Abstract
Purpose
The suburethral sling procedure has been widely used as the first-line treatment for female stress urinary incontinence (SUI). This study retrospectively compared the long-term surgical outcomes and complications between retropubic and transobturator suburethral sling procedures.
Methods
From 2010 to 2022, a total of 533 women with SUI underwent retropubic pubovaginal sling (PVS) or transobturator tape (TOT) procedures using a synthetic polypropylene mesh with or without concomitant anterior colporrhaphy. All patients underwent preoperative videourodynamic studies, Valsalva leak point pressure (VLPP), and voiding efficiency (VE). The success rate, postoperative complications, overactive bladder symptoms, transvaginal urethrolysis, and repeat procedures were compared among different surgical procedures.
Results
Among the patients, PVS was performed in 251 (47.1%) patients and with colporrhaphy in 58 (10.9%), TOT in 174 (32.6%) and with colporrhaphy in 50 (9.4%). The success rate was 87.4% in the PVS group and 75.4% in the TOT group, with or without colporrhaphy (p = 0.001). Urethrolysis was performed in 4.7% of the patients, and repeat suburethral sling procedures were performed in 8.3%. The overall success rate was significantly lower in TOT group, either with high or low VLPP, or with high or low VE. The rate of persistent OAB was significantly higher in TOT group regardless of VLPP or VE, whereas patients with VE < 90% at baseline had a significantly higher rate of postoperative dysuria.
Conclusion
TOT procedures had an inferior long-term success rate than PVS procedures for female SUI. Additionally, no differences in the success rate were observed between patients with different bladder functions, high or low VLPP, and high or low VE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) commonly occurs in women after delivery and has a significant impact on their quality of life. Currently, anti-incontinence surgeries using a suburethral sling either through the retropubic route (pubovaginal sling, PVS) [1] or transobturator route (transobturator tape, TOT) [2] have been widely used as the second-line treatment after conservative treatment and physiotherapy. An effective suburethral sling procedure can create a hammock effect without bladder outlet obstruction (BOO) [3]. The success rate of both PVS and TOT procedures is satisfactory, with 10- and 20-year subjective success rates of approximately 80% and 60%, respectively [4,5,6].
Although the success rates of PVS and TOT are satisfactory, postoperative complications, such as urinary retention, dysuria, sling erosion, and other surgery-related complications, occur [7]. Persistent or de novo overactive bladder (OAB) symptoms, including urgency and urgency urinary incontinence, still bother patients [8, 9], and repeat suburethral sling procedures for SUI recurrence are necessary for some women after anti-incontinence surgery [10].
Bladder dysfunctions are highly prevalent in women with SUI, including detrusor overactivity (DO), detrusor underactivity (DU), detrusor hyperactivity and inadequate contractility (DHIC), and dysfunctional voiding. Patients with DO may have persistent OAB symptoms [11], and patients with DU or DHIC may develop dysuria or urinary retention after anti-incontinence surgery [12]. When BOO develops after anti-incontinence surgery, transvaginal urethrolysis is necessary to resume spontaneous and efficient voiding. Although most patients may remain continent, SUI recurrence may develop after urethrolysis [13].
Few studies have investigated postoperative complications, surgical outcomes, and long-term success rates of patients with SUI with different lower urinary tract conditions and with different suburethral sling procedures. Therefore, this retrospective study aimed to analyze the long-term surgical outcomes of anti-incontinence surgery using different suburethral sling procedures. The findings of this study provide evidence for the selection of an appropriate surgical procedure (PVS or TOT) in women with SUI with different lower urinary tract conditions.
Methods
This was a retrospective study including female patients with pure SUI or predominant SUI in mixed urinary incontinence who underwent suburethral sling procedures from 2010 to 2022. All patients underwent videourodynamic studies (VUDS) before suburethral sling surgery. Lower urinary tract conditions were recorded as stable bladder, hypersensitive bladder, DO, DU, DHIC, or BOO, such as dysfunctional voiding or urethral stricture. Data on Valsalva leak point pressure (VLPP) and voiding efficiency (VE, calculated by voided volume divided by the cystometric bladder capacity) were also recorded. All patients should have VUDS confirming genuine SUI with or without pelvic organ prolapse. Lower urinary tract conditions were defined according to the International Continence Society [14]. A stable bladder was defined as having a cystometric capacity of more than 350 ml, whereas a hypersensitive bladder was defined as less than 350 ml in VUDS.
The suburethral sling procedure was performed either by retropubic PVS or TOT using a synthetic polypropylene mesh (APIS I-Stop System, Aubonne CH, Switzerland) at the middle portion of the urethra [2, 15]. The procedures were performed by three authors. About 90% of procedures were performed by the senior urologist (HCK), who also supervised the procedures by the other two junior urologists (YHJ and SFC). The surgical procedures can be considered to perform by the surgeons with similar experience. The selection of the suburethral sling procedure was not randomized but was based on the surgeon’s preference and judgment. In patients with cystocele, uterine prolapse, or vault prolapse, concomitant transvaginal colporrhaphy was performed using a commercial vaginal mesh or another TOT to fix the bladder base and prevent vaginal prolapse [16], and suburethral sling procedures were performed using PVS or TOT.
After surgery, an indwelling urethral catheter was inserted overnight, and the patients were allowed to urinate the next morning. If patients could urinate freely without high postvoid residual (PVR) volume, they were discharged and followed up at the outpatient clinic. If patients had symptoms of difficult urination or urinary retention, they were managed with clean intermittent catheterization. VUDS were performed if a high PVR volume remained. Transvaginal urethrolysis was performed on the third postoperative day if the presence of BOO was confirmed by VUDS [13]. The procedure was performed by cutting the suburethral sling without removing it. After urethrolysis, patients who could urinate smoothly were discharged from the hospital. Patients with poor pelvic floor relaxation or DU without BOO proven by postoperative VUDS were instructed to continue clean intermittent catheterization and be followed up at the outpatient clinic.
All patients were regularly followed up annually after the suburethral sling procedures. If SUI recurrence had an impact on the quality of life, a repeat suburethral sling procedure was performed [17]. The repeat procedure was similar to the previous one, but without removing the old sling. Patients were also investigated by transrectal sonography or VUDS for de novo or persistent OAB symptoms, such as urgency and urgency urinary incontinence, and medical treatment for OAB symptoms was administered.
Patients were classified as having successful outcomes if they became dry or had minimal SUI (less than 1 episode of SUI per week), improved outcomes if they had fewer SUI episodes than those in the preoperative condition but still had bothersome SUI, or failure outcomes if they had SUI with similar or increased episodes of SUI [18]. The rates of urethrolysis, repeat suburethral sling procedure, and postoperative lower urinary tract symptoms (LUTS) were recorded during the follow-up period. The rates of postoperative LUTS, urethrolysis, repeat suburethral sling procedure, and successful outcomes were compared among patients with different lower urinary tract conditions and different VLPP and VE and between PVS and TOT procedures.
Statistical analysis was performed using SPSS statistical software version 25 (IBM, Armonk, NY, USA). Between-group statistical comparisons in each study arm were performed using Pearson’s chi-square or Fisher’s exact test for categorical variables. A p-value < 0.05 indicated statistical significance.
Results
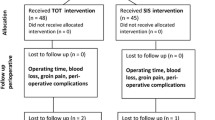
A total of 533 patients were included in this retrospective analysis. The mean age was 62.4 ± 12.2 (28−93) years, and the follow-up duration was 4.9 ± 3.0 (1.0−22.0) years. PVS procedures were performed in 251 patients (45.8%), PVS procedures combined with colporrhaphy in 58 (10.9%), TOT procedures in 174 (32.6%), and TOT procedures combined with colporrhaphy in 50 (9.4%). The baseline patient demographics are shown in Table 1.
The overall success rate was 82.4% (439/533). Of the 533 patients, 68 (12.8%) showed mild improvement, whereas 26 (4.9%) failed the treatment. Persistent OAB was observed in 92 (17.3%), dysuria in 30 (5.6%), and recurrent SUI requiring repeat suburethral sling procedure in 44 (8.3%). The success rate was 87.4% (270/309) in patients who underwent PVS procedures with or without colporrhaphy and 75.4% (169/224) in patients who underwent TOT procedures with or without colporrhaphy (p = 0.001) (Table 1).
Among the patients, VUDS at baseline showed that 271 (50.8%) patients had a stable or hypersensitive bladder, 62 (11.6%) had DU or detrusor acontractile (DA), 126 (23.6%) had DO or DHIC, and 74 (13.9%) had BOO. After suburethral sling procedures, patients with DO or DHIC had a higher rate of persistent OAB, and more patients with stable or hypersensitive bladder were symptom-free. However, the rates of postoperative dysuria, urethrolysis, and repeat suburethral sling procedures were similar among patients with different bladder or voiding conditions (Table 2). All except two patients (one with DU and one with DHIC) still had PVR more than 250 ml, and continued CIC after being discharged from the hospital. The success rate was also similar among patients with different lower urinary tract conditions. However, patients with stable or hypersensitive bladders had a relatively higher success rate than the other subgroups.
Regarding the postoperative complications and reoperation rates, the success rate was similar among patients with VLPP ≥ 90 cmH2O, VLPP < 90 cmH2O, and cystocele without VLPP. However, a higher rate of patients with persistent OAB was noted in patients with VLPP ≥ 90 cmH2O (Table 3). The success rate was also similar in patients with baseline VE ≥ 90% and VE < 90%, and a higher rate of dysuria was observed after suburethral sling procedures in patients with VE < 90% at baseline (Table 4).
The comparison of the treatment outcomes between patients who underwent PVS and TOT procedures showed that the overall success rate was significantly lower in patients who underwent TOT procedures with or without concomitant colporrhaphy, either with VLPP ≥ 90 cmH2O or VLPP < 90 cmH2O or VE ≥ 90% or VE < 90%. A significantly higher rate of de novo and persistent OAB was observed in patients who underwent TOT procedures regardless of VLPP or VE (Table 5).
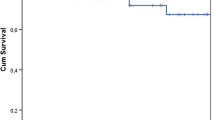
Figure 1 shows the long-term success rates among patients who underwent PVS and TOT suburethral sling procedures with or without concomitant anterior colporrhaphy. The Kaplan–Meier curves showed that the long-term success rates of PVS with or without colporrhaphy were significantly higher than those of TOT with or without colporrhaphy (p = 0.000). Regarding the impact of bladder dysfunction on the treatment outcomes of suburethral slings, no significant differences in the long-term success rates were observed among subgroups with different lower urinary tract conditions (Fig. 2).
Discussion
The results of this study showed that the overall success rate was significantly higher in patients who received PVS than in those who received TOT with or without colporrhaphy (87.4% vs. 75.4%, p = 0.001). The success rates were not different between PVS or TOT alone and PVS or TOT combined with colporrhaphy. The success rates were also not significantly different among patients with different bladder and bladder outlet conditions or those with high or low VLPP or VE. Patients with DA or DU showed an insignificantly lower success rate than the other bladder function subgroups. Patients with a higher VLPP at baseline had a significantly higher rate of postoperative OAB symptoms, whereas those with VE < 90% at baseline had a significantly higher rate of postoperative dysuria.
The results of this study are similar to those of previous studies on the long-term success rates of retropubic tension-free vaginal tape (TVT) and TOT [18,19,20,21]. The rates of transvaginal urethrolysis and repeat suburethral sling procedures are also similar to those reported in previous studies [18, 21]. These similar results indicate that the suburethral sling procedure, either by TOT or PVS, is a long-standing effective procedure for women with SUI. Regarding long-term treatment outcomes, a randomized clinical trial reported no difference between the TOT and TVT procedures [22]. This study revealed that PVS is superior to TOT during a 5-year follow-up period. This result is consistent with that of a previous study, which showed that the success rate of retropubic midurethral sling procedures is superior to that of TOT procedures [23].
Retropubic midurethral sling procedures, such as PVS or TVT, have been advocated as the first-line surgical treatment after conservative treatment has failed for female SUI [1]. However, early complications, such as bladder perforation, wound pain, and vaginal sling erosion, have limited the wide application of this treatment until the advent of TOT [8]. Currently, the TOT procedure is widely performed by most urologists and urogynecologists as the treatment of choice for the midurethral sling procedure because it is relatively safe and easy to learn. Although minor complications could occur in inexperienced hands, the TOT procedure remains the most popular for female SUI, with or without concomitant colporrhaphy.
Recently, the treatment outcomes of PVS, TVT, and TOT have been reported to be similar. The long-term success rate ranged from 75 to 87% [5, 6, 8, 15, 17, 18]. Furthermore, the rates of urethrolysis and reoperation for complications ranged from 5 to 10% [18, 22]. Among patients with different bladder functions at baseline, our previous study showed a higher long-term success rate in patients with a stable bladder (98%), followed by those with DU (82%) and DO (75%) [24]. In this study, the success rate was similar among patients with different bladder functions. This discrepancy may be because all patients underwent VUDS before suburethral sling surgery, which allows physicians to adjust the sling tension during surgery to avoid over-tightening of the sling in patients with DU/DA and place the suburethral sling at the proximal urethra to make the incompetent bladder neck and proximal urethra competent [25, 26]. These adjustments during sling operation based on the VUDS findings may improve the success rate in patients with SUI and different bladder dysfunctions.
Few studies have compared long-term treatment outcomes between retropubic and transobturator suburethral slings for female SUI. Although similar treatment outcomes have been reported, these studies performed retrospective analyses without randomized control clinical trials [6, 22, 23]. In this study, TOT had less favorable long-term outcomes to achieve continence than PVS, and the results were irrelevant to VLPP or VE in baseline VUDS. This inferiority of TOT to PVS may be due to the lower increase in urethral resistance with TOT. Because the suspending angle is smaller in TOT than in PVS, the increase in urethral coaptation with time is also slightly lower in TOT. Although patients might be continent after the TOT procedure in the short term, the success rate will decrease with time. Our previous study on retropubic suburethral sling procedures showed that a higher bladder outlet resistance after PVS provides longer successful outcomes [5]. The lower inclination of the sling created by TOT might limit the effective increase in bladder outlet resistance compared with PVS. Additionally, urethral resistance decreases with aging [27]. After a long-term follow-up, patients will have SUI recurrence and require repeat suburethral sling procedures.
Furthermore, the results of this study showed a significantly higher rate of postoperative OAB symptoms in patients who underwent TOT procedures. Our previous study on persistent OAB symptoms showed that an incompetent bladder neck was responsible for this outcome [25]. A midurethral sling placed at a distal site of the urethra may not close the bladder neck and proximal urethra, resulting in an open bladder neck and persistent OAB. A large cohort retrospective study of de novo OAB after the midurethral sling procedure showed that the incidence of de novo OAB was 6.1% [28]. This incidence is much higher than that reported in this study. We speculated that most of the women who complained of OAB after the midurethral sling procedure might have preoperative OAB coexisting with SUI. Interestingly, among all patients with OAB before surgery, only 17% had persistent OAB symptoms. Among patients who had DO or DHIC in the preoperative VUDS, only 27.8% had persistent OAB. These findings indicate that an effective suburethral sling procedure not only treats SUI but also improves OAB symptoms.
Another common complication of the midurethral sling procedure is dysuria or urinary retention. In a recent retrospective analysis of women who had chronic LUTS after midurethral sling surgery with a mean 5-year follow-up period, urodynamic studies showed that 60% of the patients met the criteria of BOO [29]. In this study, 4.7% of the patients underwent urethrolysis for BOO after the suburethral sling procedure, and 5.6% complained of dysuria. The rate of postoperative dysuria was significantly higher in patients with VE < 90% at baseline and was insignificantly higher in patients with DA or DU and BOO before sling surgery. These findings are consistent with those of a recent study that reported that DU is associated with voiding dysfunction after single-incision sling surgery [30]. Therefore, urodynamic studies before the sling procedure are necessary and should be performed in patients with high PVR volume or BOO symptoms before the suburethral sling procedure to avoid postoperative complications of urinary retention. After the excision of the suburethral sling for postoperative urinary retention, SUI may recur in a high percentage of patients [31].
The results of this study have several implications for the selection of surgical procedures for women with SUI. Patients with preoperative DO or DHIC associated with SUI should be informed that OAB may persist and require continuing medication after the sling procedure. Furthermore, patients with VE < 90% and urodynamic BOO might have de novo dysuria after the sling procedure. The TOT procedure has a significantly higher rate of persistent OAB and a lower success rate than PVS. Therefore, in selecting the suburethral sling procedure for female SUI, the PVS procedure could provide a better long-term success rate than the TOT procedure, especially in women with an open bladder neck and a high grade of SUI.
This study has some limitations. This was a retrospective study. Thus, there could be bias in the selection of the surgical procedure. Because all patients underwent VUDS before sling surgery, physicians might adjust the tension of the sling to avoid urinary retention in patients with DA or DU or place the sling at the proximal urethra to close the incompetent bladder neck. Therefore, the long-term success rate was satisfactory, and postoperative complications were limited in retropubic and transobturator suburethral sling procedures.
Conclusion
This study revealed that the TOT procedure had an inferior long-term success rate than the PVS procedure for female SUI. The success rate was not different between patients with different bladder functions, high or low VLPP, and high or low VE. However, patients with DO or DHIC at baseline had a higher rate of postoperative OAB symptoms, and patients with VE < 90% at baseline had a higher rate of postoperative dysuria.
Data availability
The data of this study can be obtained after contacting the corresponmding authors aftert approval of the IRB of the institution.
References
Kobashi KC, Vasavada S, Bloschichak A, Hermanson L, Kaczmarek J, Kim SK, Kirkby E, Malik R (2023) Updates to surgical treatment of female stress urinary incontinence (SUI): AUA/SUFU guideline. J Urol 209:1091–1098
Rechberger E, Wróbel A, Kulik-Rechberger B, Miotla P, Ziętek A, Rechberger T (2023) The clinical efficacy and safety of outside-in transobturator sling with additional paraurethral fixation—the prospective longitudinal study. Eur J Obstet Gynecol Reprod Biol 290:22–26
Kuo HC (2001) Comparison of video urodynamic results after the pubovaginal sling procedure using rectus fascia and polypropylene mesh for stress urinary incontinence. J Urol 165:163–168
Ong HL, Kuo HC (2019) Bladder dysfunction does not affect long-term success rate of the retropubic suburethral sling procedure in women with stress urinary incontinence. Low Urin Tract Symptoms 11:O168–O173
Liu HH, Kuo HC (2019) Durability of retropubic suburethral sling procedure and predictors for successful treatment outcome in women with stress urinary incontinence. Urology 131:83–88
Chmaj-Wierzchowska K, Raba G, Dykczyński P, Wilczak M, Turlakiewicz K, Latańska I, Sujka W (2022) Clinical outcomes of mid-urethral sling (MUS) procedures for the treatment of female urinary incontinence: a multicenter study. J Clin Med 11:6656
Farag F, Osman NI, Pang KH, Castro-Diaz D, Chapple CR, Cruz F, Gamé X, Goldman H, Greenwell T, Hampel C, Scailteux LM, Roovers JP, Welk B, Heesakkers J (2023) Complications of synthetic midurethral slings: is there a relevant discrepancy between observational data and clinical trials? Eur Urol Focus S2405-4569(23):00244–00254
O’Leary BD, McCreery A, Redmond AE, Keane DP (2023) The efficacy and complications of retropubic tension-free vaginal tapes after 20 years: a prospective observational study. BJOG 130:107–113
Padoa A, Levy E, Fligelman T, Tomashev-Dinkovich R, Tsviban A, Serati M (2023) Predictors of persistent overactive bladder following surgery for advanced pelvic organ prolapse. Int Urogynecol J 34:759–767
Six JC, Pinsard M, Guerin S, Gasmi A, Coiffic J, Richard C, Haudebert C, Nyangoh Timoh K, Hascoet J, Peyronnet B (2023) Risk factors for stress urinary incontinence recurrence after midurethral sling revision. Int J Urol 30:1008–1013
Ozkurkcugil C, Avci IE (2023) Factors predicting treatment success in mixed urinary incontinence treated with midurethral sling. Low Urin Tract Symptoms 15:50–56
Lee PJ, Kuo HC (2023) Low detrusor contractility has a less favorable outcome of anti-incontinence surgery for women with stress urinary incontinence. Int Urol Nephrol 55:2789–2798
Wu SY, Kuo HC (2019) Long-term outcomes of anti-incontinence surgery and subsequent transvaginal sling incision for urethral obstruction. Int Urogynecol J 30:761–766
Rosier PFWM, Gammie A, Valdevenito JP, Speich J, Smith P, Sinha S, Members of the ICS working group PFS23 (2023) ICS-SUFU standard: theory, terms, and recommendations for pressure-flow studies performance, analysis, and reporting .Part 2: analysis of PFS, reporting and diagnosis. Neurourol Urodyn 42(7):1603–1627
Kuo HC (2001) Anatomical and functional results of pubovaginal sling procedure using polypropylene mesh for the treatment of stress urinary incontinence. J Urol 166:152–157
Ahmed AA, Abdellatif AH, El-Helaly HA, Tagreda IA, El-Feky MM, Agha MM, Abdelraouf AG, Abdelrahim AF (2020) Concomitant transobturator tape and anterior colporrhaphy versus transobturator subvesical mesh for cystocele-associated stress urinary incontinence. Int Urogynecol J 31:1633–1640
Ong HL, Jiang YH, Kuo HC (2019) Repeat retropubic suburethral sling procedure is effective for recurrent female stress urinary incontinence. Low Urin Tract Symptoms 11:O89–O92
Kuo HC (2005) Long-term surgical results of pubovaginal sling procedure using polypropylene mesh in the treatment of stress urinary incontinence. Urol Int 74:147–152
Goessens EMV, Cammu H (2023) A 10- to 20-year follow-up after tension-free vaginal tape for stress urinary incontinence. Int Urogynecol J 34:2107–2114
Zilberlicht A, Karmakar D, DwyeR PL, Murray C, Kugelman N (2023) Predictors of surgical failure of open burch colposuspension versus retropubic midurethral sling for stress urinary incontinence. Urology 177:69–73
Solhaug BR, Nyhus MØ, Svenningsen R, Vølloyhaug I (2023) Rates of subjective and objective cure, satisfaction, and pain 10-20 years after tension free vaginal tape (TVT) surgery: a retrospective cohort study. BJOG. https://doi.org/10.1111/1471-0528.17738
Salo H, Sova H, Laru J, Talvensaari-Mattila A, Nyyssönen V, Santala M, Piltonen T, Koivurova S, Rossi H-R (2023) Long-term results of a prospective randomized trial comparing tension-free vaginal tape versus transobturator tape in stress urinary incontinence. Int Urogynecol J 34:2249–2256
Alexandridis V, Lundmark Drca A, Ek M, Westergren Söderberg M, Andrada Hamer M, Teleman P (2023) Retropubic slings are more efficient than transobturator at 10-year follow-up: a swedish register-based study. Int Urogynecol J 34:1307–1315
Kuo HC (2007) Effect of detrusor function on the therapeutic outcome of a suburethral sling procedure using a polypropylene sling for stress urinary incontinence in women. Scand J Urol Nephrol 41:138–143
Chen YC, Chen HW, Kuo HC (2023) Bladder neck incompetence could be an etiology of overactive bladder syndrome in women with stress urinary incontinence after anti-incontinence surgery: insights from transrectal sonography. World J Urol 41:3083–3089
Jiang YH, Wang CC, Chuang FC, Ke QS, Kuo HC (2013) Positioning of a suburethral sling at the bladder neck is associated with a higher recurrence rate of stress urinary incontinence. J Ultrasound Med 32:239–245
Chai TC, Huang L, Kenton K, Richter HE, Baker J, Kraus S, Litman H (2012) Urinary incontinence treatment network (UITN) association of baseline urodynamic measures of urethral function with clinical, demographic and other urodynamic variables in women prior to undergoing midurethral sling surgery. Neurourol Urodyn 31:496–501
Serna-Gallegos T, Dutta S, Crowder C, Wadensweiler P, Whitcomb EL, Guaderrama NM (2024) Risk factors for de novo overactive bladder after midurethral sling. Urogynecol (Phila) 30:59–64
Ross J, Avvakoumova L, Yassein A, Payne M, Maciejewski C, Mallick R, Breau RH, Vigil H, Hickling D (2023) Prevalence and predictors of bladder outlet obstruction in women with chronic urinary symptoms and a history of urethral sling surgery. J Urol 209(2):384–390
Morán Pascual E, Zabalo A, Colet Guitert O, Bonillo MÁ, Martínez-Cuenca E, Broseta Rico E, Budía A, Arlandis S (2023) Is detrusor underactivity associated with voiding dysfunction after single incision sling surgery? Minerva Urol Nephrol 75:642–648
Juhl C, Thimm MH, Glavind K (2023) Impact on urinary incontinence after management of complications related to a retropubic midurethral sling. Int Urogynecol J 34:2767–2774
Funding
This study was supported by the grant from Tzu Chi Medical Foundation, grant number TCMF-MP 110-03-01 and TCMF-SP 112-01.
Author information
Authors and Affiliations
Contributions
Yuan-Hong Jiang and Shenf-Fu Chen collect data and investigations Yuan-Hong Jiang wrote the draft manuscript Hann-Chorng Kuo supervised the study and revised the manuscript
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, YH., Chen, SF. & Kuo, HC. Effect of lower urinary tract conditions on surgical outcomes of different suburethral sling procedures for female stress urinary incontinence. Int Urol Nephrol 56, 2905–2912 (2024). https://doi.org/10.1007/s11255-024-04047-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-024-04047-z