Abstract
Mitochondria are complex organelles that undergo constant fusion and fission in order to adapt to the ever-changing cellular environment. The fusion/fission proteins, localized in the inner and outer mitochondrial membrane, play critical roles under pathological conditions such as acute brain injury and neurodegenerative diseases. Post-translational modifications of these proteins tightly regulate their function and activity, ultimately impacting mitochondrial dynamics and their efficiency to generate ATP. The individual post-translational modifications that are known to affect mitochondrial dynamics include SUMOylation, ubiquitination, phosphorylation, S-nitrosylation, acetylation, O-linked N-acetyl-glucosamine glycosylation, ADP-ribosylation, and proteolytic cleavage. Under stress or pathologic conditions, several of these modifications are activated leading to a complex regulatory mechanism that shifts the state of the mitochondrial network. The main goal is to accommodate and adapt the cellular bioenergetics metabolism to the energetic demand of the new extra- and/or intracellular environment. Understanding the complex relationship between these modifications on fusion and fission proteins in particular pathologic stress or diseases can provide new promising therapeutic targets and treatment approaches. Here, we discuss the specific post-translational modifications of mitochondrial fusion/fission proteins under pathologic conditions and their impact on mitochondrial dynamics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
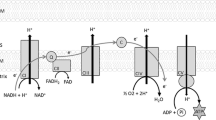
Mitochondria are subcellular organelles that are involved in a variety of essential cellular functions, the most prominent role being to supply the cell with metabolic energy in the form of ATP [1]. The type of function mitochondria performs is reflected in its structure, more specifically its unique ability to undergo fusion and fission. This dynamic behavior allows mitochondria to respond to physiological and pathological stimuli, resulting in their fragmentation into smaller organelles or forming elongated, interconnected forms [2]. Fusion mixes solutes, metabolites, and proteins in newly formed mitochondria and helps to promote a healthy environment and counter post-stressful conditions. Fission functions to create new smaller mitochondria when needs arise but also performs damage control by allowing removal of dysfunctional mitochondrial segments [3].
A group of guanosine triphosphatases (GTPases)-dependent proteins mediate fusion and fission. These proteins work in unison to quickly divide and fuse the double lipid bilayers of the mitochondrial membranes. Fusion of the outer membrane is mediated by two core proteins, mitofusin 1 (Mfn1) and mitofusin 2 (Mfn2), while inner membrane fusion is mediated by a singular protein, mitochondrial dynamin-like GTPase encoded by optic atrophy 1 gene (Opa1). Fission, on the other hand, is mediated by dynamin-related protein 1 (Drp1) and Drp1 regulating proteins mitochondrial fission 1 (Fis1), mitochondrial fission factor (Mff), and mitochondrial dynamics protein 49/51 (MiD49/51) [4]. These regulatory proteins are required for Drp1 recruitment to the mitochondria where it is then responsible for outer membrane division [5]. Due to the mitochondrial highly dynamic environment, the activity of these proteins is tightly regulated by proteolysis and post-translational modifications that include SUMOylation, ubiquitination, phosphorylation, S-nitrosylation, acetylation, and O-linked-N-acetyl-glucosamine glycosylation [6,7,8]. Fine tuning of the mitochondrial fusion/fission process by post-translational modifications plays a central role not only in facilitating normal mitochondrial function but also is crucial in cellular bioenergetic stress responses to various pathologic conditions, such as neurodegenerative diseases, ischemia, and traumatic brain injury (TBI). Here, we discuss post-translational modifications of fission and fusion proteins and how they alter mitochondrial dynamics and functions in response to pathologic stress in the brain.
SUMOylation and Regulation of Mitochondrial Dynamics
The post-translational modification, SUMOylation, involves covalent attachment of small ubiquitin-like modifiers (SUMOs) to lysine residues of substrate proteins via an enzyme cascade similar to that of the ubiquitination pathway. Unlike polyubiquitination at the lysine 48 residue that targets proteins for degradation, SUMOylation can alter protein function, activity, stability, and subcellular localization offering an effective way to rapidly adapt to the stress-induced changing environment. Mammals have four SUMO paralogs (SUMO1–4) that are conjugated to target proteins by a process that is controlled by a heterodimer of SUMO-activating enzyme subunits 1 and 2 (SAE1/2), a single SUMO-specific conjugating enzyme Ubc9 (E2), and several E3 ligases [9, 10]. SUMO-1 was identified as a covalent protein modifier of the nuclear pore protein RanGAP1 (Ran-GTP-ase-activated protein 1) [11]. SUMO-2 and SUMO-3 differ from each other by only three N-terminal residues and are referred to as SUMO-2/3. SUMO-4 isoform has been proposed from DNA sequence analysis, and the conjugation of a mature form of SUMO-4 has been reported in conditions of extreme cellular stress [12].
Recently, a new mitochondrial SUMO-3 ligase was identified [13]. The mitochondrial-anchored protein ligase (MAPL) functionally stabilizes ER/mitochondrial contact sites that act as hotspots for mitochondrial constriction, calcium flux, cristae remodeling, and cytochrome c release. MAPL can be a crucial component in regulation of mitochondrial functions and events related to mitochondrial interaction with other organelles since a large number of unidentified mitochondrial SUMO targets were detected [13].
SUMOs are de-conjugated from proteins by sentrin-specific proteases (SENPs) (for review see [14, 15]). In mammals, there are six SENPs. SENP1 and SENP2 remove SUMO1 and SUMO-2/3 while SENP3 and SENP5 are more specific for the removal of SUMO-2/3 [16]. Thus, the level of SUMOylated proteins in cells is determined by both, the activity of enzymes that perform SUMO modifications and the activity of de-SUMOylating SENPs isopeptidases.
Under stress, the SUMOylation of proteins increases. This results in the adjustment of cells to changes in environmental conditions yielding a protective effect. For example, during hibernation that convenes a robust resistance to severe reduction of blood flow (state resembling ischemic conditions), there is a marked increase in protein SUMOylation in the brain with concomitant loss of free SUMO [17].
A number of studies have reported that in experimental models of ischemia, there is a global increase in SUMOylation, especially in the brain, and that it is associated with a protective cellular response [18,19,20,21]. Although it was reported that several mitochondrial proteins show SUMOylation as a post-translational modification [22,23,24], Drp1 has been reported as the only mitochondrial fission protein that is regulated by SUMOylation. Compared to other mitochondrial proteins that regulate fusion and fission, the majority of Drp1 is cytoplasmic. Therefore, the translocation to the mitochondria is crucial for the mitochondrial fragmentation process.
As a physiological response, mitochondrial fission is triggered during the cell cycle in the G2/M phase [25]. The SUMO protease SENP5 translocates from the nucleoli to the mitochondrial membrane and deSUMOylates Drp1. This is followed by mitochondrial fragmentation during mitosis [25]. Interestingly, the same laboratory reported that overexpression of SENP5 catalyzes the cleavage of SUMO1 from a number of mitochondrial substrates, including Drp1, leading to the reduction of mitochondrial fragmentation. Silencing of SENP5 resulted in fragmented mitochondria, promoting fission [23]. These seemingly opposing results might reflect a differential effect of Drp1 SUMOylation depending on the particular changes in intracellular environment, and possible synergistic effect of pathways that lead to differential post-translational modifications of Drp1 (Fig. 1).
Effect of SUMOylation on mitochondrial dynamics. SUMOylation affects only the Drp1 protein from the family of proteins involved in mitochondria fission and fusion control. There is one group of enzymes that perform SUMOylation by attaching SUMO paralog, SUMO-1 or SUMO-2/3, to the lysine residue of the target protein (SEA1 and SEA2 SUMO-activators, SUMO conjugating enzyme Ubc9, and E3 ligases). De-SUMOylation of individual paralogs is carried out in a more specific manner by sentrin-specific proteases SENP1–6. SENP1/2 removes both SUMO1 and SUMO2/3 while SENP3/5 more specifically removes SUMO2/3. Regulation of fusion and fission by SUMOylation depends on which SUMO conjugate is attached to Drp1, SUMO-2/3 (S2/3), or SUMO-1 (S1). Removal of SUMO1 by SENP5 and SENP2 leads to decreased mitochondrial fragmentation. SENP3 removes SUMO2/3 which favors activated fission. The balance between SUMO1 and SUMO2/3 remains unclear even more so in pathological conditions
Similarly, sustained, low activity of SENP2 triggers pathologic changes in the brain [26]. The knockout of SENP2 increased levels of SUMO1 association with Drp1 causing mitochondrial fragmentation and ultimately severe developmental abnormalities [26]. Overexpression of SENP2 prevented the SUMO1-induced accumulation of Drp1 to the mitochondria and also decreased the SUMO1-induced accumulation of Drp1 in the cytoplasm. Thus, suggesting that Drp1 reduction mediated by SENP2 is caused by protein degradation rather than decreased targeting to mitochondria [26].
Interestingly Drp1 is also modified by SUMO2/3. SUMO2/3-ylation acts to separate Drp1 from the mitochondria, ultimately promoting fusion or a less fragmented population of these organelles. DeSUMOylation of SUMO2/3 by SENP3 enhances Drp1 localization with mitochondria promoting apoptosis and fission. Oxygen glucose deprivation (OGD), an in vitro model of ischemia, downregulates expression of SENP3 during the OGD insult, which results in a shift toward SUMOylated Drp1 and dissociation from the mitochondria. However, following re-oxygenation, the SENP3 levels recover allowing deSUMOylation of Drp1, which leads to Drp1 localization to mitochondria and promotes fragmentation and cytochrome c release [27].
The balance and regulation between conjugations of SUMO1 versus SUMO2/3 to Drp1 still remains unclear. However, SUMO1 generally does not exhibit increase in acute stress conditions, which might suggest that SUMO2/3 conjugation to Drp1 has precedence in ischemia and brain injury in the attempt to ensure cell survival [23].
Thus, there is also a seemingly opposite effect of Drp1 SUMOylation on mitochondrial fission between SUMO1 and SUMO2/3 modifications. The final effect of Drp1 modifications on its functional outcome can depend on the combinations of several post-translational modifications, depending on the environmental changes that can trigger different signaling pathways. Therefore, when assessing the possible functional outcome of post-translational modifications in studied pathologic stress, one needs to screen for possible combinations of different modifications rather than determine only one particular change in the modification of the protein of interest.
SUMOylation is also involved in the regulation of Parkin, a cytosolic E3 ligase that carries out the attachment of ubiquitin monomers to proteins located at the outer mitochondrial membrane and facilitates mitochondria specific autophagy (mitophagy). Parkin is SUMO1-ylated, which appears to enhance its ubiquitination activity and ultimately mitophagy [28]. This increased activity affects downstream targets of Parkin, such as the mitochondrial fusion proteins Mfn1/2 [29]. Increased ubiquitination of Mfn1/2 targets them for degradation and ultimately a reduction in fusion activity. It has yet to be determined whether in brain ischemic conditions there is a greater amount of SUMO1-Parkin, which could lead to degradation of Mfn1/2 and subsequent decreased fusion.
Data from studies examining changes in mitochondrial proteins suggest that levels of SUMOylation are primarily regulated not by the activity of the SUMOylation process (E1, E2, E3 enzymes) but rather by controlling the deSUMOyation mechanisms via altering specific SENPs activities. Thus, the targeted alterations of distinct SENP levels provide an efficient mechanism for the changing of SUMOs metabolism and could offer a promising therapeutic approach. However, generally, the SUMOylation of cellular proteins is regulated through a complex interplay between SUMOylation and other post-translational modifications through modification of the proteins involved in their enzymatic pathways [28, 30].
Of note, increased activity of the SUMOylation/deSUMOylation cycle can also have potentially adverse effects on mitochondrial functions, particularly under bioenergetic stress. This is because the activity of the E1 enzyme is an ATP-dependent process that leads to consumption of ATP and generation of AMP and pyrophosphate (PPi) [28]. Prolonged, increased levels of intracellular AMP and PPi can inhibit mitochondrial oxidative phosphorylation by interfering with mitochondrial adenine nucleotide transporter, thus compromising mitochondrial ATP production [31]. Furthermore, depleting mitochondria of adenine nucleotide leads to increased sensitivity to calcium-induced mitochondrial permeability transition pore opening [32].
In summary, SUMOylation regulates mitochondrial fusion/fission via several pathways. Drp1 SUMOylation/deSUMOylation directly alters availability of Drp1 at the mitochondrial membrane while Parkin SUMOylation indirectly increases Mfn1/2 degradation resulting in decreased mitochondrial fusion. Furthermore, protein levels of SENPs and availability of ATP can alter the activity of the SUMOylation/deSUMOylation cycle. During stress conditions, it is unclear how these various pathways are altered; however, future studies in this field would gain a possible therapeutic advantage.
Ubiquitination
Ubiquitin is a small regulatory protein that can be reversibly added to lysine residues of proteins by ubiquitin ligases. The addition of this modification has broad effects on protein function and stability depending on whether a monomer or polymer of ubiquitin is attached. The addition of a monomer regulates protein activity while the formation of an ubiquitin chain to a single lysine targets the protein to the proteasome for degradation [33]. It is reported that the core proteins involved in mitochondrial dynamics, Drp1, Mfn1/2, and Fis1, can be regulated by ubiquitination. Drp1 is ubiquitinated by either MARCH5 or Parkin, both of which are E3 ubiquitin ligases [34,35,36]. Fis1 is ubiquitinated by MARCH5 while Mfn1/2 by Parkin and MARCH5 [29, 37].
The mitochondrial E3 ubiquitin ligase MARCH5 was identified as a protein of the mitochondrial outer membrane that interacts with Mfn2 and ubiquitinated forms of Drp1 [34]. Originally, it was proposed that ubiquitination by MARCH5 promotes the formation of long tubular mitochondria as a result of Mfn2-dependent fusion [34, 38]. However, later, an opposite functional outcome of MARCH5-induced Drp1 ubiquitination was demonstrated, suggesting that MARCH5 may support fission by facilitating the subcellular trafficking and recruitment of Drp1 to actual sites of mitochondrial division [35]. MARCH5-dependent ubiquitination of Mfn1 was significantly elevated under mitochondrial stress conditions and with an increase in acetylated Mfn1. Thus, it may reflect mitochondrial adaptation to stress and mitochondrial quality control [39].
Parkin functions as an E3 ubiquitin ligase and it translocates from the cytosol to damaged or dysfunctional mitochondria to promote their degradation by mitophagy [29, 40]. However, Parkin can also affect mitochondrial fusion/fission dynamics. In primary mouse neurons, downregulation of Parkin lead to an increase in mitochondrial fragmentation and a decrease in ATP production [41]. Normally, Parkin interacts with Drp1 leading to its ubiquitination and promoting its proteasome-dependent degradation [42]. This suggests downregulation of Parkin would decrease the proteasome-dependent degradation of Drp1, leading to an increase in mitochondrial fission. In contrary, another report showed that Parkin does not interact with Drp1 but promotes ubiquitination and consequent degradation of Mfn1 [29]. Both studies used genetic manipulation to alter the expression levels of Parkin and immunoprecipitation technique to show Drp1 interaction with Parkin. Wang et al. [42] presented positive Drp1 and Parkin interaction using 293 T cells, whereas a lack of Drp1 interaction with Parkin was shown in SH-SY5Y cells [29]. Thus, it seems there are other unknown factors that can affect the Parkin-dependent Drp1 ubiquitination and consequently the functional effect on mitochondrial dynamics. Further experiments are needed, preferentially carried out with primary neuronal cells, to shed more light on the effect of Parkin and Drp1 interaction and its impact on the mitochondrial fusion/fission equilibrium in brain cells.
There is also a complex interplay relationship between ubiquitination and phosphorylation. It was noted that Mfn2 can be phosphorylated by both PTEN-induced putative kinase 1 (PINK1) and c-Jun N-terminal kinase (JNK) under different stress conditions [43]. The phosphorylation on Mfn2 by JNK recruits ubiquitin ligase, Huwe1, triggering Mfn2 degradation and mitochondrial fragmentation, whereas phosphorylation of Mfn2 on the PINK1 site contributes to recruitment of Parkin to the mitochondria [44].
In cerebral ischemic insult models, it remains unclear how ubiquitination of Drp1, Fis1, and Mfn1/2 are altered. However, it is understood that in global cerebral ischemia, there is a general increase in ubiquitinated proteins in the brain [45, 46]. Under these conditions, ubiquitination of mitochondrial proteins are most likely affected, probing future studies in this area.
Drp1 Phosphorylation
Phosphorylation is a well-studied and characterized post-translational modification found typically on serine, threonine, or tyrosine residues. So far Drp1 is the only protein among fusion and fission proteins that was found to be regulated by phosphorylation. Two sites are phosphorylated on Drp1 (P-Drp1), Ser616 of human Drp1 isoform 1 (equivalent to Ser585 in rat Drp1 or ser579 in human Drp1 isoform 3), and Ser637 human Drp1 (equivalent to Ser600, 617, and 656, depending on species and splice variants), which upon phosphorylation usually exhibit opposing effects on Drp1 associated mitochondrial fragmentation. Protein kinase A (PKA) phosphorylates at Ser637 under conditions of nutrient starvation and leads to inhibition of fission [47]. In contrast, phosphorylation by Ca2+/camodulin-dependent protein kinase-1α (CaMK1α) or Rho-associated coiled-coil-containing protein kinase 1 (ROCK1) at the same serine residue increases Drp1 translocation to the mitochondria and enhances fission [48, 49] (Fig. 2). The calcium-dependent protein phosphatase, calcineurin (CaN), removes phosphate groups at the Ser637 site and promotes fission in the model of Huntington’s disease (HD) [50]. The specific pathological conditions and mechanisms leading to opposing functional outcome of phosphorylation at the same serine residue of the Drp1 remain so far elusive and need further investigation.
Modulation of mitochondrial dynamics by Drp1 phosphorylation. So far only Drp1 was identified from the proteins regulating fusion and fission as a target for phosphorylation. There are two serine residues that can be phosphorylated on the Drp1 protein: Ser616 (equivalent to Ser585/579 dependent on species and human Drp1 isoform 3) and Ser637 (equivalent to Ser600/617/656). Ser616 is phosphorylated by cyclin-dependent kinase 1 (CDK1) or protein kinase C δ (PKCδ), leading to Drp1 activated fission. So far, it is not known whether a specific phosphatase de-phosphorylates the Ser616 on Drp1. Ser637 can be phosphorylated by three kinases: ROCK1, CaMK1α, and PKA. Interestingly, although all these kinases phosphorylate the same serine residue, the functional outcome is different. Phosphorylation by the kinases ROCK1 and CaMK1α leads to mitochondrial fragmentation while PKA-induced phosphorylation of Ser637 leads to increased mitochondrial fusion due to inhibition of Drp1. This modification is reversed by calcium-dependent phosphatase calcineurin (CaN)
The cyclin-dependent kinase 1 (CDK1)-cyclin B complex phosphorylates Drp1 at Ser616. During mitosis, P-Drp1 (Ser616) enhances mitochondrial fragmentation and facilitates the proper distribution of mitochondrial mass into daughter cells [51]. Under oxidative stress conditions, protein kinase C δ (PKCδ), phosphorylates the same serine, resulting in increased mitochondrial fragmentation (Fig. 2) [52].
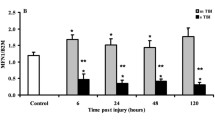
Ischemia and traumatic brain injury usually leads to an enhanced fragmented state of neuronal and glial mitochondria [53,54,55,56]. The model of focal cerebral ischemia induced by middle cerebral artery occlusion (MCAO) resulted in a progressive increase in P-Drp1 at site Ser637 reaching a peak at 2 days of recovery. At this recovery time point, there was increased co-localization of Drp1 and mitochondrial cytochrome oxidase suggesting an increase in mitochondrial fission mediated by CaMK1α [49]. However, mitochondrial fission was not quantified nor the phosphorylation of Ser616, which also regulates fission dynamics. Additionally, the global cerebral ischemic model exhibited enhanced mitochondrial fission but was mediated through the phosphorylation of Ser616 rather than Ser637 [53, 57].
Recently, it was suggested that the PTEN-induced putative kinase 1 (PINK1) could also affect the fusion/fission dynamics following ischemic insult [57]. There was an accumulation of PINK1 in the vulnerable CA1 sub-region of the hippocampus as well as an increase in P-Drp1 levels (Ser616, but not Ser637) following cerebral ischemic insult. Administration of PINK1-siRNA caused a further increase in P-Drp Ser616 and oxidative DNA damage [57]. The authors suggested that PINK1 could affect the activity of CDK1/cyclin B kinase and inhibit the fission process. However, PINK1 accumulation in post-cerebral ischemic tissue is probably due to excessive fission that leads to large number of small non-functional mitochondria [58] which triggers the mitophagy process. PINK1 recruits Parkin, an E3 ubiquitin ligase, whose activity leads to the ubiquitination of mitochondrial outer membrane proteins and triggers the removal of damaged mitochondria [35, 58, 59]. This process leads to decreased reactive oxygen species (ROS) production and reduction of oxidative damage to DNA. Thus, knocking down PINK1 can inhibit mitophagy and ultimately increase ROS production and P-Drp1 levels leading to more extensive post-ischemic fission. Thus, the increase in PINK1 levels is probably the result and not the cause of increased mitochondrial fission.
Nevertheless, it still remains unclear how under particular pathologic conditions mitochondria regulate which Drp1 serine residue (Ser616 or Ser637) is phosphorylated and for what duration of time. It is possible that the functional outcome of a particular Drp1 serine phosphorylation depends on other concomitant post-translational modification as SUMOylation or S-nitrosylation.
S-Nitrosylation
Nitric oxide (NO) is an important second messenger that is generated through the oxidation of l-arginine by nitric oxide synthases (NOS) in the presence of NADPH and oxygen, and is implicated in mechanisms of neuronal cell survival and death [55, 60]. NO represents a reactive nitrogen species (RNS) and signals primarily through formation of S-nitrosothiols (SNOs), representing S-nitrosylation [61]. Furthermore, NO reacts readily with superoxide generating highly reactive peroxynitrate, which can nitrate tyrosine residues to form nitrotyrosine adducts [61]. These modifications can alter protein structure and function, as well as affect protein aggregation. The cysteine residue (Cys644) of Drp1 can be S-nitrosylated resulting in increased Drp1 activity by its dimerization [5]. The ultimate outcome is extensive mitochondrial fission leading to neuronal damage. A mutation of Cys644 has been shown to prevent mitochondrial fragmentation and inhibit the neurotoxicity of NO [62]. However, these findings were challenged by another study showing S-nitrosylation of Drp1 had no impact on Drp1 oligomerization and did not affect its enzymatic activity [63]. Furthermore, it was postulated that there is interplay between S-nitrosylation and phosphorylation of Drp1 [63]. It was reported that Drp1 S-nitrosylation is a modification that is required for phosphorylation of Drp1 at Ser616 by PKCδ or CDK1 (Fig. 3). Thus, treatment of cells with an NO donor enhanced Drp1 phosphorylation at Ser616 resulting in increased translocation to the mitochondria and ultimately fragmentation [63]. Ischemic stroke and neurodegenerative diseases, such as Alzheimer’s, generate NO in excess, which results in increased RNS and S-nitrosylation modifications [64, 65].
S-nitrosylation-dependent modulation of mitochondrial dynamics. Nitric oxide (NO) generated by activated nitric oxide synthase (NOS) can form S-nitrosothiols (SNOs) on target proteins. Drp1 was shown to be modified by S-nitrosylation on cysteine residue (Cys644), leading to increased fragmentation of mitochondria. Additionally, later it was reported that the Drp1 S-nitrosylation is a modification that is required for phosphorylation of Drp1 at Ser616, which leads to activated fission. The NO-induced S-nitrosylation can be reversed by S-nitroglutathione reductase (GSNOR) in the presence of reduced glutathione (GSH) or by thioredoxin (Trx) reductase (TrxR). When NO reacts with another free radical, superoxide, a highly reactive peroxynitrate (ONOO) is generated that reacts with tyrosine residues generating 3-nitrotyrosine. Although mitochondrial proteins are affected by this modification, e.g., pyruvate dehydrogenase (PDH), currently there are no reports showing 3-nitrotyrosine modifications on proteins regulating mitochondrial fission or fusion
S-nitrosylation also regulates the protein activity of Parkin, an E3 ubiquitin ligase. This modification on Parkin abolishes its ubiquitin ligase activity and as a result has negative effects on the process of mitophagy. In addition, S-nitrosylation of Parkin can cause p53-mediated apoptosis in neuronal cells and may contribute to some idiopathic forms of Parkinson’s disease [66]. Consequently, under pathologic stress conditions, extensively fragmented mitochondria may have decreased quality control and degradation leading to an increase in free radical production and cellular damage.
Since NO-induced S-nitrosylation is considered a mechanism that regulates enzymatic activity, the removal of NO groups from cystein thiol (de-nitrosylation) acts as a control to this modification. This is an important but less studied process of NO-induced post-translational modifications. De-nitrosylation has been shown to be catalyzed by two enzymes in vivo (for review see [67, 68] ). These cellular systems were identified as physiological de-nitrosylases: the S-nitroglutathione reductase (GSNOR) system and the thioredoxin (Trx) system [67]. GSNOR is comprised from glutathione (GSH) and GSH-dependent formaldehyde dehydrogenase and class III alcohol dehydrogenase (ADH5). The Trx system is comprised of Trx and Trx reductase (TrxR) [68].
As mentioned above, excess production of NO can generate two different protein modifications: S-nitrosylation due to a reaction of NO with cysteine thiol groups and formation of 3-nitrotyrosine that is generated by the reaction of peroxynitrate with tyrosine residues [69]. Peroxynitrate is a product of NO and superoxide. Thus, the levels of NO depend not only on the activity of nitric oxide synthase (NOS) but also on the rate of superoxide generation that will “scavenge” NO and produce peroxynitrate. Interestingly, we found that following global cerebral ischemia, the 3-nitrotyrosine immunoreactivity was significantly higher in ischemia-resistant hippocampal sub-regions (CA3 and DG) where the mitochondria in neurons were able to refuse. In contrary, within the ischemia vulnerable CA1 neurons, with excessively fragmented mitochondria, the 3-nitrotyrosine immunoreactivity was significantly lower; suggesting higher levels of Drp1 S-nitrosylation, probably leading to permanently fragmented mitochondria [53]. It is still unclear whether 3-nitrotyrosine modifications play significant role in regulation of mitochondrial dynamics.
Acetylation
Acetylation of proteins is a common post-translational modification that has considerable impact on their activity and expression. Enzymatic acetylation of histones and non-histone proteins is dependent on the availability of acetyl CoA [70,71,72,73,74]. This modification is tightly regulated by two opposing families of enzymes, histone acetyltransferases (HATs) and histone deacetylases (HDACs).
Post-translational lysine acetylation of proteins is highly reversible. In humans, there are 18 potential enzymes that remove the acetyl group from lysine and are characterized into four classes: class I HDACs (HDACs 1,2,3 and 8), class II HDACs (HDACs 4,5,6,7,9 and 10), class III HDACs (sirtuin family: SIRT1-SIRT7), and class IV HDACs (HDACs 11) [75]. HDACs also possess substrate specificity and can deacetylate non-histone proteins [76, 77]. Sirtuins (SIRT1–7), the class III HDACs, require NAD+ for their catalytic activity and are known to deacetylate non-histone proteins [75, 78]. The cellular compartmentalization of SIRTs is diverse. SIRT1, SIRT6, and SIRT7 are predominantly nuclear proteins [79], SIRT2 is considered a cytosolic enzyme [80], and SIRT3–5 are localized to the mitochondria [81]. However, SIRT4 acts rather as an ADP-ribosyl transferase and not as a deacetylase [81]. Furthermore, it was shown that SIRT5 can act as a desuccinylase [82, 83] and also as a lysine deglutarylase [84]. However, so far these types of lysine residue modifications were not identified in proteins regulating mitochondrial dynamics.
HATs are broadly categorized into type A, nucleic HATs, or type B, cytoplasmic HATs [70, 71]. Type A HATs are transcription related and sub-classified into five families [77]. The cytoplasmic type B HATs are responsible for deposition-related acetylation of free histone substrates in the cytoplasm during the process of chromatin assembly [85].
Recently, it was reported that there is a mitochondria specific acetyltransferase, general control of amino acid synthesis 5-like 1 (GCN5L1), that counters the activity of mitochondrial deacetylase SIRT3 [86]. GCN5L1 promotes acetylation of SIRT3 respiratory chain targets and reverses global SIRT3 effects on mitochondrial protein acetylation [86]. GCN5L1 is a non-transmembrane globular protein located within mitochondria in either the intermembrane space or matrix-soluble fractions [86].
Interestingly, the level of mitochondrial protein acetylation, controlled by GCN5L1 and SIRT3, also affects the mitophagy process [87]. This mechanism is independent of the E3-ligase Parkin-mediated mitophagy. However, the mitochondrial targets that trigger this program were not identified. Since GCN5L1 is classified as an intra-mitochondrial protein, it is difficult to envision how the acetylation of an intra-mitochondrial protein is affecting the interaction between cytosolic mitophagy components and the outer mitochondrial membrane proteins. However, although not functionally characterized in autophagy, a cytosolic fraction of GCN5L1 (also named BLOC1 component BLOS1) has been shown to be part of a protein complex involved in protein transport to lysosomes [88]. These finding also support the hypothesis that mitochondrial protein lysine deacetylation enables lysine ubiquitination. Thus, acetyl transferases and ubiquitin ligases could compete for certain lysine residues of the target protein.
Under pathological stress, Opa1 is hyperacetylated and this post-translational modification reduces its GTPase activity. SIRT3 deacetylates Opa1 and re-activates this enzyme leading to increased mitochondrial fusion [8]. The acetylation status of Mfn1 is also crucial for mitochondria under stress conditions. Under metabolic stress induced by fasting (glucose removal), Mfn1 is deacetylated by HDAC6, which induces mitochondrial hyperfusion, an attempt to preserve structure [89]. HDAC6 deacetylates Mfn1 at lysine residue (K222), leading to increased Mfn1 activity toward fusion. Surprisingly, it was also shown that under mitochondrial stress conditions induced by exposing cells to antimycin A, a respiratory Complex III inhibitor, acetylated Mfn1 levels increase [39].
Interestingly, the acetylation at lysine residue K491 promoted the interaction of MARCH5 with Mfn1. As a result, MARCH5 binds to Mfn1 leading to its subsequent ubiquitination. Furthermore, it was reported that increased ubiquitination was dependent on increased acetylation of Mfn1 as well [39]. Ultimately, this resulted in Mfn1 degradation by the ubiquitin-proteasome mechanism. This system is an important quality control check for mitochondria under stress conditions. Thus, there are acetylation modifications of Mfn1 induced by mitochondrial stress that have opposing functional outcomes on the mitochondrial dynamics. Exactly how these two regulation states interact with one another under stress remains unclear and needs to be further examined.
Another example of the complex interplay between different post-translational protein modifications was reported by Verdone et al. [90]. A decrease in poly-ADP-ribosylation due to pharmacological inhibition of poly (ADP-ribose) polymerase (PARP) activity or by overexpressing poly-(ADP-ribose) glycohydrolase (PARG) leads to decrease of global histone H3 and H4 acetylation [90]. Since the global acetyltransferase activity did not changed, this suggests that poly-ADP-ribosylation has a role in the regulation of histone deacetylase activity [90].
HDAC inhibitors have neuroprotective, neurotrophic, and anti-inflammatory properties [91]. Following ischemic brain injury, reduced histone acetylation was found at lysine residues, which were restored with HDAC inhibitors resulting in neuroprotection [92,93,94,95,96]. Similarly, nicotinamide (Nam) that inhibits the NAD+-dependent deacetylases, sirtuins, [91], and PARP1 activity, also showed significant protection against acute brain damage (for review [78]).
Together, this data suggests that targeting acetylation statuses of mitochondrial fusion proteins and histones has the ability to alter mitochondrial dynamics and overall function. Therapeutically, this would represent an efficient approach for neuroprotection.
O-GlcNAcylation
O-linked N-acetyl-glucosamine glycosylation (O-GlcNAcylation) represents a dynamic modification of serine and threonine hydroxyl moieties on nuclear and cytoplasmic proteins by O-linked N-acetylglucosamine, termed O-β-GlcNAc or simply O-GlcNAc. Two enzymes regulate protein O-GlcNAcylation, O-GlcNAc-transferase catalyzes the addition of O-GlcNAc while N-acetyl-glucosaminidase (NAG) remove O-GlcNAc residues [97].
O-GlcNAc is particularly relevant to chronic diseases including diabetes, cardiovascular disease, neurodegenerative diseases, and cancer. O-GlcNAc cycles rapidly and the cycling rates are similar to those seen for protein phosphorylation. Interestingly, O-GlcNAcylation and phosphorylation sites overlap which results in opposing functions. O-GlcNAc and O-phosphate exhibit a complex interplay on signaling, transcriptional, and cytoskeletal regulatory proteins within the cell [97]. A shorter splice variant of O-GlcNAc-transferase has been identified that exhibits preferred mitochondrial localization [98, 99]. Increased O-GlcNAcylation of mitochondrial fusion protein Opa1 was observed in cells exposed to high glucose causing mitochondrial fragmentation and inhibition of Complex IV activity [100]. Furthermore, hyperglycemic conditions also increased O-GlcNAcylation of Drp1 protein [7]. An overall increase in O-GlcNAcylation actually decreased phosphorylation of Drp1 at Ser637 leading to increased GTP binding that allows for the translocation of Drp1 to the mitochondria [7]. It has been shown that various stress stimuli elevate global levels of O-GlcNAcylation, which can account for the increased mitochondrial fragmentation observed under these conditions [101]. O-GlcNAcylation thus represents another post-translational modification that contributes to regulation of mitochondrial dynamics. However, further research is needed to understand how this modification specifically plays a role in acute and neurodegenerative brain injury.
ADP-Ribosylation
ADP-ribosylation refers to the transfer of one or more ADP-ribose units from NAD+ onto target proteins as a post-translational modification. ADP-ribose groups can be attached either singularly (mono-ADP-ribose) or as multiples (poly-ADP-ribose chain) catalyzed by the poly-ADP-ribose polymerases (PARP) family [102, 103]. Several amino acids can be ribosylated such as glutamate, aspartate, lysine, arginine, and cysteine [104]. Several enzymes, depending on whether they cleave mono- or poly-ADP-ribose, can mediate cleavage of ADP-ribose. ADP-ribosylhydrolase 1 (ARH1) removes single ADP-ribose groups from conjugated amino acids while ARH3 cleaves the ribose-ribose bond between ADP-ribose subunits in poly-ADP-ribose [105]. Poly-ADP-ribose glycohydrolase (PARG) is also responsible for cleaving ribose-ribose bonds between subunits. Another set of ADP-ribosylhydrolases, MacroD1, MacroD2, and TARG1 are responsible for removing remaining ADP-ribose units from polymer chains as well as single ADP-ribose groups that are conjugated to acidic amino acid residues [105]. As a result, this modification has diverse effects on protein stability/activity.
Immunoprecipitation and mass spectrometry identified mitochondrial fusion proteins Opa1 and Mfn1/2 to be poly-ADP-ribosylated [106, 107]. Mass spectrometry also recognized mitochondrial fission protein Drp1 to be ADP-ribosylated [108]. It remains unclear which specific PARP ADP-ribosylates these proteins; however, PARP1 has been suggested to be localized to the mitochondria, which could be responsible for ribosylation of these proteins [109, 110]. Removal of these ADP-ribose units is possibly mediated by mitochondrial localized ARH3 [111]. Although these proteins have been identified as ADP-ribosylated, it remains unclear how this alters functionality or activity. Post-ischemic injury shows an increase in poly-ADP-ribose levels in the hippocampus, which could drive the increase of this modification on these proteins [112]. However, further research is needed to understand how this modification specifically plays a role in acute and neurodegenerative brain injury.
Proteolytic Cleavage
Proteolysis is a modification involving the breakdown of proteins into smaller polypeptides or amino acids. This modification varies from the modifications mentioned above mainly due to its irreversibility. Cleavage of proteins can result in inactivation, activation, or even altered protein function [113]. Among the proteins regulating mitochondrial fusion, Opa1 activity is directly regulated by proteolytic cleavage. Thus, Opa1 fusogenic ability is modulated by proteolytic processing and depends on the interaction of both the long (non-cleaved) and short, cleaved forms [114,115,116].
Opa1 was demonstrated to control both mitochondrial fusion and cristae morphology [114, 117,118,119,120,121,122]. This protein is localized in the mitochondrial intermembrane space in soluble forms or is attached to the inner mitochondrial membrane [114, 123]. After being imported into the mitochondria, the mitochondrial targeting sequence is removed to produce a long isoform of Opa1 embedded in the inner membrane. At steady state, about half of Opa1 exists as the long form, with the remainder cleaved to create short forms that are no longer membrane anchored [114]. Under normal conditions, proteolytic cleavage of long isoforms of Opa1 results in the balanced accumulation of long and short Opa1 forms [114, 122]. Long isoforms are crucial for Opa1-mediated mitochondrial fusion while short isoforms are unable to fuse mitochondria [124, 125].
Prohibitins, membrane scaffolds, are required for long Opa1 stability and are essential for the formation and maintenance of mitochondrial structure [126]. A recent study demonstrated a marked increase in Opa1 cleavage by the lack of Prohibitin 2 (Phb2) [121]. Furthermore, overexpression of prohibitin by viral gene transfection protected hippocampal CA1 neurons from cerebral ischemic insult [127].
Two proteolytic cleavage sites in the primary sequence of Opa1 have been identified (S1 and S2) [125]. Two peptidases, m-AAA (mitochondrial matrix oriented) OMA1 and the i-AAA (intermembrane space oriented) protease YME1L, cleave Opa1 at S1 and S2, respectively [116, 125, 128]. YME1L is responsible for cleavage of S2 under basal conditions [115]. OMA1 is activated upon various stress insults, resulting in the complete degradation of long Opa1 and leading to mitochondrial fragmentation [129, 130]. The third protease that was identified to cleave Opa1 was the presenilin-associated rhomboid-like protease (PARL) [125, 131,132,133,134]. The main role of PARL is the generation of a soluble Opa1 isoform detected in the intermembrane space (IMS), which represents 4% of total IMS Opa1 in mitochondria [131, 133]. This soluble Opa1 isoform controls the shape of mitochondrial cristae, independently of its role in mitochondrial fusion.
The focal ischemia model, induced by middle cerebral artery occlusion (MCAO), shows an increase in the long form of Opa1 lasting a few days after insult [49]. Increased Opa1 cleavage and excessive mitochondrial fragmentation was also observed following global cerebral ischemia [53, 56] and neonatal hypoxic-ischemic brain injury [135]. Similarly, there was a cessation of mitochondrial fusion, mitochondrial cristae dilation and reduction of Opa1 levels in a model of excitotoxicity due to increased glutamate release, which is common in stroke, trauma, and neurodegenerative diseases [136]. Overexpressing Opa1 reversed these pathologic changes and increased neuronal survival following excitotoxic stress [136]. As mentioned above, Opa1 activity is also regulated by acetylation and ADP-ribosylation. All these post-translational modifications of Opa1 can ultimately alter mitochondrial morphology and function.
Transcriptional Control
Cells can also alter protein levels via post-transcriptional regulation of gene expression. MicroRNA (miRNA) are small non-coding RNAs that bind to mRNA and silence mRNA usually by initiating its cleavage. Thus, miRNAs are a new class of regulatory RNA molecules whose primary function is to downregulate gene expression. A primary transcript (pri-miRNA) is synthesized from nuclear DNA by RNA polymerase II and then processed by nucleases DROSHA and DGCR8/PASHA. The resulting molecule (pre-miRNA) is transported to the cytoplasm where it is further processed by the nuclease DICER and forms a complex with RNA-inducing silencing complex (RISC) [137]. This complex binds mRNAs by imperfect base pairing and ultimately represses translation [138].
Several miRNAs have been reported to either directly or indirectly regulate mitochondrial fusion and fission proteins. MiRNA-499 regulates calcineurin expression, which is responsible for de-phosphorylation of Drp1. Ischemia/reperfusion (I/R) injury resulted in a downregulation of miRNA-499 which increased calcineurin expression. This resulted in elevated mitochondrial fission due to Drp1 availability at the mitochondrial membrane [139]. MiR-761 targets Mff and is also downregulated in I/R injury, which drives an increase in mitochondrial fission. Delivery of miR-761 rescued fragmented mitochondria in I/R injury [140]. Fis1 expression is directly regulated by miR-484. Anoxic conditions drive increased mitochondrial fission due to decreased miR-484 and elevated Fis1 levels [141]. Fusion protein, Mfn1, is directly targeted by miR-140. Treatment of cardiomyocytes with hydrogen peroxide increases miR-140 levels and reduces Mfn1 expression resulting in fragmented mitochondria [142]. This data suggests that manipulating levels of miRNAs targeting fusion/fission proteins could be used as a therapeutic tool to shift the balance of mitochondrial dynamics in stress or pathological conditions.
Conclusions
Alterations in mitochondrial dynamics are intimately related to mitochondrial function and cellular requirements. Published data suggests the main function of mitochondrial dynamics is to ensure proper inheritance and distribution of mitochondria and to maintain a healthy state. Although the key players regulating mammalian mitochondrial fusion and fission have been identified, their coordination and pathophysiological implications of perturbation in these processes remain poorly understood.
Post-translational protein modifications are important for the spatial and temporal regulation of their function. Under stress or pathologic conditions, several modifications are activated that show complex interactions yielding to a particular functional outcome associated with adaptation of the cellular mitochondrial network to the changing environment (Fig. 4).
Overview of post-translational modifications on mitochondrial proteins that regulate mitochondrial fission and fusion. a Mitochondrial fission is driven by removal of SUMO2/3 as well as the conjugation of SUMO1 to Drp1. Additionally, phosphorylation at serine 616 by CDK1/PKCδ and serine 637 by ROCK1/CaMK1α leads to increased fission of mitochondria. Other modifications such as S-nitrosylation and O-GlcNAcylation of Drp1 and Opa1 additionally drive fragmentation. Ubiquitination of Mfn1/2 leads to proteasomal degradation, which results in decreased fusion. Additionally, acetylated Mfn1/2 and Opa1 drive an increase in mitochondrial fission. Proteolytic cleavage of Opa1 produces short forms of Opa1 that are unable to fuse inner membranes of mitochondria. Together these modifications can alter availability of Drp1 at the mitochondrial outer membrane or alter protein stability/function, which results in a shift to favor mitochondrial fragmentation. b Post-translational modifications shifting mitochondrial dynamics toward fusion. Conjugation of Drp1 to SUMO2/3 and removal of SUMO1 both shift the dynamic toward enhanced mitochondrial fusion. Phosphorylation of serine 637 by PKA drives a similar response. Drp1 and Fis1 can also be proteasomally degraded after ubiquitination, which decreases fragmentation
A significant or persistent perturbation in the complex regulatory machinery of the mitochondrial dynamics can lead to pathophysiological consequences and cell death. A better understanding of these regulatory mechanisms related to post-translational modifications can likely lead to the development of new therapeutic agents to prevent and treat mitochondria-related neurodegenerative disease. Thus, future studies will need to determine which alterations or combinations of post-translational modifications are significant contributors to pathophysiology of a particular stress or disease. Due to the complexity and synergistic nature of these modifications, it is feasible to assume that several targets will need to be considered for pharmaceutical intervention to achieve a significant therapeutic effect.
References
Ni HM, Williams JA, Ding WX. Mitochondrial dynamics and mitochondrial quality control. Redox Biol. 2015;4:6–13. https://doi.org/10.1016/j.redox.2014.11.006.
Westermann B. Mitochondrial fusion and fission in cell life and death. Nat Rev Mol Cell Biol. 2010;11(12):872–84. https://doi.org/10.1038/nrm3013.
Youle RJ, van der Bliek AM. Mitochondrial fission, fusion, and stress. Science. 2012;337(6098):1062–5. https://doi.org/10.1126/science.1219855.
Anderson CA, Blackstone C. SUMO wrestling with Drp1 at mitochondria. EMBO J. 2013;32(11):1496–8. https://doi.org/10.1038/emboj.2013.103.
Chen H, Chan DC. Mitochondrial dynamics—fusion, fission, movement, and mitophagy—in neurodegenerative diseases. Hum Mol Genet. 2009;18(R2):R169–76. https://doi.org/10.1093/hmg/ddp326.
Wilson TJ, Slupe AM, Strack S. Cell signaling and mitochondrial dynamics: implications for neuronal function and neurodegenerative disease. Neurobiol Dis. 2013;51:13–26. https://doi.org/10.1016/j.nbd.2012.01.009.
Gawlowski T, Suarez J, Scott B, Torres-Gonzalez M, Wang H, Schwappacher R, et al. Modulation of dynamin-related protein 1 (DRP1) function by increased O-linked-beta-N-acetylglucosamine modification (O-GlcNAc) in cardiac myocytes. J Biol Chem. 2012;287(35):30024–34. https://doi.org/10.1074/jbc.M112.390682.
Samant SA, Zhang HJ, Hong Z, Pillai VB, Sundaresan NR, Wolfgeher D, et al. SIRT3 deacetylates and activates OPA1 to regulate mitochondrial dynamics during stress. Mol Cell Biol. 2014;34(5):807–19. https://doi.org/10.1128/MCB.01483-13.
Wilkinson KA, Nakamura Y, Henley JM. Targets and consequences of protein SUMOylation in neurons. Brain Res Rev. 2010;64(1):195–212. https://doi.org/10.1016/j.brainresrev.2010.04.002.
Yang W, Paschen W. SUMO proteomics to decipher the SUMO-modified proteome regulated by various diseases. Proteomics. 2015;15(5–6):1181–91. https://doi.org/10.1002/pmic.201400298.
Mahajan R, Delphin C, Guan T, Gerace L, Melchior F. A small ubiquitin-related polypeptide involved in targeting RanGAP1 to nuclear pore complex protein RanBP2. Cell. 1997;88(1):97–107.
Wei W, Yang P, Pang J, Zhang S, Wang Y, Wang MH, et al. A stress-dependent SUMO4 sumoylation of its substrate proteins. Biochem Biophys Res Commun. 2008;375(3):454–9. https://doi.org/10.1016/j.bbrc.2008.08.028.
Braschi E, Zunino R, McBride HM. MAPL is a new mitochondrial SUMO E3 ligase that regulates mitochondrial fission. EMBO Rep. 2009;10(7):748–54. https://doi.org/10.1038/embor.2009.86.
Martin S, Wilkinson KA, Nishimune A, Henley JM. Emerging extranuclear roles of protein SUMOylation in neuronal function and dysfunction. Nat Rev Neurosci. 2007;8(12):948–59. https://doi.org/10.1038/nrn2276.
Gareau JR, Lima CD. The SUMO pathway: emerging mechanisms that shape specificity, conjugation and recognition. Nat Rev Mol Cell Biol. 2010;11(12):861–71. https://doi.org/10.1038/nrm3011.
van der Veen AG, Ploegh HL. Ubiquitin-like proteins. Annu Rev Biochem. 2012;81:323–57. https://doi.org/10.1146/annurev-biochem-093010-153308.
Lee YJ, Miyake S, Wakita H, McMullen DC, Azuma Y, Auh S, et al. Protein SUMOylation is massively increased in hibernation torpor and is critical for the cytoprotection provided by ischemic preconditioning and hypothermia in SHSY5Y cells. J Cereb Blood Flow Metab. 2007;27(5):950–62. https://doi.org/10.1038/sj.jcbfm.9600395.
Hochrainer K, Jackman K, Benakis C, Anrather J, Iadecola C. SUMO2/3 is associated with ubiquitinated protein aggregates in the mouse neocortex after middle cerebral artery occlusion. J Cereb Blood Flow Metab. 2015;35(1):1–5. https://doi.org/10.1038/jcbfm.2014.180.
Cimarosti H, Lindberg C, Bomholt SF, Ronn LCB, Henley JM. Increased protein SUMOylation following focal cerebral ischemia. Neuropharmacology. 2008;54(2):280–9. https://doi.org/10.1016/j.neuropharm.2007.09.010.
Yang W, Sheng H, Warner DS, Paschen W. Transient focal cerebral ischemia induces a dramatic activation of small ubiquitin-like modifier conjugation. J Cereb Blood Flow Metab. 2008;28(5):892–6. https://doi.org/10.1038/sj.jcbfm.9600601.
Yang W, Sheng H, Thompson JW, Zhao S, Wang L, Miao P, et al. Small ubiquitin-like modifier 3-modified proteome regulated by brain ischemia in novel small ubiquitin-like modifier transgenic mice: putative protective proteins/pathways. Stroke. 2014;45(4):1115–22. https://doi.org/10.1161/STROKEAHA.113.004315.
Harder Z, Zunino R, McBride H. Sumo1 conjugates mitochondrial substrates and participates in mitochondrial fission. Curr Biol. 2004;14(4):340–5. https://doi.org/10.1016/j.cub.2004.02.004.
Zunino R, Schauss A, Rippstein P, Andrade-Navarro M, McBride HM. The SUMO protease SENP5 is required to maintain mitochondrial morphology and function. J Cell Sci. 2007;120(Pt 7):1178–88. https://doi.org/10.1242/jcs.03418.
Wasiak S, Zunino R, McBride HM. Bax/Bak promote sumoylation of DRP1 and its stable association with mitochondria during apoptotic cell death. J Cell Biol. 2007;177(3):439–50. https://doi.org/10.1083/jcb.200610042.
Zunino R, Braschi E, Xu L, McBride HM. Translocation of SenP5 from the nucleoli to the mitochondria modulates DRP1-dependent fission during mitosis. J Biol Chem. 2009;284(26):17783–95. https://doi.org/10.1074/jbc.M901902200.
Fu J, Yu HM, Chiu SY, Mirando AJ, Maruyama EO, Cheng JG, et al. Disruption of SUMO-specific protease 2 induces mitochondria mediated neurodegeneration. PLoS Genet. 2014;10(10):e1004579. https://doi.org/10.1371/journal.pgen.1004579.
Guo C, Hildick KL, Luo J, Dearden L, Wilkinson KA, Henley JM. SENP3-mediated deSUMOylation of dynamin-related protein 1 promotes cell death following ischaemia. EMBO J. 2013;32(11):1514–28. https://doi.org/10.1038/emboj.2013.65.
Wilkinson KA, Henley JM. Mechanisms, regulation and consequences of protein SUMOylation. Biochem J. 2010;428(2):133–45. https://doi.org/10.1042/BJ20100158.
Glauser L, Sonnay S, Stafa K, Moore DJ. Parkin promotes the ubiquitination and degradation of the mitochondrial fusion factor mitofusin 1. J Neurochem. 2011;118(4):636–45. https://doi.org/10.1111/j.1471-4159.2011.07318.x.
Nunez-O'Mara A, Berra E. Deciphering the emerging role of SUMO conjugation in the hypoxia-signaling cascade. Biol Chem. 2013;394(4):459–69. https://doi.org/10.1515/hsz-2012-0319.
Formentini L, Macchiarulo A, Cipriani G, Camaioni E, Rapizzi E, Pellicciari R, et al. Poly(ADP-ribose) catabolism triggers AMP-dependent mitochondrial energy failure. J Biol Chem. 2009;284(26):17668–76. https://doi.org/10.1074/jbc.M109.002931.
Lapidus RG, Sokolove PM. The mitochondrial permeability transition. Interactions of spermine, ADP, and inorganic phosphate. J Biol Chem. 1994;269(29):18931–6.
Wojcik C, Di Napoli M. Ubiquitin-proteasome system and proteasome inhibition: new strategies in stroke therapy. Stroke. 2004;35(6):1506–18. https://doi.org/10.1161/01.STR.0000126891.93919.4e.
Nakamura N, Kimura Y, Tokuda M, Honda S, Hirose S. MARCH-V is a novel mitofusin 2- and Drp1-binding protein able to change mitochondrial morphology. EMBO Rep. 2006;7(10):1019–22. https://doi.org/10.1038/sj.embor.7400790.
Karbowski M, Neutzner A, Youle RJ. The mitochondrial E3 ubiquitin ligase MARCH5 is required for Drp1 dependent mitochondrial division. J Cell Biol. 2007;178(1):71–84. https://doi.org/10.1083/jcb.200611064.
Buhlman L, Damiano M, Bertolin G, Ferrando-Miguel R, Lombes A, Brice A, et al. Functional interplay between Parkin and Drp1 in mitochondrial fission and clearance. Biochim Biophys Acta. 2014;1843(9):2012–26. https://doi.org/10.1016/j.bbamcr.2014.05.012.
Zhang Q, Wu J, Wu R, Ma J, Du G, Jiao R, et al. DJ-1 promotes the proteasomal degradation of Fis1: implications of DJ-1 in neuronal protection. Biochem J. 2012;447(2):261–9. https://doi.org/10.1042/BJ20120598.
Yonashiro R, Ishido S, Kyo S, Fukuda T, Goto E, Matsuki Y, et al. A novel mitochondrial ubiquitin ligase plays a critical role in mitochondrial dynamics. EMBO J. 2006;25(15):3618–26. https://doi.org/10.1038/sj.emboj.7601249.
Park YY, Nguyen OT, Kang H, Cho H. MARCH5-mediated quality control on acetylated Mfn1 facilitates mitochondrial homeostasis and cell survival. Cell Death Dis. 2014;5:e1172. https://doi.org/10.1038/cddis.2014.142.
Narendra D, Tanaka A, Suen DF, Youle RJ. Parkin is recruited selectively to impaired mitochondria and promotes their autophagy. J Cell Biol. 2008;183(5):795–803. https://doi.org/10.1083/jcb.200809125.
Lutz AK, Exner N, Fett ME, Schlehe JS, Kloos K, Lammermann K, et al. Loss of parkin or PINK1 function increases Drp1-dependent mitochondrial fragmentation. J Biol Chem. 2009;284(34):22938–51. https://doi.org/10.1074/jbc.M109.035774.
Wang H, Song P, Du L, Tian W, Yue W, Liu M, et al. Parkin ubiquitinates Drp1 for proteasome-dependent degradation: implication of dysregulated mitochondrial dynamics in Parkinson disease. J Biol Chem. 2011;286(13):11649–58. https://doi.org/10.1074/jbc.M110.144238.
Leboucher GP, Tsai YC, Yang M, Shaw KC, Zhou M, Veenstra TD, et al. Stress-induced phosphorylation and proteasomal degradation of mitofusin 2 facilitates mitochondrial fragmentation and apoptosis. Mol Cell. 2012;47(4):547–57. https://doi.org/10.1016/j.molcel.2012.05.041.
Chen Y, Dorn GW II. PINK1-phosphorylated mitofusin 2 is a Parkin receptor for culling damaged mitochondria. Science. 2013;340(6131):471–5. https://doi.org/10.1126/science.1231031.
Liu CL, Martone ME, Hu BR. Protein ubiquitination in postsynaptic densities after transient cerebral ischemia. J Cereb Blood Flow Metab. 2004;24(11):1219–25. https://doi.org/10.1097/01.WCB.0000136706.77918.21.
Hochrainer K, Jackman K, Anrather J, Iadecola C. Reperfusion rather than ischemia drives the formation of ubiquitin aggregates after middle cerebral artery occlusion. Stroke. 2012;43(8):2229–35. https://doi.org/10.1161/STROKEAHA.112.650416.
Rambold AS, Kostelecky B, Elia N, Lippincott-Schwartz J. Tubular network formation protects mitochondria from autophagosomal degradation during nutrient starvation. Proc Natl Acad Sci U S A. 2011;108(25):10190–5. https://doi.org/10.1073/pnas.1107402108.
Han XJ, Lu YF, Li SA, Kaitsuka T, Sato Y, Tomizawa K, et al. CaM kinase I alpha-induced phosphorylation of Drp1 regulates mitochondrial morphology. J Cell Biol. 2008;182(3):573–85. https://doi.org/10.1083/jcb.200802164.
Liu W, Tian F, Kurata T, Morimoto N, Abe K. Dynamic changes of mitochondrial fusion and fission proteins after transient cerebral ischemia in mice. J Neurosci Res. 2012;90(6):1183–9. https://doi.org/10.1002/jnr.23016.
Cribbs JT, Strack S. Reversible phosphorylation of Drp1 by cyclic AMP-dependent protein kinase and calcineurin regulates mitochondrial fission and cell death. EMBO Rep. 2007;8(10):939–44. https://doi.org/10.1038/sj.embor.7401062.
Taguchi N, Ishihara N, Jofuku A, Oka T, Mihara K. Mitotic phosphorylation of dynamin-related GTPase Drp1 participates in mitochondrial fission. J Biol Chem. 2007;282(15):11521–9. https://doi.org/10.1074/jbc.M607279200.
Qi X, Disatnik MH, Shen N, Sobel RA, Mochly-Rosen D. Aberrant mitochondrial fission in neurons induced by protein kinase C{delta} under oxidative stress conditions in vivo. Mol Biol Cell. 2011;22(2):256–65. https://doi.org/10.1091/mbc.E10-06-0551.
Owens K, Park JH, Gourley S, Jones H, Kristian T. Mitochondrial dynamics: cell-type and hippocampal region specific changes following global cerebral ischemia. J Bioenerg Biomembr. 2015;47(1–2):13–31. https://doi.org/10.1007/s10863-014-9575-7.
Zhao YX, Cui M, Chen SF, Dong Q, Liu XY. Amelioration of ischemic mitochondrial injury and Bax-dependent outer membrane permeabilization by Mdivi-1. CNS Neurosci Ther. 2014;20(6):528–38. https://doi.org/10.1111/cns.12266.
Barsoum MJ, Yuan H, Gerencser AA, Liot G, Kushnareva Y, Graber S, et al. Nitric oxide-induced mitochondrial fission is regulated by dynamin-related GTPases in neurons. EMBO J. 2006;25(16):3900–11.
Kumar R, Bukowski MJ, Wider JM, Reynolds CA, Calo L, Lepore B, et al. Mitochondrial dynamics following global cerebral ischemia. Mol Cell Neurosci. 2016; https://doi.org/10.1016/j.mcn.2016.08.010.
Chen SD, Lin TK, Yang DI, Lee SY, Shaw FZ, Liou CW, et al. Roles of PTEN-induced putative kinase 1 and dynamin-related protein 1 in transient global ischemia-induced hippocampal neuronal injury. Biochem Biophys Res Commun. 2015;460(2):397–403. https://doi.org/10.1016/j.bbrc.2015.03.045.
Jin SM, Youle RJ. PINK1- and Parkin-mediated mitophagy at a glance. J Cell Sci. 2012;125(Pt 4):795–9. https://doi.org/10.1242/jcs.093849.
Geisler S, Holmstrom KM, Skujat D, Fiesel FC, Rothfuss OC, Kahle PJ, et al. PINK1/Parkin-mediated mitophagy is dependent on VDAC1 and p62/SQSTM1. Nat Cell Biol. 2010;12(2):119–31. https://doi.org/10.1038/ncb2012.
Brown GC. Nitric oxide and neuronal death. Nitric Oxide. 2010;23(3):153–65. https://doi.org/10.1016/j.niox.2010.06.001.
Nakamura T, Lipton SA. Protein S-nitrosylation as a therapeutic target for neurodegenerative diseases. Trends Pharmacol Sci. 2016;37(1):73–84. https://doi.org/10.1016/j.tips.2015.10.002.
Cho DH, Nakamura T, Fang J, Cieplak P, Godzik A, Gu Z, et al. S-nitrosylation of Drp1 mediates beta-amyloid-related mitochondrial fission and neuronal injury. Science. 2009;324(5923):102–5. https://doi.org/10.1126/science.1171091.
Bossy B, Petrilli A, Klinglmayr E, Chen J, Lutz-Meindl U, Knott AB, et al. S-Nitrosylation of DRP1 does not affect enzymatic activity and is not specific to Alzheimer’s disease. J Alzheimers Dis. 2010;20(Suppl 2):S513–26. https://doi.org/10.3233/JAD-2010-100552.
Garcia-Bonilla L, Moore JM, Racchumi G, Zhou P, Butler JM, Iadecola C, et al. Inducible nitric oxide synthase in neutrophils and endothelium contributes to ischemic brain injury in mice. J Immunol. 2014;193(5):2531–7. https://doi.org/10.4049/jimmunol.1400918.
Butterfield DA, Di Domenico F, Swomley AM, Head E, Perluigi M. Redox proteomics analysis to decipher the neurobiology of Alzheimer-like neurodegeneration: overlaps in Down’s syndrome and Alzheimer’s disease brain. Biochem J. 2014;463(2):177–89. https://doi.org/10.1042/BJ20140772.
Sunico CR, Nakamura T, Rockenstein E, Mante M, Adame A, Chan SF, et al. S-Nitrosylation of parkin as a novel regulator of p53-mediated neuronal cell death in sporadic Parkinson's disease. Mol Neurodegener. 2013;8:29. https://doi.org/10.1186/1750-1326-8-29.
Nakamura T, Lipton SA. Emerging role of protein-protein transnitrosylation in cell signaling pathways. Antioxid Redox Signal. 2013;18(3):239–49. https://doi.org/10.1089/ars.2012.4703.
Benhar M, Forrester MT, Stamler JS. Protein denitrosylation: enzymatic mechanisms and cellular functions. Nat Rev Mol Cell Biol. 2009;10(10):721–32. https://doi.org/10.1038/nrm2764.
Morris G, Berk M, Klein H, Walder K, Galecki P, Maes M. Nitrosative stress, hypernitrosylation, and autoimmune responses to nitrosylated proteins: new pathways in neuroprogressive disorders including depression and chronic fatigue syndrome. Mol Neurobiol. 2016; https://doi.org/10.1007/s12035-016-9975-2.
Marmorstein R, Trievel RC. Histone modifying enzymes: structures, mechanisms, and specificities. Biochim Biophys Acta. 2009;1789(1):58–68. https://doi.org/10.1016/j.bbagrm.2008.07.009.
Roth SY, Denu JM, Allis CD. Histone acetyltransferases. Annu Rev Biochem. 2001;70:81–120. https://doi.org/10.1146/annurev.biochem.70.1.81.
Lee KK, Workman JL. Histone acetyltransferase complexes: one size doesn’t fit all. Nat Rev Mol Cell Biol. 2007;8(4):284–95. https://doi.org/10.1038/nrm2145.
Kouzarides T. Acetylation: a regulatory modification to rival phosphorylation? EMBO J. 2000;19(6):1176–9. https://doi.org/10.1093/emboj/19.6.1176.
Norvell A, McMahon SB. Cell biology. Rise of the rival. Science. 2010;327(5968):964–5. https://doi.org/10.1126/science.1187159.
Yoon S, Eom GH. HDAC and HDAC inhibitor: from cancer to cardiovascular diseases. Chonnam Med J. 2016;52(1):1–11. https://doi.org/10.4068/cmj.2016.52.1.1.
Glozak MA, Sengupta N, Zhang X, Seto E. Acetylation and deacetylation of non-histone proteins. Gene. 2005;363:15–23. https://doi.org/10.1016/j.gene.2005.09.010.
Wang Y, Miao X, Liu Y, Li F, Liu Q, Sun J, et al. Dysregulation of histone acetyltransferases and deacetylases in cardiovascular diseases. Oxidative Med Cell Longev. 2014;2014:641979. https://doi.org/10.1155/2014/641979.
Owens K, Park JH, Schuh R, Kristian T. Mitochondrial dysfunction and NAD+ metabolism alterations in the pathophysiology of acute brain injury. Transl Stroke Res. 2013;4:618–34.
Michishita E, Park JY, Burneskis JM, Barrett JC, Horikawa I. Evolutionarily conserved and nonconserved cellular localizations and functions of human SIRT proteins. Mol Biol Cell. 2005;16(10):4623–35. https://doi.org/10.1091/mbc.E05-01-0033.
Jing E, Gesta S, Kahn CR. SIRT2 regulates adipocyte differentiation through FoxO1 acetylation/deacetylation. Cell Metab. 2007;6(2):105–14. https://doi.org/10.1016/j.cmet.2007.07.003.
Morris KC, Lin HW, Thompson JW, Perez-Pinzon MA. Pathways for ischemic cytoprotection: role of sirtuins in caloric restriction, resveratrol, and ischemic preconditioning. J Cereb Blood Flow Metab. 2011;31(4):1003–19. https://doi.org/10.1038/jcbfm.2010.229.
Rardin MJ, He W, Nishida Y, Newman JC, Carrico C, Danielson SR, et al. SIRT5 regulates the mitochondrial lysine succinylome and metabolic networks. Cell Metab. 2013;18(6):920–33. https://doi.org/10.1016/j.cmet.2013.11.013.
Park J, Chen Y, Tishkoff DX, Peng C, Tan M, Dai L, et al. SIRT5-mediated lysine desuccinylation impacts diverse metabolic pathways. Mol Cell. 2013;50(6):919–30. https://doi.org/10.1016/j.molcel.2013.06.001.
Tan M, Peng C, Anderson KA, Chhoy P, Xie Z, Dai L, et al. Lysine glutarylation is a protein posttranslational modification regulated by SIRT5. Cell Metab. 2014;19(4):605–17. https://doi.org/10.1016/j.cmet.2014.03.014.
Parthun MR. Hat1: the emerging cellular roles of a type B histone acetyltransferase. Oncogene. 2007;26(37):5319–28. https://doi.org/10.1038/sj.onc.1210602.
Scott I, Webster BR, Li JH, Sack MN. Identification of a molecular component of the mitochondrial acetyltransferase programme: a novel role for GCN5L1. Biochem J. 2012;443(3):655–61. https://doi.org/10.1042/BJ20120118.
Webster BR, Scott I, Han K, Li JH, Lu Z, Stevens MV, et al. Restricted mitochondrial protein acetylation initiates mitochondrial autophagy. J Cell Sci. 2013;126(Pt 21):4843–9. https://doi.org/10.1242/jcs.131300.
Starcevic M, Dell'Angelica EC. Identification of snapin and three novel proteins (BLOS1, BLOS2, and BLOS3/reduced pigmentation) as subunits of biogenesis of lysosome-related organelles complex-1 (BLOC-1). J Biol Chem. 2004;279(27):28393–401. https://doi.org/10.1074/jbc.M402513200.
Lee JY, Kapur M, Li M, Choi MC, Choi S, Kim HJ, et al. MFN1 deacetylation activates adaptive mitochondrial fusion and protects metabolically challenged mitochondria. J Cell Sci. 2014;127(Pt 22):4954–63. https://doi.org/10.1242/jcs.157321.
Verdone L, La Fortezza M, Ciccarone F, Caiafa P, Zampieri M, Caserta M. Poly(ADP-ribosyl)ation affects histone acetylation and transcription. PLoS One. 2015;10(12):e0144287. https://doi.org/10.1371/journal.pone.0144287.
Chuang DM, Leng Y, Marinova Z, Kim HJ, Chiu CT. Multiple roles of HDAC inhibition in neurodegenerative conditions. Trends Neurosci. 2009;32(11):591–601. https://doi.org/10.1016/j.tins.2009.06.002.
Ren M, Leng Y, Jeong M, Leeds PR, Chuang DM. Valproic acid reduces brain damage induced by transient focal cerebral ischemia in rats: potential roles of histone deacetylase inhibition and heat shock protein induction. J Neurochem. 2004;89(6):1358–67. https://doi.org/10.1111/j.1471-4159.2004.02406.x.
Kim HJ, Rowe M, Ren M, Hong JS, Chen PS, Chuang DM. Histone deacetylase inhibitors exhibit anti-inflammatory and neuroprotective effects in a rat permanent ischemic model of stroke: multiple mechanisms of action. J Pharmacol Exp Ther. 2007;321(3):892–901. https://doi.org/10.1124/jpet.107.120188.
Faraco G, Pancani T, Formentini L, Mascagni P, Fossati G, Leoni F, et al. Pharmacological inhibition of histone deacetylases by suberoylanilide hydroxamic acid specifically alters gene expression and reduces ischemic injury in the mouse brain. Mol Pharmacol. 2006;70(6):1876–84. https://doi.org/10.1124/mol.106.027912.
Meisel A, Harms C, Yildirim F, Bosel J, Kronenberg G, Harms U, et al. Inhibition of histone deacetylation protects wild-type but not gelsolin-deficient neurons from oxygen/glucose deprivation. J Neurochem. 2006;98(4):1019–31. https://doi.org/10.1111/j.1471-4159.2006.04016.x.
Yildirim F, Gertz K, Kronenberg G, Harms C, Fink KB, Meisel A, et al. Inhibition of histone deacetylation protects wildtype but not gelsolin-deficient mice from ischemic brain injury. Exp Neurol. 2008;210(2):531–42. https://doi.org/10.1016/j.expneurol.2007.11.031.
Hart GW, Akimoto Y. The O-GlcNAc modification. In: Varki A, Cummings RD, Esko JD, Freeze HH, Stanley P, Bertozzi CR, et al., editors. Essentials of Glycobiology. 2nd ed. NY: Cold Spring Harbor; 2009.
Hanover JA, Yu S, Lubas WB, Shin SH, Ragano-Caracciola M, Kochran J, et al. Mitochondrial and nucleocytoplasmic isoforms of O-linked GlcNAc transferase encoded by a single mammalian gene. Arch Biochem Biophys. 2003;409(2):287–97.
Love DC, Kochan J, Cathey RL, Shin SH, Hanover JA. Mitochondrial and nucleocytoplasmic targeting of O-linked GlcNAc transferase. J Cell Sci. 2003;116(Pt 4):647–54.
Makino A, Suarez J, Gawlowski T, Han W, Wang H, Scott BT, et al. Regulation of mitochondrial morphology and function by O-GlcNAcylation in neonatal cardiac myocytes. Am J Physiol Regul Integr Comp Physiol. 2011;300(6):R1296–302. https://doi.org/10.1152/ajpregu.00437.2010.
Liu J, Marchase RB, Chatham JC. Increased O-GlcNAc levels during reperfusion lead to improved functional recovery and reduced calpain proteolysis. Am J Physiol Heart Circ Physiol. 2007;293(3):H1391–9. https://doi.org/10.1152/ajpheart.00285.2007.
Schreiber V, Dantzer F, Ame JC, de Murcia G. Poly(ADP-ribose): novel functions for an old molecule. Nat Rev Mol Cell Biol. 2006;7(7):517–28. https://doi.org/10.1038/nrm1963.
Vyas S, Matic I, Uchima L, Rood J, Zaja R, Hay RT, et al. Family-wide analysis of poly(ADP-ribose) polymerase activity. Nat Commun. 2014;5:4426. https://doi.org/10.1038/ncomms5426.
Daniels CM, Ong SE, Leung AK. The promise of proteomics for the study of ADP-ribosylation. Mol Cell. 2015;58(6):911–24. https://doi.org/10.1016/j.molcel.2015.06.012.
Barkauskaite E, Jankevicius G, Ahel I. Structures and mechanisms of enzymes employed in the synthesis and degradation of PARP-dependent protein ADP-ribosylation. Mol Cell. 2015;58(6):935–46. https://doi.org/10.1016/j.molcel.2015.05.007.
Gagne JP, Isabelle M, Lo KS, Bourassa S, Hendzel MJ, Dawson VL, et al. Proteome-wide identification of poly(ADP-ribose) binding proteins and poly(ADP-ribose)-associated protein complexes. Nucleic Acids Res. 2008;36(22):6959–76. https://doi.org/10.1093/nar/gkn771.
Gagne JP, Pic E, Isabelle M, Krietsch J, Ethier C, Paquet E, et al. Quantitative proteomics profiling of the poly(ADP-ribose)-related response to genotoxic stress. Nucleic Acids Res. 2012;40(16):7788–805. https://doi.org/10.1093/nar/gks486.
Carter-O'Connell I, Jin H, Morgan RK, Zaja R, David LL, Ahel I, et al. Identifying family-member-specific targets of mono-ARTDs by using a chemical genetics approach. Cell Rep. 2016;14(3):621–31. https://doi.org/10.1016/j.celrep.2015.12.045.
Szczesny B, Brunyanszki A, Olah G, Mitra S, Szabo C. Opposing roles of mitochondrial and nuclear PARP1 in the regulation of mitochondrial and nuclear DNA integrity: implications for the regulation of mitochondrial function. Nucleic Acids Res. 2014;42(21):13161–73. https://doi.org/10.1093/nar/gku1089.
Rossi MN, Carbone M, Mostocotto C, Mancone C, Tripodi M, Maione R, et al. Mitochondrial localization of PARP-1 requires interaction with mitofilin and is involved in the maintenance of mitochondrial DNA integrity. J Biol Chem. 2009;284(46):31616–24. https://doi.org/10.1074/jbc.M109.025882.
Niere M, Mashimo M, Agledal L, Dolle C, Kasamatsu A, Kato J, et al. ADP-ribosylhydrolase 3 (ARH3), not poly(ADP-ribose) glycohydrolase (PARG) isoforms, is responsible for degradation of mitochondrial matrix-associated poly(ADP-ribose). J Biol Chem. 2012;287(20):16088–102. https://doi.org/10.1074/jbc.M112.349183.
Park JH, Long A, Owens K, Kristian T. Nicotinamide mononucleotide inhibits post-ischemic NAD(+) degradation and dramatically ameliorates brain damage following global cerebral ischemia. Neurobiol Dis. 2016;95:102–10. https://doi.org/10.1016/j.nbd.2016.07.018.
Rogers LD, Overall CM. Proteolytic post-translational modification of proteins: proteomic tools and methodology. Mol Cell Proteomics. 2013;12(12):3532–42. https://doi.org/10.1074/mcp.M113.031310.
Ishihara N, Fujita Y, Oka T, Mihara K. Regulation of mitochondrial morphology through proteolytic cleavage of OPA1. EMBO J. 2006;25(13):2966–77. https://doi.org/10.1038/sj.emboj.7601184.
Mishra P, Carelli V, Manfredi G, Chan DC. Proteolytic cleavage of Opa1 stimulates mitochondrial inner membrane fusion and couples fusion to oxidative phosphorylation. Cell Metab. 2014;19(4):630–41. https://doi.org/10.1016/j.cmet.2014.03.011.
Anand R, Wai T, Baker MJ, Kladt N, Schauss AC, Rugarli E, et al. The i-AAA protease YME1L and OMA1 cleave OPA1 to balance mitochondrial fusion and fission. J Cell Biol. 2014;204(6):919–29. https://doi.org/10.1083/jcb.201308006.
Cipolat S, Martins de Brito O, Dal Zilio B, Scorrano L. OPA1 requires mitofusin 1 to promote mitochondrial fusion. Proc Natl Acad Sci U S A. 2004;101(45):15927–32. https://doi.org/10.1073/pnas.0407043101.
Olichon A, Baricault L, Gas N, Guillou E, Valette A, Belenguer P, et al. Loss of OPA1 perturbates the mitochondrial inner membrane structure and integrity, leading to cytochrome c release and apoptosis. J Biol Chem. 2003;278(10):7743–6. https://doi.org/10.1074/jbc.C200677200.
Olichon A, Guillou E, Delettre C, Landes T, Arnaune-Pelloquin L, Emorine LJ, et al. Mitochondrial dynamics and disease, OPA1. Biochim Biophys Acta. 2006;1763(5–6):500–9. https://doi.org/10.1016/j.bbamcr.2006.04.003.
Satoh M, Hamamoto T, Seo N, Kagawa Y, Endo H. Differential sublocalization of the dynamin-related protein OPA1 isoforms in mitochondria. Biochem Biophys Res Commun. 2003;300(2):482–93.
Merkwirth C, Dargazanli S, Tatsuta T, Geimer S, Lower B, Wunderlich FT, et al. Prohibitins control cell proliferation and apoptosis by regulating OPA1-dependent cristae morphogenesis in mitochondria. Genes Dev. 2008;22(4):476–88. https://doi.org/10.1101/gad.460708.
Song Z, Ghochani M, McCaffery JM, Frey TG, Chan DC. Mitofusins and OPA1 mediate sequential steps in mitochondrial membrane fusion. Mol Biol Cell. 2009;20(15):3525–32. https://doi.org/10.1091/mbc.E09-03-0252.
Akepati VR, Muller EC, Otto A, Strauss HM, Portwich M, Alexander C. Characterization of OPA1 isoforms isolated from mouse tissues. J Neurochem. 2008;106(1):372–83. https://doi.org/10.1111/j.1471-4159.2008.05401.x.
Duvezin-Caubet S, Jagasia R, Wagener J, Hofmann S, Trifunovic A, Hansson A, et al. Proteolytic processing of OPA1 links mitochondrial dysfunction to alterations in mitochondrial morphology. J Biol Chem. 2006;281(49):37972–9. https://doi.org/10.1074/jbc.M606059200.
Song Z, Chen H, Fiket M, Alexander C, Chan DC. OPA1 processing controls mitochondrial fusion and is regulated by mRNA splicing, membrane potential, and Yme1L. J Cell Biol. 2007;178(5):749–55. https://doi.org/10.1083/jcb.200704110.
Kasashima K, Sumitani M, Satoh M, Endo H. Human prohibitin 1 maintains the organization and stability of the mitochondrial nucleoids. Exp Cell Res. 2008;314(5):988–96. https://doi.org/10.1016/j.yexcr.2008.01.005.
Kurinami H, Shimamura M, Ma T, Qian L, Koizumi K, Park L, et al. Prohibitin viral gene transfer protects hippocampal CA1 neurons from ischemia and ameliorates postischemic hippocampal dysfunction. Stroke. 2014;45(4):1131–8. https://doi.org/10.1161/STROKEAHA.113.003577.
Stiburek L, Cesnekova J, Kostkova O, Fornuskova D, Vinsova K, Wenchich L, et al. YME1L controls the accumulation of respiratory chain subunits and is required for apoptotic resistance, cristae morphogenesis, and cell proliferation. Mol Biol Cell. 2012;23(6):1010–23. https://doi.org/10.1091/mbc.E11-08-0674.
Ehses S, Raschke I, Mancuso G, Bernacchia A, Geimer S, Tondera D, et al. Regulation of OPA1 processing and mitochondrial fusion by m-AAA protease isoenzymes and OMA1. J Cell Biol. 2009;187(7):1023–36. https://doi.org/10.1083/jcb.200906084.
Baker MJ, Lampe PA, Stojanovski D, Korwitz A, Anand R, Tatsuta T, et al. Stress-induced OMA1 activation and autocatalytic turnover regulate OPA1-dependent mitochondrial dynamics. EMBO J. 2014;33(6):578–93. https://doi.org/10.1002/embj.201386474.
Cipolat S, Rudka T, Hartmann D, Costa V, Serneels L, Craessaerts K, et al. Mitochondrial rhomboid PARL regulates cytochrome c release during apoptosis via OPA1-dependent cristae remodeling. Cell. 2006;126(1):163–75. https://doi.org/10.1016/j.cell.2006.06.021.
Duvezin-Caubet S, Koppen M, Wagener J, Zick M, Israel L, Bernacchia A, et al. OPA1 processing reconstituted in yeast depends on the subunit composition of the m-AAA protease in mitochondria. Mol Biol Cell. 2007;18(9):3582–90. https://doi.org/10.1091/mbc.E07-02-0164.
Frezza C, Cipolat S, Martins de Brito O, Micaroni M, Beznoussenko GV, Rudka T, et al. OPA1 controls apoptotic cristae remodeling independently from mitochondrial fusion. Cell. 2006;126(1):177–89. https://doi.org/10.1016/j.cell.2006.06.025.
Griparic L, Kanazawa T, van der Bliek AM. Regulation of the mitochondrial dynamin-like protein Opa1 by proteolytic cleavage. J Cell Biol. 2007;178(5):757–64. https://doi.org/10.1083/jcb.200704112.
Baburamani AA, Hurling C, Stolp H, Sobotka K, Gressens P, Hagberg H, et al. Mitochondrial optic atrophy (OPA) 1 processing is altered in response to neonatal hypoxic-ischemic brain injury. Int J Mol Sci. 2015;16(9):22509–26. https://doi.org/10.3390/ijms160922509.
Jahani-Asl A, Pilon-Larose K, Xu W, MacLaurin JG, Park DS, McBride HM, et al. The mitochondrial inner membrane GTPase, optic atrophy 1 (Opa1), restores mitochondrial morphology and promotes neuronal survival following excitotoxicity. J Biol Chem. 2011;286(6):4772–82. https://doi.org/10.1074/jbc.M110.167155.
Ha M, Kim VN. Regulation of microRNA biogenesis. Nat Rev Mol Cell Biol. 2014;15(8):509–24. https://doi.org/10.1038/nrm3838.
Paul P, Chakraborty A, Sarkar D, Langthasa M, Rahman M, Bari M, et al. Interplay between miRNAs and human diseases. J Cell Physiol. 2017; https://doi.org/10.1002/jcp.25854.
Wang JX, Jiao JQ, Li Q, Long B, Wang K, Liu JP, et al. miR-499 regulates mitochondrial dynamics by targeting calcineurin and dynamin-related protein-1. Nat Med. 2011;17(1):71–8. https://doi.org/10.1038/nm.2282.
Long B, Wang K, Li N, Murtaza I, Xiao JY, Fan YY, et al. miR-761 regulates the mitochondrial network by targeting mitochondrial fission factor. Free Radic Biol Med. 2013;65:371–9. https://doi.org/10.1016/j.freeradbiomed.2013.07.009.
Wang K, Long B, Jiao JQ, Wang JX, Liu JP, Li Q, et al. miR-484 regulates mitochondrial network through targeting Fis1. Nat Commun. 2012;3:781. https://doi.org/10.1038/ncomms1770.
Li J, Li Y, Jiao J, Wang J, Li Y, Qin D, et al. Mitofusin 1 is negatively regulated by microRNA 140 in cardiomyocyte apoptosis. Mol Cell Biol. 2014;34(10):1788–99. https://doi.org/10.1128/MCB.00774-13.
Funding
This study was funded by U.S. Veterans Affairs Merit grant BX000917 to TK.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Nina Klimova, Aaron Long, and Dr. Tibor Kristian declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Klimova, N., Long, A. & Kristian, T. Significance of Mitochondrial Protein Post-translational Modifications in Pathophysiology of Brain Injury. Transl. Stroke Res. 9, 223–237 (2018). https://doi.org/10.1007/s12975-017-0569-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-017-0569-8