Abstract
Purpose
The development of secondary complications following spontaneous subarachnoid hemorrhage (SAH) largely depends on sympathetic overexcitation. The roles of vagal activities, however, are poorly defined. Because both components of the autonomic nervous system can be explored in the frequency domain of heart rate variability (HRV), the present study aimed to determine the dynamic evolution of autonomic activities and to identify patients at high risk for complications following hemorrhage.
Methods
Thirty patients with SAH were enrolled in our study. Those who suffered from symptomatic vasospasm, cerebral infarction, neurogenic pulmonary edema, or early mortality within 1 week of ictus were categorized into the complication group. Spectral analysis of HRV explored three important indices of sympathetic and vagal modulations: low-frequency (LF), high-frequency (HF), and LF/HF ratios. Patterns of HRV dynamics within the first 3 days were compared between complication and non-complication groups. The group trends, estimated by the slopes of HRV changes, were determined for further univariate and multivariate analysis.
Results
Our study showed that daily HRV in the complication group exhibited an approximately 2.7-fold increase of sympathovagal ratio (denoted by LF/HF). This resulted from reciprocal changes of sympathoexcitation (LF) and vagal withdrawal (HF). Multivariate analysis revealed that LF/HF slope, an indicator of the trend of sympathovagal change, was an independent variable significantly associated with the development of complications.
Conclusions
This study confirmed that during early SAH period, patients with and without complications presented different patterns of sympathovagal changes. LF/HF slope during the first 3 days was a significant predictor of secondary complications after SAH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Treatment of subarachnoid hemorrhage (SAH) remains challenging in neurocritical care. Those who survive the initial hemorrhage are still susceptible to secondary complications, including rebleeding, cardiopulmonary compromise, neurogenic pulmonary edema, and delayed ischemic neurological deficits [15, 18, 22]. Because some secondary insults are potentially treatable with good outcomes, patients might benefit from intensive monitoring and management if a high-risk group could be identified early after SAH.
Early morbidity in patients with SAH is dependent on the extent of autonomic dysregulation. Most studies have focused on sympathoexcitations. Naredi et al. reported that SAH patients exhibited an approximately three-fold increase in norepinephrine spillover within 48 h after insult [19]. Benedict and Loach reported that norepinephrine concentration was particularly increased in SAH patients with poor outcomes [5]. The importance of parasympathetic dysregulation, however, is poorly defined, probably because vagal activities are not measurable in routine laboratories. Because cardiac rhythms are mainly affected through the interplay of the sympathetic and vagal outflows, fluctuation of heart rate provides important information about autonomic nervous system (ANS) [2]. Based on measuring intervals of consecutive R-wave peaks, spectral analysis of heart rate variability (HRV) has become a well-established method for estimating both components of ANS activities.
Autonomic components can be explored in the frequency domain of HRV [2, 17]. Previous studies have demonstrated that the power of the high-frequency (HF) band reflected parasympathetic modulations of cardiac rhythm, whereas low-frequency (LF) power denoted predominantly sympathetic modulations. The LF-to-HF ratio (LF/HF) is commonly regarded as an index of sympathovagal balance. In other words, HRV analysis appears to offer a noninvasive and quantitative evaluation of sympathovagal interactions.
In the present report, we adapted this powerful technique to examine the autonomic alterations following SAH. The objective of this study was to assess differential profiles of autonomic modulations between SAH patients with and without complications and to identify significant predictors of secondary complications.
Materials and methods
Study population
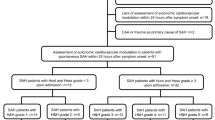
From April 2008 to January 2009, we enrolled patients with SAH of non-traumatic origin who were admitted to the Department of Neurosurgery, National Taiwan University Hospital, within 24 h of onset. The diagnosis of SAH was based on non-contrast computed tomography (CT) imaging. Locations of the ruptured aneurysms were confirmed either by conventional cerebral angiography or three-dimensional CT angiography. Patients with prior cardiac disease or autonomic dysfunctions were excluded. Informed consent was obtained from the patients or, in case of unconsciousness, from a family member. The local Ethics Committee approved the protocol.
On admission, demographic characteristics, clinical severities, and radiological images were recorded. Degree of neurological severity was classified by following the World Federation of Neurosurgical Societies (WFNS) grading system [1]. WFNS grades I, II, and III were defined as low grade, whereas grades IV and V were defined as high grade.
Patient management
All patients underwent early aneurysm treatment within 48 h, when feasible. All patients underwent continuous monitoring of arterial blood pressure and cardiac status by electrocardiography (ECG). Patients were evaluated hourly for neurological signs. Arterial blood gas levels were assessed daily in the first week after SAH. All patients received nimodipine for prevention of cerebral vasospasm.
Definition of primary outcome
Complications following SAH varied in severity. The present study focused only on severe complications that occurred within the first week after SAH. These included neurogenic pulmonary edema, symptomatic vasospasm, cerebral infarction, and death. The diagnosis of neurogenic pulmonary edema was defined as the presence of a butterfly pattern of the pulmonary field with a cardiothoracic ratio below 50% on the chest film and arterial blood gas showing hypoxia and respiratory alkalosis that required endotracheal intubation and controlled mechanical ventilation [18]. Clinical criteria of symptomatic vasospasm included both the presence of neurological deterioration and arterial narrowing on CT angiography and/or conventional cerebral angiography. For patients who developed cerebral infarction, low-density regions of a certain arterial territory were demonstrated by noncontrast CT scanning.
Assessment of HRV
-
1.
Data acquisition
ECG signals were exported to a personal computer via a data-acquisition card (DAQ Card-6024E), with a sampling rate of 500 Hz. All data were divided and stored in 60-min intervals for off-line analysis. Recordings started from the day of admission (day 1) to day 3.
-
2.
Sampling of representative ECG data
Data recorded during day time (09:00–17:00 hours) were chosen for analysis because HRV has been reported to have circadian differences [7]. For every patient, three segments of non-successive 5-min recordings of stationary ECG were chosen per day for further spectral analysis. ECG recordings were excluded if more than 5% of the recorded segments had nonsinus rhythm, ectopic beats, or noise.
-
3.
Generation of RR interval sequence
The procedure of HRV analysis was designed according to the guidelines outlined by the task force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology [2]. R waves were detected automatically by using a threshold-plus-derivative method, followed by manual verification and correction. All ectopic and other nonsinus beats were excluded and replaced with interpolative RR interval data. The generated RR interval sequence was irregularly sampled in time, so cubic interpolation was used for resampling with a rate of 2 Hz.
-
4.
Frequency-domain analysis
Three major HRV parameters, including LF power, HF power, and LF/HF, were computed using an HRV analysis toolkit (version 1.1, Kuopio, Finland) [20]. In brief, after the ectopic-free data were detrended and resampled, the power spectral density of each 5-min recording was estimated using the fast Fourier transform (FFT) algorithm. The FFT parameters were based on a Welch periodogram with a Hanning window width of 1,024 points and an overlap of 512 points.
The power spectra were quantified into the standard frequency-domain measurements, including very low frequency (VLF) (0.003–0.04 Hz), LF (0.04–0.15 Hz), and HF (0.15–0.40 Hz) power. To minimize the effect on the values of LF and HF components of the changes in total power (TP), normalized HF (HF(n)) and LF (LF(n)) power components were measured in normalized units, which represent the value of each power component divided by TP minus VLF components [2]. HF(n) was mediated by parasympathetic modulation to the sinus, and LF(n) was mediated by sympathetic modulations predominantly with various vagal components. The ratio of LF/HF power was measured as an index of sympathovagal balance. To minimize the error imposed by the analysis of short segments of ECG, the mean value of each parameter was then obtained from the three 5-min segments on each day [2].
-
5.
Dynamic changes of HRV indices
Malik et al. demonstrated that specific spectral components of HRV were merely markers of the autonomic influences on the modulations of heart rate, but not direct measurements of the autonomic tones [16]. Therefore, HRV indices themselves were probably not comparable between patients in different physiological conditions. Therefore, in the present study, we attempted to determine the dynamic changes of HRV indices in the same patient but did not compare HRV indices between different patients. We regarded LF(n) on day 1 as the baseline value. The ratios of LF(n) on day 2 and day 3 to baseline value were then measured to evaluate the extent of LF changes. The same procedure was also applied to HF(n) and LF/HF.
The amount of change from day 1 to day 3 in each HRV parameter was estimated using the least squares regression line. The slopes of these three lines, labeled as LF-slope, HF-slope, and LF/HF slope, were thus determined to represent the trend of HRV changes.
Statistical analysis
All data were expressed as median and their 25th–75th percentile. Comparisons between HRV parameters on day 2 and day 1 (or day 3 and day 1) in the same group were performed using the paired Wilcoxon signed rank test. Numerical (age, slopes of HRV parameters) and categorical variables (sex, WFNS grading) were compared between the complication and non-complication groups by using the Wilcoxon signed-rank test and Fisher exact test, respectively. To investigate whether the trend of sympathovagal balance was an independent predictor of severe complications, we applied logistic regression multivariate analysis to adjust for baseline age, sex, and WFNS grade. A probability value of less than 0.05 was defined as statistically significant. Data were analyzed with commercially available software Number Crunching Statistical System (NCSS) 2004 (NCSS Inc., Kaysville, UT).
Results
Demographic data
A total of 30 patients fulfilled the inclusion criteria and were enrolled in the present study. There were 11 men and 19 women with a median age of 52 years. The clinical severity of SAH was high in half of the subjects. Eighteen patients underwent aneurysm clipping, and seven underwent embolization of their aneurysms. The following 17 complications were observed in 16 patients in decreasing order of frequency: cerebral infarctions (six patients), early death (four patients), neurogenic pulmonary edema (four patients), and symptomatic vasospasm (three patients). The median duration between SAH and the diagnosis of a complication (or death) was 4 days (25th–75th percentile, 3–5 days). Table 1 summarizes the demographic data, aneurysm locations, treatment of choice, and occurrence of complications in all patients.
Daily HRV values exhibited different trends in both groups, as shown in Fig. 1. Compared to HRV parameters on day 1, patients with complications showed a significantly higher LF(n) on day 2 (1.31-fold, 25th–75th percentile: 0.95 ∼ 1.67, p = 0.01) and day 3 (1.35-fold, 25th–75th percentile: 1.05 ∼ 1.71, p = 0.01). HF(n) significantly reduced on day 2 (0.56-fold, 25th–75th percentile: 0.38 ∼ 1.09, p < 0.01) and day 3 (0.51-fold, 25th–75th percentile: 0.38 ∼ 0.96, p = 0.01). Reciprocal changes of LF(n) and HF(n) resulted in an approximately 2.7-fold increase of LF/HF on day 2 (p < 0.01) and day 3 (p < 0.01), a statistically significant change. In contrast, no significant changes of HRV indices were observed on day 2 and day 3 in non-complication group.
Differential patterns of LF(n), HF(n), and LF/HF from post-SAH day 1 to day 3 in the complication and noncomplication groups. Evolutions of three HRV indices among two groups were significantly different. All data were expressed as median and interquartile range with day 1 value defined as 1. * p < 0.01 versus day 1; # p = 0.01 versus day 1 by paired Wilcoxon signed-rank test
When SAH patients with and without complications were compared (Table 2), neither group differed in terms of age, sex, and WNFS grading. Using Wilcoxon signed-rank test, the only two variables with significant group differences were HF slope and LF/HF slope. In the complication group, HF slope was more negative (−0.21 versus −0.04, p = 0.02), whereas LF/HF slope was much more positive (0.80 versus 0.09, p = 0.03). In the multivariate analysis (Table 3), high WFNS grades (odds ratio: 11.47, p = 0.04) and LF/HF slope (odds ratio: 14.98, p = 0.02) were independent variables significantly associated with the development of complications.
Discussions
HRV, which can be quantified in frequency domain, was determined by the complex interplay between sympathetic and vagal activities [17]. We applied a spectral technique to analyze daily HRV in patients with SAH to identify individuals at high risk for subsequent complications. The major findings of this study were as follows. During the early SAH period, patients with and without complications presented with different patterns of sympathovagal changes. The LF/HF slope, representative of the trend of sympathovagal change, was a significant predictor of subsequent complications.
Sympathetic overexcitation has been etiologically correlated with various kinds of complications following SAH. Dilraj et al. found that cerebrospinal fluid catecholamine levels were higher in SAH patients complicated with cerebral vasospasm [8]. Excessive secretion of catecholamines has also been reported in patients with cardiac compromise or neurogenic pulmonary edema after SAH [15, 18]. Similar results were also shown in our series. LF(n) power, an index of sympathetic modulation, exhibited an 1.3-fold increase in the complication group on day 2 and day 3 after SAH. In contrast, LF(n) power in the non-complication group remained similar within the first 3 days. All these results implied the presence of a strong correlation between sympathetic acceleration and secondary complications following SAH. Though the causal relationships between them were not clear, sympathoexcitation-induced cerebral vasospasm, neurogenic pulmonary edema, and other possible complications have been demonstrated in numerous animal studies [15]. In our study, LF(n) obviously increased before complications occurred. Based on these findings, we hypothesized that sympathetic over-excitation was important in determining subsequent complication events. The reasons why the acceleration rate of sympathetic activities, denoted by LF slope, had no significant group differences were not clear. Possible explanations included: (1) a larger number of subjects may be required to demonstrate statistical significance. (2) Increased sensitivity of target organs to sympathetic activities have been noticed in experimental SAH models even though the catecholamine levels were not higher [9, 13]. In this situation, measurement of LF(n) or plasma catecholamine would fail to demonstrate sympathetic hyperexcitation. (3) The meaning of LF(n) remained equivocal. In some conditions, it was regarded as the marker of sympathetic activity predominantly, while in others, it seemed to be modulated by both sympathetic and parasympathetic activities [2]. In the latter situation, the increase of sympathetic activity in combination of a reduction of vagal activity would result in an unpredictable change of LF(n).
The role of the parasympathetic nervous system in SAH remains obscure clinically. In animal studies, vagal stimulations have been shown to decrease or prevent secondary insults to some extents. Excitation of vagal activities via sphenopalatine ganglion stimulation [24] or transcorneal stimulation of trigeminal nerve afferents [3] have been shown to reverse cerebral vasospasm in canine and rat models of SAH. In contrast, acute vagal withdrawal by bilateral vagotomy was able to generate profound neurogenic pulmonary edema [6, 10]. Though these findings were not directly comparable to clinical conditions, our results concurred with these animal experiments in that patients with complications exhibited a significant decrease of HF(n). This reduction was absent in non-complication group. Besides, we also demonstrated that the reduction rate of HF(n) in complication group, denoted by HF-slope, was much greater compared to that in non-complication group. Ŝvigelj et al. who examined 22 SAH patients with uneventful courses, also showed a steady pattern of HF power in the first 3 days after SAH [21]. We could therefore propose that in addition to sympathetic excitation, vagal reduction during early SAH period was possibly another contributing factor to the genesis of complications.
The reciprocal nature of the sympathetic and parasympathetic nervous systems raised the important issue of overall autonomic balances, which could be estimated by LF/HF. Results of the present study showed that sympathovagal balance in the complication group exhibited an approximately 2.7-fold increase on the second day after SAH. This was attributed to a simultaneous acceleration of sympathetic modulations (i.e., LF(n)) and an abrupt declination of vagal influences (i.e., HF(n)) on day 2 and day 3. As for the non-complication group, LF/HF remained similar from day 1 to day 3. In univariate analysis, LF/HF slope was significantly higher in the complication group. After adjusting for other clinical variables, LF/HF slope and WFNS grade were the only two significant predictors of the subsequent complications. These results strongly suggested that when measuring ANS activities, not only sympathetic activities but also vagal tones should be taken into consideration. Therefore, we believed that the predictive value of sympathovagal ratio would be higher during the early period of SAH.
Our findings raised another well-known issue in that ECG abnormalities were common following SAH [11, 12]. Typical ECG changes in the acute phase of SAH, including ST elevations and QT prolongation, mimicked ECG findings in acute myocardial infarction (AMI). Interestingly, HRV spectral profiles in our complication group, characterized by increases in LF(n) component and in LF/HF ratio, were also similar to those in the early hours of true AMI attacks [14]. These findings suggested that both physiological conditions shared a common autonomic dysregulation, that was, a prevailing sympathetic augmentation and parasympathetic inhibition. The possibility of mis-interpretation between SAH and AMI could not be over emphasized.
There were several limitations to this study. First of all, a larger study population was mandatory to validate our hypotheses. Secondly, the underlying mechanisms of autonomic dysregulations following SAH were largely unknown. Although a possible explanation was the differential ischemic injury to the hypothalamus, there was no strong evidence to support this hypothesis [8, 23]. Finally, it was important to mention that HF was significantly related to the respiratory sinus rhythm. According to Aysin et al., HF power was proportional to the fundamental respiratory frequency (FRF); that was, FRF*0.65 to FRF*1.35 [4]. Therefore, a slow respiration rate, for example six per minute (i.e., FRF = 0.1), can cause an erroneous increase in the predefined area of LF power and misinterpretation of sympathetic hyperactivity. However, for a normal breathing rate around 10 ∼ 16 per minute, the FRF ranged from 0.16 ∼ 0.26. The resulting HF area calculated from FRF therefore resided mainly within the default HF area (i.e., 0.15 ∼ 0.40 Hz). In our series, 20 out of 30 patients were mechanically ventilated during the ECG recording. All patients, whether intubated or not, had a breathing rate ranging from 10 ∼ 18 per minute. Therefore, we hypothesized that our results remained valid in consideration of respiration effects. However, we still believed that integrating respiratory signals into spectral analysis of HRV could provide a more accurate interpretation in human autonomic nervous activities.
Despite these uncertainties, we concluded that spectral analysis of HRV provided important information regarding ANS dynamics during the early SAH period. Investigation of the possible relationships between HRV indices and secondary complications revealed that both sympathetic overexcitation and vagal withdrawal might contribute to the genesis of complications after SAH. Although the exact cause of different autonomic dysregulations following SAH remains unclear, measurements of the LF/HF slope after admission might assist clinical assessment in identifying patients at high risk for early secondary complications.
References
(1988) Report of World Federation of Neurological Surgeons Committee on a Universal Subarachnoid Hemorrhage Grading Scale. J Neurosurg 68:985–986
(1996) Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J 17:354–381
Atalay B, Bolay H, Dalkara T, Soylemezoglu F, Oge K, Ozcan OE (2002) Transcorneal stimulation of trigeminal nerve afferents to increase cerebral blood flow in rats with cerebral vasospasm: a noninvasive method to activate the trigeminovascular reflex. J Neurosurg 97:1179–1183
Aysin B, Aysin E (2006) Effect of respiration in heart rate variability (HRV) analysis. Conf Proc IEEE Eng Med Biol Soc 1:1776–1779
Benedict CR, Loach AB (1978) Clinical significance of plasma adrenaline and noradrenaline concentrations in patients with subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry 41:113–117
Berry D, Ikegami M, Jobe A (1986) Respiratory distress and surfactant inhibition following vagotomy in rabbits. J Appl Physiol 61:1741–1748
Bilan A, Witczak A, Palusinski R, Myslinski W, Hanzlik J (2005) Circadian rhythm of spectral indices of heart rate variability in healthy subjects. J Electrocardiol 38:239–243
Dilraj A, Botha JH, Rambiritch V, Miller R, van Dellen JR (1992) Levels of catecholamine in plasma and cerebrospinal fluid in aneurysmal subarachnoid hemorrhage. Neurosurgery 31:42–50 discussion 50–41
Edvinsson L, Egund N, Owman C, Sahlin C, Svendgaard NA (1982) Reduced noradrenaline uptake and retention in cerebrovascular nerves associated with angiographically visible vasoconstriction following experimental subarachnoid hemorrhage in rabbits. Brain Res Bull 9:799–805
Goldenberg VE, Buckingham S, Sommers SC (1967) Pulmonary alveolar lesions in vagotomized rats. Lab Invest 16:693–705
Kawahara E, Ikeda S, Miyahara Y, Kohno S (2003) Role of autonomic nervous dysfunction in electrocardio-graphic abnormalities and cardiac injury in patients with acute subarachnoid hemorrhage. Circ J 67:753–756
Lanzino G, Kongable GL, Kassell NF (1994) Electrocardiographic abnormalities after nontraumatic subarachnoid hemorrhage. J Neurosurg Anesthesiol 6:156–162
Lobato RD, Marin J, Salaices M, Rivilla F, Burgos J (1980) Cerebrovascular reactivity to noradrenaline and serotonin following experimental subarachnoid hemorrhage. J Neurosurg 53:480–485
Lombardi F, Sandrone G, Spinnler MT, Torzillo D, Lavezzaro GC, Brusca A, Malliani A (1996) Heart rate variability in the early hours of an acute myocardial infarction. Am J Cardiol 77:1037–1044
Macmillan CS, Grant IS, Andrews PJ (2002) Pulmonary and cardiac sequelae of subarachnoid haemorrhage: time for active management? Intensive Care Med 28:1012–1023
Malik M, Camm AJ (1993) Components of heart rate variability–what they really mean and what we really measure. Am J Cardiol 72:821–822
Malliani A, Pagani M, Lombardi F, Cerutti S (1991) Cardiovascular neural regulation explored in the frequency domain. Circulation 84:482–492
Muroi C, Keller M, Pangalu A, Fortunati M, Yonekawa Y, Keller E (2008) Neurogenic pulmonary edema in patients with subarachnoid hemorrhage. J Neurosurg Anesthesiol 20:188–192
Naredi S, Lambert G, Eden E, Zall S, Runnerstam M, Rydenhag B, Friberg P (2000) Increased sympathetic nervous activity in patients with nontraumatic subarachnoid hemorrhage. Stroke 31:901–906
Niskanen JP, Tarvainen MP, Ranta-Aho PO, Karjalainen PA (2004) Software for advanced HRV analysis. Comput Methods Programs Biomed 76:73–81
Svigelj V, Grad A, Kiauta T (1996) Heart rate variability, norepinephrine and ECG changes in subarachnoid hemorrhage patients. Acta Neurol Scand 94:120–126
van Gijn J, Kerr RS, Rinkel GJ (2007) Subarachnoid haemorrhage. Lancet 369:306–318
Wilkins RH (1975) Hypothalamic dysfunction and intracranial arterial spasms. Surg Neurol 4:472–480
Yarnitsky D, Lorian A, Shalev A, Zhang ZD, Takahashi M, Agbaje-Williams M, Macdonald RL (2005) Reversal of cerebral vasospasm by sphenopalatine ganglion stimulation in a dog model of subarachnoid hemorrhage. Surg Neurol 64:5–11 discussion 11
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
Neurointensive care after subarachnoid hemorrhage is challenging, and many patients still suffer from secondary complications not reliably predictable by routine assessment. Spectral analysis of the patients' heart rate variability potentially is a first step in this direction. On the other hand, one has to consider that the present study only provides results with restricted expressiveness, as also discussed by the authors. However, it seems to be of value to perform further studies with more patients.
Marcus Reinges
Aachen, Germany
Rights and permissions
About this article
Cite this article
Su, IC., Li, CH., Wang, KC. et al. Prediction of early secondary complications in patients with spontaneous subarachnoid hemorrhage based on accelerated sympathovagal ratios. Acta Neurochir 151, 1631–1637 (2009). https://doi.org/10.1007/s00701-009-0517-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-009-0517-9