Abstract
Dysfunctions in NAD+ metabolism are associated with neurodegenerative diseases, acute brain injury, diabetes, and aging. Loss of NAD+ levels results in impairment of mitochondria function, which leads to failure of essential metabolic processes. Strategies to replenish depleted NAD+ pools can offer significant improvements of pathologic states. NAD+ levels are maintained by two opposing enzymatic reactions, one is the consumption of NAD+ while the other is the re-synthesis of NAD+. Inhibition of NAD+ degrading enzymes, poly-ADP-ribose polymerase 1 (PARP1) and ectoenzyme CD38, following brain ischemic insult can provide neuroprotection. Preservation of NAD+ pools by administration of NAD+ precursors, such as nicotinamide (Nam) or nicotinamide mononucleotide (NMN), also offers neuroprotection. However, NMN treatment demonstrates to be a promising candidate as a therapeutic approach due to its multi-targeted effect acting as PARP1 and CD38 inhibitor, sirtuins activator, mitochondrial fission inhibitor, and NAD+ supplement. Many neurodegenerative diseases or acute brain injury activate several cellular death pathways requiring a treatment strategy that will target these mechanisms. Since NMN demonstrated the ability to exert its effect on several cellular metabolic pathways involved in brain pathophysiology it seems to be one of the most promising candidates to be used for successful neuroprotection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nicotinamide adenine dinucleotide (NAD+) is a ubiquitous and abundant molecule in biological organisms that is required as a cofactor or substrate for about 500 cellular reactions, therefore playing a key role in cellular metabolism. Originally NAD+ was determined as a cofactor for redox reactions [1]. NAD+, its reduced form NADH, and its phosphorylated forms (NADP and NADPH) are involved in glycolysis, the pentose phosphate pathway, oxidative phosphorylation, TCA cycle, as well ketone bodies, lipids, and amino acid metabolism. Apart from facilitating enzymatic reactions associated with transfer of electrons from one molecule to another, NAD+ also serves as a substrate for several NAD+ consuming enzymes associated with post-translational modifications or second messenger generation [1,2,3,4,5,6]. The pyridine nucleotide metabolism has a cyclic nature since NAD+ degradation is the major biological source of nicotinamide (Nam) and at least part of Nam is used for conversion back to NAD+ [7].
Recently, the interest in NAD+ and its related metabolic pathways dramatically increased. This is because new findings revealed that dysfunctions in NAD+ metabolism are associated with several diseases and pathologic states. Decreased NAD+ levels were observed under conditions of neurodegenerative disease, following acute brain injury, in diabetes, or during aging. Loss of NAD+ results in impaired mitochondrial function, thus failure in cellular bioenergetics metabolism and in perturbation of essential metabolic processes. Strategies that attempt to replenish NAD+ pools therefore can offer significant improvements of tissue in pathologic state.
Two opposing enzymatic processes determine cellular NAD+ levels. One represents activity of enzymes that consume NAD+ (degradation by NAD+ glycohydrolases) and the other facilitates re-synthesis of NAD+ pools. Consequently, there have been two main approaches to improve tissue NAD+ levels. Since NAD+ consumption is accelerated by over-activation of NAD+ glycohydrolases under bioenergetic stress conditions, the main focus of neuroprotection was on inhibition of NAD+ degrading enzymes [8,9,10,11]. In another approach, the preservation of NAD+ pools was achieved by supplying the tissue with precursors for NAD+ synthesis [12,13,14,15,16,17,18,19,20].
In this short review we will focus on the advantages of therapeutic approaches that use NAD+ synthesis precursors to improve the pathologic conditions associated with neurodegeneration and acute brain injury.
Major Pathways of NAD+ Catabolism
As mentioned above, there are several NAD+ glycohydrolases that contribute to NAD+ catabolism. A main NAD+ consuming enzyme is poly-ADP-ribose polymerase 1 (PARP1), which is activated particularly following DNA damage [9, 21, 22]. PARP1, by poly-ADP-ribosylation (PAR) of histone and non-histone proteins, activates the repair of single stranded DNA breaks [23]. Significant or sustained DNA damage can lead to over-activation of PARP1, resulting in depletion of intracellular NAD+ pools, decreased activity of NAD+-dependent enzymes and accumulation of PAR polymers [24,25,26]. Both pharmacologic and genetic inhibition of PARP1 activity demonstrated significant protection against acute brain injury [8,9,10,11].
Poly-ADP-ribose polymerization is a post-translational modification that is removed by poly-ADP-ribose glycohydrolase (PARG) [27]. There are two major forms of PARG [27, 28]. The 110 kDa PARG110 is localized predominantly in nucleus and the 60 kDa PARG60 is found only in the cytoplasm [29, 30]. The original hypothesis of PARP1 over-activation induced NAD+ depletion as a major death factor was challenged by data showing that the poly-ADP-ribose molecules per se are toxic to the cells [31]. Thus, overexpression of PARG was protective and animals with reduced levels of PARG showed significantly increased brain damage following ischemic insult [31]. However, there are several reports suggesting that inhibition of PARG activity is protective [32,33,34] and the selective knockdown of nuclear form of PARG110 reduces genotoxic agent induced cell death [35]. However, focal ischemia in the same transgenic mouse model with selective knockdown of PARG110 resulted in increased infarct volume when compared to wild type (WT) animals [30]. These conflicting data suggest that the mechanisms responsible for cellular death following PARP1 over-activation are still elusive and the significant contribution of the individual adverse factors might depend on the type of the insult or pathologic conditions. Furthermore, strong and prolonged inhibition of PARP1 activity will compromise the main biological role of this enzyme, damaged DNA repair, which can have adverse effects on cells survival after longer recovery periods.
Another enzyme that has a significant role in NAD+ metabolism is the ectoenzyme CD38. CD38 generates Nam and second messengers, cyclic ADP-ribose or ADP-ribose from NAD+ [36, 37]. In CD38 knockout (CD38KO) mice, brain NAD+ pools were reported significantly higher when compared to WT animals [38], however, the changes in NAD+ levels were dependent on the brain region [39]. It was demonstrated that CD38 expression levels increase with age, which leads to decline in cellular NAD+ [40]. Interestingly, stereologic quantification of hippocampal neurons in adult CD38KO animals showed about 15% higher number of CA1 neurons when compared to WT mice [39]. Unexpectedly to previous findings, although these animals exhibit higher number of hippocampal neurons their PAR levels were 140% higher compared to WT mice due to lower expression of nuclear PARG isoform [39]. Furthermore, the most abundant immunoreactivity of PAR antibody was detected in the perinuclear region of neurons, and following ischemic insult there was an additional increase in PAR predominantly within astrocytes [39]. The experiments with CD38KO animals also revealed that CD38 significantly contributes to post-ischemic NAD+ depletion during the late recovery period, after 4 h of reperfusion [39]. These data suggest that apart from PARP1, CD38 also contributes to increased post-ischemic NAD+ consumption.
Recently, a research group exploring mechanism of axonal degeneration discovered an enzyme, SARM1 (sterile alpha and Toll/interleukin-1 receptor motif-containing 1), that is triggered by axonal damage and initiates a local destruction program involving rapid breakdown of NAD+ after injury [41, 42]. SARM1 is a negative regulator of Toll-like receptor-activated transcription program [43] and it has intrinsic NADase activity, cleaving NAD+ into ADP-ribose, cyclic ADPR, and Nam [42].
Another post-translational modification that is regulated by NAD+ is protein acetylation. This modification is carried out by acetyltransferases that transfer the acetyl group from acetyl-CoA to the lysine residue of the target protein [44]. Enzymes that remove the acetyl group from the acetylated lysine are represented by several classes of deacetylases [44,45,46]. Sirtuins (SIRTs), NAD+ depended class III deacetylases, remove Nam from NAD+ and transfer the acetyl group from the lysine residue to the ADP-ribose moiety [47,48,49]. During this process NAD+ is consumed and Nam plus O-acetyl-ADP-ribose is released. SIRTs deacetylate histone and non-histone proteins, thus they regulate gene expression and also different metabolic pathways within the cell. Generally, increased sirtuin activity is considered beneficial for cells since sirtuin dependent deacetylation is associated with protective effects against neurodegeneration, acute brain injury, prolonged life span, suppression of adverse effects of diabetes, and beneficial impact of exercise [47,48,49,50]. So far it was not shown whether increased sirtuin activity can also significantly reduce cellular NAD+ pools, however, low NAD+ level leads to increased protein acetylation. There are several isoforms of sirtuins that are localized to specific intracellular compartments. Sirt1, Sirt6, and Sirt7 were predominantly found in the nucleus, Sirt2 is considered to be cytosolic enzyme, and mitochondria harbor several sirtuins (Sirt3-5), although only Sirt3 was shown to have robust deacetylase activity and to control the mitochondrial acetylome [51, 52].
NAD+ Replenishment
To maintain tissue NAD+ pools cells express enzymes that can generate and replace the consumed NAD+. There are two major metabolic pathways that serve this purpose. NAD+ can be synthesized de novo from tryptophan, however, the main source of NAD+ is from the salvage pathway [2], where it is generated in two enzymatic reactions that use Nam, nicotinic acid (NA), or nicotinamide riboside (NR) as precursors, respectively. In mammals, Nam is considered to be the main precursor for NAD+ synthesis [53]. In the first rate-limiting step of the salvage pathway, nicotinamide phosphoribosyltransferase (NAMPT) forms nicotinamide mononucleotide (NMN) from Nam and 5-phosphoribosyl-1-pyrophosphate (PRPP). In the next step, NMN is converted to NAD+ by NMN adenylyl transferase (NMNAT) in the presence of ATP [5, 54]. Thus, the salvage pathway is part of the cyclic NAD+ metabolism where the product of NAD+ glycohydrolases, Nam, is recycled to generate new NAD+ (Fig. 1).
Schematic diagram showing the major pathways of NAD+ metabolism. NAD+ can be degraded by poly-ADP-ribose polymerase (PARP1), CD38 ectoenzyme, sterile alpha and toll/interleukin-1 receptor motif-containing 1 enzyme (SARM1), and sirtuins (SIRTs). These enzymes remove nicotinamide (Nam) from NAD+ and generate poly-, cyclic-, mono-, or O-acetyl-ADP-ribose. Nam is recycled into NAD+ by the salvage pathway. NAMPT generates NMN from Nam and PRPP. In the next step NMN is used by nicotinamide mononucleotide adenylyltransferase (NMNAT) to generate NAD+
Stimulating NAD+ Synthesis as a Strategy for Therapeutic Intervention
As we mentioned above, pathologic conditions associated with neurodegenerative diseases or excessive bioenergetic and oxidative stress lead to depletion of cellular NAD+ pools. Apart from inhibiting the NAD+ degrading enzymes a simple approach to improve cellular metabolic conditions is to stimulate the NAD+ generation by increasing the substrate supply for the salvage pathway. Therefore, Nam was one of the first metabolic compounds used to elevate NAD+ levels [55, 56]. Since Nam is readily available and can pass the cellular membranes, it was the most logical candidate to use for treatment of conditions of brain tissue NAD+ deficiency.
Administration of Nam improved bioenergetics following brain ischemia or oxidative stress and ameliorated ischemic and traumatic brain injury [13, 14, 57, 58]. The ability of Nam to pass the cellular membranes explains its rapid penetration of the blood–brain barrier (BBB) [59], however, it also suggests that the Nam can be readily removed from the tissue by blood flow [5]. Consequently, although Nam administration showed improved post-ischemic outcome at 125 mg/kg dose, the most neuroprotective dose of Nam was rather high at 500 mg/kg [57]. Several mechanisms were suggested to play a role in Nam neuroprotection following acute brain injury. These included prevention of ATP depletion [55, 57], inhibition of PARP1, CD38, and SIRTs [9, 60, 61], lipid peroxidation [62], anti-inflammatory activity [63], and prevention of apoptosis [55, 64].
Since Nam is a substrate for the Nampt enzyme its impact on the NAD+ synthesis is limited by Nampt activity. Therefore, administration of Nam under conditions where the Nampt enzyme is inhibited or dysfunctional will not lead to increased NAD+ synthesis by the salvage pathway.
NMN as a Promising Candidate for Treatment of NAD+ Deficiency
To even more efficiently facilitate NAD+ synthesis, by bypassing the rate-limiting step in the salvage pathway, one can administer NMN that will directly feed into the one-step enzymatic generation of NAD+ via NMNAT. There are several reports showing that intraperitoneal administration of NMN can significantly increase brain tissue NAD+ levels within 15 min post-injection ([65, 66], for review see [67]). This suggests that there is an active transport of NMN or its metabolites into the intracellular compartments, where it is converted to NAD+. However, the mechanisms of NMN transport across the BBB or cellular and mitochondrial membranes need to be determined.
Recently published data suggest that NMN is metabolized extracellularly to NR by CD73 [68]. NR is then transported across the plasma membrane through dipyridamole-sensitive nucleoside transporters [69] and phosphorylated intracellularly by NR kinase 1 (NRK1) to NMN [2, 69, 70]. Finally, intracellular NMN is converted to NAD+ by isoforms of NMNAT [2]. Experiments with NRK1 knockout mice demonstrated the requirement of NRK1 activity for generation of NAD+ from NR and NMN [71]. Interestingly, although not all the enzymes required for generation of NAD+ from NR or NMN are present in plasma, already 5 min after an intraperitoneal injection of NMN the plasma NAD+ levels increased significantly. These data suggest that NMN is rapidly absorbed from the gut into blood, however, the NMN in vivo pharmacokinetics and its conversion to NAD+ in cells or blood are so far poorly understood. Thus, NMN and NR demonstrated superior pharmacokinetics when compared to Nam, primarily due to involvement of active transport mechanisms that allow for better control of the translocation process of these compounds from plasma into intracellular compartments. As a result there is more effective intracellular accumulation of NMN and its conversion to NAD+.
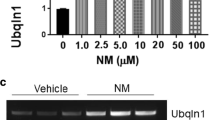
NMN administration improved several neuronal functions in the brain and showed significant neuroprotection against both neurodegenerative conditions or acute brain injury [15, 16, 19, 72,73,74,75]. There were several mechanisms identified as targets of NMN induced changes in cellular metabolism. These were linked to its direct inhibitory effect of PARP1 and CD38 or indirectly regulating gene expression and enzyme activity via modulating acetylation of histone and non-histone proteins due to increased NAD+ levels (Fig. 2). Since the most effective dose for Nam administration was 500 mg/kg, the majority of studies with NMN treatment used similar 300–1000 mg/kg doses. However, high intracellular levels of NMN can be less effective or have adverse effects under particular pathologic conditions [15, 76]. Reports from cell culture studies of the Wallerian degeneration model support these findings by showing that accumulation of intracellular NMN due to inhibition of NMNAT promotes axonal degeneration [77]. While so far there are no reports of significant adverse effects of NMN on physiological parameters like temperature, blood pressure, cerebral blood flow [15], or other forms of toxicity, the studies that used different doses of NMN suggest that pharmacological titration of NMN administration should be applied to determine the most effective treatment protocol for particular disease conditions.
Schematic diagram showing direct and indirect NMN targets. Administration of NMN leads to inhibition of PARP1 and CD38 activity. Cellular and mitochondrial NAD+ levels are increased following NMN treatment causing increased activity of NAD+- dependent deacetylases SIRT1 and SIRT3. As a result, PGC1α is deacetylated and its activity increases, SIRT1—dependent hypoxia inducing factor 1α (HIF-1α) accumulation is decreased, and nuclear factor (erythroid-derived 2)-like 2 (Nrf2) protein levels are increased. Higher SIRT3 activity deacetylates mitochondrial proteins leading to increased oxidative phosphorylation and ATP production (mito resp, ATP), more efficient mitochondrial reactive oxygen species (mito ROS) detoxification, and inhibition of mitochondrial fission (mito fission)
The beneficial outcomes of NMN administration were reported via downstream effects of SIRTs stimulation, particularly SIRT1 and SIRT3. The protective effect of SIRT1 activation against ischemic brain damage were showed after treatment of animals with SIRT1 activator, resveratrol [78,79,80]. Similarly, mitochondrial SIRT3 mediates neuroprotection following ischemic insult [81]. Therefore, it was not surprising that NMN administration, which leads to increased cellular NAD+ levels, stimulated SIRT1, and ameliorated several pathologic conditions. For example, NMN-induced activation of SIRT1 prevented axonal degeneration [82], similarly overexpression of Nampt or NMN treatment reduced brain infarction following focal ischemia via the AMPK pathway which is SIRT1 dependent [74]. It was also reported that NMN can stimulate Nrf2 expression or neurogenesis via increased activity of SIRT1 [18, 75]. Furthermore there are reports of neuroprotective mechanisms by NMNAT (enzyme that uses NMN to generate NAD+) due to its possible chaperon activity [83].
The beneficial effect of NMN administration was also showed in models of heart disease [20, 84,85,86,87]. Additionally, NMN was able to reverse pathologic alterations induced by aging via modulation of PGC1α , HIF-1α, and CD38 activity [17, 76, 88, 89] (for review see [90]), or diabetes via activation of SIRT1 [65, 91].
We have reported a dramatic neuroprotection of NMN against ischemic insult following a single, about 60 mg/kg, dose administration [15]. Additionally, in a mouse model of Alzheimer’s disease repeated NMN administration every other day for 28 days improved mitochondrial functions, normalized brain SIRT1 and CD38 levels [16]. Surprisingly, we found that NMN administration can also affect mitochondrial dynamics after both chronic and single intraperitoneal treatment [16, 66]. After NMN administration the size distribution of brain mitochondria was shifted towards longer organelles [66]. The NMN treatment resulted in significant increase of hippocampal mitochondria NAD+ levels leading to improved bioenergetics metabolism as reflected in higher brain tissue ATP [66]. Increase in intra-mitochondrial NAD+ activated SIRT3 led to deacetylation of mitochondrial proteins including manganese superoxide dismutase [66]. This was accompanied by lower mitochondrial reactive oxygen species generation and reduction of Drp1 phosphorylation, ultimately leading to reduced fission [66].
Finally, we found that in addition to the dramatic neuroprotection, NMN also inhibits NAD+ glycohydrolase activity of PARP1 and CD38 [15, 39].
Conclusion
Research from our and other laboratories demonstrates that NMN has multiple effects on cellular metabolism under both physiologic and pathologic conditions. Following NMN treatment there was a significant reduction of PAR, increase in brain and mitochondrial NAD+ levels, and normalization of post-ischemic mitochondrial proteins acetylation and morphology. Thus, NMN has a multi-targeted effect and acts as a combination of several neuroprotective compounds (as PARP1 and CD38 inhibitors, sirtuin activators, mitochondrial fission inhibitors and NAD+ supplements).
Another advantage of using NMN administration as a therapeutic approach is that it is an endogenous cellular metabolic compound. Thus, even at the highest dose used no toxicity or side effects after NMN injection was detected, nor were there significant changes in animal physiological parameters [15]. Since many neurodegenerative diseases and acute brain injury due to ischemic or traumatic attack activate several mechanisms that can lead to cell death, these diseases lead to complex and devastating neurologic conditions. Therefore, a successful treatment strategy needs to implement a multi-targeted approach that will affect several mechanisms in multiple cell types. Since NMN demonstrated the ability to exert its effect on several cellular metabolic pathways involved in brain pathophysiology, it seems to be one of the most promising candidates to be used for successful neuroprotection.
References
Berger F, Ramirez-Hernandez MH, Ziegler M (2004) The new life of a centenarian: signalling functions of NAD(P). Trends Biochem Sci 29:111–118
Belenky P, Bogan KL, Brenner C (2007) NAD + metabolism in health and disease. Trends Biochem Sci 32:12–19
Houtkooper RH, Canto C, Wanders RJ, Auwerx J (2010) The secret life of NAD+: an old metabolite controlling new metabolic signaling pathways. Endocr Rev 31:194–223
Imai S, Guarente L (2014) NAD + and sirtuins in aging and disease. Trends Cell Biol 24:464–471
Owens K, Park JH, Schuh R, Kristian T (2013) Mitochondrial dysfunction and NAD + metabolism alterations in the pathophysiology of acute brain injury. Transl Stroke Res 4:618–634
Klimova N, Long A, Kristian T (2018) Significance of mitochondrial protein post-translational modifications in pathophysiology of brain injury. Transl Stroke Res 9:223–237
Gholson RK (1966) The pyridine nucleotide cycle. Nature 212:933–935
Endres M, Wang ZQ, Namura S, Waeber C, Moskowitz MA (1997) Ischemic brain injury is mediated by the activation of poly(ADP-ribose)polymerase. J Cereb Blood Flow Metab 17:1143–1151
Szabo C, Dawson VL (1998) Role of poly(ADP-ribose) synthetase in inflammation and ischaemia-reperfusion. Trends Pharmacol Sci 19:287–298
Whalen MJ, Clark RS, Dixon CE, Robichaud P, Marion DW, Vagni V, Graham SH, Virag L, Hasko G, Stachlewitz R, Szabo C, Kochanek PM (1999) Reduction of cognitive and motor deficits after traumatic brain injury in mice deficient in poly(ADP-ribose) polymerase. J Cereb Blood Flow Metab 19:835–842
Chiarugi A, Moskowitz MA (2003) Poly(ADP-ribose) polymerase-1 activity promotes NF-kappaB-driven transcription and microglial activation: implication for neurodegenerative disorders. J Neurochem 85:306–317
Yang J, Klaidman LK, Nalbandian A, Oliver J, Chang ML, Chan PH, Adams JD Jr (2002) The effects of nicotinamide on energy metabolism following transient focal cerebral ischemia in Wistar rats. Neurosci Lett 333:91–94
Ayoub IA, Lee EJ, Ogilvy CS, Beal MF, Maynard KI (1999) Nicotinamide reduces infarction up to two hours after the onset of permanent focal cerebral ischemia in Wistar rats. Neurosci Lett 259:21–24
Mokudai T, Ayoub IA, Sakakibara Y, Lee EJ, Ogilvy CS, Maynard KI (2000) Delayed treatment with nicotinamide (vitamin B(3)) improves neurological outcome and reduces infarct volume after transient focal cerebral ischemia in Wistar rats. Stroke 31:1679–1685
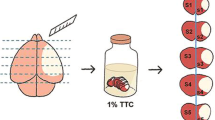
Park JH, Long A, Owens K, Kristian T (2016) Nicotinamide mononucleotide inhibits post-ischemic NAD(+) degradation and dramatically ameliorates brain damage following global cerebral ischemia. Neurobiol Dis 95:102–110
Long AN, Owens K, Schlappal AE, Kristian T, Fishman PS, Schuh RA (2015) Effect of nicotinamide mononucleotide on brain mitochondrial respiratory deficits in an Alzheimer’s disease-relevant murine model. BMC Neurol 15:19
de Picciotto NE, Gano LB, Johnson LC, Martens CR, Sindler AL, Mills KF, Imai S, Seals DR (2016) Nicotinamide mononucleotide supplementation reverses vascular dysfunction and oxidative stress with aging in mice. Aging Cell 15:522–530
Wei CC, Kong YY, Li GQ, Guan YF, Wang P, Miao CY (2017) Nicotinamide mononucleotide attenuates brain injury after intracerebral hemorrhage by activating Nrf2/HO-1 signaling pathway. Sci Rep 7:717
Wei CC, Kong YY, Hua X, Li GQ, Zheng SL, Cheng MH, Wang P, Miao CY (2017) NAD replenishment with nicotinamide mononucleotide protects blood-brain barrier integrity and attenuates delayed tissue plasminogen activator-induced haemorrhagic transformation after cerebral ischaemia. Br J Pharmacol 174:3823–3836
Yamamoto T, Byun J, Zhai P, Ikeda Y, Oka S, Sadoshima J (2014) Nicotinamide mononucleotide, an intermediate of NAD + synthesis, protects the heart from ischemia and reperfusion. PLoS ONE 9:e98972
Strosznajder RP, Czubowicz K, Jesko H, Strosznajder JB (2010) Poly(ADP-ribose) metabolism in brain and its role in ischemia pathology. Mol Neurobiol 41:187–196
Dawson VL (2005) Inhibition of poly(adenosine diphosphate-ribose) polymerase (PARP) in experimental models of neurologic diseases: cell death prevention. Retina 25:S31–S32
Althaus FR, Kleczkowska HE, Malanga M, Muntener CR, Pleschke JM, Ebner M, Auer B (1999) Poly ADP-ribosylation: a DNA break signal mechanism. Mol Cell Biochem 193:5–11
Kauppinen TM, Swanson RA (2007) The role of poly(ADP-ribose) polymerase-1 in CNS disease. Neuroscience 145:1267–1272
Ha HC, Snyder SH (2000) Poly(ADP-ribose) polymerase-1 in the nervous system. Neurobiol Dis 7:225–239
Dawson VL, Dawson TM (2004) Deadly conversations: nuclear-mitochondrial cross-talk. J Bioenerg Biomembr 36:287–294
Davidovic L, Vodenicharov M, Affar EB, Poirier GG (2001) Importance of poly(ADP-ribose) glycohydrolase in the control of poly(ADP-ribose) metabolism. Exp Cell Res 268:7–13
Brochu G, Shah GM, Poirier GG (1994) Purification of poly(ADP-ribose) glycohydrolase and detection of its isoforms by a zymogram following one- or two-dimensional electrophoresis. Anal Biochem 218:265–272
Di Meglio S, Denegri M, Vallefuoco S, Tramontano F, Scovassi AI, Quesada P (2003) Poly(ADPR) polymerase-1 and poly(ADPR) glycohydrolase level and distribution in differentiating rat germinal cells. Mol Cell Biochem 248:85–91
Cozzi A, Cipriani G, Fossati S, Faraco G, Formentini L, Min W, Cortes U, Wang ZQ, Moroni F, Chiarugi A (2006) Poly(ADP-ribose) accumulation and enhancement of postischemic brain damage in 110-kDa poly(ADP-ribose) glycohydrolase null mice. J Cereb Blood Flow Metab 26:684–695
Andrabi SA, Kim NS, Yu SW, Wang H, Koh DW, Sasaki M, Klaus JA, Otsuka T, Zhang Z, Koehler RC, Hurn PD, Poirier GG, Dawson VL, Dawson TM (2006) Poly(ADP-ribose) (PAR) polymer is a death signal. Proc Natl Acad Sci USA 103:18308–18313
Formentini L, Arapistas P, Pittelli M, Jacomelli M, Pitozzi V, Menichetti S, Romani A, Giovannelli L, Moroni F, Chiarugi A (2008) Mono-galloyl glucose derivatives are potent poly(ADP-ribose) glycohydrolase (PARG) inhibitors and partially reduce PARP-1-dependent cell death. Br J Pharmacol 155:1235–1249
Blenn C, Althaus FR, Malanga M (2006) Poly(ADP-ribose) glycohydrolase silencing protects against H2O2-induced cell death. Biochem J 396:419–429
Lu XC, Massuda E, Lin Q, Li W, Li JH, Zhang J (2003) Post-treatment with a novel PARG inhibitor reduces infarct in cerebral ischemia in the rat. Brain Res 978:99–103
Burns DM, Ying W, Kauppinen TM, Zhu K, Swanson RA (2009) Selective down-regulation of nuclear poly(ADP-ribose) glycohydrolase. PLoS ONE 4:e4896
Schuber F, Lund FE (2004) Structure and enzymology of ADP-ribosyl cyclases: conserved enzymes that produce multiple calcium mobilizing metabolites. Curr Mol Med 4:249–261
Malavasi F, Deaglio S, Funaro A, Ferrero E, Horenstein AL, Ortolan E, Vaisitti T, Aydin S (2008) Evolution and function of the ADP ribosyl cyclase/CD38 gene family in physiology and pathology. Physiol Rev 88:841–886
Aksoy P, White TA, Thompson M, Chini EN (2006) Regulation of intracellular levels of NAD: a novel role for CD38. Biochem Biophys Res Commun 345:1386–1392
Long A, Park JH, Klimova N, Fowler C, Loane DJ, Kristian T (2017) CD38 knockout mice show significant protection against ischemic brain damage despite high level poly-ADP-ribosylation. Neurochem Res 42:283–293
Chini CCS, Tarrago MG, Chini EN (2017) NAD and the aging process: role in life, death and everything in between. Mol Cell Endocrinol 455:62–74
Gerdts J, Brace EJ, Sasaki Y, DiAntonio A, Milbrandt J (2015) SARM1 activation triggers axon degeneration locally via NAD(+) destruction. Science 348:453–457
Essuman K, Summers DW, Sasaki Y, Mao X, DiAntonio A, Milbrandt J (2017) The SARM1 toll/interleukin-1 receptor domain possesses intrinsic NAD(+) cleavage activity that promotes pathological axonal degeneration. Neuron 93:1334–1343
O’Neill LA, Fitzgerald KA, Bowie AG (2003) The Toll-IL-1 receptor adaptor family grows to five members. Trends Immunol 24:286–290
Saha RN, Pahan K (2006) HATs and HDACs in neurodegeneration: a tale of disconcerted acetylation homeostasis. Cell Death Differ 13:539–550
Glozak MA, Sengupta N, Zhang X, Seto E (2005) Acetylation and deacetylation of non-histone proteins. Gene 363:15–23
Marmorstein R, Trievel RC (2009) Histone modifying enzymes: structures, mechanisms, and specificities. Biochim Biophys Acta 1789:58–68
Michan S, Sinclair D (2007) Sirtuins in mammals: insights into their biological function. Biochem J 404:1–13
Houtkooper RH, Pirinen E, Auwerx J (2012) Sirtuins as regulators of metabolism and healthspan. Nat Rev Mol Cell Biol 13:225–238
Jesko H, Wencel P, Strosznajder RP, Strosznajder JB (2016) Sirtuins and their roles in brain aging and neurodegenerative disorders. Neurochem Res 42:876–890
Morris KC, Lin HW, Thompson JW, Perez-Pinzon MA (2011) Pathways for ischemic cytoprotection: role of sirtuins in caloric restriction, resveratrol, and ischemic preconditioning. J Cereb Blood Flow Metab 31:1003–1019
He W, Newman JC, Wang MZ, Ho L, Verdin E (2012) Mitochondrial sirtuins: regulators of protein acylation and metabolism. Trends Endocrinol Metab 23:467–476
Hirschey MD, Shimazu T, Huang JY, Schwer B, Verdin E (2011) SIRT3 regulates mitochondrial protein acetylation and intermediary metabolism. Cold Spring Harb Symp Quant Biol 76:267–277
Collins PB, Chaykin S (1972) The management of nicotinamide and nicotinic acid in the mouse. J Biol Chem 247:778–783
Magni G, Amici A, Emanuelli M, Raffaelli N, Ruggieri S (1999) Enzymology of NAD + synthesis. Adv Enzymol Relat Areas Mol Biol 73:135–182, xi
Klaidman LK, Mukherjee SK, Hutchin TP, Adams JD (1996) Nicotinamide as a precursor for NAD + prevents apoptosis in the mouse brain induced by tertiary-butylhydroperoxide. Neurosci Lett 206:5–8
Knip M, Douek IF, Moore WP, Gillmor HA, McLean AE, Bingley PJ, Gale EA, European Nicotinamide Diabetes Intervention Trial G (2000) Safety of high-dose nicotinamide: a review. Diabetologia 43:1337–1345
Yang J, Klaidman LK, Chang ML, Kem S, Sugawara T, Chan P, Adams JD (2002) Nicotinamide therapy protects against both necrosis and apoptosis in a stroke model. Pharmacol Biochem Behav 73:901–910
Hoane MR, Gilbert DR, Holland MA, Pierce JL (2006) Nicotinamide reduces acute cortical neuronal death and edema in the traumatically injured brain. Neurosci Lett 408:35–39
Spector R (1979) Niacin and niacinamide transport in the central nervous system. In vivo studies. J Neurochem 33:895–904
Banasik M, Komura H, Shimoyama M, Ueda K (1992) Specific inhibitors of poly(ADP-ribose) synthetase and mono(ADP-ribosyl)transferase. J Biol Chem 267:1569–1575
Klaidman LK, Mukherjee SK, Adams JD Jr (2001) Oxidative changes in brain pyridine nucleotides and neuroprotection using nicotinamide. Biochim Biophys Acta 1525:136–148
Chong ZZ, Lin SH, Maiese K (2002) Nicotinamide modulates mitochondrial membrane potential and cysteine protease activity during cerebral vascular endothelial cell injury. J Vasc Res 39:131–147
Ungerstedt JS, Blomback M, Soderstrom T (2003) Nicotinamide is a potent inhibitor of proinflammatory cytokines. Clin Exp Immunol 131:48–52
Mukherjee SK, Klaidman LK, Yasharel R, Adams JD Jr (1997) Increased brain NAD prevents neuronal apoptosis in vivo. Eur J Pharmacol 330:27–34
Yoshino J, Mills KF, Yoon MJ, Imai S (2011) Nicotinamide mononucleotide, a key NAD(+) intermediate, treats the pathophysiology of diet- and age-induced diabetes in mice. Cell Metab 14:528–536
Klimova N, Kristian T (2019) Nicotinamide mononucleotide alters mitochondrial dynamics by SIRT3 dependent mechanism in male mice. J Neurosci Res (in press)
Yoshino J, Baur JA, Imai SI (2018) NAD(+) intermediates: the biology and therapeutic potential of NMN and NR. Cell Metab 27:513–528
Grozio A, Sociali G, Sturla L, Caffa I, Soncini D, Salis A, Raffaelli N, De Flora A, Nencioni A, Bruzzone S (2013) CD73 protein as a source of extracellular precursors for sustained NAD+ biosynthesis in FK866-treated tumor cells. J Biol Chem 288:25938–25949
Nikiforov A, Dolle C, Niere M, Ziegler M (2011) Pathways and subcellular compartmentation of NAD biosynthesis in human cells: from entry of extracellular precursors to mitochondrial NAD generation. J Biol Chem 286:21767–21778
Trammell SA, Schmidt MS, Weidemann BJ, Redpath P, Jaksch F, Dellinger RW, Li Z, Abel ED, Migaud ME, Brenner C (2016) Nicotinamide riboside is uniquely and orally bioavailable in mice and humans. Nat Commun 7:12948
Ratajczak J, Joffraud M, Trammell SA, Ras R, Canela N, Boutant M, Kulkarni SS, Rodrigues M, Redpath P, Migaud ME, Auwerx J, Yanes O, Brenner C, Canto C (2016) NRK1 controls nicotinamide mononucleotide and nicotinamide riboside metabolism in mammalian cells. Nat Commun 7:13103
Wang X, Hu X, Yang Y, Takata T, Sakurai T (2016) Nicotinamide mononucleotide protects against beta-amyloid oligomer-induced cognitive impairment and neuronal death. Brain Res 1643:1–9
Yao Z, Yang W, Gao Z, Jia P (2017) Nicotinamide mononucleotide inhibits JNK activation to reverse Alzheimer disease. Neurosci Lett 647:133–140
Wang P, Xu TY, Guan YF, Tian WW, Viollet B, Rui YC, Zhai QW, Su DF, Miao CY (2011) Nicotinamide phosphoribosyltransferase protects against ischemic stroke through SIRT1-dependent adenosine monophosphate-activated kinase pathway. Ann Neurol 69:360–374
Zhao Y, Guan YF, Zhou XM, Li GQ, Li ZY, Zhou CC, Wang P, Miao CY (2015) Regenerative neurogenesis after ischemic stroke promoted by nicotinamide phosphoribosyltransferase-nicotinamide adenine dinucleotide cascade. Stroke 46:1966–1974
Mills KF, Yoshida S, Stein LR, Grozio A, Kubota S, Sasaki Y, Redpath P, Migaud ME, Apte RS, Uchida K, Yoshino J, Imai SI (2016) Long-term administration of nicotinamide mononucleotide mitigates age-associated physiological decline in mice. Cell Metab 24:795–806
Di Stefano M, Nascimento-Ferreira I, Orsomando G, Mori V, Gilley J, Brown R, Janeckova L, Vargas ME, Worrell LA, Loreto A, Tickle J, Patrick J, Webster JR, Marangoni M, Carpi FM, Pucciarelli S, Rossi F, Meng W, Sagasti A, Ribchester RR, Magni G, Coleman MP, Conforti L (2014) A rise in NAD precursor nicotinamide mononucleotide (NMN) after injury promotes axon degeneration. Cell Death Differ 22:731
Girbovan C, Morin L, Plamondon H (2012) Repeated resveratrol administration confers lasting protection against neuronal damage but induces dose-related alterations of behavioral impairments after global ischemia. Behav Pharmacol 23:1–13
Della-Morte D, Dave KR, DeFazio RA, Bao YC, Raval AP, Perez-Pinzon MA (2009) Resveratrol pretreatment protects rat brain from cerebral ischemic damage via a sirtuin 1-uncoupling protein 2 pathway. Neuroscience 159:993–1002
Raval AP, Dave KR, Perez-Pinzon MA (2006) Resveratrol mimics ischemic preconditioning in the brain. J Cereb Blood Flow Metab 26:1141–1147
Yin J, Han P, Tang Z, Liu Q, Shi J (2015) Sirtuin 3 mediates neuroprotection of ketones against ischemic stroke. J Cereb Blood Flow Metab 35:1783–1789
Araki T, Sasaki Y, Milbrandt J (2004) Increased nuclear NAD biosynthesis and SIRT1 activation prevent axonal degeneration. Science 305:1010–1013
Zhai RG, Zhang F, Hiesinger PR, Cao Y, Haueter CM, Bellen HJ (2008) NAD synthase NMNAT acts as a chaperone to protect against neurodegeneration. Nature 452:887–891
Karamanlidis G, Lee CF, Garcia-Menendez L, Kolwicz SC Jr, Suthammarak W, Gong G, Sedensky MM, Morgan PG, Wang W, Tian R (2013) Mitochondrial complex I deficiency increases protein acetylation and accelerates heart failure. Cell Metab 18:239–250
Lee CF, Chavez JD, Garcia-Menendez L, Choi Y, Roe ND, Chiao YA, Edgar JS, Goo YA, Goodlett DR, Bruce JE, Tian R (2016) Normalization of NAD + redox balance as a therapy for heart failure. Circulation 134:883–894
Martin AS, Abraham DM, Hershberger KA, Bhatt DP, Mao L, Cui H, Liu J, Liu X, Muehlbauer MJ, Grimsrud PA, Locasale JW, Payne RM, Hirschey MD (2017) Nicotinamide mononucleotide requires SIRT3 to improve cardiac function and bioenergetics in a Friedreich’s ataxia cardiomyopathy model. JCI Insight 2:93885
Nadtochiy SM, Wang YT, Nehrke K, Munger J, Brookes PS (2018) Cardioprotection by nicotinamide mononucleotide (NMN): involvement of glycolysis and acidic pH. J Mol Cell Cardiol 121:155–162
Gomes AP, Price NL, Ling AJ, Moslehi JJ, Montgomery MK, Rajman L, White JP, Teodoro JS, Wrann CD, Hubbard BP, Mercken EM, Palmeira CM, de Cabo R, Rolo AP, Turner N, Bell EL, Sinclair DA (2013) Declining NAD(+) induces a pseudohypoxic state disrupting nuclear-mitochondrial communication during aging. Cell 155:1624–1638
Camacho-Pereira J, Tarrago MG, Chini CC, Nin V, Escande C, Warner GM, Puranik AS, Schoon RA, Reid JM, Galina A, Chini EN (2016) CD38 dictates age-related NAD decline and mitochondrial dysfunction through an SIRT3-dependent mechanism. Cell Metab 23:1127–1139
Imai S (2009) The NAD World: a new systemic regulatory network for metabolism and aging–Sirt1, systemic NAD biosynthesis, and their importance. Cell Biochem Biophys 53:65–74
Ramsey KM, Mills KF, Satoh A, Imai S (2008) Age-associated loss of Sirt1-mediated enhancement of glucose-stimulated insulin secretion in beta cell-specific Sirt1-overexpressing (BESTO) mice. Aging Cell 7:78–88
Acknowledgements
The project described was supported by Award Number I01BX000917 from the Biomedical Laboratory Research & Development Service of the VA Office of Research and Development to TK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Special issue in honor of Prof Vera Adam-Vizi.
Rights and permissions
About this article
Cite this article
Klimova, N., Kristian, T. Multi-targeted Effect of Nicotinamide Mononucleotide on Brain Bioenergetic Metabolism. Neurochem Res 44, 2280–2287 (2019). https://doi.org/10.1007/s11064-019-02729-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-019-02729-0