Abstract
Purpose
To examine changes in retinal ganglion cell complex (GCC) and peripapillary retinal nerve fiber layer (RNFL) thicknesses by optical coherence tomography (OCT) in contralateral and ipsilatateral eyes of carotid artery stenosis (CAS) patients before and after carotid endarterectomy (CEA).
Methods
Forty-two consecutive patients diagnosed with CAS (70–99% stenosis rate) who underwent CEA were included in this prospective cross-sectional study. The indication for CEA was based on the Asymptomatic Carotid Atherosclerosis Study. Doppler ultrasonography and computed tomography angiography were performed to calculate CAS. All the subjects underwent an ophthalmological examination, including best corrected visual acuity (BCVA), intraocular pressure (IOP) measurements, biomicroscopy, fundoscopy, and OCT before and after the surgery.
Results
The mean preoperative intraocular pressure was 15.2 ± 2.1 mmHg in the ipsilateral eye and 15.8 ± 2.7 in the contralateral eye. The mean postoperative intraocular pressure in the ipsilateral and contralateral eye was 18.6 ± 3.0 and 19.3 ± 3.8, respectively. The intraocular pressure was significantly higher in postoperative eyes (p = 0.0001). There was a statistically significant decrease in peripapillary RNFL thickness in superior quadrants postoperatively in ipsilateral eyes. The retinal GCC layer thickness was not significantly different before and after CEA in ipsilateral and contralateral eyes.
Conclusions
Carotid endarterectomy results in thinning of the superior peripapillary RNFL thickness. To the best of our knowledge, this is the first study to examine peripapillary RNFL and GCC thicknesses before and after CEA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The ophthalmic artery is the first intradural branch of the carotid artery. Thus, carotid artery blood flow plays an important role in ocular microcirculation [1]. Internal carotid artery (ICA) stenosis leads to chronic progressive hypoperfusion of the eye [2]. Previous studies reported that various ophthalmic manifestations, including decreased visual function, amaurosis fugax, rubeosis iridis, neovascular glaucoma, ischemic ocular pain, and optic disk edema or atrophy, were associated with reduced blood flow in the ophthalmic artery in carotid artery stenosis (CAS) patients [3, 4]. Ocular ischemia in CAS patients is thought to be due to direction of reverse blood flow from the ophthalmic artery to ipsilateral brain, known as the steal phenomenon [3]. However, in some patients with ICA disease, the eyes show no clinical symptoms of ocular ischemia [3]. The underlying reason for the lack of symptoms is unknown. Carotid endarterectomy (CEA) is a widely accepted, effective surgical treatment option for symptomatic and asymptomatic patients with high-grade CAS [2, 5, 6]. Numerous studies demonstrated improved retinal blood flow after CEA [7, 8]. However, information is lacking on changes in peripapillary retinal nerve fiber layer (RNFL) and ganglion cell complex (GCC) thicknesses after CEA.
Spectral domain optical coherence tomography (SD-OCT) is a noninvasive, reproducible imaging method, which allows demonstration of macular and peripapillary regions in a short time, with high axial resolution [9, 10]. Thinning of peripapillary retinal nerve fiber and ganglion cell thicknesses, resulting in progressive injury of the optic nerve, is a well-known phenomenon in various diseases, such as glaucoma, optic neuritis, and non-arteritic ischemic optic neuropathy (NAION) [11,12,13,14,15].
There is a major risk of cerebral and ocular ischemic attacks in CAS patients, and CEA plays a vital role in preventing further cerebral and ocular ischemic events [5, 16]. Changes in RNFL and GCC layer thicknesses before and after CAS could provide valuable information to aid the management of CAS, determine the requirement for CEA, and assess the effect of CEA surgery. This study aimed to examine changes in retinal GCC layer and peripapillary RNFL thicknesses by OCT in contralateral and ipsilateral eyes of CAS patients before and after CEA.
Methods
The present study was approved by the local ethics committee and followed the tenets of the Declaration of Helsinki. Written informed consent was obtained from all subjects.
Forty-two patients who were diagnosed with CAS (70–99% stenosis rate) and underwent CEA surgery were included in this prospective cross-sectional study. The exclusion criteria were as follows: a history of any symptoms or signs of an ocular ischemic attack; a history of any ocular disease (glaucoma, diabetic retinopathy, maculopathy, age-related macular degeneration, ocular ischemic syndrome, epiretinal membranes, NAION or arteritic ischemic optic neuropathy, and optic neuritis) and any ocular surgery; a high refractive error (≥ ± 6D spherical ≥ ± 3D cylindrical); disk abnormalities; a history of previous CEA or carotid artery stenting; total CAS; and bilateral CAS > 50%.
All the subjects underwent an ophthalmological examination, including best corrected visual acuity (BCVA), intraocular pressure (IOP) measurements, biomicroscopy, fundoscopy, and OCT. Only patients with BCVA of 20/20 were included. Preoperative and postoperative single measurement of IOP was performed to the all patients in the daytime (at 14.00 pm) in upright posture with Goldmann applanation tonometry. In the study group, 21 patients had systemic hypertension and atherosclerosis, 11 had diabetes mellitus (without diabetic retinopathy), and 3 were current smokers or ex-smokers. The indication for CEA was based on the Asymptomatic Carotid Atherosclerosis Study [17]. Doppler ultrasonography and computed tomography angiography were performed to calculate CAS. All the patients underwent CEA under general anesthesia. The carotid artery was exposed by making a longitudinal incision along the anterior border of the sternocleidomastoid muscle. The common carotid artery, ICA, and external carotid artery were occluded with vascular clamps. The common carotid artery and ICA were longitudinally opened along the anterior vessel walls, and atheromatous plaques and nearby intima were carefully removed from the carotid bifurcation. The longitudinal incision was closed using a polytetrafluoroethylene patch. The vascular clamps were then removed, and the skin incision was closed.
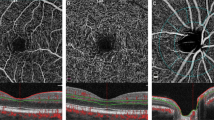
An experienced investigator who was blinded to the study monitored the patients using SD-OCT (RS-3000 Lite, Nidek, Japan), according to macula map and disk map protocols. Macular thickness was examined in the following areas: the central 1 mm of the macula (fovea), 1–3 mm of the parafoveal macular area, and 3–6 mm of the perifoveal macular area. The GCC thickness [consisting of the RNFL, GCL, and inner plexiform layer (IPL)] was examined in the following areas: 1–3 mm of the parafoveal macular area and 3–6 mm of the perifoveal macular area. The RNFL thickness was examined in the following areas: superior, inferior, nasal, and temporal quadrants.
Statistical analysis
The Shapiro–Wilk test was conducted to assess the distribution of normality for continuous variables prior to the data analysis. For independent groups, the Student’s t test was used for continuous variables with a normal distribution, whereas the Mann–Whitney U test was performed for continuous variables with a non-normal distribution. For dependent groups, a paired samples t test was used for continuous variables with a normal distribution, whereas Wilcoxon’s signed-rank test was performed for continuous variables with a non-normal distribution. Descriptive statistics were expressed as mean and standard deviation for normally distributed variables and as median and first-quartile and third-quartile values for non-normally distributed variables. The significance level was determined as 0.05 in all statistical analyses. All statistical analyses were performed using IBM SPSS 20 (IBM Corp., Armonk, NY, USA).
Results
The study included 42 ipsilateral and 42 contralateral eyes of 42 patients (30 males and 12 females), with a mean age of 63.7 ± 5.58 years. The mean preoperative IOP was 15.2 ± 2.1 mmHg in the ipsilateral eye and 15.8 ± 2.7 in the contralateral eye. The mean postoperative IOP in the ipsilateral and contralateral eye was 18.6 ± 3.0 and 19.3 ± 3.8, respectively. The IOP was significantly higher in postoperative eyes (p = 0.0001) (Fig. 1). There was a statistically significant decrease in peripapillary RNFL thickness in superior quadrants postoperatively in ipsilateral eyes (Tables 1, 2, Fig. 2). There was no statistically significant difference between preoperative and postoperative eyes in terms of foveal thickness (all p values > 0.05, Tables 3, 4). Parafoveal and perifoveal thicknesses were not significantly different before and after carotid surgery (all p values > 0.05, Tables 3, 4). The GCC thickness was not significantly different before and after CEA in ipsilateral and contralateral eyes (all p values > 0.05, Tables 5, 6).
Discussion
In this study, there was a statistically significant increase in IOP in both eyes 1 month after CAE. Peripapillary RNFL thickness in the superior quadrant was decreased in ipsilateral eyes postoperatively.
An autoregulation mechanism provides stable ocular blood flow to the retina, choroid, and optic disk [18]. However, in patients with CAS, dysfunction of this autoregulation mechanism leads to reduced blood flow, resulting in ischemia and hypoxia of astrocytes in the disk and mitochondria in retinal ganglion cell axons [18, 19]. This leads to apoptosis and autophagia of retinal ganglion cells [20]. Autoregulation of ocular blood flow is determined by ocular perfusion pressure. When the ocular perfusion pressure decreases below a threshold value, symptoms of ocular ischemic syndrome begin to appear [18]. Arterial hypertension reduces the ability of the eye to autoregulate blood flow when ocular perfusion pressure changes and exacerbates the ocular ischemic symptoms [21] Fluctuations in ocular perfusion pressure associated with atherosclerosis can have adverse effects on vessel diameters, thereby increasing the risk of ischemic injury [22]. Chronic hypertension adjusts the autoregulation mechanism to high levels and adapts the mechanism to higher blood pressures. This mechanism ensures that the patient is resistant to high but not low blood pressure [20]. In this study, most of the patients were hypertensive and accustomed to high blood pressure. The sudden decrease in ocular blood flow during surgery could contribute to ganglion cell death.
CEA is a well-known procedure to decrease the risk of strokes in CAS patients. However, the procedure is associated with a connatural risk of perioperative complications [23, 24]. For example, previous studies demonstrated that CEA increased cerebral and ocular blood flow [2, 25,26,27,28]. Research also reported that ciliary body ischemia caused normal or low IOP in CAS patients and that the blood supply of the ciliary body increased after CEA, leading to an increase in aqueous humor production and a subsequent rise in IOP [27, 29,30,31]. Kozobolis et al. [18] found no difference in IOP between eyes operated on and fellow eyes before surgery and IOP in postoperative month 6. In contrast, we found increased IOPs after CEA. However, the increase was slight (i.e., no greater than 3–4 mmHg). Thus, none of the patients required antiglaucomatous therapy and surgery. As the patients in the present study were assessed just 1 month after CEA, the increase in IOP could be attributed to the carotid surgery.
Numerous previous studies demonstrated thinning of the inner retina in chronic NAION patients [32,33,34,35,36]. Tesser et al. [37] reported the presence of infarcts in the superior quadrant in NAION patients. The loss of ganglion cells in NAION results in a reduction in macular and central retinal thicknesses. Other researchers showed that macular thinning in cases of chronic NAION was a good clinical determinant of visual dysfunction [33]. Kupersmith et al. [34] demonstrated decreased GCL and IPL thickness at month 1 in NAION patients but not RNFL thinning 1 month after NAION. In the present study, none of the patients had NAION or decreased visual acuity. Reperfusion was present in our patients.
During carotid surgery, hypoperfusion syndrome can occur because of clamping of the ICA [38]. Regional cerebral ischemia may also develop, depending on the capacity of compensatory mechanisms, such as collateral blood flow, oxygenation, and blood pressure [31, 38]. After removal of the carotid clamp and elimination of atherosclerotic plaques, ICA blood flow returns, with variable degrees of reperfusion. In cases of relative ischemia reperfusion, subclinical injury (reversible or irreversible) may occur [39,40,41,42].
Many previous studies reported that increased activation of the N-methyl-d-aspartate (NMDA) receptor was responsible for neuronal degeneration induced by ischemia reperfusion [43,44,45]. Retinal neurodegeneration (i.e., retinal ganglion cell apoptosis and thinning of the inner retina) occurred following intravitreal injections of high doses of NMDA [46, 47]. In experimental models of retinal neurodegeneration, decreased retinal blood flow exacerbated ischemic retinal injury [48, 49]. In addition, recent studies revealed that vascular endothelial growth factors (VEGFs) played an important role in retinal neuroprotection [50, 51]. Nishijima et al. reported that VEGF-A had neuroprotective effects in ischemia and that VEGF inhibition appeared to aggravate ischemia-induced neural damage [51, 52]. Research also demonstrated that VEGF and VEGFR-2 were upregulated in carotid stenosis and that circulating levels of VEGF and VEGFR-2 decreased after CEA [53]. Shvartsman et al. [54] reported that VEGF reduced axonal disruption and promoted axonal regeneration after acute ischemic injury.
Our findings pointed to reduced superior peripapillary RNFL thickness but relatively little loss in GCC thickness (macular RNFL, GCL, and IPL) after CEA. The observed pattern of injury may be explained by the protective effect of VEGF on axons relative to that of the ganglion cell body. As noted above, VEGF plays a role in axonal protection. In the present study, ischemia reperfusion injury due to CEA may have reduced VEGF levels. The limited and relatively short period of ischemia may have caused localized superior peripapillary RNFL quadrant defects in ipsilateral eyes. We did not detect a significant difference between preoperative and postoperative RNFL thicknesses in contralateral eyes. The aforementioned may be explained by the regular blood flow of the contralateral carotid artery and absence of ischemia.
Zhang et al. [55] demonstrated that anti-VEGF treatment improved neurological function in patients with malignant tumors of the nervous system. Novitzky et al. [56] showed neuroprotective effect of bevacizumab after middle cerebral artery occlusion. These studies researched the situations where the VEGF levels are abnormally high. Anti-VEGF agents might have a neuroprotective effect in cases that the level of VEGF is high. We believe that the anti-VEGFs may have a negative effect on neuroprotection by reducing the levels of VEGF, which is already shown to decrease after CEA.
The outer retina is more resistant to ischemia than the inner retina [57]. This could be the reason that the disk was affected without any change in retina in our study. Previous histopathological studies have demonstrated that the peripheral superior sector of the optic nerve head demonstrates the greatest mean retinal ganglion cell axonal diameter. It was shown that axons of larger retinal ganglion cells might be more vulnerable to ischemic axonal injury. Because neurofilament phosphorylation requirement is greatest in this site of the optic nerve [58].
The limitations of our study are the relatively small number of patients and absence of long-term postoperative outcomes of the patients. In addition, we did not use laser speckle flowgraphy to measure ocular blood flow.
In summary, ischemia and reperfusion injury due to CEA results in thinning of the superior peripapillary RNFL. Patients may be prescribed anti-VEGF agents for various reasons. For axonal protection, patients should cease the use of such agents if possible in the early preoperative and postoperative periods of CEA. To the best of our knowledge, this is the first study to examine peripapillary RNFL and GCC thicknesses before and after CEA. Further long-term studies with large samples are needed to investigate whether these alterations are progressive and accompanied by GCC thinning in the following period.
References
Shii M, Hayashi M, Yagi F, Sato K, Tomita G, Iwabuchi S (2016) Relationship between the direction of ophthalmic artery blood flow and ocular microcirculation before and after carotid artery stenting. J Ophthalmol 2016:2530914. https://doi.org/10.1155/2016/2530914 (Epub 2016 Dec 14)
Enaida H, Nagata S, Takeda A, Nakao S, Ikeda Y, Ishibash T (2016) Changes in chorioretinal blood flow velocity and cerebral blood flow after carotid endarterectomy. Jpn J Ophthalmol 60:459–465
Yamamato T, Mori K, Yasuhara T et al (2004) Ophthalmic artery blood flow in patients with internal carotid artery occlusion. Br J Ophthalmol 88:505–508
Kozobolis VP, Detorakis ET, Georgiadis GS, Achtaropoulos AA, Papas TT, Lazarides MK (2007) Perimetric and retrobulbar blood flow changes following carotid endarterectomy. Graefes Arch Clin Exp Ophthalmol 245(11):1639–1645
Barnett HJ, Taylor DW, Eliasziw M et al (1998) Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med 339:1415–1425
Naylor AR, Rothwell PM, Bell PR (2003) Overview of the principal results and secondary analyses from the European and North American randomised trials of endarterectomy for symptomatic carotid stenosis. Eur J Vasc Endovasc Surg 26:115–129
Ishikawa K, Kimura I, Shinoda K et al (2002) In situ confirmation of retinal blood flow improvement after carotid endarterectomy in a patient with ocular ischaemic syndrome. Am J Ophthalmol 134:295–297
Evlice M, Akcakoyun M, Velioglu M et al (2016) Effects of obstructive carotid artery disease on ocular circulation and the safety of carotid artery stenting. Heart Lung Circ. https://doi.org/10.1016/j.Hlc.2016.11.020 (Epub ahead of print)
Huang D, Swanson EA, Lin CP et al (1991) Optical coherence tomography. Science 254:1178–1181
Arthur SN, Smith SD, Wright MM et al (2011) Reproducibility and agreement in evaluating retinal nerve fibre layer thickness between Stratus and Spectralis OCT. Eye 25:192–200
Raza A, Jungsuk C, de Moraes CG et al (2011) Retinal ganglion cell layer thickness and local visual field sensitivity in glaucoma. Arch Ophthalmol 129:1529–1536
Takagi S, Kita Y, Fumihiko Y, Tomita G (2012) Macular retinal ganglion cell complex damage in the apparently normal visual field glaucomatous eyes with hemifield defects. J Glaucoma 21:318–325
Hood DC, Anderson S, Rouleau J et al (2008) Retinal nerve fiber structure versus visual field function in patients with ischemic optic neuropathy. Ophthalmology 115:904–910
Mwanza JC, Durbin MK, Budenz DL et al (2012) Glaucoma diagnostic accuracy of ganglion cell-inner plexiform layer thickness: comparison with nerve fiber layer and optic nerve head. Ophthalmology 119:1151–1158
Koh V, Tham YC, Cheung CY et al (2012) Determinants of ganglion cell-inner plexiform layer thickness measured by high definition optical coherence tomography. Investig Ophthalmol Vis Sci 53:5853–5859
Rothwell PM, Eliasziw M, Gutnikov SA et al (2003) Carotid endarterectomy trialists’ collaboration. Analysis of pooled data from the randomised controlled trials of endarterectomy for symptomatic carotid stenosis. Lancet 11:107–116
Rothwell PM (2006) Symptomatic and asymptomatic carotid stenosis: How, when, and who to treat? Curr Atheroscler Rep 8:290–297
Kozobolis VP, Detorakis ET, Georgiadis GS, Achtaropoulos AA, Papas TT, Lazarides MK (2007) Perimetric and retrobulbar blood flow changes following carotid endarterectomy. Graefes Arch Clin Exp Ophthalmol 245(11):1639–1645
Keunen RW, Eikelboom BC, Stegeman DF, Ackerstaff RG (1994) Chronic cerebral hypotension induces a downward shift of the cerebral autoregulation: a hypothesis based on TCD and OPG-GEE studies in ambulatory patients with occlusive cerebrovascular disease. Neurol Res 16(6):413–416
Prada D, Harris A, Guidoboni G, Siesky B, Huang AM, Arciero J (2016) Autoregulation and neurovascular coupling in the optic nerve head. Surv Ophthalmol 61(2):164–186
Hayreh SS (1995) The optic nerve head circulation in health and disease. Exp Eye Res 61(3):259–272 (The 1994 Von Sallman lecture)
Harris A, Jonescu-Cuypers C, Martin B, Kagemann L, Zalish M, Garzozi HJ (2001) Simultaneous management of blood flow and IOP in glaucoma. Acta Ophthalmol Scand 79(4):336–341
Kragsterman B, Bergqvist D, Siegbahn A, Parsson H (2017) Carotid endarterectomy induces the release of inflammatory markers and the activation of coagulation as measured in the jugular bulb. J Stroke Cerebrovasc Dis. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.05.020 (Epub ahead of print)
Halliday A, Mansfield A, Marro J et al (2004) Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomised controlled trial. Lancet 363:1491–1502
Kawaguchi S, Iida J, Uchiyama Y (2012) Ocular circulation and chronic ocular ischemic syndrome before and after carotid artery revascularization surgery. J Ophthalmol 2012:350475. https://doi.org/10.1155/2012/350475
Wang J, Wang W, Jin B et al (2016) Improvement in cerebral and ocular hemodynamics early after carotid endarterectomy in patients of severe carotid artery stenosis with or without contralateral carotid occlusion. Biomed Res Int 2016:2901028. https://doi.org/10.1155/2016/2901028
Geroulakos G, Botchway LT, Pai V, Wilkinson AR, Galloway JM (1996) Effect of carotid endarterectomy on the ocular circulation and on ocular symptoms unrelated to emboli. Eur J Vasc Endovasc Surg 11(3):359–363
Neroev VV, Kiseleva TN, Vlasov SK, Pak NV, Gavrilenko AV, Kuklin AV (2012) Visual outcomes after carotid reconstructive surgery for ocular ischemia. Eye (Lond) 26(10):1281–1287. https://doi.org/10.1038/eye.2012.118
Katsuta T, Fujimoto A, Oba K (2013) Deterioration of glaucoma after carotid endarterectomy. Neurol Med Chir (Tokyo) 53(6):418–421
Cuevas-Lestienne C, Chiquet C, Zech J, Burillon C, Trepsat C, Denis P (2000) Neovascular glaucoma diagnosed following carotid endarterectomy. J Fr Ophtalmol 23(6):599–602
Nguyen QH, Hamed LM, Sherwood MB, Roseman RL (1996) Neovascular glaucoma after carotid endarterectomy. Ophthalmic Surg Lasers 27(10):881–884
Bellusci C, Savini G, Carbonelli M, Carelli V, Sadun AA, Barboni PB (2008) Retinal nerve fiber layer thickness in nonarteritic anterior ischemic optic neuropathy: OCT characterization of the acute and resolving phases. Graefes Arch Clin Exp Ophthalmol 246(5):641–647
Akbari M, Abdi P, Fard MA et al (2016) Retinal ganglion cell loss precedes retinal nerve fiber thinning in nonarteritic anterior ischemic optic neuropathy. J Neuroophthalmol 36(2):141–146
Kupersmith MJ, Garvin MK, Wang JK, Durbin M, Kardon R (2016) Retinal ganglion cell layer thinning within one month of presentation for non-arteritic anterior ischemic optic neuropathy. Investig Ophthalmol Vis Sci 57(8):3588–3593
Gonul S, Koktekir BE, Bakbak B, Gedik S (2013) Comparison of the ganglion cell complex and retinal nerve fibre layer measurements using Fourier domain optical coherence tomography to detect ganglion cell loss in non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol 97(8):1045–1050
Aggarwal D, Tan O, Huang D, Sadun AA (2012) Patterns of ganglion cell complex and nerve fiber layer loss in nonarteritic ischemic optic neuropathy by Fourier-domain optical coherence tomography. Investig Ophthalmol Vis Sci 53(8):4539–4545
Tesser RA, Niendorf ER, Levin LA (2003) The morphology of an infarct in nonarteritic anterior ischemic optic neuropathy. Ophthalmology 110:2031–2035
Lee JH, Choi CG, Kim DK, Kim GE, Lee HK, Suh DC (2004) Relationship between circle of Willis morphology on 3D time-of-flight MR angiograms and transient ischemia during vascular clamping of the internal carotid artery during carotid endarterectomy. AJNR Am J Neuroradiol 25:558–564
Jaranyi Z, Szekely M, Bobek I, Gálfy I, Gellér L, Selmeci L (2003) Impairment of blood-brain barrier integrity during carotid surgery as assessed by serum S-100B protein concentrations. Clin Chem Lab Med 41:1320–1322
Szabo P, Lantos J, Nagy L et al (2016) l-Arginine pathway metabolites predict need for intra-operative shunt during carotid endarterectomy. Eur J Vasc Endovasc Surg 52:721–728
Muller M, Reiche W, Langenscheidt P, Hassfeld J, Hagen T (2000) Ischemia after carotid endarterectomy: comparison between transcranial Doppler sonography and diffusion-weighted MR imaging. AJNR Am J Neuroradiol 21:47–54
Arfvidsson B, Nilsson TK, Norgren L (2015) S100B concentrations increase perioperatively in jugular vein blood despite limited metabolic and inflammatory response to clinically uneventful carotid endarterectomy. Clin Chem Lab Med 53:111–117
Nakahara T, Hoshino M, Hoshino S, Mori A, Sakamoto K, Ishii K (2015) Structural and functional changes in retinal vasculature induced by retinal ischemia-reperfusion in rats. Exp Eye Res 135:134–145
Lagrèze WA, Knörle R, Bach M, Feuerstein TJ (1998) Memantine is neuroprotective in a rat model of pressure-induced retinal ischemia. Investig Ophthalmol Vis Sci 39(6):1063–1066
Lam TT, Siew E, Chu R, Tso MO (1997) Ameliorative effect of MK-801 on retinal ischemia. J. Ocul. Pharmacol. Ther. 13:129–137
Manabe S, Lipton SA (2003) Divergent NMDA signals leading to proapoptotic and antiapoptotic pathways in the rat retina. Investig Ophthalmol Vis Sci 44(1):385–392
Lam TT, Abler AS, Kwong JM, Tso MO (1999) N-methyl-d-aspartate (NMDA)–induced apoptosis in rat retina. Investig Ophthalmol Vis Sci 40(10):2391–2397
Zheng L, Gong B, Hatala DA, Kern TS (2007) Retinal ischemia and reperfusion causes capillary degeneration: similarities to diabetes. Investig Ophthalmol Vis Sci 48:361–367
Chen B, Caballero S, Seo S, Grant MB, Lewin AS (2009) Delivery of antioxidant enzyme genes to protect against ischemia/reperfusion-induced injury to retinal microvasculature. Investig Ophthalmol Vis Sci 50:5587–5595
Foxton RH, Finkelstein A, Vijay S et al (2013) VEGF-A is necessary and sufficient for retinal neuroprotection in models of experimental glaucoma. Am J Pathol 182:1379–1390
Nishijima K, Ng YS, Zhong L et al (2007) Vascular endothelial growth factor-A is a survival factor for retinal neurons and a critical neuroprotectant during the adaptive response to ischemic injury. Am J Pathol 171:53–67
Ayar O, Alpay A, Koban Y et al (2017) the effect of dexamethasone intravitreal implant on retinal nerve fiber layer in patients diagnosed with branch retinal vein occlusion. Curr Eye Res 20:1–6. https://doi.org/10.1080/02713683.2017.1313430 (Epub ahead of print)
Papalambros E, Georgopoulos S, Sigala F et al (2004) Changes in circulating levels of vascular endothelial growth factor and vascular endothelial growth factor receptor-2 after carotid endarterectomy. Int J Mol Med 14(1):133–136
Shvartsman D, Storrie-White H, Lee K et al (2014) Sustained delivery of VEGF maintains innervation and promotes reperfusion in ischemic skeletal muscles via NGF/GDNF signaling. Mol Ther 22(7):1243–1253
Zhang N, Chen J, Ferraro GB, Wu L, Datta M, Jain RK, Plotkin SR, Stemmer-Rachamimov A, Xu L (2018) Anti-VEGF treatment improves neurological function in tumors of the nervous system. Exp Neurol 299:326–333. https://doi.org/10.1016/j.expneurol.2017.09.008
Novitzky I, Marianayagam NJ, Weiss S, Muhsinoglu O, Fridman M, Leibovitch TA, Goldenberg-Cohen N, Michowiz S (2016) Comparison of neuroprotective effect of bevacizumab and sildenafil following induction of stroke in a mouse model. Biomed Res Int 2016:3938523. https://doi.org/10.1155/2016/3938523 (Epub 2016 May 29)
Hughes WF (1991) Quantitation of ischemic damage in the rat retina. Exp Eye Res 53(5):573–582
Kang MH, Law-Davis S, Balaratnasingam C, Yu DY (2014) Sectoral variations in the distribution of axonal cytoskeleton proteins in the human optic nerve head. Exp Eye Res 128:141–150. https://doi.org/10.1016/j.exer.2014.10.006 (Epub 2014 Oct 7)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guclu, O., Guclu, H., Huseyin, S. et al. Retinal ganglion cell complex and peripapillary retinal nerve fiber layer thicknesses following carotid endarterectomy. Int Ophthalmol 39, 1523–1531 (2019). https://doi.org/10.1007/s10792-018-0973-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-018-0973-4