Abstract
It is not uncommon for brain metastasis (BM) treated with stereotactic radiosurgery (SRS) to demonstrate radiographic enlargement, with the patient developing neurological deficits attributable to a lesion at the site of SRS. The management of both local recurrence and radiation-induced necrosis (RN) poses a significant therapeutic dilemma, if surgical resection is not feasible, and effective therapies have yet to be established. This preliminary study introduces our initial experience with salvage SRS using adjuvant bevacizumab for this refractory entity. We retrospectively reviewed five patients who had received salvage SRS using adjuvant bevacizumab for recurrent BM complicated by RN. The diagnosis was based on clinical features, serial imaging studies and/or histopathological findings. Patients underwent salvage SRS followed by the first cycle of bevacizumab (7.5–10 mg/kg intravenous). Bevacizumab was repeated every 3–4 weeks until tumor progression or significant toxic events. The number of bevacizumab doses ranged from 2 to 16 (median 4). Follow-up MR imaging demonstrated a clear radiographic response in all lesions. Neurological symptoms improved in three patients and stabilized in two. In two patients, bevacizumab treatment was discontinued due to anemia and gastrointestinal bleeding, respectively. At the time of data analysis, four patients had died and the other was still alive. The causes of death were neurological decline and systemic disease progression in two patients each. Salvage SRS with adjuvant bevacizumab use appeared to provide an adequate radiographic response as well as neurological palliation for selected patients with heavily treated recurrent BM complicated by RN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stereotactic radiosurgery (SRS) has been shown to be an effective and relatively non-invasive therapeutic option for small to medium-sized brain metastases (BM) [1]. It is, however, not uncommon for BM treated with SRS to demonstrate radiographic enlargement, with the patient developing neurological deficits attributable to a lesion at the site of SRS [2]. Differentiation of local recurrence (LR) from radiation-induced necrosis (RN) is paramount for effective subsequent management. However, it is not always possible to accurately distinguish among enlarging lesions even with advanced imaging techniques. Previous studies have demonstrated that there are three rather than two possibilities; LR, RN and a pathology combining these two entities (Table 1) [3–9]. The management of both LR and RN poses a significant therapeutic dilemma, if surgical resection is not feasible, and effective therapies have yet to be established. In this preliminary report, we introduce our initial experience with salvage SRS using adjuvant bevacizumab, a monoclonal antibody against vascular endothelial growth factor (VEGF), for complicated entities involving both LR and RN. We also discuss the safety and efficacy of this treatment strategy.
Methods
The present study was conducted in compliance with the Declaration of Helsinki (sixth revision, 2008), and fulfilled all of the requirements for patient anonymity. The institutional review board of the Saitama Gamma Knife Center approved this retrospective clinical study in January 2015. Eligibility criteria were as follows. Inclusion criteria were (i) intracranial metastasis previously treated with SRS, (ii) lesions diagnosed as a mixture of LR and surrounding radiation injury based on the clinical course, contrast-enhanced magnetic resonance (MR) imaging features, and histopathological studies when available, (iii) lesions causing severe progressive neurological deterioration and refractory to conservative management, (iv) lesions not surgically resectable based on neuroanatomical considerations and/or poor systemic condition. Exclusion criterion were (i) hemoptysis, (ii) documented hemorrhagic diathesis or coagulopathy, (iii) clinically significant cardiovascular disease; and medically uncontrolled hypertension. The patients were allowed to have undergone systemic chemotherapy for their primary cancer. Five patients meeting the inclusion criteria, but none of the exclusion criteria, were thus enrolled in the present study. All patients and/or their relatives were fully informed that salvage SRS with adjuvant use of bevacizumab remains an unproven strategy in terms of safety and efficacy, and all provided written informed consent.
A schematic model of salvage SRS with adjuvant use of bevacizumab is presented in Fig. 1
Schematic model of salvage SRS with adjuvant use of bevacizumab. SRS highly selective for focal recurrence controls tumor progression, but simultaneously aggravates radiation-induced necrosis and perifocal edema by increasing the release of vascular endothelial growth factor (VEGF). Adjuvant bevacizumab suppresses this cascade by neutralizing the harmful effects of overexpressed VEGF
. Salvage SRS was planned before the initiation of anti-VEGF therapy because bevacizumab is known to reduce contrast leakage and to produce an apparent decrease in enhancement [10–12], thereby obscuring the border of the tumor on MR imaging and reducing the accuracy of dose planning. SRS was performed using the Leksell G stereotactic frame (Elekta Instruments, Stockholm, Sweden). The frame was placed on the patient’s head under local anesthesia supplemented with mild sedation. High-resolution 3-deminsional (3-D) volumetric gadolinium-enhanced T1-weighted MR images, 2 mm in thickness T2-weighted MR images and computed tomography with a 1 mm slice thickness were routinely used for dose planning with Leksell Gamma Plan software (Elekta Instruments). On imaging studies conducted at the time of the salvage SRS, the two components, LR and RN, were meticulously identified in varying proportions. The former was typically recognized as a nodule with reduced intensity on T2-weighted images within an enlarging contrast-enhanced lesion (Fig. 2) [5, 6]. The radiation target was limited to only the part representing true recurrence, with the RN portion being excluded from the target as much as possible (Fig. 2). Prescribed and isodose doses were selected according to tumor size, accumulated radiation dose and proximity to critical structures.
Detailed treatment plan for salvage SRS with adjuvant use of bevacizumab for Patient 5. The upper and lower images are contrast-enhanced T1-weighted and T2-weighted axial MR images, respectively. Images obtained 2 months before salvage SRS showing the small-enhanced nodule of true recurrence (red arrows) surrounded by radiation-induced edema and cyst formation (a). Images obtained at the time of salvage SRS with adjuvant use of bevacizumab showing evident growth of the recurrent nodule, whereas the surrounding radiation-induced tissue changes had not significantly worsened. The target of salvage SRS was strictly limited to true recurrence. The yellow lines represent the prescription isodose volumes (20 Gy at 55 %) (b). Images obtained 16 months after salvage SRS showing the irradiated nodule to still be diminished (red arrow-heads) and the surrounding radiation-induced tissue changes to be controlled as well (c)
The first dose of bevacizumab was administered (7.5–10 mg/kg, intravenously) after monitoring for at least 24 h after salvage SRS. Physical examinations and blood chemical analyses were regularly conducted at the initial and subsequent administrations of bevacizumab. Patients continued to receive bevacizumab every 3–4 weeks unless intolerable toxicity or tumor progression was documented. If an abnormality was observed, additional examinations and treatment were carried out, as appropriate, and the administration schedule was postponed or discontinued accordingly. The endpoint of the present study was perifocal edema enlargement on T2-weighted images and/or neurological worsening caused by the lesion of interest. Clinical follow-up data as well as repeat contrast-enhanced MR images were obtained every 4–12 weeks. Any adverse events attributable to SRS procedures were recorded and graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE), version 3.0.
Results
The patient characteristics are summarized in Table 2. There were two males and three females. Patient ages at the time of the first SRS intervention ranged from 63 to 78 years. Their primary diseases were 3 non-small cell lung cancers and 2 colon cancers. Four of the five patients had solitary BM and the other had multiple BM. All patients had initially been treated with Gamma Knife SRS at our institution. One (Patient 4) had undergone two-session SRS because of a large tumor volume (>10 mL) [13]. Prior to the salvage SRS with adjuvant use of bevacizumab, three patients (Patients 1, 2 and 5) had already undergone repeat SRS and Patients 1 and 5 had also received surgical resection. The intervals between the first intervention and salvage SRS followed by bevacizumab ranged from 6 to 45 months (median 13 months). All lesions caused progressive neurological deterioration and showed enlargement of an area of contrast enhancement and perifocal edema on serial MR imaging, despite prior radical and conservative managements. Karnofsky performance status (KPS) scores ranged from 50 to 70 at the time of salvage SRS with adjuvant use of bevacizumab. The recurrent tumor volumes ranged from 1.3 to 6.4 mL (median 4.4 ml), peripheral doses from 15 to 20 Gy (median 18 Gy). The volumes of hyperintense areas on T2-weighted images ranged from 23 to 122 mL (median 64 mL).
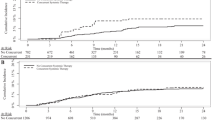
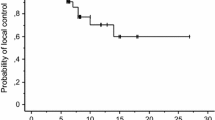
The number of bevacizumab doses ranged 2–16. The MR imaging follow-up periods ranged from 1.5 to 13 months (median 4.5 months) after the start of bevacizumab therapy. The last follow-up MR images clearly demonstrated the radiological response of a diminished contrast enhancement area and the volume of hyperintense areas on T2-weighted images at the last follow-up was significantly reduced within a range from 1.8 to 23 mL (median 11 mL) (p = 0.0459, paired t test) (Figs. 3, 4a). Significant neurological improvement (≥20 KPS) was observed in three patients and stabilization in two (p ≥ 0.05, paired t test) (Table 2; Fig. 4b). Oral steroids (dexamethasone) had been used in all patients for control of the associated symptoms prior this treatment and the doses had ranged from 1 to 3 mg/day. Salvage SRS with bevacizumab allowed steroids to be reduced or discontinued, according to the neurological improvements achieved, in all patients.
T2-weighted MR images before and after salvage SRS with adjuvant use of bevacizumab. Patient 1 (a), Patient 2 (b), Patient 3 (c), Patient 4 (d) and Patient 5 (e). The upper images are T2-weighted and were obtained before salvage SRS with adjuvant use of bevacizumab. The yellow lines represent the prescription isodose volumes. The lower images are those obtained at the last follow up
Imaging and clinical responses to salvage SRS with adjuvant use of bevacizumab. Volume changes in perilesional edema (a). The median volumes of hyperintense areas on T2-weighted images were significantly reduced from 64 (range 23–122 mL) to 11 mL (range 1.8–23 mL) (p = 0.0459, paired t test). Changes in KPS scores (b). Neurological symptoms improved significantly in three patients and stabilized in two (p > 0.05, paired t test)
Significant adverse events necessitating the discontinuation of bevacizumab occurred in two patients. One patient (Patient 2) had acute progressive anemia (CTCAE grade III) after two doses of bevacizumab. Further investigation failed to identify any hemorrhagic cause but, thereafter, blood transfusion stabilized his systemic condition. Another patient (Patient 4) experienced gastrointestinal bleeding (CTCAE grade III) after 4 doses of bevacizumab, which showed no further aggravation after bevacizumab discontinuation and conservative medical management was thus instituted. These two patients eventually did reach the study endpoint after discontinuation of bevacizumab, and then succumbed to BM progression, specifically aspiration pneumonia and status epilepticus. Two other patients (Patients 1 and 3) received repeated administrations of bevacizumab and showed no neurological decline until death due to systemic disease progression. Patient 5 remains alive and continues to receive bevacizumab treatment with no adverse effects, and showed neither intracranial recurrence nor neurological symptoms at the last follow-up. Treatment results are summarized in Table 2.
Discussion
The fundamental problem tackled in the present study is determining treatment indications. The use of bevacizumab has been strictly limited to cases in which symptomatic edema was refractory to corticosteroids, neurological symptoms were severe and surgical intervention apparently carried a potential risk of significant morbidity. However, we can not necessarily exclude the possibility that patients included in the present study were over-treated. Were the five patients reported herein actually appropriate candidates for repeat SRS with adjuvant bevacizumab? Only the accumulation of further cases can answer this question.
In managing BM after SRS, differentiation between LR and RN is crucial for appropriate salvage treatment. Accurate diagnosis of both entities, however, remains difficult even with various diagnostic modalities ranging from MR-based imaging including perfusion [14] and spectroscopy [15] to nuclear medicine scans such as 11C-methionine positron emission tomography [16, 17] and single photon emission computed tomography [18]. One of the main reasons for imperfect imaging diagnosis might be that microscopic analyses have varied among reported cases and have included various degrees of viable tumor, necrotic tissue and reactive gliosis in surrounding brain tissues [3–9, 19].
Surgical extirpation of an enlarging irradiated lesion is a treatment of choice, irrespective of the histological diagnosis, which achieves rapid symptom relief as well as a confirmed histological diagnosis. However, surgical resection in deep or eloquent locations may not necessarily be feasible because of the potential for neurological complications. Other factors such as patient age, advanced systemic disease and limited life expectancy can make such an invasive treatment unattractive.
Stereotactic re-irradiation for locally recurring BM is not generally supported given the lack of sufficient clinical evidence, although several small studies have shown the efficacy and safety of stereotactic re-irradiation for recurrent tumors [20]. Additional salvage SRS might be beneficial for selected patients with small recurrences, while being contraindicated for those with symptomatic RN. In such a clinical setting, further enlargement of perilesional edema after salvage SRS would directly exacerbate neurological symptoms. These patients have few if any alternative treatment options.
The common characteristic change in both LR and RN is an enlarging area of contrast enhancement and perilesional edema, which may cause significant neurological deficits. Animal and in vitro data indicate that VEGF is a primary mediator of perilesional edema [21, 22]. In the clinical setting, perilesional edema has also been found to be induced mainly by excessive secretion of VEGF in various pathological entities [23–27]. Bevacizumab is a humanized recombinant antibody that prevents VEGF receptor binding, and thereby inhibits angiogenesis and tumor growth. Knowledge concerning the safety and efficacy of concurrent bevacizumab with SRS for recurrent glioblastoma has been accumulating [28–30]. Quite recently, bevacizumab was also found to be effective for controlling the growth of intracranial benign tumors and even for delayed RN [26, 27, 31, 32]. Given that VEGF is a final common mediator of perilesional edema related to both LR and RN [19], this anti-angiogenic agent can be expected to significantly reduce perilesional edema coupled with neurological symptom relief [23, 24, 26, 33, 34].
The management of both LR and RN poses a significant therapeutic dilemma unless surgical resection is feasible. Thus, no effective therapies have yet been identified. When evaluated in the context of recent studies of bevacizumab for intracranial diseases such as glioblastoma and delayed RN, bevacizumab is a potentially valuable tool in the armamentarium for managing these refractory conditions. In the short-term, treatment with bevacizumab alone may tentatively achieve radiological and clinical improvements. However, in the medium- and long-term there exists a risk of progression without increased enhancement, the so-called “pseudo-response” [10, 12, 35], which can delay the determination of local failure in the absence of worsening enhancement. It would appear to be rational that salvage SRS with adjuvant use of bevacizumab can achieve local tumor control as well as reducing perilesional edema related to RN (Fig. 1).
Patients’ neurological symptoms improved or at least stabilized, while corticosteroids were tapered and discontinued. We consider this new treatment approach to have potential beneficial effects, given the serious multiple side effects and toxicities associated with corticosteroid use. However, the reasons for two of our cases experiencing no net clinical improvement despite their evident imaging responses, merit serious analysis. These cases had been extensively treated prior to enrollment in this study and had severe neurological morbidities at the time of salvage re-irradiation followed by bevacizumab. Previously, bevacizumab use was contraindicated in patients with BM in Japan, and this was the primary reason for delayed use of this agent in our five cases. The resulting neurological deficits would have been attributed to direct insults involving eloquent areas due to RN rather than extension of perifocal edema. Once there is direct injury, functional recovery would be difficult to achieve even with a good radiological response secondary to bevacizumab administration. If earlier intervention with bevacizumab had been conducted before the progression of direct injury, greater improvement in the patient’s quality of life might well have been achieved.
The authors advocate that the treatment indications be strictly limited to cases having no alternative but to undergo such an unproven treatment given its potential toxicity. In fact, two of the five patients in our series experienced serious adverse events probably related to bevacizumab administration. When this agent is used after salvage SRS, patients must be monitored meticulously with physical and hematological examinations and serial imaging studies for potential development of bevacizumab-associated toxicity. Considering the remarkable improvement in radiological examination outcomes, dose tapering of bevacizumab would be warranted to elucidate the minimal effective dose as well as to reduce the potential risk of adverse events. The timing of bevacizumab therapy discontinuation is also a matter of debate. Previous studies showed relapse of RN after bevacizumab was discontinued [32, 34] and second line bevacizumab treatment was effective in some patients. As yet, we have no specific exit strategy and, in our opinion, these problems should also be addressed taking into account the balance between medical costs and clinical efficacy.
In a situation of morbidity induced by a heavy local tumor burden and under conditions in which further surgical intervention is not feasible, this relatively low-invasive treatment may have a potential role in achieving clinical benefits and could thereby expand our treatment armamentarium. Given the very limited number of patients and the short imaging follow-up term (median 4.5 months) in the present study, however, the data are not sufficient to provide proof of a synergistic effect of SRS and bevacizumab. We consider the present study to have been necessary as a means of hypothesis generation, providing the groundwork for future investigation. A prospective pilot study with salvage SRS using adjuvant bevacizumab for recurrent BM will be required to determine the efficacy as well as the toxicity of this novel approach.
Conclusion
Judicious radiosurgical salvage with adjuvant use of bevacizumab to treat recurrent BM complicated by RN appeared to achieve clinical benefits for a small group of patients in the short-term. Further studies are required to determine the medium- to long-term efficacy and toxicity of this treatment.
References
Yamamoto M, Serizawa T, Shuto T, Akabane A, Higuchi Y, Kawagishi J, Yamanaka K, Sato Y, Jokura H, Yomo S, Nagano O, Kenai H, Moriki A, Suzuki S, Kida Y, Iwai Y, Hayashi M, Onishi H, Gondo M, Sato M, Akimitsu T, Kubo K, Kikuchi Y, Shibasaki T, Goto T, Takanashi M, Mori Y, Takakura K, Saeki N, Kunieda E, Aoyama H, Momoshima S, Tsuchiya K (2014) Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 15:387–395. doi:10.1016/S1470-2045(14)70061-0
Sneed PK, Mendez J, Vemer-van den Hoek JG, Seymour ZA, Ma L, Molinaro AM, Fogh SE, Nakamura JL, McDermott MW (2015) Adverse radiation effect after stereotactic radiosurgery for brain metastases: incidence, time course, and risk factors. J Neurosurg. doi:10.3171/2014.10.JNS141610
Vecil GG, Suki D, Maldaun MV, Lang FF, Sawaya R (2005) Resection of brain metastases previously treated with stereotactic radiosurgery. J Neurosurg 102:209–215. doi:10.3171/jns.2005.102.2.0209
Truong MT, St Clair EG, Donahue BR, Rush SC, Miller DC, Formenti SC, Knopp EA, Han K, Golfinos JG (2006) Results of surgical resection for progression of brain metastases previously treated by gamma knife radiosurgery. Neurosurgery 59:86–97. doi:10.1227/01.NEU.0000219858.80351.38 (discussion 86–97)
Dequesada IM, Quisling RG, Yachnis A, Friedman WA (2008) Can standard magnetic resonance imaging reliably distinguish recurrent tumor from radiation necrosis after radiosurgery for brain metastases? A radiographic-pathological study. Neurosurgery 63:898–903. doi:10.1227/01.NEU.0000333263.31870.31 (discussion 904)
Kano H, Kondziolka D, Lobato-Polo J, Zorro O, Flickinger JC, Lunsford LD (2010) T1/T2 matching to differentiate tumor growth from radiation effects after stereotactic radiosurgery. Neurosurgery 66:486–491. doi:10.1227/01.NEU.0000360391.35749.A5 (discussion 491–482)
Stockham AL, Tievsky AL, Koyfman SA, Reddy CA, Suh JH, Vogelbaum MA, Barnett GH, Chao ST (2012) Conventional MRI does not reliably distinguish radiation necrosis from tumor recurrence after stereotactic radiosurgery. J Neurooncol 109:149–158. doi:10.1007/s11060-012-0881-9
Leeman JE, Clump DA, Flickinger JC, Mintz AH, Burton SA, Heron DE (2013) Extent of perilesional edema differentiates radionecrosis from tumor recurrence following stereotactic radiosurgery for brain metastases. Neuro Oncol 15:1732–1738. doi:10.1093/neuonc/not130
Nath SK, Sheridan AD, Rauch PJ, Yu JB, Minja FJ, Vortmeyer AO, Chiang VL (2014) Significance of histology in determining management of lesions regrowing after radiosurgery. J Neurooncol 117:303–310. doi:10.1007/s11060-014-1389-2
Mathews MS, Linskey ME, Hasso AN, Fruehauf JP (2008) The effect of bevacizumab (Avastin) on neuroimaging of brain metastases. Surg Neurol 70:649–652. doi:10.1016/j.surneu.2007.06.029 (discussion 653)
Iwamoto FM, Fine HA (2010) Bevacizumab for malignant gliomas. Arch Neurol 67:285–288. doi:10.1001/archneurol.2010.11
Kleinschmidt-DeMasters BK, Damek DM (2010) The imaging and neuropathological effects of Bevacizumab (Avastin) in patients with leptomeningeal carcinomatosis. J Neurooncol 96:375–384. doi:10.1007/s11060-009-9969-2
Yomo S, Hayashi M (2014) A minimally invasive treatment option for large metastatic brain tumors: long-term results of two-session Gamma Knife stereotactic radiosurgery. Radiat Oncol 9:132. doi:10.1186/1748-717X-9-132
Mitsuya K, Nakasu Y, Horiguchi S, Harada H, Nishimura T, Bando E, Okawa H, Furukawa Y, Hirai T, Endo M (2010) Perfusion weighted magnetic resonance imaging to distinguish the recurrence of metastatic brain tumors from radiation necrosis after stereotactic radiosurgery. J Neurooncol 99:81–88. doi:10.1007/s11060-009-0106-z
Chernov M, Hayashi M, Izawa M, Ochiai T, Usukura M, Abe K, Ono Y, Muragaki Y, Kubo O, Hori T, Takakura K (2005) Differentiation of the radiation-induced necrosis and tumor recurrence after gamma knife radiosurgery for brain metastases: importance of multi-voxel proton MRS. Minim Invasive Neurosurg 48:228–234. doi:10.1055/s-2005-870952
Tsuyuguchi N, Sunada I, Iwai Y, Yamanaka K, Tanaka K, Takami T, Otsuka Y, Sakamoto S, Ohata K, Goto T, Hara M (2003) Methionine positron emission tomography of recurrent metastatic brain tumor and radiation necrosis after stereotactic radiosurgery: is a differential diagnosis possible? J Neurosurg 98:1056–1064. doi:10.3171/jns.2003.98.5.1056
Terakawa Y, Tsuyuguchi N, Iwai Y, Yamanaka K, Higashiyama S, Takami T, Ohata K (2008) Diagnostic accuracy of 11C-methionine PET for differentiation of recurrent brain tumors from radiation necrosis after radiotherapy. J Nucl Med 49:694–699. doi:10.2967/jnumed.107.048082
Serizawa T, Saeki N, Higuchi Y, Ono J, Matsuda S, Sato M, Yanagisawa M, Iuchi T, Nagano O, Yamaura A (2005) Diagnostic value of thallium-201 chloride single-photon emission computerized tomography in differentiating tumor recurrence from radiation injury after gamma knife surgery for metastatic brain tumors. J Neurosurg 102(Suppl):266–271
Nonoguchi N, Miyatake S, Fukumoto M, Furuse M, Hiramatsu R, Kawabata S, Kuroiwa T, Tsuji M, Fukumoto M, Ono K (2011) The distribution of vascular endothelial growth factor-producing cells in clinical radiation necrosis of the brain: pathological consideration of their potential roles. J Neurooncol 105:423–431. doi:10.1007/s11060-011-0610-9
Ammirati M, Cobbs CS, Linskey ME, Paleologos NA, Ryken TC, Burri SH, Asher AL, Loeffler JS, Robinson PD, Andrews DW, Gaspar LE, Kondziolka D, McDermott M, Mehta MP, Mikkelsen T, Olson JJ, Patchell RA, Kalkanis SN (2010) The role of retreatment in the management of recurrent/progressive brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 96:85–96. doi:10.1007/s11060-009-0055-6
Papavassiliou E, Gogate N, Proescholdt M, Heiss JD, Walbridge S, Edwards NA, Oldfield EH, Merrill MJ (1997) Vascular endothelial growth factor (vascular permeability factor) expression in injured rat brain. J Neurosci Res 49:451–460
Proescholdt MA, Heiss JD, Walbridge S, Muhlhauser J, Capogrossi MC, Oldfield EH, Merrill MJ (1999) Vascular endothelial growth factor (VEGF) modulates vascular permeability and inflammation in rat brain. J Neuropathol Exp Neurol 58:613–627
Gonzalez J, Kumar AJ, Conrad CA, Levin VA (2007) Effect of bevacizumab on radiation necrosis of the brain. Int J Radiat Oncol Biol Phys 67:323–326. doi:10.1016/j.ijrobp.2006.10.010
Torcuator R, Zuniga R, Mohan YS, Rock J, Doyle T, Anderson J, Gutierrez J, Ryu S, Jain R, Rosenblum M, Mikkelsen T (2009) Initial experience with bevacizumab treatment for biopsy confirmed cerebral radiation necrosis. J Neurooncol 94:63–68. doi:10.1007/s11060-009-9801-z
Schmid S, Aboul-Enein F, Pfisterer W, Birkner T, Stadek C, Knosp E (2010) Vascular endothelial growth factor: the major factor for tumor neovascularization and edema formation in meningioma patients. Neurosurgery 67:1703–1708. doi:10.1227/NEU.0b013e3181fb801b (discussion 1708)
Levin VA, Bidaut L, Hou P, Kumar AJ, Wefel JS, Bekele BN, Prabhu S, Loghin M, Gilbert MR, Jackson EF (2011) Randomized double-blind placebo-controlled trial of bevacizumab therapy for radiation necrosis of the central nervous system. Int J Radiat Oncol Biol Phys 79:1487–1495. doi:10.1016/j.ijrobp.2009.12.061
Williams BJ, Park DM, Sheehan JP (2012) Bevacizumab used for the treatment of severe, refractory perilesional edema due to an arteriovenous malformation treated with stereotactic radiosurgery. J Neurosurg 116:972–977. doi:10.3171/2012.1.JNS111627
Gutin PH, Iwamoto FM, Beal K, Mohile NA, Karimi S, Hou BL, Lymberis S, Yamada Y, Chang J, Abrey LE (2009) Safety and efficacy of bevacizumab with hypofractionated stereotactic irradiation for recurrent malignant gliomas. Int J Radiat Oncol Biol Phys 75:156–163. doi:10.1016/j.ijrobp.2008.10.043
Park KJ, Kano H, Iyer A, Liu X, Niranjan A, Flickinger JC, Lieberman FS, Lunsford LD, Kondziolka D (2012) Salvage gamma knife stereotactic radiosurgery followed by bevacizumab for recurrent glioblastoma multiforme: a case-control study. J Neurooncol 107:323–333. doi:10.1007/s11060-011-0744-9
Cuneo KC, Vredenburgh JJ, Sampson JH, Reardon DA, Desjardins A, Peters KB, Friedman HS, Willett CG, Kirkpatrick JP (2012) Safety and efficacy of stereotactic radiosurgery and adjuvant bevacizumab in patients with recurrent malignant gliomas. Int J Radiat Oncol Biol Phys 82:2018–2024. doi:10.1016/j.ijrobp.2010.12.074
Plotkin SR, Stemmer-Rachamimov AO, Barker FG 2nd, Halpin C, Padera TP, Tyrrell A, Sorensen AG, Jain RK, di Tomaso E (2009) Hearing improvement after bevacizumab in patients with neurofibromatosis type 2. N Engl J Med 361:358–367. doi:10.1056/NEJMoa0902579
Furuse M, Kawabata S, Kuroiwa T, Miyatake S (2011) Repeated treatments with bevacizumab for recurrent radiation necrosis in patients with malignant brain tumors: a report of 2 cases. J Neurooncol 102:471–475. doi:10.1007/s11060-010-0333-3
Boothe D, Young R, Yamada Y, Prager A, Chan T, Beal K (2013) Bevacizumab as a treatment for radiation necrosis of brain metastases post stereotactic radiosurgery. Neuro Oncol 15:1257–1263. doi:10.1093/neuonc/not085
Deibert CP, Ahluwalia MS, Sheehan JP, Link MJ, Hasegawa T, Yomo S, Feng WH, Li P, Flickinger JC, Lunsford LD, Kondziolka D (2013) Bevacizumab for refractory adverse radiation effects after stereotactic radiosurgery. J Neurooncol 115:217–223. doi:10.1007/s11060-013-1214-3
Iwamoto FM, Abrey LE, Beal K, Gutin PH, Rosenblum MK, Reuter VE, DeAngelis LM, Lassman AB (2009) Patterns of relapse and prognosis after bevacizumab failure in recurrent glioblastoma. Neurology 73:1200–1206. doi:10.1212/WNL.0b013e3181bc0184
Acknowledgements
The authors certify that no funding was received to conduct this study and/or for preparation of this manuscript. We are grateful to Bierta Barfod, M.D., M.P.H. for her help with the language editing of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Yomo receives speaking fees from Chugai Pharmaceutical Corporation.
Rights and permissions
About this article
Cite this article
Yomo, S., Hayashi, M. Salvage stereotactic radiosurgery with adjuvant use of bevacizumab for heavily treated recurrent brain metastases: a preliminary report. J Neurooncol 127, 119–126 (2016). https://doi.org/10.1007/s11060-015-2019-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-2019-3