Abstract
High-grade aneurysmal subarachnoid hemorrhage patients are monitored in the ICU for up to 21 days, as they are at risk for complications such as vasospasm of cerebral arteries, cardiac arrhythmias and neurogenic stress cardiomyopathy. The diagnosis of these treatable complications is often delayed by the limitations of monitoring capabilities. We applied computational analysis to a cohort of 24 aneurysmal subarachnoid hemorrhage patients, to identify heart rate variability and ECG frequency profiles that may be potential biomarkers of severe vasospasm, reversible cardiomyopathy and death.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Background
High-grade aneurysmal subarachnoid hemorrhage (SAH) patients are at risk for neurologic and cardiovascular complications. They warrant ICU monitoring for between 14 and 21 days as irreversible secondary brain injury can occur over a short period of time. These complications include delayed cerebral ischemia, vasospasm of cerebral arteries, cardiac arrhythmias, and neurogenic stress cardiomyopathy. The peak period for vasospasm (VSP) is 3–14 days after aneurysmal rupture, resolving usually by 14 and almost all by 21 days. Reversible stress cardiomyopathy (RCM) occurs early but is often delayed in its diagnosis (requiring a transthoracic echocardiogram). Treatment interventions include avoiding secondary brain injury from hypotension (as a result of low cardiac output states) using enlightened choices of vasopressors, amplification of blood pressure in impending delayed cerebral ischemia, and endovascular intervention for targeted vessel dilation. The challenges in timely detection and intervention lie in the insidious and subtle features of these complications at onset. The development of non-invasive indices for early detection of these complications is likely to improve patient outcomes.
There is a large body of literature that suggests that changes in heart rate variability (HRV) measures are associated with untoward clinical events and can be predictive of outcome [1–3]; the literature prior to 2011 is nicely reviewed by Mazzeo et al. [4]. ECG can reflect important characteristics of complex autonomic control. Indices reflecting sympatho-vagal imbalance (shifted adjustment between sympathetic and vagal activity) provides predictive value after stroke [5]. In a study of non-neurologic patients with RCM, HRV was decreased during the acute phase [6] relative to the chronic phase. Specifically in SAH, the acute (Day 1) phase has both increased sympathetic (catecholamines) and parasympathetic activity (perhaps associated with increased intracranial pressure after SAH onset) relative to the chronic phase (Day 30) that can be quantified using spectral analysis of HRV [7].
If the predictive value of a HRV measure depends on the relative comparison of acute vs chronic values, this would limit its online application in identifying treatable events with insidious or subtle clinical onset. Su et al. [8] showed that standalone intra-individual acute measures may have value in prediction of clinical events after SAH. An increasing slope of the ratio of low frequency/high frequency spectral power (LF/HF ratio) in the first 3 days after SAH ictus was a predictor of secondary complications (neurogenic pulmonary edema, symptomatic vasospasm, cerebral infarction, or death); interestingly, this pattern is also seen in myocardial infarction [8].
The present study is hypothesis generating, with the overall goal to identify biomarkers to facilitate early detection (as opposed to prediction) of post-SAH complications. Specifically, we evaluate intra-individual HRV features in a clinically annotated dataset of consecutive SAH patients.
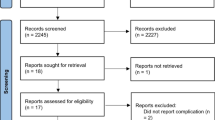
2 Methods
2.1 Monitoring and clinical data
Digital acquisition and storage of physiologic signals was protocolized in the Neurocritical Care Unit at the Hospital of the University of Pennsylvania in 2011. The clinical protocol includes severely brain injured patients who meet specific criteria (traumatic brain injury, subarachnoid hemorrhage, coma, and/or intracranial pressure monitoring). Data from 24 consecutively admitted SAH patients from 2011 to 2012 were analysed retrospectively for the purpose of this study, which was approved by the Institutional Review Board. Physiological signals were sampled at a frequency of 200 Hz. ECG was monitored continuously, and data was recorded using ICM + software (Cambridge Enterprise, Cambridge, UK, http://www.neurosurg.cam.ac.uk/icmplus/) or Component Neuromonitoring System (CNS Technology LLC, Ambler, PA), based on resource availability.
VSP-Rx was defined as angiographic vasospasm that was treated with targeted intra-arterial vasodilator therapy. RCM was identified by attending cardiologist clinical read of transthoracic echocardiograms, and diagnosis confirmed by observation of resolution of wall motion abnormalities.
2.2 Data analysis
Various time and frequency domain methods can be used to quantify HRV. An in-depth description of these methods can be found in a consensus guideline for the measurement and physiologic interpretation of ECG for clinical use [9].
We calculated HRV using both the time domain and frequency domain measures. Time domain measures included standard deviation of interbeat intervals (SDNN), root mean square of successive differences of interbeat intervals (RMSSD), coefficient of variation of interbeat intervals (CV of HR) and the Poincaré plot statistics SD1, SD2 and their ratio. Frequency domain measures included normalized LF power, normalized HF power, and LF/HF ratio (see Table 1).
To facilitate analysis of the ECG data, a custom GUI (Graphical User Interface) was developed in Matlab™. The GUI (Fig. 1a) allows users to view the raw time series data, to identify and remove outliers based on a statistical analysis of the data, automatically detect and confirm R-waves, compute HRV measures, and visualize the results of the HRV analysis. The design and implementation of the GUI was accomplished through an iterative process involving the engineering and clinical team members, and the final form of the GUI was customized to conveniently allow users to correlate the data and results to clinical meaningful findings. The GUI is capable of loading and automatically processing several days of recorded ECG data, and the results of the HRV analysis are saved to a single file for review and statistical analysis. HRV analysis was restricted to non-overlapping 300-s (5-min) epochs of ECG data, as is standard practice [9]. To correlate HRV analysis with time-stamped clinical data, a 60-min non-overlapping moving average filter was used to smooth the HRV results. To assist in correlating HRV analysis results with clinical data, a change point detection algorithm [10] was used to detect statistically significant changes in the HRV measures (Fig. 1b). The goal of change-point detection is to segment the time-series into epochs with stationary or statistically invariant properties. Then, the nonparametric statistical method developed by Brodsky [10], based on the model of the Brownian bridge process, is used to detect changes in the statistical characteristics of the signal.
a Screen shot of GUI with functionality for loading patient data, selecting epoch size, automated R-wave detection with the ability to remove outliers and real-time visualization of HRV statistics for the epoch under consideration; b Change point detection was incorporated into the GUI to facilitate correlation of patterns in HRV statistics. GUI contained functionality for selecting patient for analysis, HRV statistic and average window size, as well as displaying the timing of clinical events
Clinically meaningful outcomes were the following: severe vasospasm warranting endovascular intervention (VSP-Rx), RCM, and death. Because the highest risk for onset of VSP-Rx or RCM was in the relative time interval up to 1 week after aneurysm rupture, we focused our analyses on post bleed days (PBD) 0-7.
Our first goal was to determine if there were any visually apparent temporal relationships between changes in HRV measures and clinical outcomes that might support the future use of graphically displayed analyses in enhancing early detection. HRV measures for each subject were graphed against PBD and annotated for clinical events. They were individually inspected by 2 independent investigators (SP and FJ).
Our second goal was to determine if the absolute values of these analyses were correlated with clinical outcomes. Standard HRV measures were calculated using the program described above. HRV analyses for each patient resulted in data with non-normal distribution (ranging from 860 to 1,636 data points per patient); medians were calculated and taken as a distilled proxy for Absolute Value for PBD 0-7 (see Table 2). These single Absolute Values per patient were categorized by events including any event (7)/no event (6), VSP-Rx (3)/No VSP-Rx (10), RCM (5)/No RCM (8), and death (4)/no death (9). The category values were compared using unpaired t test.
Our last goal was to determine if there were any meaningful intra-subject patterns in HRV measures associated with the clinical outcomes. Change point analysis was used to determine the number of times the mean of a particular HRV statistic changed significantly over the time period of PBD 0-7. The results of HRV analyses on the smoothed measures were evaluated for change points that exceeded a set threshold. The average number of changes per data day in the mean of each HRV statistic was quantified in all patients. The number of change points were tallied for subject categories of Any event vs. No event, as well as Individual Specified event vs. No Individual Specified event (RCM, VSP-Rx, death). Differences between groups were compared using an unpaired t test.
For both Absolute Values and Change Point Analyses, the possibility of type 1 error was increased by the multiple comparisons made on a single data set. However, as this was hypothesis-generating work with the goal of identifying biomarkers for future study, we minimized false negatives by not statistically accounting for multiple comparisons.
3 Results
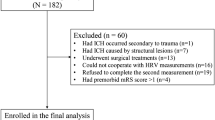
From a consecutive cohort of 24 high-grade SAH patients in a single neurointensive care unit, 11 were excluded from the final analysis because they did not have continuous data segments available for analysis for the majority of the time frame PBD 0-7. The remaining 13 patients were examined to determine if indices of HRV correlated with the occurrence of clinical events. Five patients experienced RCM (on PBD 0-7), and 3 were treated for VSP (on PBD 4-6). Two of the patients in these categories experienced both VSP-Rx and RCM. Four patients died between PBD 6-13 (including 2 of the RCM patients and 1 VSP-Rx patient).
3.1 Graphical display
Representative results that met subjective criteria of a meaningful trend or non-random pattern are displayed below.
In a SAH patient with RCM, we found a decrease in HRV that predated the discovery of cardiomyopathy as well as the onset of respiratory distress by several hours (see Fig. 2).
It was noted that the presence of events may correlate with a subjectively more non-random pattern, for example in CV of HR analyses of these SAH patients (see Fig. 3).
3.2 Absolute values
The only comparison that reached significance was RMSSD analysis; patients with RCM had a lower mean RMSSD over PBD 0-7 than those that did not experience RCM (p = 0.03) (see Table 3).
3.2.1 Mean change points (intra-subject patterns)
Patients with any clinically significant event (n = 7) had a higher frequency of changes in the mean as compared to patients without events (n = 6) for SDNN (1.3 ± 0.3 vs. 0.7 ± 0.4; p = 0.008) and CV (1.3 ± 0.3 vs. 0.7 ± 0.3; p = 0.005) and SD2 (1.1 ± 0.4 vs. 0.6 ± 0.3; p = 0.026). Statistically significant differences were not seen with average HR (1.3 ± 0.2 vs. 0.9 ± 0.5; p = 0.093), or RMSSD (1.0 ± 0.4 vs. 0.8 ± 0.3; p = 0.311).
In patients with VSP-Rx (n = 3), the frequency of mean changes was higher than in those without VSP-Rx (n = 10) for the following parameters: SDNN (1.5 ± 0.4 vs. 0.9 ± 0.4; p = 0.039), RMSSD (1.3 ± 0.2 vs. 0.8 ± 0.3; p = 0.006), CV (1.4 ± 0.3 vs. 0.9 ± 0.4; p = 0.037), SD1 (1.3 ± 0.3 vs. 0.8 ± 0.3; p = 0.014) and SD2 (1.2 ± 0.3 vs. 0.7 ± 0.3; p = 0.049). The frequency of change points differences in average HR was similar between the groups (p = 0.373).
The number of mean changes per day was greater in patients with RCM (n = 5) as compared to patients in this cohort without evidence of RCM (n = 8) for SDNN (1.4 ± 0.4 vs. 0.8 ± 0.4; p = 0.012), CV (1.4 ± 0.3 vs. 0.8 ± 0.3; p = 0.007) and SD2 (1.2 ± 0.3 vs. 0.6 ± 0.3; p = 0.005). No differences were observed between these groups for average HR (p = 0.093), RMSSD (p = 0.815) and SD1 (p = 0.183).
No significant differences were seen in the occurrence rate of mean changes in any of the HRV statistics examined over PBD 0-7 in patients who died as compared to those who survived. p values are as follows: average HR (p = 0.0359), SDNN (p = 0.500), RMSSD (p = 0.782), CV (p = 0.621), SD1 (p = 0.564) and SD2 (p = 0.752) (Table 4).
4 Discussion
The early clinical detection of untoward but treatable events after aneurysmal subarachnoid hemorrhage (including severe vasospasm and reversible cardiomyopathy) would be of tremendous clinical value. Our results suggest that there is promise in intra-individual ECG HRV analysis for the early detection of clinically important events.
We identified a decrease in the absolute value of RMSSD in patients who develop reversible cardiomyopathy after SAH. There is a physiologic rationale for monitoring RMSSD in patients at risk for RCM as this index reflects the integrity of vagal control of the heart; interestingly, lower values have been found to be associated with high risk scores in predictive models in Sudden Unexplained Death in People with Epilepsy [11]. Whether the critical threshold that distinguishes patients with RCM from those without exists between 0.01 and 0.03 needs to be proven by a larger sample size in a prospective study.
The ability of graphics to enhance human cognition in recognizing patterns in large data sets is well-acknowledged. Whether this could be superior to computational decision models has been questioned across domains [12–14]. Both independent investigators observed that the presence of clinical events in subjects was associated with a non-random appearance in the graphical representation of HRV analyses. This observation was supported in our data set by an increase in the frequency of change points that quantify statistically significant changes in mean HRV measures (a way of looking at the variability of variability) in subjects with untoward clinical events. Thus, in some cases it may be that the absolute value of a given parameter is not the key, but rather changes in values from their baseline levels that are associated with changes in clinical status.
Our pilot study is limited by the retrospective nature of our analyses, small sample size, multiple simultaneous statistical tests, and an incompletely annotated dataset (for confounders that may affect autonomic tone). This hypothesis-generating work allows us to focus future study on those HRV measures that suggest predictive value (i.e. RMSSD for absolute value threshold; SDNN, CV, and SD2 for change point analysis in RCM; SDNN, RMSSD, CV, SD1, and SD2 for change point analysis in VSP-Rx). Furthermore, as the present study is underpowered and subject to the possibility of additional type I error, validation of statistically significant differences will be evaluated in larger more appropriately powered future studies on a selected subset of HRV measures. Confounders that affect autonomic tone may pose a barrier for HRV indices in providing additional informative value beyond conventional clinical parameters. Whether this may be overcome could be tested using a larger, more complete and prospectively well-annotated dataset.
Baseline ECG visualization is universal in the ICU but pragmatically unfeasible to have human oversight at all times for all patients. Online computational analyses have already made the detection of ectopy and other arrhythmias feasible by linking such events to alarms, allowing intermittent and goal-directed attention [15–17]. The universal availability of cardiac telemetry in critical care units positions it as a high-yield target for further investigation of HRV analyses as the basis for clinical alarms.
References
Binici Z, Mouridsen MR, Kober L, Sajadieh A. Decreased nighttime heart rate variability is associated with increased stroke risk. Stroke. 2011;42:3196–201.
Moorman JR, Delos JB, Flower AA, Cao H, Kovatchev BP, Richman JS, Lake DE. Cardiovascular oscillations at the bedside: early diagnosis of neonatal sepsis using heart rate characteristics monitoring. Physiol Meas. 2011;32:1821–32.
Ryan ML, Ogilvie MP, Pereira BM, Gomez-Rodrigues JC, Manning RJ, Vargas PA, Duncan RC, Proctor KG. Heart rate variability is an independent predictor of morbidity and mortality in hemodynamically stable trauma patients. J Trauma. 2011;70(6):1371–80.
Mazzeo AT, La Monaca E, Di Leo R, Vita G, Santamaria LB. Heart rate variability: a diagnostic and prognostic tool in anesthesia and intensive care. Acta Anaesthesiol Scand. 2011;55:797–811.
Gunther A, Witte OW, Hoyer D. Autonomic dysfunction and risk stratification assessed from heart rate pattern. Open Neurol J. 2010;4:39–49.
Waldenborg M, Soholat M, Kahari A, Emilsson K, Frobert O. Multidisciplinary assessment of tako tsubo cardiomyopathy: a prospective case study. BMC Cardiovasc Disord. 2011;11:14.
Kawahara E, Ikeda S, Miyahara Y, Kohno S. Role of autonomic nervous dysfunction in electrocardiographic abnormalities and cardiac injury in patients with acute subarachnoid hemorrhage. Circ J. 2003;67(9):753–6.
Su IC, Li CH, Wang KC, Lai DM, Huang SJ, Shieh JS, Tu YK. Prediction of early secondary complications in patients with spontaneous subarachnoid hemorrhage based on accelerated sympathovagal ratios. Acta Neurochir (Wien). 2009;151(12):1631–7.
Task Force of The European Society of Cardiology and The North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation. 1996;93(5):1043–65.
Brodsky B, Darkhovsky B. Nonparametric methods in change-point problems. Dordrecht: Kluwer Academic Publishers; 1993.
DeGiorgio CM, Miller P, Meymandi S, Chin A, Epps J, Gordon S, Gornbein J, Harper RM. RMSSD, a measure of heart rate variability, is associated with risk factors for SUDEP: the SUDEP-7 inventory. Epilepsy Behav. 2010;19(1):78–81.
Stock D, Watson CJ. Human judgment accuracy, multidimensional graphics, and humans vs. models. J Account Res. 1984;22(1):192–206.
Lott JA, Durbridge TC. Use of Chernoff faces to follow trends in laboratory data. J Clin Lab Anal. 1990;4(1):59–63.
Wenkebach U, Pollwein B, Finsterer U (1992) Visualization of large datasets in intensive care. Proc Annu Symp Comput Appl Med Care 18–22.
Spann JF Jr, Moellering RC Jr, Haber E, Wheeler EO. Arrhythmias in acute myocardial infarction—a study utilizing an electrocardiographic monitor for automatic detection and recording of arrhythmias. N Engl J Med. 1964;271:427–31.
Julian DG, Valentine PA, Miller GG. Disturbances of rate, rhythm and conduction in acute myocardial infarction: a prospective study of 100 consecutive unselected patients with the aid of electrocardiographic monitoring. Am J Med. 1964;37:915–27.
Stock E, Goble A, Sloman G. Assessment of arrhythmias in myocardial infarction. Br Med J. 1967;2:719–23.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, S., Kaffashi, F., Loparo, K.A. et al. The use of heart rate variability for the early detection of treatable complications after aneurysmal subarachnoid hemorrhage. J Clin Monit Comput 27, 385–393 (2013). https://doi.org/10.1007/s10877-013-9467-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-013-9467-0