Abstract
Background
Although abnormal heart rate variability (HRV) is frequently observed in patients with spontaneous intracerebral hemorrhage (ICH), its time course and presentation of different indices remain unclear, and few studies have focused on its association with clinical outcomes.
Methods
We prospectively recruited consecutive patients with spontaneous ICH between June 2014 and June 2021. HRV was evaluated twice during hospitalization (within 7 days and 10–14 days after stroke). Time and frequency domain indices were calculated. A modified Rankin Scale score ≥ 3 at 3 months was defined as a poor outcome.
Results
Finally, 122 patients with ICH and 122 age- and sex-matched volunteers were included. Compared with controls, time domain and absolute frequency domain HRV parameters (total power, low frequency [LF], and high frequency [HF]) in the ICH group were significantly decreased within 7 days and 10–14 days. For relative values, normalized LF (LF%) and LF/HF were significantly higher, whereas normalized HF (HF%) was significantly lower, in the patient group than in the control group. Furthermore, LF% and HF% measured at 10–14 days were independently associated with 3-month outcomes.
Conclusions
HRV values were impaired significantly within 14 days after ICH. Furthermore, HRV indices measured 10–14 days after ICH were independently associated with 3-month outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spontaneous intracerebral hemorrhage (ICH) represents 10–15% of all types of stroke worldwide but is associated with significantly higher rates of mortality and disability. It is estimated that 50% of patients with ICH die within the first 30 days after onset and that two thirds of survivors remain moderately or even severely disabled [1,2,3]. Although the high burden of this disease has been recognized, there are disproportionately few proven prognostic predictors and effective treatment targets for improving clinical outcomes in patients with ICH.
Heart rate variability (HRV), the beat‐by‐beat variance in heart rate, is regarded as a noninvasive indicator of autonomic nervous system modulation [4]. Since the association between post infarction mortality and reduced HRV in patients with myocardial infarction was first found in 1977 by Wolf et al., HRV was confirmed in the late 1980s and early 1990s to be significantly and independently predictive of mortality after an acute myocardial infarction [5,6,7,8]. During the past 30 years, an increasing number of studies have related the imbalance of the autonomic nervous system (as assessed by HRV) to cardiovascular disease [9]. Taking into consideration strict heart–brain relationships, HRV assessment has been widely used as an important and robust diagnostic tool in the detection of autonomic impairment and prediction of prognosis in several neurological disorders, such as cerebrovascular diseases, multiple sclerosis, Parkinson disease, and epilepsy [10]. Previous studies have reported impaired autonomic function in patients with ICH, and it is associated with functional outcomes and mortality in these patients [11, 12]. Therefore, theoretically, HRV may present significant alternations after ICH onset; however, few studies have focused on the association between HRV and ICH.
Hence, the main objective of this study was to investigate (1) the time course and characteristics of HRV in patients with ICH and (2) the association between HRV and clinical outcomes.
Methods
Patient Selection and Study Protocol
Patients with spontaneous ICH presenting to the Stroke Center in the Department of Neurology at the First Hospital of Jilin University between June 2014 and June 2021 were prospectively and consecutively enrolled in this observational cohort study. Our center is the National Advanced Stroke Center verified by the National Health Commission, the highest level of stroke center in China, and houses the Key Laboratory of Cerebrovascular Disease Precision Medicine of Jilin Province. The inclusion criteria were as follows: (1) age 18–80 years, (2) premorbid modified Rankin Scale (mRS) score ≤ 1, (3) computed tomography images showing ICH, and (4) initial HRV measurements completed within 7 days after ictus. We excluded patients (1) whose ICH occurred secondary to trauma, hemorrhagic conversion of ischemic stroke, or structural lesions (i.e., aneurysm, tumor, arteriovenous malformation, and vasculitis); (2) who underwent any surgical treatments, including ventricular drainage, clot removal, and craniotomies, during hospitalization; (3) with a medical history that may undermine hemodynamic stability, such as current arrhythmia, hyperthyroidism, and anemia; and (4) who were unable to complete all HRV measurements. During the same period, age-matched (± 2 years) and sex-matched medically and psychiatrically healthy volunteers were selected as controls at a ratio of 1:1. All participants or their direct relatives provided written informed consent for this study, which was approved by the Ethics Review Committee of the First Hospital of Jilin University (2017-042).
For each patient with ICH, HRV measurements were performed twice during hospitalization: within 7 days and 10–14 days after stroke onset. HRV measurements were performed once for each control participant. The clinical outcome was the mRS score at 3 months, which was collected via telephone interview with participants or their relatives by an examiner who was blinded to the HRV results. An mRS score of ≥ 3 was defined as a poor outcome, and an mRS score of ≤ 2 was defined as a good outcome.
Data Collection
Baseline characteristics, including demographic information (age and sex), lifestyle history (alcohol consumption and cigarette smoking), and medical history (hypertension, diabetes mellitus, previous stroke, and antihypertensive medication history), were documented. Previous stroke was defined as a history of transient ischemic attack, ischemic stroke, ICH, or subarachnoid hemorrhage [13].
Documented clinical data included ICH severity, blood pressure, heart rate, medications, and imaging data. Clinical severity on admission was evaluated using National Institutes of Health Stroke Scale (NIHSS) scores. Blood pressure and heart rate were measured from the brachial artery using an automatic blood pressure monitor (Omron 711, Japan). Imaging data, including hematoma location, ICH volume, the presence of intraventricular hemorrhage, perihematomal edema, and midline shift, were measured from the initial computed tomography (64-slice, Somatom Definition; Siemens Healthcare, Germany) scan on admission for each patient by a neuroradiologist blinded to the HRV parameters and clinical outcomes. The ICH volume was measured as delineated by the ABC/2 score [14]. Perihematomal edema was rated using the five-point visual rating scale reported by Lietke et al. [15]. Midline shift ≥ 3 mm was defined as positive [16]. Additionally, computed tomography images were reexamined one day before discharge, and hematoma enlargement was defined as an absolute hematoma volume increase > 6 mL or relative hematoma volume increase > 33% [17].
Measurements of HRV
HRV was evaluated by noninvasively measuring beat-to-beat signals for 5 min using a servo-controlled plethysmograph (Finometer model 1, FMS, Rotterdam, the Netherlands) placed on the middle finger. All investigations were performed in a quiet examination room with a controlled temperature ranging from 20 to 24 °C between 9:00 and 10:00 a.m. All participants were asked to relax in a supine position for 10 min in the room before the examination.
Beat-to-beat recordings were processed as previously reported [18]. Briefly, scripts developed by the research team in MATLAB (R2017b, MathWorks, USA) were used to detect inflection points and to identify each cardiac cycle [19]. Ectopic beats and artifacts were automatically detected, visually reviewed, and removed using linear interpolation [20]. HRV indices were evaluated in the time and frequency domains. Values in the time domain were evaluated as the standard deviation of all normal-to-normal intervals (SDNN), the most widely used time domain HRV values. The coefficient of variance of normal-to-normal intervals (CV), calculated as the ratio of SDNN and mean normal-to-normal intervals, was also calculated to eliminate the effects of mean levels [21]. The power spectra were quantified using the Welch method, based on a fast Fourier transform, by measuring the areas in the following frequency power bands: very low frequency (VLF) (< 0.04 Hz), low frequency (LF) (0.04–0.15 Hz), and high frequency (HF) (0.15–0.40 Hz) bands and total power (TP) (< 0.40 Hz). The variables in the frequency domain were expressed in absolute patterns (power of TP, VLF, LF, and HF [ms2]) and relative patterns (normalized LF and HF [LF% and HF%] and the ratio of LF to HF [LF/HF]) in accordance with international guidelines [22]. Table 1 shows the methods used to calculate these indices and their physiological correlates.
Statistical analysis
All statistical analyses were performed using SPSS version 26.0 (SPSS; IBM, West Grove, PA). The distribution of data was assessed using a one-sample Kolmogorov–Smirnov test. The mean value ± standard deviation was calculated for normally distributed continuous variables, whereas the median (interquartile range) was calculated for non-normally distributed variables. Categorical variables were evaluated as frequencies. HRV indices measured within 7 days and 10–14 days after stroke onset were compared using the Wilcoxon signed-rank test. The Mann–Whitney U-test was used to compare data between the patient and control groups. The baseline characteristics and HRV parameters of patients with ICH were categorized according to patient outcomes. Normally distributed data were analyzed using Student’s t-test. Non-normally distributed data were compared using the Mann–Whitney U-test. χ2 or Fisher’s exact tests were used to compare categorical variables.
To explore the correlation between HRV and clinical outcomes, four models were applied in the sensitivity analysis: model 1 was unadjusted, model 2 was adjusted for age and sex, model 3 was adjusted for all variables in model 2 plus lifestyle history and medical history (including cigarette smoking, alcohol consumption, hypertension, diabetes mellitus, previous stroke, and antihypertensive medication history), and model 4 was adjusted for all variables in model 3 plus clinical data (including admission NIHSS score, systolic and diastolic blood pressure, antihypertensive and dehydration drugs, ICH location, ICH volume, presence of intraventricular hemorrhage, perihematomal edema, midline shift, and hematoma enlargement). Only the statistical results that were consistent in all four models were considered conclusive. All tests were two-tailed, and p values < 0.05 were considered statistically significant.
Results
Overall, 182 patients were recruited initially. One patient with ICH that occurred secondary to trauma, seven patients with ICH caused by structural lesions (two with tumor and five with arteriovenous malformation), 13 patients who underwent surgical treatments, and 16 patients who could not cooperate with HRV measurements because of arrhythmia and hyperthyroidism were excluded. Nineteen patients who refused to complete the second measurement and four patients who had premorbid mRS scores > 1 were also excluded. The flowchart is shown in Fig. 1. Finally, 122 patients with ICH (54.7 ± 10.0 years; 78.3% male) and 122 age- and sex-matched healthy adults (55.6 ± 12.0 years; 78.3% male) were included in the analysis. Table 2 shows demographic and clinical information for patients with ICH.
Temporary Course of HRV in Patients with ICH
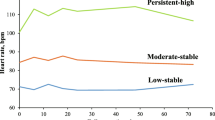
As shown in Table 3 and Fig. 2, when compared with healthy controls, patients with ICH exhibited significantly decreased SDNN, CV, TP, LF, and HF within 7 days after onset. LF% and LF/HF were significantly higher, whereas HF% was significantly lower, in the patient group than in the control group. These HRV impairments were sustained 10–14 days after onset in the ICH group, who exhibited lower SDNN, CV, TP, VLF, LF, HF, and HF%, as well as higher LF% and LF/HF, than healthy adults at 10–14 days after onset. Moreover, when we compared HRV data obtained within 7 days and 10–14 days after onset, no recovery phenomenon was observed. Conversely, abnormal HRV tended to progress, although the changes were not significant.
Association Between HRV and Clinical Outcomes
Among the 122 patients with ICH, 83 (68.0%) experienced good outcomes, whereas 39 (32.0%) experienced poor outcomes. The demographic and clinical information of patients with different outcomes is shown in Table 4. Patients in the poor outcome group had higher admission NIHSS scores (10.0 vs. 4.0, p < 0.001) and larger ICH volumes (15.6 vs. 8.7 mL, p < 0.001) than those in the good outcome group. The distribution of perihematomal edema scores in patients with good and poor outcomes was significantly different. Furthermore, the proportion of patients with midline shift and hematoma enlargement was significantly higher in patients with poor outcomes. No significant differences in other baseline characteristics were observed (all p > 0.1).
Table 4 also shows HRV data for the two groups. At 10–14 days after onset, patients with poor outcomes exhibited significant increases in LF% (51.7 vs. 41.5, p = 0.004) and LF/HF (1.1 vs. 0.7, p = 0.004) and a significant decrease in HF% (48.3 vs. 58.5, p = 0.004) when compared with patients who experienced good outcomes. Other variables measured at 10–14 days and all variables measured within 7 days were similar for patients with good and poor outcomes. Additionally, no statistical difference was found in all HRV variables measured between within 7 days and 10–14 days in patients with either good outcome or poor outcomes.
Further, LF%, HF%, and LF/HF were included in three separate multivariate analyses. In the multivariate logistic regression analysis, LF% and HF% at 10–14 days post ICH were independently associated with 3-month poor outcomes, and this association remained stable in the sensitivity analysis (Table 5).
Discussion
In the current study, we investigated the characteristics of HRV values in patients with ICH and its association with clinical outcomes. Our findings indicated that HRV values were impaired significantly within 14 days after ICH. Furthermore, HRV indices (LF% and HF%) measured 10–14 days after ICH were independently associated with 3-month outcomes.
HRV is regarded as a non-invasive and easily applicable method for the assessment of cardiac autonomic nervous system activity and has been widely used in different physiological conditions and clinical studies [4]. Autonomic control of the heart is a dynamic process that plays an essential role in maintaining physiological homeostasis. Several types of brain injury can impair the cerebral control of cardiac autonomic regulation [23]. The current data clearly demonstrate that patients with ICH experience significant autonomic dysfunction based on decreases in HRV parameters, consistent with previous results [11, 12, 24]. However, previous studies have focused only on autonomic activation within 24 h after ICH, and its evolution over longer periods remains unknown. In our study, autonomic disturbances in the ICH group were sustained for at least 10–14 days after ictus, and no tendency for recovery was observed. Conversely, although the change was not significant, autonomic function seemed to further deteriorate within 10–14 days.
Results regarding the characteristics of autonomic dysfunction and changes in sympathetic and parasympathetic/vagal activity after ICH remain controversial. Feibel et al. reported markedly elevated catecholamine excretion in two patients with ICH [24]. Animal experiments by Reis et al. further verified that activation of sympathetic neurons and release of adrenomedullary catecholamines are the principal early reflex responses to ICH [25]. Conversely, recent studies in both humans and animals have demonstrated increases in parasympathetic/vagal nervous activity and decreases in sympathetic nervous activity after onset [11, 26, 27]. As shown in Table 1, different HRV indices could be used to reflect the absolute and relative activation of the sympathetic and vagal systems [22]. Therefore, we increased the sample size to explore the post-ICH characteristics of autonomic dysfunction according to the results of HRV measurements. In our study, absolute frequency domain values of HRV (TP, VLF, LF, and HF) were significantly decreased. As shown in Table 1, TP reflected the sum of sympathetic and vagal activity, LF reflected both sympathetic and vagal activity, and HF reflected vagal activity. The higher values indicated that the activity of autonomic function was more active. Thus, the decreased TP, LF, and HF indicated significant decreases in both sympathetic and vagal activity within 14 days after ICH. For relative frequency domain values, LF% was calculated as LF in proportion to the sum of LH and HF (TP minus the VLF component), HF% was calculated as HF in proportion to the sum of LH and HF, and LF/HF was calculated as the ratio of LF and HF. Physiologically, LF% and HF% correlated with relative sympathetic and vagal activity in the balanced behavior of autonomic nervous system, respectively. LF/HF reflected the balance between sympathetic and vagal activity. In patients with ICH, LF% and LF/HF were significantly higher, whereas HF% was significantly lower, than in the control group, indicating disturbances in the balance of the sympathetic and vagal systems and excessive modulation of the sympathetic nervous system in comparison with the vagal nervous system. Moreover, these changes were prolonged and even tended to progress, lasting for at least 10–14 days after ICH.
The mechanism underlying the tendency of decreased HRV is unclear. We considered it may be because of the natural progression of ICH, which can be divided into primary and secondary injury phases. The initial damage that occurs during the hyperacute stage of ICH involves mechanical damage of surrounding tissues (hematoma). The secondary injury is complex and occurs over days to weeks [28, 29]. Studies have found over the 7–14 days after ICH, perihematomal edema continues to expand in the setting of several classical secondary injury pathways, including release of thrombin, inflammation, and iron-induced injury [29]. We speculated that the secondary injury may contribute to the decreased tendency of HRV at 10–14 days after ICH.
In patients with stroke, especially ischemic stroke, the close association between abnormal HRV/autonomic dysfunction and outcome has been widely investigated [30,31,32]. However, to the best of our knowledge, few studies have explored the predictive function of autonomic disturbance assessed using HRV in patients with ICH. Two studies found that HRV, when assessed based on frequency and nonlinear parameters, was related to functional outcomes after ICH [11, 12]; however, the association was not confirmed by Swor et al. [33]. Swor et al. [33] calculated HRV in the time domain, which was independently associated with the development of fever and the number of febrile days but not with outcomes of ICH. This may suggest that HRV in the time domain predicts post-stroke complications rather than functional outcomes. In the present study, we found that HRV assessed by frequency domain parameters (LF% and HF%) measured 10–14 days after ICH was independently associated with 3-month outcomes in patients with ICH. Because the two values reflect the relative activity of the sympathetic and vagal systems, the results also indicated that higher relative sympathetic activation and lower relative vagal activation predicted poor functional outcomes. Therefore, autonomic dysfunction assessed by abnormal HRV may be regarded as an indicator of prognosis in patients with ICH and may serve as a treatment target to improve the long-term prognosis of these patients.
The present study has several limitations. First, even though we had enlarged our sample size, this study still had a relatively small sample size and was conducted at a single stroke center, highlighting the need for further multi-center studies to verify our findings. Second, because the numbers of patients with lobar, brainstem, and cerebellum hematoma was limited, these cases were combined for analysis, meaning that we could not evaluate the impact of these conditions on HRV individually. Third, to ensure that the pathogenesis of our patients’ conditions was similar, we excluded patients whose ICH occurred secondary to trauma, hemorrhagic conversion of ischemic stroke, or structural lesions, as well as patients who underwent any surgical treatments. Therefore, the conclusion of our study does not apply to these types of patients. Further studies are needed to explore HRV characteristics in patients with different types of ICH. Fourth, because this was an observational study, we were unable to establish a conclusive causal relationship.
Conclusions
To conclude, HRV values were impaired significantly within 14 days after ICH. Furthermore, HRV indices measured 10–14 days after ICH were independently associated with 3-month outcomes.
References
Al-Kawaz MN, Hanley DF, Ziai W. Advances in therapeutic approaches for spontaneous intracerebral hemorrhage. Neurotherapeutics. 2020;17:1757–67.
Veltkamp R, Purrucker J. Management of spontaneous intracerebral hemorrhage. Curr Neurol Neurosci Rep. 2017;17:80.
Gidday J. Cerebrovascular ischemic protection by pre- and post-conditioning. Brain Circ. 2015;1:97.
Catai AM, Pastre CM, Godoy MF, Silva ED, Takahashi ACM, Vanderlei LCM. Heart rate variability: Are you using it properly? Standardisation checklist of procedures. Braz J Phys Ther. 2020;24:91–102.
Wolf MM, Varigos GA, Hunt D, Sloman JG. Sinus arrhythmia in acute myocardial infarction. Med J Aust. 1978;2:52–3.
Kleiger RE, Miller JP, Bigger JT Jr, Moss AJ. Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am J Cardiol. 1987;59:256–62.
Malik M, Farrell T, Cripps T, Camm AJ. Heart rate variability in relation to prognosis after myocardial infarction: selection of optimal processing techniques. Eur Heart J. 1989;10:1060–74.
Bigger JT Jr, Fleiss JL, Steinman RC, Rolnitzky LM, Kleiger RE, Rottman JN. Frequency domain measures of heart period variability and mortality after myocardial infarction. Circulation. 1992;85:164–71.
Xhyheri B, Manfrini O, Mazzolini M, Pizzi C, Bugiardini R. Heart rate variability today. Prog Cardiovasc Dis. 2012;55:321–31.
Cygankiewicz I, Zareba W. Heart rate variability. Handb Clin Neurol. 2013;117:379–93.
Szabo J, Smielewski P, Czosnyka M, et al. Heart rate variability is associated with outcome in spontaneous intracerebral hemorrhage. J Crit Care. 2018;48:85–9.
Chen CH, Tang SC, Lee DY, et al. Impact of supratentorial cerebral hemorrhage on the complexity of heart rate variability in acute stroke. Sci Rep. 2018;8:11473.
Wang Y, Cui L, Ji X, et al. The China National Stroke Registry for patients with acute cerebrovascular events: design, rationale, and baseline patient characteristics. Int J Stroke. 2011;6:355–61.
Kothari RU, Brott T, Broderick JP, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996;27:1304–5.
Lietke S, Zausinger S, Patzig M, Holtmanspotter M, Kunz M. CT-based classification of acute cerebral edema: association with intracranial pressure and outcome. J Neuroimaging. 2020;30:640–7.
McKeown ME, Prasad A, Kobsa J, et al. Midline shift greater than 3 mm independently predicts outcome after ischemic stroke. Neurocrit Care. 2022;36:46–51.
Dowlatshahi D, Demchuk AM, Flaherty ML, et al. Defining hematoma expansion in intracerebral hemorrhage: relationship with patient outcomes. Neurology. 2011;76:1238–44.
Qu Y, Liu J, Guo ZN, et al. The impact of remote ischaemic conditioning on beat-to-beat heart rate variability circadian rhythm in healthy adults. Heart Lung Circ. 2021;30:531–9.
Jeyhani V, Mahdiani S, Peltokangas M, Vehkaoja A. Comparison of HRV parameters derived from photoplethysmography and electrocardiography signals. Conf Proc IEEE Eng Med Biol Soc. 2015;2015:5952–5.
Webb AJS, Mazzucco S, Li L, Rothwell PM. Prognostic significance of blood pressure variability on beat-to-beat monitoring after transient ischemic attack and stroke. Stroke. 2018;49:62–7.
Bodapati RK, Kizer JR, Kop WJ, Kamel H, Stein PK. Addition of 24-Hour Heart Rate Variability Parameters to the Cardiovascular Health Study Stroke Risk Score and Prediction of Incident Stroke: The Cardiovascular Health Study. J Am Heart Assoc. 2017;6:e004305.
Camm AJ, et al. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996;93:1043–65.
Jimenez-Ruiz A, Racosta JM, Kimpinski K, Hilz MJ, Sposato LA. Cardiovascular autonomic dysfunction after stroke. Neurol Sci. 2021;42:1751–8.
Feibel JH, Baldwin CA, Joynt RJ. Catecholamine-associated refractory hypertension following acute intracranial hemorrhage: control with propranolol. Ann Neurol. 1981;9:340–3.
Reis DJ, Ruggiero DA, Morrison SF. The C1 area of rostral ventrolateral medulla: a central site integrating autonomic responses to hemorrhage. Resuscitation. 1989;18:269–88.
Kox M, Vrouwenvelder MQ, Pompe JC, van der Hoeven JG, Pickkers P, Hoedemaekers CW. The effects of brain injury on heart rate variability and the innate immune response in critically ill patients. J Neurotrauma. 2012;29:747–55.
Marins FR, Limborco-Filho M, D’Abreu BF, et al. Autonomic and cardiovascular consequences resulting from experimental hemorrhagic stroke in the left or right intermediate insular cortex in rats. Auton Neurosci. 2020;227:102695.
Zhu H, Wang Z, Yu J, et al. Role and mechanisms of cytokines in the secondary brain injury after intracerebral hemorrhage. Prog Neurobiol. 2019;178:101610.
Magid-Bernstein J, Girard R, Polster S, et al. Cerebral hemorrhage: pathophysiology, treatment, and future directions. Circ Res. 2022;130:1204–29.
Lee KJ, Kim BJ, Han MK, et al. Effect of heart rate on stroke recurrence and mortality in acute ischemic stroke with atrial fibrillation. Stroke. 2020;51:162–9.
Li C, Meng X, Pan Y, Li Z, Wang M, Wang Y. The association between heart rate variability and 90-day prognosis in patients with transient ischemic attack and minor stroke. Front Neurol. 2021;12:636474.
Carandina A, Lazzeri G, Villa D, et al. Targeting the autonomic nervous system for risk stratification, outcome prediction and neuromodulation in ischemic stroke. Int J Mol Sci. 2021;22:2357.
Swor DE, Thomas LF, Maas MB, et al. Admission heart rate variability is associated with fever development in patients with intracerebral hemorrhage. Neurocrit Care. 2019;30:244–50.
Funding
This article was supported by the Natural Science Foundation of China (81901192) to Xin Sun, by the Science and Technology Department of Jilin Province (YDZJ202302CXJD061) and the Jilin Provincial Key Laboratory (YDZJ202302CXJD017) to Yi Yang, and by Norman Bethune Program of Jilin University (2022B02) to Zhen-Ni Guo.
Author information
Authors and Affiliations
Contributions
All authors fulfill the criteria for authorship set by the International Committee of Medical Journal Editors. Individual authors put special emphasis on conception and design (YY, ZNG), acquisition of data (YQ, HYM, XS, RA, HJZ,), analysis and interpretation of data (YQ, PZ, JL, PDZ), and drafting and revising (ZNG, YQ).
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval/informed consent
All participants or their direct relatives provided written informed consent for this study, which was approved by the Ethics Review Committee of the First Hospital of Jilin University (2017-042).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qu, Y., Yang, Y., Sun, X. et al. Heart Rate Variability in Patients with Spontaneous Intracerebral Hemorrhage and its Relationship with Clinical Outcomes. Neurocrit Care 40, 282–291 (2024). https://doi.org/10.1007/s12028-023-01704-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-023-01704-6