation to the type of midurethral sling, the incidence of de novo OAB was 9.7% for mini-slings, 11.2% for TVT-O, 8.7% for TOT and 9.8% for TVTs. The chi-squared test did not reveal significant differences (p = 0.58). The meta-analysis of proportions revealed significant heterogeneity among the nonrandomized studies (OAB in 11.76% of women, 95% CI 9.351–14.406, data from 2,570 women; Supplementary Fig. 1). Subgroup analysis revealed the following: OAB in 14.91% of women treated with TVT (95% CI 9.578–21.169, data from 768 women; Supplementary Fig. 2), OAB in 8.45% of women treated with TOT (95% CI 5.115–12.714, data from 716 women; Supplementary Fig. 3), OAB in 11.04% of women treated with mini-sling (95% CI 6.769–16.200, data from 500 women; Supplementary Fig. 4), and OAB in 12.66% of women treated with TVT-O (95% CI 7.305–19.217, data from 520 women; Supplementary Fig. 5).
The meta-analysis of proportions revealed moderate heterogeneity In the randomized studies (OAB in 5.88% of women, 95% CI 3.321–9.127, data from 635 women; Supplementary Fig. 6).
Discussion
The incidence of de novo OAB following sling surgery for stress urinary incontinence, ranges between 5% and 22%. The overall prevalence of OAB has been reported to be 16.9% in the USA [56, 57]; in Europe, the prevalence in the general population aged over 40 years is similar (16.6%) [58]. Billions of dollars are spent annually in the USA alone on its management [59]. OAB and urinary urgency incontinence can have a detrimental negative impact on QoL [60]. This is why it is always important to advise the patient about the risks of stress urinary incontinence surgery and the probability of developing OAB later on. According to Boustead, de novo OAB, urinary urgency incontinence and persisting urgency are the most troublesome complications following midurethral tape surgery [61].
This review summarizes the existing data in the literature on de novo OAB following midurethral sling surgery. This will enable the clinician to appropriately advise patients preoperatively on the benefits and risks of the procedure so that the outcome of surgery will better meet patient expectations. During the design of the present systematic review we hoped that current data would be sufficient to reach definitive conclusions regarding differences in the risk of de novo OAB with the different types of sling. However, to date, evidence remains inconclusive and the design of randomized trials, which will specifically include de novo OAB as one of the primary outcome measures, seems to be important, as the majority of studies included in the present systematic review reported de novo OAB as a secondary outcome with a variety of assessment tools.
Previous clinical studies and reviews have proposed various potential pathophysiological mechanisms that may contribute to this pathology. Therefore, postoperative OAB may be part of mixed preoperative incontinence which becomes more prominent for the patient after the cure of stress urinary incontinence. Alternatively, surgery may affect part of the nerve supply to the lower urinary tract leading to OAB. Bladder outlet obstruction is another possible cause of de novo OAB after continence procedures. Sling division may be required in some patients if the symptoms are very bothersome; this is the case for 2–3% of midurethral or pubovaginal slings [15, 62].
Limitations of the study
A number of possible limitations should be considered in the assessment of the results of the present review. Firstly, the nonrandomized design of the majority of studies included introduced several potential biases, including selective reporting, attrition and publication bias. The wide variation in the definitions and terminology made the selection and assessment of the current literature difficult. OAB is often termed urinary urgency, frequency, nocturia, detrusor instability and detrusor overactivity, which makes a literature review on this subject even more puzzling. Furthermore, in the majority of included studies, the follow-up was limited to a maximum of 12 months; therefore, our review provides information mainly about short-term “de novo” OAB. In this context, it would be of interest to evaluate the course of OAB with time from surgery. All the studies included evaluated urinary symptoms but with different, albeit validated, questionnaires. It is therefore possible that some of the studies underestimated the impact of sling surgery on the occurrence of OAB.
Conclusions
Current evidence suggests that the overall incidence of de novo OAB following midurethral sling procedures is approximately 9%. There is not enough evidence to support the beneficial effect of specific types of sling. Given the fact that bladder overactivity may significantly affect the QoL of patients, physicians should inform women prior to midurethral sling procedures for the treatment of uncomplicated stress urinary incontinence about this possible side effect and its anticipated incidence rate.
References
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26. doi:10.1007/s00192-009-0976-9.
Miranne JM, Lopes V, Carberry CL, Sung VW. The effect of pelvic organ prolapse severity on improvement in overactive bladder symptoms after pelvic reconstructive surgery. Int Urogynecol J. 2013;24:1303–8. doi:10.1007/s00192-012-2000-z.
Coyne KS, Sexton CC, Kopp ZS, Ebel-Bitoun C, Milsom I, Chapple C. The impact of overactive bladder on mental health, work productivity and health-related quality of life in the UK and Sweden: results from EpiLUTS. BJU Int. 2011;108:1459–71. doi:10.1111/j.1464-410X.2010.10013.x.
Wang Y, Xu K, Hu H, et al. Prevalence, risk factors, and impact on health related quality of life of overactive bladder in China. Neurourol Urodyn. 2011;30:1448–55. doi:10.1002/nau.21072.
Jain P, Jirschele K, Botros SM, Latthe PM. Effectiveness of midurethral slings in mixed urinary incontinence: a systematic review and meta-analysis. Int Urogynecol J. 2011;22:923–32. doi:10.1007/s00192-011-1406-3.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi:10.1136/bmj.b2700.
OCEBM Levels of Evidence Working Group. The Oxford levels of evidence 2.Oxford: Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/index.aspx?o=5653. Accessed 9 Jul 2017.
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12.
de Boer TA, Kluivers KB, Withagen MIJ, Milani AL, Vierhout ME. Predictive factors for overactive bladder symptoms after pelvic organ prolapse surgery. Int Urogynecol J. 2010;21:1143–9. doi:10.1007/s00192-010-1152-y.
Liang CC, Chang YL, Chang SD, Lo TS, Soong YK. Pessary test to predict postoperative urinary incontinence in women undergoing hysterectomy for prolapse. Obstet Gynecol. 2004;104:795–800. doi:10.1097/01.aog.0000140689.90131.01.
Takahashi S, Obinata D, Sakuma T, et al. Tension-free vaginal mesh procedure for pelvic organ prolapse: a single-center experience of 310 cases with 1-year follow up. Int J Urol. 2010;17:353–8. doi:10.1111/j.1442-2042.2010.02469.x.
Tamanini JT, Castro RC, Tamanini JM, et al. Treatment of anterior vaginal wall prolapse with and without polypropylene mesh: a prospective, randomized and controlled trial – part II. Int Braz J Urol. 2013;39:531–41. doi:10.1590/s1677-5538.ibju.2013.04.11.
Weber AM, Walters MD, Piedmonte MR, Ballard LA. Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol. 2001;185:1299–1304; discussion 1304–6. doi:10.1067/mob.2001.119081.
Futyma K, Miotla P, Bartuzi A, et al. Does a midurethral sling inserted at the time of pelvic organ prolapse mesh surgery increase the rate of de novo OAB? A prospective longitudinal study. Ginekol Pol. 2014;85:652–7.
Klutke C, Siegel S, Carlin B, Paszkiewicz E, Kirkemo A, Klutke J. Urinary retention after tension-free vaginal tape procedure: incidence and treatment. Urology. 2001;58:697–701.
Lensen EJ, Withagen MI, Kluivers KB, Milani AL, Vierhout ME. Urinary incontinence after surgery for pelvic organ prolapse. Neurourol Urodyn. 2013;32:455–9. doi:10.1002/nau.22327.
Liu XC, Zhu L, Lang JH, et al. Total Prolift(TM) system surgery for the repair of recurrent severe pelvic organ prolapse. Zhonghua Yi Xue Za Zhi. 2010;90:2907–10.
Pushkar D, Kasyan G, Malkhasyan V, Abramyan K, Sumerova N. N62 pelvic organ prolapse repair with Prolift transvaginal mesh: retrospective study of 204 cases. Eur Urol Suppl. 2010;9:549–50. doi:10.1016/S1569-9056(10)61263-8.
Rogowski A, Bienkowski P, Tarwacki D, et al. Retrospective comparison between the Prolift and Elevate anterior vaginal mesh procedures: 18-month clinical outcome. Int Urogynecol J. 2015;26:1815–20. doi:10.1007/s00192-015-2772-z.
Salerno J, de Tayrac R, Droupy S, et al. Impact of laparoscopic sacrocolpopexy, with or without a midurethral sling, on lower urinary tract symptoms. Prog Urol. 2016;26:401–8. doi:10.1016/j.purol.2016.03.003.
Sergent F, Resch B, Diguet A, Verspyck E, Marpeau L. Vaginal prolapse and stress urinary incontinence: combined treatment by a single prosthesis. Prog Urol. 2006;16:361–7.
Wu CJ, Chuang FC, Chu LC, Kung FT, Huang KH, Wu MP. Concomitant trocar-guided transvaginal mesh surgery with a midurethral sling in treating advanced pelvic organ prolapse associated with stress or occult stress urinary incontinence. Taiwan J Obstet Gynecol. 2013;52:516–22. doi:10.1016/j.tjog.2013.10.011.
Xiao-chun L, Lan Z, Jing-he L, et al. Total pelvic floor reconstruction surgery for repair of severe pelvic organ prolapse. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2011;33:180–4. doi:10.3881/j.issn.1000-503X.2011.02.016.
Neuman M. Perioperative complications and early follow-up with 100 TVT-SECUR procedures. J Minim Invasive Gynecol. 2008;15:480–4. doi:10.1016/j.jmig.2008.04.006.
Krofta L, Feyereisl J, Velebil P, Otcenasek M, Kasikova E, Krcmar M. TVT-S for surgical treatment of stress urinary incontinence: prospective trial, 1-year follow-up. Int Urogynecol J. 2010;21:779–85. doi:10.1007/s00192-010-1128-y.
Lee KS, Lee YS, Seo JT, et al. A prospective multicenter randomized comparative study between the U- and H-type methods of the TVT SECUR procedure for the treatment of female stress urinary incontinence: 1-year follow-up. Eur Urol. 2010;57:973–9. doi:10.1016/j.eururo.2010.02.018.
Meschia M, Barbacini P, Ambrogi V, Pifarotti P, Ricci L, Spreafico L. TVT-secur: a minimally invasive procedure for the treatment of primary stress urinary incontinence. One year data from a multi-centre prospective trial. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:313–7. doi:10.1007/s00192-008-0772-y.
Renganathan A, Basu M, Duckett J. A series of advantage suburethral slings. J Obstet Gynaecol. 2011;31:521–3. doi:10.3109/01443615.2011.587911.
Sevestre S, Ciofu C, Deval B, Traxer O, Amarenco G, Haab F. Results of the tension-free vaginal tape technique in the elderly. Eur Urol. 2003;44:128–31.
Zhang L, Zhu L, Chen J, Xu T, Lang JH. Tension-free polypropylene mesh-related surgical repair for pelvic organ prolapse has a good anatomic success rate but a high risk of complications. Chin Med J. 2015;128:295–300. doi:10.4103/0366-6999.150088.
Laurikainen E, Valpas A, Aukee P, et al. Five-year results of a randomized trial comparing retropubic and transobturator midurethral slings for stress incontinence. Eur Urol. 2014;65:1109–14. doi:10.1016/j.eururo.2014.01.031.
Masata J, Svabik K, Zvara K, Hubka P, Toman A, Martan A. Comparison of the efficacy of tension-free vaginal tape obturator (TVT-O) and single-incision tension-free vaginal tape (Ajust) in the treatment of female stress urinary incontinence: a 1-year follow-up randomized trial. Int Urogynecol J. 2016;27:1497–505. doi:10.1007/s00192-016-3012-x.
Liapis A, Bakas P, Creatsas G. Comparison of the TVT SECUR system “hammock” and “U” tape positions for management of stress urinary incontinence. Int J Gynaecol Obstet. 2010;111:233–6. doi:10.1016/j.ijgo.2010.07.013.
Oliveira R, Silva A, Pinto R, et al. Short-term assessment of a tension-free vaginal tape for treating female stress urinary incontinence. BJU Int. 2009;104:225–8. doi:10.1111/j.1464-410X.2008.08330.x.
Tommaselli GA, Di Carlo C, Gargano V, Formisano C, Scala M, Nappi C. Efficacy and safety of TVT-O and TVT-Secur in the treatment of female stress urinary incontinence: 1-year follow-up. Int Urogynecol J. 2010;21:1211–7. doi:10.1007/s00192-010-1181-6.
Cornu JN, Sebe P, Peyrat L, Ciofu C, Cussenot O, Haab F. Midterm prospective evaluation of TVT-Secur reveals high failure rate. Eur Urol. 2010;58:157–61. doi:10.1016/j.eururo.2010.04.021.
Chung E, Tse V, Chan L. Mid-urethral synthetic slings in the treatment of urodynamic female stress urinary incontinence without concomitant pelvic prolapse repair: 4-year health-related quality of life outcomes. BJU Int. 2010;105:514–7. doi:10.1111/j.1464-410X.2009.08837.x.
Segal JL, Vassallo B, Kleeman S, Silva WA, Karram MM. Prevalence of persistent and de novo overactive bladder symptoms after the tension-free vaginal tape. Obstet Gynecol. 2004;104:1263–9. doi:10.1097/01.aog.0000147596.44421.72.
Romero Nava LE, Velázquez Sánchez Mdel P, Kunhardt Rasch JR. Mechanical changes of the detrusor after antiincontinence surgery. Ginecol Obstet Mex. 2004;72:227–38.
Castillo-Pino E, Sasson A, Pons JE. Comparison of retropubic and transobturator tension-free vaginal implants for the treatment of stress urinary incontinence. Int J Gynaecol Obstet. 2010;110:23–6. doi:10.1016/j.ijgo.2010.02.019.
Groutz A, Cohen A, Gold R, Pauzner D, Lessing JB, Gordon D. The safety and efficacy of the “inside-out” trans-obturator TVT in elderly versus younger stress-incontinent women: a prospective study of 353 consecutive patients. Neurourol Urodyn. 2011;30:380–3. doi:10.1002/nau.20976.
Cho ST, Song HC, Song HJ, Lee YG, Kim KK. Predictors of postoperative voiding dysfunction following transobturator sling procedures in patients with stress urinary incontinence. Int Neurourol J. 2010;14:26–33. doi:10.5213/inj.2010.14.1.26.
Botros SM, Abramov Y, Goldberg RP, et al. Detrusor overactivity and urge urinary incontinence [corrected] following midurethral versus bladder sling procedures. Am J Obstet Gynecol. 2005;193:2144–8. doi:10.1016/j.ajog.2005.07.009.
Botros SM, Miller JJ, Goldberg RP, et al. Detrusor overactivity and urge urinary incontinence following trans obturator versus midurethral slings. Neurourol Urodyn. 2007;26:42–5. doi:10.1002/nau.20377.
Law TS, Cheung RY, Chung TK, Chan SS. Efficacy and outcomes of transobturator tension-free vaginal tape with or without concomitant pelvic floor repair surgery for urinary stress incontinence: five-year follow-up. Hong Kong Med J. 2015;21:333–8. doi:10.12809/hkmj144397.
Mathias DA, Kharat DS, Fonseca MN. To study and compare the effectiveness of transobturator tape versus Kelly’s repair in the treatment of female stress urinary incontinence. Int J Reprod Contracept Obstet Gynecol. 2016;5:3336–8. doi:10.18203/2320-1770.ijrcog20163160.
Serati M, Braga A, Athanasiou S, et al. Tension-free vaginal tape-obturator for treatment of pure urodynamic stress urinary incontinence: efficacy and adverse effects at 10-year follow-up. Eur Urol. 2017;71:674–9. doi:10.1016/j.eururo.2016.08.054.
Simsek A, Ozgor F, Kirecci SL, et al. Results of tension-free vaginal tape for recurrent stress urinary incontinence after unsuccessful transobturator tape surgery. J Obstet Gynaecol Res. 2014;40:1764–9. doi:10.1111/jog.12410.
Al-Zahrani AA, Gajewski J. Long-term patient satisfaction after retropubic and transobturator mid-urethral slings for female stress urinary incontinence. J Obstet Gynaecol Res. 2016;42:1180–5. doi:10.1111/jog.13035.
Dias J, Xambre L, Costa L, Costa P, Ferraz L. Short-term outcomes of Altis single-incision sling procedure for stress urinary incontinence: a prospective single-center study. Int Urogynecol J. 2014;25:1089–95. doi:10.1007/s00192-014-2355-4.
El-Azab A, El-Nashar S. The tension free vaginal tape versus the pubovaginal slings for women with neurogenic stress urinary incontinence [abstract PD10-06]. J Urol. 2015;193(4 Suppl):e202. doi:10.1016/j.juro.2015.02.946.
Losco GS, Burki JR, Omar YA, Shah PJ, Hamid R. Long-term outcome of transobturator tape (TOT) for treatment of stress urinary incontinence in females with neuropathic bladders. Spinal Cord. 2015;53:544–6. doi:10.1038/sc.2015.70.
Ulrich D, Tammaa A, Holbfer S, et al. Ten-year followup after tension-free vaginal tape-obturator procedure for stress urinary incontinence. J Urol. 2016;196:1201–6. doi:10.1016/j.juro.2016.05.036.
Wang CL, Shen CJ, Lin KL, Long CY. Clinical effects of transobturator tape procedure with porcine small intestine submucosa for female stress urinary incontinence. Kaohsiung J Med Sci. 2016;32:142–6. doi:10.1016/j.kjms.2016.02.005.
Yasa C, Gungor Ugurlucan F, Dural O, Yumru H, Gunaydin C, Yalcin O. Transobturator tape operation for the treatment of stress urinary incontinence in postmenopausal women aged over 65 years. Low Urin Tract Symptoms. 2017. doi:10.1111/luts.12154.
Wein AJ, Rovner ES. Definition and epidemiology of overactive bladder. Urology. 2002;60:7–12. discussion 12
Stewart WF, Van Rooyen JB, Cundiff GW, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20:327–36. doi:10.1007/s00345-002-0301-4.
Milsom I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001;87:760–6.
Ganz ML, Smalarz AM, Krupski TL, et al. Economic costs of overactive bladder in the United States. Urology. 2010;75:526–532, 532.e1–e18. doi:10.1016/j.urology.2009.06.096.
van der Vaart CH, de Leeuw JR, Roovers JP, Heintz AP. The effect of urinary incontinence and overactive bladder symptoms on quality of life in young women. BJU Int. 2002;90:544–9.
Boustead GB. The tension-free vaginal tape for treating female stress urinary incontinence. BJU Int. 2002;89:687–93.
Morgan Jr TO, Westney OL, McGuire EJ. Pubovaginal sling: 4-year outcome analysis and quality of life assessment. J Urol. 2000;163:1845–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest
S. Doumouchtsis has received travel grants and sponsorship to attend conferences from Speciality European Pharma. He has also received speaker Honorarium from Astellas. The other authors have no conflicts of interest to report.
Electronic supplementary material
Supplementary Fig. 1
(GIF 396 kb)
suppl. Figure 2
(JPEG 143 kb)
suppl. Figure 3
(JPEG 115 kb)
suppl. Figure 4
(JPEG 104 kb)
suppl. Figure 5
(JPEG 98 kb)
Supplementary Fig. 6
(GIF 228 kb)
Rights and permissions
About this article
Cite this article
Pergialiotis, V., Mudiaga, Z., Perrea, D.N. et al. De novo overactive bladder following midurethral sling procedures: a systematic review of the literature and meta-analysis. Int Urogynecol J 28, 1631–1638 (2017). https://doi.org/10.1007/s00192-017-3417-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3417-1