Abstract
In the present study we have evaluated the efficacy and toxicity of repeated stereotactic radiosurgery (SRS) in patients with recurrent/progressive brain metastases. Between March 2006 and October 2014, 43 patients (21 men and 22 women) with 47 lesions received a second course of SRS given in three daily fractions of 7–8 Gy. With a follow-up study of 19 months, the 1- and 2-year survival rates from repeated SRS were 37 and 20 %, respectively, and the 1- and 2-year local control rates were 70 and 60 %, respectively. Actuarial local control was significantly better for breast and lung metastases as compared with melanoma metastases; specifically, 1-year local control rates were 38 % for melanoma, 78 % for breast carcinoma and 73 % for non-small cell lung cancer (NSCLC) metastases (p = 0.01). The cause of death was progressive systemic disease in 25 patients and progressive brain disease in 11 patients. Stable extracranial disease (p = 0.01) and Karnofsky performance status (KPS; p = 0.03) were predictive of longer survival. Radiologic changes suggestive of brain radionecrosis were observed in 9 (19 %) out of 47 lesions, with an actuarial risk of 34 % at 12 months. Neurological deficits (RTOG Grade 2 or 3) associated with brain necrosis occurred in 14 % of patients. In conclusion, a second course of SRS given in three daily fractions is a feasible treatment for selected patients with recurrent/progressive brain metastases. Further studies are needed to explore the efficacy and safety of different dose-fractionation schedules, especially in patients with melanoma or large metastases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stereotactic radiosurgery (SRS) has been increasingly used for the treatment of patients with brain metastases, with a reported local control of 70–90 % at 12 months [1–5]. Two randomized trials showed similar survival benefits and functional independence between patients with 1–4 brain metastases treated with SRS alone or SRS plus whole brain radiation therapy (WBRT) [3, 5], indicating that brain metastases can be managed initially with SRS alone, potentially avoiding the decline of neurocognitive function and quality of life associated with WBRT [6].
For patients whom brain metastases recur after SRS, the evidence regarding the safety and efficacy of salvage therapies is limited. Treatment options include WBRT (3,5), surgery [7, 8] or SRS [9–16]. For patients with recurrent/progressive brain metastases receiving salvage SRS, a few studies report a variable survival time of 7–10 months (9–16); however, most of the series include metastases that recur after WBRT or distant from the irradiated tumor site. Thus, the efficacy and risk of radiation-induced toxicity following a second course of SRS for recurrence/progression at the previously irradiated sites remain unsubstantiated.
In the present study we have evaluated the clinical outcomes and toxicity of repeated SRS given as three daily fractions (3 × 7–8 Gy) in patients with recurrent/progressive brain metastases. In addition, the prognostic significance of different clinical and treatment parameters has been investigated.
Patients and methods
Patients’ data were obtained from a prospectively maintained database of patients with brain tumors treated at Sant’Andrea University Hospital. We identified 936 patients who received SRS alone for brain metastases between March 2006 and October 2014. After SRS, patients had a complete neurological examination and brain magnetic resonance imaging (MRI) every 2–3 months or as appropriate according to the neurological conditions. Among them, 43 patients who received a second course of SRS for recurrent/progressive disease at original sites of irradiation were included in the final analysis. All patients initiated dexamethasone therapy the first day of treatment at doses of 4–8 mg per day and maintained high doses steroids for 1 week. The Institutional Review Board approved the study.
The gross tumor volume (GTV) was identified on the basis of 1 mm gadolinium enhanced axial MRI fused with computerized tomography (CT) images. A margin of 1–2 mm was geometrically added to GTV to generate the planning target volume (PTV). A margin of 2 mm was used in our initial clinical experience with multi-fraction SRS (n = 26), and subsequently reduced to 1 mm (n = 17). Doses were 3 × 8 Gy for metastases <2 cm and 3 × 7 Gy for metastases ≥2 cm in maximum size, prescribed to the 80–90 % isodose line to achieve at least 95 % coverage of the PTV by the planned dose. Dose distributions were achieved with 4–7 noncoplanar dynamic arcs or 6–12 conformal beams by using a 120-leaf multileaf collimator in a Varian linear accelerator with 6-MV photon beam. CT imaging and, more recently, the ExacTrac® image-guided system were used for setup verification before each fraction. Patients were treated in 3 consecutive days in outpatient clinic.
After treatment, patients were examined clinically every 2 months. At each visit, a neurologic examination was performed, and the severity of complications was rated according to the Radiation Therapy Oncology Group (RTOG) toxicity criteria. MRI was made every 2 months or as appropriate according to the neurological conditions. Complete and partial responses were defined as total radiographic disappearance of lesion or decrease in tumor volume >50 %. Distant failure was defined by the presence of new brain metastases or leptomeningeal enhancement outside the irradiated volume. Diagnoses of tumor progression or radionecrosis were determined on the basis of histologic findings (in patients who underwent surgical resection) or assessed subjectively using dynamic susceptibility-weighted contrast-enhanced (DSC) perfusion MRI and 3,4-dihydroxy-6-(18)F-fluoro-l-phenylalanine (18F-DOPA) positron emission tomography (PET)-CT scans. as previously reported [17]. In summary, tumor progression was defined by any increase of tumor on contrast-enhanced T1-weighted images in at least two subsequent MRI studies associated with: a cerebral blood volume ratio (rCBV) > 2.0 at dynamic susceptibility-weighted contrast-enhanced (DSC) perfusion images (calculated for each lesion by dividing the tumor CBV by the mean CBV value obtained in the contralateral normal appearing white matter), and—a maximum lesion to maximum background uptake ratio (SUVLmax/Bkgrmax) > 1.6 at F-DOPA PET-CT. Stable or shrinking contrast-enhanced lesions over a 6-month observational period associated with: a rCBV < 2.0 at DSC perfusion images, and—a SUVLmax/Bkgrmax < 1.6 at F-DOPA PET-CT, were diagnosed as radionecrosis. The same neuroradiology team reviewed all neuroimages to assess the therapeutic response and radionecrosis.
Local control, survivals, and risk of brain radionecrosis were estimated using the Kaplan–Meier method calculated from the time of repeated SRS. Patients who did not show recurrence were censored at the time of last follow-up. Patients who had received salvage WBRT were subsequently excluded from the analysis. Univariate analysis, using the log-rank test for categorical variables and the Cox proportional hazards model for continuous variables, was performed to identify prognostic factors associated with clinical outcomes. The following factors were tested: tumor size (<2 vs ≥2 cm), SRS dose and conformity index (prescribed isodose volume/tumor volume encompassed by the prescription isodose volume) during either first or second SRS, interval between treatments, sex, age (<65 vs ≥65 years), pretreatment KPS score (≤70 vs >70), number of brain metastases (1 vs >1), diagnosis-specific graded prognostic assessment (DS-GPA) class [18], histology (melanoma vs others), and extracranial disease (stable vs progressive). In addition, we have analyzed the correlation between the risk of radionecrosis and—normal brain volume receiving 12 Gy (V12Gy) during the initial SRS—and the volumes receiving 15 Gy (V15Gy), 18 Gy (V18Gy) and 21 Gy (V21Gy) during repeated SRS. Prognostic factors with a p value < 0.1 were included in a multivariate analysis performed using a Cox proportional hazards regression model.
Results
Patient and treatment characteristics
Between March 2006 and October 2014, a total of 43 patients received a second course of SRS (3 × 7–8 Gy) for recurrent or progressive brain metastases. Patients and tumor characteristics are summarized in Table 1. There were 21 men and 22 women for a total of 47 lesions. Originally, patients received single-fraction SRS for a single metastasis (n = 18) or for 2–3 metastases (n = 25). The median time interval between SRS treatments was 17 months (range 6–56 months). Thirty-one patients had extracranial disease at the time of reirradiation. Median GTV volume was 12.3 cc (range 1.5–33.1 cc) and median PTV volume was 16.4 cc (range 2.4–37.9 cc). The mean conformity index was 1.55 (range, 1.29–2.1). The median minimum coverage was 97 % (range 93–100 %). At the time of analysis (March 2015), 36 patients had died.
Local control
With a median follow-up study of 19 months (range 2–27 months), the crude local control was 81 %, with the 1- and 2-year local control rates of 70 and 60 %, respectively (Fig. 1). Nine lesions recurred locally after repeated SRS; salvage therapy consisted of WBRT in 3 patients, surgical resection in 5 patients, and supportive care in one patient. Seven (15 %) metastases had a complete response, 15 (32 %) had a partial response, and 16 (34 %) remained stable. A clinical neurological improvement of pre-SRS existing symptoms was recorded in 11 (27 %) out of 43 patients during the follow-up.
At univariate analysis, melanoma histology (p = 0.02), radiation schedule of 3 × 7 Gy (p = 0.03), and large volumes (p = 0.04) were associated with worse control; however, only melanoma histology was predictive of local failure at multivariate analysis (p = 0.01; HR 7.1, 95 %CI 1.9–21) (Table 2). Specifically, the 1-year local control rates were 38 % for melanoma, 78 % for breast carcinoma and 73 % for NSCLC metastases. No other factors, including the maximum size of metastases at the time of first SRS, and the interval between the first and the second course of SRS were predictive of local control.
Overall survival and distant failure
The median survival was 10 months, and the 1- and 2-year survival rates were 37 and 20 % (Fig. 2). 25 (58 %) patients succumbed to their extracranial disease and 11 (26 %) to their brain disease. Nineteen patients had new brain metastases at distant sites and 4 patients progressed at either local or distant brain sites of reirradiation. The 1- and 2-year actuarial rates of developing new brain metastases were 58 and 72 %, respectively (Fig. 3). Salvage therapy consisted of WBRT (n = 6), SRS (n = 14), or both (n = 3). Median survival was similar for patients receiving WBRT or SRS (5.6 vs 7.1 months, respectively; p = 0.2).
At multivariate analysis, stable extracranial disease (p = 0.01; HR 0.18, 95 %CI 0.11–0.58) and KPS > 70 (p = 0.03; HR 0.44, 95 %CI 0.28–0.83) were associated with a significant survival benefit (Table 2). According to the DS-GPA, median survival times were 16.5, 11 and 7.3 months in patients with DS-GPA scores of 0–1, 1–2.5, and 3–4, respectively (p = 0.001); however, DS-GPA scores were not included in the multivariate analysis because they are not independent of age, KPS, and presence of extracranial disease. The presence of multiple metastases was the only factor associated with early distant brain failure (p = 0.03).
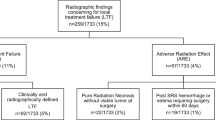
Toxicity
Brain radionecrosis, as suggested by MR/PET imaging (n = 5) or confirmed by histology (n = 4), was the most important complication occurring in 9 (19 %) out of 47 lesions. Median time to necrosis was 8 months (range 4–15 months). Neurological complications associated with radiological changes suggestive of radionecrosis occurred in 6 patients (grade 3 motor deficits in 3, grade 2 speech deficits in 1, and grade 2 confusion in 2 patients), requiring surgery or high-dose dexamethasone; symptoms improved in 4 patients as results of medical or surgical treatment. Other complications included headache, seizures, and haemorrhage in 2,3 and 2 patients, respectively.
The actuarial risk of radionecrosis after repeated SRS was 34 and 44 % at 1 and 2 years, respectively. Median V15Gy, V18Gy, and V21Gy were 24.8, 16.1, and 6.6 cm3, respectively. The only factor significantly associated with the development of brain radionecrosis was the magnitude of overlap between the volume of normal brain receiving 18 Gy at repeated SRS and the volume of normal brain receiving 12 Gy at the first course of SRS (V18–12Gy). The risk of radionecrosis was 53 % for V18–12Gy ≥ 10 cm3 and 15 % for V18–12Gy < 10 cm3 (p = 0.02). At univariate analysis, no other factors were predictive of radionecrosis, including radiation dose, size of lesion, and interval between the first and second course of SRS; however, large V18Gy (p = 0.09) and the interval between treatments 0f less than 2 years (p = 0.07) were of borderline significance.
Discussion
For patients who develop recurrent/progressive brain metastases at the site of the primary SRS, the potential clinical benefits of further irradiation, surgery or chemotherapy remain undetermined. WBRT is a feasible treatment for patients with progressive intracranial disease after SRS with a reported median survival of 4-6 months [3, 5], although data on local control and neurologic death for patients with metastases progressing at the site of the primary SRS treatment are limited. A few studies report the outcome of surgical resection for patients with recurrent/progressive brain metastases who had previously received SRS with or without WBRT [7, 8]. In a series of 32 patients with progressive/recurrent brain metastases who had SRS as part of their initial treatment and then treated with surgical resection, Truong et al. [8] observed a median survival of 8.9 months, with 48 % of patients who died for neurological causes. In another series of 61 patients who underwent surgical resection for 1–3 progressive/recurrent brain metastases, Vecil et al. [7] reported a median survival time and a distant recurrence time of 11.1 months and 8.4 months, respectively, while the median local recurrence was not reached. Cause of death was neurologic in 15 % of patients and neurologic/systemic combined in 34 % of patients.
Using a second course of SRS given in three fractions of 7–8 Gy, we observed actuarial 1- and 2-year local tumor control rates of 70 and 60 %, respectively. The 1- and 2-year survival rates were 37 and 20 %, and respective distant failure rates were 58 and 72 %, necessitating further SRS or WBRT in 44 and 21 % of patients, respectively. A few studies have evaluated the use of SRS for progressive/recurrent brain metastases in patients whose initial treatment included SRS or WBRT [9–16]. Kwon et al. [16] observed a median survival time of 8 and 6-month local control rate of 91 % in 43 patients who received a second course of SRS for progressive brain metastases. In another series of 45 patients initially treated with SRS with or without WBRT, Chen et al. [10] showed a local control rate of 90 % and a median survival of 8 months after repeated SRS. A similar local control of 77–90 % and median survival of 7–10 months have been reported with the use of SRS for brain metastases progressive after WBRT [11–15]. Overall, our study confirms that repeated SRS is a feasible option for patients with recurrent/progressive brain metastases which is associated with local control and survival advantages, possibly avoiding the potential neurocognitive impairment associated with WBRT.
Analysis of prognostic factors showed that the presence of extracranial disease and KPS ≤ 70 were associated with shorter survival, while the melanoma histology was the only factor predictive of worse local control as compared with breast carcinoma and NSCLC metastases. In a series of 153 melanoma brain metastases treated with SRS, Selek et al. [19] reported local control rates of 69.2 and 39.3 % for lesions ≤3 and >3 cm at 1 year, respectively. In another prospective study of 36 patients with 1–3 radioresistant brain metastases, Manon et al. [20] observed 6-month local failure and risk of neurological death of 32 and 38 %, respectively. More recently, the use of molecular targeted agents in patients with metastatic melanoma, including the BRAF inhibitor vemurafenib in patients with BRAF(V600) mutated metastatic melanoma, or the anti programmed death-1 (PD-1) receptor monoclonal antibodies pembrolizumab and nivolumab in combination with the anti cytotoxic T-lymphocyte antigen 4 (anti-CTLA-4) ipilimumab, has resulted in significant survival advantages and response rates of 40–60 % [21–23]. The potential benefits of combining SRS with targeted agents, or surgery plus SRS to the resection cavity in patients with recurrent melanoma brain metastases need to be assessed in future studies.
Radiation-induced brain necrosis represents the most important late toxicity reported after SRS, leading to neurological complications in 2–32 % of patients [11, 24–34]. A cumulative risk of radionecrosis of 5–12 % has been reported after multi-fraction SRS with doses of 27–35 Gy given in 3–5 fractions [26, 27, 29, 34]. Using multi-fraction SRS (3 × 9–12 Gy), we have recently observed a risk of radionecrosis of 9 and 18 % at 1 and 2 years, respectively, in a series of 135 patients with 171 brain metastases [34]. At multivariate analysis, the volumes of normal brain irradiated to 18 and 21 Gy were the most predictive independent risk factors for radionecrosis. In contrast, a higher risk of radionecrosis up to 69 % has been observed after single-fraction SRS, with the normal brain volume exposed to 10–12 Gy reported as the most important predictive variables [31, 32]. In view of the potential advantage of fractionation over single-fraction SRS in reducing the risk of radiation-induced toxicity, we have used a three-fraction schedule. Radiological changes suggestive of radionecrosis occurred in 19 % of treated lesions, with an estimated risk of 37 and 44 % at 1 and 2 years, respectively, and this was associated with severe neurological complications (RTOG Grade 3 or 4) in 14 % of patients. The V18–12Gy was the only significant predictor of radionecrosis, with a cumulative risk of 53 % for volumes ≥10 cm3. Although our schedule resulted in an acceptable incidence of severe neurological deficits, further studies need to explore new strategies for the management of progressive metastases, including different radiation schedules (single-fraction versus multi-fraction SRS), or alternative treatment as the use of the laser-induced thermotherapy [35], in order to decrease the risk of radionecrosis while improving the local control. In this regard, we have started a trial at our institution comparing the efficacy and safety of two different dose fractionation schedules (3 × 8 and 5 × 6 Gy) in patients with recurrent brain metastases.
In conclusion, a second course of SRS at doses of 21–24 Gy in three daily fractions appears to be a feasible treatment modality for progressive/recurrent brain metastases. It results in acceptable local control and risk of neurological toxicity; however, melanoma histology and large metastases are associated with reduced local control. Further studies are needed to define the optimal management of patients with recurrent brain metastases.
References
Sanghavi SN, Miranpuri SS, Chappell R, Buatti JM, Sneed PK, Suh JH, Regine WF, Weltman E, King VJ, Goetsch SJ, Breneman JC, Sperduto PW, Scott C, Mabanta S, Mehta MP (2001) Radiosurgery for patients with brain metastases: a multi-institutional analysis, stratified by the RTOG recursive partitioning analysis method. Int J Radiat Oncol Biol Phys 51:426–434
Sneed PK, Suh JH, Goetsch SJ, Sanghavi SN, Chappell R, Buatti JM, Regine WF, Weltman E, King VJ, Breneman JC, Sperduto PW, Mehta MP (2002) A multi-institutional review of radiosurgery alone vs. radiosurgery with whole brain radiotherapy as the initial management of brain metastases. Int J Radiat Oncol Biol Phys 53:519–526
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H, Kunieda E, Inomata T, Hayakawa K, Katoh N, Kobashi G (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295:2483–2491
Frazier JL, Batra S, Kapor S, Vellimana A, Gandhi R, Carson KA, Shokek O, Lim M, Kleinberg L, Rigamonti D (2010) Stereotactic radiosurgery in the management of brain metastases: an institutional retrospective analysis of survival. Int J Radiat Oncol Biol Phys 76:1486–1492
Kocher M, Soffietti R, Abacioglu U, Villà S, Fauchon F, Baumert BG, Fariselli L, Tzuk-Shina T, Kortmann RD, Carrie C, Hassel MB, Kouri M, Valeinis E, van den Berge D, Collette S, Collette L, Mueller RP (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol 29:134–141
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH, Meyers CA (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044
Vecil GG, Suki D, Maldaun MV, Lang FF, Sawaya R (2005) Resection of brain metastases previously treated with stereotactic radiosurgery. J Neurosurg 102:209–215
Truong MT, St Clair EG, Donahue BR, Rush SC, Miller DC, Formenti SC, Knopp EA, Han K, Golfinos JG (2006) Results of surgical resection for progression of brain metastases previously treated by gamma knife radiosurgery. Neurosurgery 59:86–97
Yamanaka K, Iwai Y, Yasui T, Nakajima H, Komiyama M, Nishikawa M, Morikawa T, Kishi H (1999) Gamma Knife radiosurgery for metastatic brain tumor: the usefulness of repeated Gamma Knife radiosurgery for recurrent cases. Stereotact Funct Neurosurg 72(Suppl):73–80
Chen JC, Petrovich Z, Giannotta SL, Yu C, Apuzzo ML (2000) Radiosurgical salvage therapy for patients presenting with recurrence of metastatic disease to the brain. Neurosurgery 46:860–866
Shaw E, Scott C, Souhami L, Dinapoli R, Kline R, Loeffler J, Farnan N (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys 47:291–298
Hoffman R, Sneed PK, McDermott MW, Chang S, Lamborn KR, Park E, Wara WM, Larson DA (2001) Radiosurgery for brain metastases from primary lung carcinoma. Cancer J 7:121–131
Noël G, Simon JM, Valery CA, Cornu P, Boisserie G, Hasboun D, Ledu D, Tep B, Delattre JY, Marsault C, Baillet F, Mazeron JJ (2003) Radiosurgery for brain metastasis: impact of CTV on local control. Radiother Oncol 68:15–21
Shuto T, Fujino H, Inomori S, Nagano H (2004) Repeated gamma knife radiosurgery for multiple metastatic brain tumours. Acta Neurochir (Wien) 146:989–993
Akyurek S, Chang EL, Mahajan A, Hassenbusch SJ, Allen PK, Mathews LA, Shiu AS, Maor MH, Woo SY (2007) Stereotactic radiosurgical treatment of cerebral metastases arising from breast cancer. Am J Clin Oncol 30:310–314
Kwon KY, Kong DS, Lee JI, Nam DH, Park K, Kim JH (2007) Outcome of repeated radiosurgery for recurrent metastatic brain tumors. Clin Neurol Neurosurg 109:132–137
Cicone F, Minniti G, Romano A, Papa A, Scaringi C, Tavanti F, Bozzao A, Maurizi Enrici R, Scopinaro F (2015) Accuracy of F-DOPA PET and perfusion-MRI for differentiating radionecrotic from progressive brain metastases after radiosurgery. Eur J Nucl Med Mol Imaging 42:103–111
Sperduto PW, Kased N, Roberge D, Xu Z, Shanley R, Luo X, Sneed PK, Chao ST, Weil RJ, Suh J, Bhatt A, Jensen AW, Brown PD, Shih HA, Kirkpatrick J, Gaspar LE, Fiveash JB, Chiang V, Knisely JP, Sperduto CM, Lin N, Mehta M (2012) Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol 30:419–425
Selek U, Chang EL, Hassenbusch SJ 3rd, Shiu AS, Lang FF, Allen P, Weinberg J, Sawaya R, Maor MH (2004) Stereotactic radiosurgical treatment in 103 patients for 153 cerebral melanoma metastases. Int J Radiat Oncol Biol Phys 59:1097–1106
Manon R, O’Neill A, Knisely J, Werner-Wasik M, Lazarus HM, Wagner H, Gilbert M, Mehta M, Eastern Cooperative Oncology Group (2005) Phase II trial of radiosurgery for one to three newly diagnosed brain metastases from renal cell carcinoma, melanoma, and sarcoma: an Eastern Cooperative Oncology Group study (E 6397). J Clin Oncol 23:8870–8876
Dummer R, Goldinger SM, Turtschi CP, Eggmann NB, Michielin O, Mitchell L, Veronese L, Hilfiker PR, Felderer L, Rinderknecht JD (2014) Vemurafenib in patients with BRAF(V600) mutation-positive melanoma with symptomatic brain metastases: final results of an open-label pilot study. Eur J Cancer 50:611–621
Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, Schadendorf D, Dummer R, Smylie M, Rutkowski P, Ferrucci PF, Hill A, Wagstaff J, Carlino MS, Haanen JB, Maio M, Marquez-Rodas I, McArthur GA, Ascierto PA, Long GV, Callahan MK, Postow MA, Grossmann K, Sznol M, Dreno B, Bastholt L, Yang A, Rollin LM, Horak C, Hodi FS, Wolchok JD (2015) Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N Engl J Med 373:23–34
Ribas A, Puzanov I, Dummer R, Schadendorf D, Hamid O, Robert C, Hodi FS, Schachter J, Pavlick AC, Lewis KD, Cranmer LD, Blank CU, O’Day SJ, Ascierto PA, Salama AK, Margolin KA, Loquai C, Eigentler TK, Gangadhar TC, Carlino MS, Agarwala SS, Moschos SJ, Sosman JA, Goldinger SM, Shapira-Frommer R, Gonzalez R, Kirkwood JM, Wolchok JD, Eggermont A, Li XN, Zhou W, Zernhelt AM, Lis J, Ebbinghaus S, Kang SP, Daud A (2015) Pembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory melanoma (KEYNOTE-002): a randomised, controlled, phase 2 trial. Lancet Oncol 16:908–918
Nedzi LA, Kooy H, Alexander E 3rd, Gelman RS, Loeffler JS (1991) Variables associated with the development of complications from radiosurgery of intracranial tumors. Int J Radiat Oncol Biol Phys 21:591–599
Voges J, Treuer H, Sturm V, Büchner C, Lehrke R, Kocher M, Staar S, Kuchta J, Müller RP (1996) Risk analysis of linear accelerator radiosurgery. Int J Radiat Oncol Biol Phys 36:1055–1063
Aoyama H, Shirato H, Onimaru R, Kagei K, Ikeda J, Ishii N, Sawamura Y, Miyasaka K (2003) Hypofractionated stereotactic radiotherapy alone without whole brain irradiation for patients with solitary and oligo brain metastasis using noninvasive fixation of the skull. Int J Radiat Oncol Biol Phys 56:793–800
Ernst-Stecken A, Ganslandt O, Lambrecht U, Sauer R, Grabenbauer G (2006) Phase II trial of hypofractionated stereotactic radiotherapy for brain metastases: results and toxicity. Radiother Oncol 8:18–24
Vogelbaum MA, Angelov L, Lee SY, Li L, Barnett GH, Suh JH (2006) Local control of brain metastases by stereotactic radiosurgery in relation to dose to the tumor margin. J Neurosurg 104:907–912
Fahrig A, Ganslandt O, Lambrecht U, Grabenbauer G, Kleinert G, Sauer R, Hamm K (2007) Hypofractionated stereotactic radiotherapy for brain metastases–results from three different dose concepts. Strahlenther Onkol 183:625–630
Williams BJ, Suki D, Fox BD, Pelloski CE, Maldaun MV, Sawaya RE, Lang FF, Rao G (2009) Stereotactic radiosurgery for metastatic brain tumors: a comprehensive review of complications. J Neurosurg 111:439–448
Blonigen BJ, Steinmetz RD, Levin L, Lamba MA, Warnick RE, Breneman JC (2010) Irradiated volume as a predictor of brain radionecrosis after linear accelerator stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 77:996–1001
Minniti G, Clarke E, Lanzetta G, Osti MF, Trasimeni G, Bozzao A, Romano A, Enrici RM (2011) Stereotactic radiosurgery for brain metastases: analysis of outcome and risk of brain radionecrosis. Radiat Oncol 6:48
Yang HC, Kano H, Lunsford LD, Niranjan A, Flickinger JC, Kondziolka D (2011) What factors predict the response of larger brain metastases to radiosurgery? Neurosurgery 68:682–690
Minniti G, D’Angelillo RM, Scaringi C, Trodella LE, Clarke E, Matteucci P, Osti MF, Ramella S, Enrici RM, Trodella L (2014) Fractionated stereotactic radiosurgery for patients with brain metastases. J Neurooncol 117:295–301
Torres-Reveron J, Tomasiewicz HC, Shetty A, Amankulor NM, Chiang VL (2013) Stereotactic laser induced thermotherapy (LITT): a novel treatment for brain lesions regrowing after radiosurgery. J Neurooncol 113:495–503
Acknowledgments
We thank Professor Alessandro Bozzao, dr Andrea Romano and dr Guido Trasimeni, neuroradiologists, at Sant’Andrea Hospital, Neuroradiology Unit, for reviewing all MRI scans.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Rights and permissions
About this article
Cite this article
Minniti, G., Scaringi, C., Paolini, S. et al. Repeated stereotactic radiosurgery for patients with progressive brain metastases. J Neurooncol 126, 91–97 (2016). https://doi.org/10.1007/s11060-015-1937-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1937-4