Abstract
Purpose
In order to analyze the data and retinal microvasculature for non-arteritic anterior ischemic optic neuropathy (NAION), patients were referred to have carotid Doppler ultrasound (CDU) from 2016 to 2020.
Methods
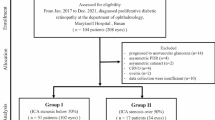
In this case–control observational study, 30 NAION patients were evaluated with CDU. Twenty-two NAION patients (at least 3 months after the onset of symptoms) and 9 normal subjects underwent a complete ophthalmic examination including optical coherence tomography (OCT) and optical coherence tomography angiography (OCT-A). NAION eyes and fellow eyes were further divided into two groups based on the presence of carotid stenosis (CS). NAION patients with CS were termed “CS-NAION”; and those without CS were termed “NCS-NAION.” Measurements of radial peripapillary capillary vessel density (RPC VD), ganglion cell complex (GCC), retinal nerve fiber layer (RNFL) thicknesses were compared among groups.
Results
Fourteen of 30 NAION patients referred to have carotid Doppler were positive for CS with each one of such referrals having less than 50% stenosis. RNLF, GCC and RPC VDs were reduced in NAION patients’ eyes, when compared to controls and the fellow eyes. RPC VD was significantly lower in the temporal-superior (P = 0.037) and the superior-temporal (P = 0.012) sectors of the NCS-NAION patients than in the CS-NAION patients. No significant differences were found between CS-fellow eyes and NCS-fellow eyes in terms of RPC VDs, RNLF or GCC.
Conclusion
Results of the study highlight the effect of the carotid artery stenosis on ocular perfusion pressure in the pathogenesis of NAION. More extensive studies are necessary.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute optic nerve injury due to non-arteritic anterior ischemic optic neuropathy (NAION) typically causes reduced visual acuity and significant retinal structural alterations, which is almost always permanent. In recent years, imaging method such as optical coherence tomography has been used extensively to document any swelling and injury at the various retinal layers [1,2,3]. Given the claimed ischemic pathophysiology, fluorescein angiography (FA) and optic coherence angiography (OCT-A) imaging techniques have explored the blood flow or the vasculature in the region of the optic nerve head (ONH), peripapillary retina and choroid. Fluorescein and indocyanine green angiographic studies of the optic disk in NAION showed complete or sectorial delay or absence of filling of the prelaminar optic disk without impairment of the choroidal circulation [4, 5]. However, FA is not sufficiently sensitive enough to measure the detailed changes of capillaries. OCT-A is a noninvasive technique that provides analysis of the microvasculature of the peripapillary region. Previous studies have reported that the swelling of the ONH in NAION causes significant changes in the peripapillary vasculature both at the acute and the atrophic stage [6,7,8,9,10]. As previously described, OCT-A findings show very good matching with retinal nerve fiber layer (RNFL) and visual field damages, confirmed by correlation analyses [8, 10].
The risk factors for the development of the NAION are hypertension, arteriosclerosis, diabetes, cardiovascular disease and internal carotid artery occlusion [11, 12]. Color-flow Doppler is a new development of duplex sonography of the peripheral vessels. In a retrospective study with duplex sonography, authors evaluated 191 ophthalmological patients with amaurosis fugax, occluded retinal veins and glaucoma, and found that ophthalmological patients suffered more often from carotid artery stenosis (CS) than asymptomatic people [13].
Given that the carotid artery disease can contribute to development of NAION either by embolism or by lowering the perfusion pressure [12], the aim of this study is to evaluate the effect of CS on the capillary density within the optic disk and within the peripapillary region in NAION eyes and the fellow eyes.
Methods
This observational cross-sectional study was conducted in Bakırköy Dr. Sadi Konuk Education and Research Hospital which is located in Istanbul, Turkey. Patients with NAION were recruited from the neuroophthalmology clinic. The research protocols were approved by the institutional review board, and it adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all volunteers prior to their participation in this study.
Diagnostic criteria for NAION were: a sudden onset of painless vision loss, sectorial or generalized optic disk edema, peripapillary hemorrhage and normal erythrocyte sedimentation rate or C-reactive protein. All of the patients underwent ophthalmic evaluation, including best-corrected visual acuity (BCVA) and refraction assessments, slit-lamp bio-microscopy, intraocular pressure measurement, ONH evaluation, fundus examination and digital color fundus photography (digital non-mydriatic retinal camera; Topcon), carotid color Doppler sonography (CDU). Representative cases of NAION are shown in Fig. 1. Twenty-two NAION patients in the atrophic phase were retrospectively identified from an internally maintained OCT-A imaging database (at least 3 months of the initial evaluation). OCT-A images of fellow, unaffected eyes were also evaluated in the study. NAION patients were categorized as either NAION with CS “CS-NAION” or NAION without CS “NCS-NAION” based on the presence or absence of CS, at the CDU.
The control group comprised age-matched subjects with a BCVA ≥ 0,8, IOP ≤ 21 mm Hg, an open angle, normal optic disk appearance on fundus examination and no RNFL defects.
The exclusion criteria were as follows: (1) refractive error greater than + 3.0 diopters (D) or less than − 4.0 D; (2) previous intraocular surgery other than cataract; (3) any other ophthalmic disorder, including corneal opacity, vitreous opacity, diabetic retinopathy and diseases affecting the optic disk such as glaucoma, optic neuritis, uveitis, retinal or choroidal diseases, and trauma; and (4) neurologic diseases that may affect the optic nerve such as multiple sclerosis, Alzheimer disease and Parkinson disease (5) poor cooperation in OCT imaging studies.
OCT-A was performed with the spectral domain system RTVue-XR Avanti (Optovue Inc. Fremont, California, USA). The peripapillary RNFL was determined using the ONH protocol. A standard 360°, 3.4-mm-diameter circular scan was utilized to measure the RNFL thickness, and the superior, nasal, temporal and inferior RNFL values were recorded. The macula cube scanning protocol measured the ganglion cell complex (GCC) thickness over a 7 mm diameter centered on the fovea, inferior, superior and the total GCC values were recorded.
The flow density map software AngioAnalytics (RTVue-XR version 2018.0.0.18) was employed to quantify the vessel density in this study. The OCT-A images were acquired within the peripapillary area (Fig. 2). The retinal peripapillary capillaries (RPC) mode, which included the signals from the internal limiting membrane to the nerve fiber layer, was utilized in this study. In the optic disk scan, the software automatically fits an ellipse to the optic disk margin and calculates the average vessel density within the ONH and peripapillary area. The peripapillary area is defined as a 0.75-mm-wide elliptical annulus that extends from the optic disk boundary. The peripapillary region is divided into sectors, and the vessel densities in each sector are calculated. The sectors are: nasal-inferior, nasal-superior, inferonasal, inferotemporal, superotemporal, superonasal, temporal-inferior and temporal-superior sectors. The vessel density (VD) was defined as the percentage of the area that is occupied by vessels within the segmented area. The signal strength index was employed to control the image quality. Images with a signal strength index less than 7 were excluded.
OCT-A images of the subjects; first row: NAION patient without carotid stenosis, second row: NAION patient with carotid stenosis, third row: fellow eye of NAION patient with carotid stenosis, last row: healthy control. First two cases showed a damage of retinal nerve fiber layer (RNLF) (A, E) which was more extensive in the NAION patient without carotid stenosis (A). Diffuse (A) and sectorial vascular perfusion defect (E) in en face optical coherence tomography angiograms in the radial peripapillary capillary (RPC) layer consistent with the blue areas on color vascular density map. OCT-A reveals a normal vascular network in the fellow eye of the NAION patient with carotid artery stenosis (J, K) and healthy control (N, O). Last column, B-scan image of the segmentation of the optic nerve head radial peripapillary capillary plexus of the subjects
Statistical analysis was performed with the Statistical Package for Social Sciences (SPSS) 26.0 version (IBM Corporation, New York, USA). The mean, standard deviation, maximum, minimum, frequency and ratio values were used as appropriate in the descriptive summary of the data. Normal distribution of the variables was assessed by the Kolmogorov–Smirnov test. The Mann–Whitney U test and the Kruskal–Wallis test were used for the comparison of quantitative data. A p value less than 0.05 was considered statistically significant.
Results
This study was designed to analyze data for NAION patients referred to have CDU from 2016 to 2020. Thirty NAION patients were evaluated with CDU in the present study. There were 14 patients with CS in the NAION group. Eight patients had contralateral CS, five patients had bilateral CS, and one patient had ipsilateral CS. The degree of stenosis was below the 50% mark in all fourteen patients.
Twenty-two of the 30 atrophic NAION patients and 9 controls were analyzed with OCT-A in the study. Nine of the 22 NAION patients (6 men and 3 women, age 60.3 ± 8.7 years) had CS; there was no CS in 13 NAION patients (6 men and 7women, age 55.0 ± 8.5 years). Patients were aged 59.82 ± 8.2 years (5 men and 4 women) in control group. Two patients with CS and three patients without CS had bilateral NAION. The mean BCVA (decimal) was 0.55 ± 0.30 in the CS-NAION patients, 0.45 ± 0.36 in the NCS-NAION patients and one in the control subjects. Of the 22 patients with NAION, 10 eyes from 9 NAION patients with CS and 16 eyes from 13 NAION patients without CS were imaged in the atrophic phase. Seventeen unaffected (fellow) eyes were also analyzed by OCT-A using the same quantitative method for comparison between the eyes with CS (n:7) and without CS (n:10). All 7 fellow eyes of CS-NAION patients had ipsilateral CS.
The mean GCC thickness parameters (μm) and RNLF thickness parameters (μm) were comparable between the CS-NAION, NCS-NAION patients and significantly lower in both of the groups than in the healthy controls. The quantitative results are presented in Table 1.
Table 1 shows the retinal peripapillary capillaries vessel density (RPC VD) (%) results for the peripapillary area in CS-NAION, NCS-NAION and control groups. The RPC VDs were significantly lower in all the sectors of the peripapillary area in both of the groups than in the healthy controls. This density was significantly lower in the temporal-superior (P = 0.037) and the superior-temporal (P = 0.012) sectors of the NCS-NAION patients than in the CS-NAION patients.
The mean GCC thickness (μm), RNLF thickness (μm) and RPC VD (%) results for the fellow eyes of the NAION patients are shown in Table 2. All of the measurements were comparable between the groups except for the visual acuity (P = 0.001 for both) (Table 2).
Fellow eyes and NAION eyes of both categories of patients showed similar disk area and cup to disk ratio, cup to disk volume ratio parameters as in healthy controls. The quantitative results are presented in Tables 1 and 2.
Discussion
The optic disk blood flow in NAION was previously investigated using various methods. Using a laser Doppler flowmeter, Leiba et al. demonstrated that the ONH blood flow in NAION eyes is significantly lower than that in healthy control eyes [14]. A decrease in peripapillary retinal perfusion has also been reported in NAION eyes by using Doppler OCT [15]. OCT-A is currently the preferred method for mapping ocular perfusion, including capillaries. Recently, several studies on ocular microvasculature in NAION have been reported. Some studies have examined NAION eyes with swollen disks using OCT-A, and reported the dilation of patent superficial capillaries in the peripapillary area [16] and the reduction of the peripapillary vascular density associated with the acute phase of NAION [6, 7]. Some other studies have also assessed microvascular changes in atrophic NAION eyes using OCT-A [8, 10, 17]. Liuet al. studied 13 eyes of 13 NAION patients and reported the quantitative OCT-A results for non-acute NAION eyes [9]. Similar to the present study, they found a reduced vascular density in peripapillary area. Two quantitative studies, also using Optovue devices, reported microvascular attenuation in the non-acute phase of NAION with correlation between the areas of vascular attenuation and RNFL atrophy or visual field loss [8, 10]. The authors proposed that the decreased RNFL and GCC owing to NAION results in decreased metabolic activities and blood flow via auto-regulatory mechanisms [8, 10, 17]. Of interest, the current study, which evaluated 22 patients with NAION and a control group, to the best of knowledge, is the first to investigate the association between NAION and carotid disease using the OCT-A derived vessel density measurements. In the present study, the eyes of the NAION patients were analyzed in subgroups based on the presence of CS, and contralateral unaffected eyes were included, in order to analyze the eventual possible differences with respect to healthy controls. This study confirmed the statistically significant vascular impairment occurring in NAION eyes, and there was a difference between the VD parameters in the sub-group analysis. VD showed significant reductions in superior-temporal region in NCS-NAION when compared to the CS-NAION patients. Previously, Yu et al. reported significantly smaller diameter RPCs in the temporal region [18]. Accordingly, it can be speculated that due to the capillaries with smaller diameters, the hemodynamic instabilities might affect the temporal sectors selectively. In the current study, all fellow eyes of the patients had ipsilateral CS. However, the fellow and normal eyes showed no significant difference in vessel density at the peripapillary region among the groups. These results indicate that the VD may not be affected in CS. It is worth noting that the degree of obstruction was below the 50% in all of the fellow eyes. However, the sample size was small to draw an accurate conclusion and more research is needed in the future, to confirm these findings as well as to determine the results in larger groups.
Keeping in mind that the human eye is an embryological protrusion of the brain and that the optic nerve is a tract of the brain, neuroimaging has been widely used to exclude neoplastic and other nervous system diseases affecting visual function and optic nerve. Magnetic resonance imaging and diffusion weighted magnetic resonance imaging have been widely employed for the evaluation of the optic nerve’s involvement of orbital disease and tumors [19,20,21]. The internal carotid artery supplies blood to the eye; therefore, the stenosis of the carotid artery caused by atherosclerosis may affect its visual functioning. A video fluorescein angiography study on 33 patients with carotid artery stenosis by Wolf et al. reported decreased retinal perfusion in all patients and prolonged arteriovenous passage of time in 18 of them [22]. Investigative modalities like CDU and computed tomography angiography (CTA) have been studied in the diagnosis of CS [23, 24]. CTA uses ionizing radiation and requires contrast agent administration. CDU is a cost effective, noninvasive and safe imaging modality that allows the operator to assess the caliber of the carotid arteries in addition to the blood flow and velocities. Operator variability is one of the biggest weaknesses of CDU as an imaging modality. The sensitivity and specificity of both imaging modalities decrease in low-grade CS [24].
The pathogenesis of acute NAION is believed to be multifactorial, including the acute hypo-perfusion of short posterior ciliary arteries [12, 25, 26] There has been no thrombosis demonstrated in the short posterior ciliary arteries in the histopathological studies performed in NAION eyes [27, 28]. This hypo-perfusion depends on several factors including variations in blood pressure, increase of intraocular pressure, local vasculopathy and impairment in blood flow autoregulation [12, 26]. There is a complex vascular supply to the eye. Kaup et al. compared the retrobulbar hemodynamics of patients with acute NAION with healthy age‐matched controls and reported that the ophthalmic artery showed no differences in hemodynamics between patients with NAION and controls [29]. In the present study, 14 of the 30 NAION patients had carotid artery stenosis. In carotid artery disease, the association of NAION has been studied previously. Hayreh et al. evaluated a cohort of 266 eyes with NAION and found a 51% prevalence of carotid artery plaques in the involved side [30]. Zhu et al. demonstrated that the presence of carotid artery plaque was more frequent in the patients with NAION, compared to either the hypertensive group or the normal controls, indicating that NAION may be associated with carotid artery atherosclerosis [31]. Although it was found that the carotid disease was more often in NAION patients, the mechanism is unclear. Zhu et al. suggested that the association might be due to similar pathological changes of the inner vascular walls in the carotid artery and the arteries supplying the optic nerve head. Carotid artery stenosis results in decrease of blood pressure in the ocular vascular bed, and the severity of blood flow reduction depends upon the degree of stenosis. In carotid artery disease, hemodynamic disturbances can also be produced by other mechanisms. One possible explanation might be the disruption of vazomotor autoregulation. It has been showed that the serotonin released by platelets aggregation on atherosclerotic plaques in the carotid artery may trigger transient vasospastic occlusion [32]. Recently, Mense et al. demonstrated that patients with CS had impaired baroreceptor reflex and reduced cerebral autoregulation, which could lead to hemodynamic insufficiency [33]. It is not known why the sensitivity of baroreceptors in the carotid sinus is impaired in patients with CS. Previously Kitagawa proposed that the thickness and rigidity of carotid atheromatous plaque could impede the transmission of intraluminal pressure to the adventitia where baroreceptors exist [34].
Given that the CS was at the contralateral side in most of the NAION patients, this result was unexpected. Based on the findings of the current study, it can be suggested that the CS might activate the compensatory mechanisms to avoid the reduction of the ocular blood flow on the ipsilateral side in chronic situations. These mechanisms might be protective against the serious perfusion reduction which could be responsible for an irreversible vascular damage. However, this hypothesis requires further studies to be proved.
The study had several limitations. One of the main drawbacks was the small study population. This is a cross-sectional study with a single observation at one specific point, and therefore, larger scale prospective longitudinal studies with the implementation of both OCT-A and carotid imaging must be conducted to obtain data that are more reliable. Additionally, vasculature in different layers was not evaluated due to the limits of the current technology. Finally, here, this study focused on carotid disease, yet retro-orbital circulation was not analyzed.
In conclusion, this study showed normal VD of the clinically normal fellow eyes in the presence of CS in NAION. Further prospective studies with a large number of patients are warranted to elucidate the associations between carotid disease and NAION and to investigate the pathophysiology of NAION. Larger prospective longitudinal studies will need to be conducted in order to clarify the long-term effect of CS on ocular vasculature.
References
Gonul S, Koktekir BE, Bakbak B et al (2013) Comparison of the ganglion cell complex and retinal nerve fibre layer measurements using Fourier domain optical coherence tomography to detect ganglion cell loss in non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol 97(8):1045–1050
Aggarwal D, Tan O, Huang D et al (2012) Patterns of ganglion cell complex and nerve fiber layer loss in nonarteritic ischemic optic neuropathy by Fourier-domain optical coherence tomography. Invest Ophthalmol Vis Sci 53(8):4539–4545
Goto K, Miki A, Araki S et al (2016) Time course of macular and peripapillary inner retinal thickness in non-arteritic anterior ischaemic optic neuropathy using spectral-domain optical coherence tomography. Neuroophthalmology 40(2):74–85
Oto S, Yilmaz G, Cakmakci S et al (2002) Indocyanine green and fluorescein angiography in nonarteritic anterior ischemic optic neuropathy. Retina 22:187–191
Arnold AC, Hepler RS (1994) Fluorescein angiography in acute nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol 117:222–230
Rougier MB, Delyfer MN, Korobelnik JF (2017) OCT angiography of acute non-arteritic anterior ischemic optic neuropathy. J Fr Ophtalmol 40:102–109
Sharma S, Ang M, Najjar RP, Sng C, Cheung CY et al (2017) Optical coherence tomography angiography in acute non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol 101:1045–1051
Wright Mayes E, Cole ED, Dang S et al (2017) Optical coherence tomography angiography in nonarteritic anterior ıschemic optic neuropathy. J Neuroophthalmol 37(4):358–364
Liu CH, Wu WC, Sun MH et al (2017) Comparison of the retinal microvascular density between open angle glaucoma and nonarteritic anterior ıschemic optic neuropathy. Invest Ophthalmol Vis Sci 58(9):3350–3356
Hata M, Oishi A, Muraoka Y et al (2017) Structural and functional analyses in nonarteritic anterior ıschemic optic neuropathy: optical coherence tomography angiography study. J Neuroophthalmol 37(2):140–148
Burde RM (1993) Optic disk risk factors for nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol 116:759–764
Hayreh SS (2000) Ischaemic optic neuropathy. Indian J Ophthalmol 48(3):171–194
Metzler W, Kessler G, Benzer W et al (1990) Ophthalmologische Bedeutung stenosierender Karotisprozesse [Ophthalmological significance of stenosing carotid processes]. Wien Med Wochenschr 140(14):387–389
Leiba H, Rachmiel R, Harris A et al (2000) Optic nerve head blood flow measurements in non-arteritic anterior ischaemic optic neuropathy. Eye (Lond) 14(Pt 6):828–833
Wang Y, Fawzi AA, Varma R et al (2011) Pilot study of optical coherence tomography measurement of retinal blood flow in retinal and optic nerve diseases. Invest Ophthalmol Vis Sci 52:840–845
Gaier ED, Wang M, Gilbert AL et al (2018) Quantitative analysis of optical coherence tomographic angiography (OCT-A) in patients with non-arteritic anterior ischemic optic neuropathy (NAION) corresponds to visual function. PLoS ONE 13(6):e0199793
Higashiyama T, Ichiyama Y, Muraki S et al (2016) Optical coherence tomography angiography in a patient with optic atrophy after non-arteritic anterior ischaemic optic neuropathy. Neuroophthalmology 40(3):146–149
Yu PK, Cringle SJ, Yu DY (2014) Correlation between the radial peripapillary capillaries and the retinal nerve fibre layer in the normal human retina. Exp Eye Res 129:83–92
Razek AA, Elkhamary S (2011) MRI of retinoblastoma. Br J Radiol 84(1005):775–784
Abdel Razek AA, Elkhamary S, Al-Mesfer S, Alkatan HM (2012) Correlation of apparent diffusion coefficient at 3T with prognostic parameters of retinoblastoma. AJNR Am J Neuroradiol 33(5):944–948
Eissa L, Abdel Razek AAK, Helmy E (2021) Arterial spin labeling and diffusion-weighted MR imaging: utility in differentiating idiopathic orbital inflammatory pseudotumor from orbital lymphoma. Clin Imaging 71:63–68
Wolf S, Rebstock J, Bertram B et al (1989) Retinal hemodynamics and morphologic findings in patients with occlusion of the internal carotid artery. Fortschritte der Ophthalmologie: Zeitschrift der Deutschen Ophthalmologischen Gesellschaft 86(4):339–342
Abdel Razek AA, Denewer AT, Hegazy MA, Hafez MT (2014) Role of computed tomography angiography in the diagnosis of vascular stenosis in head and neck microvascular free flap reconstruction. Int J Oral Maxillofac Surg 43(7):811–815
Forjoe T, Asad Rahi M (2019) Systematic review of preoperative carotid duplex ultrasound compared with computed tomography carotid angiography for carotid endarterectomy. Ann R Coll Surg Engl 101(3):141–149
Hayreh SS, Zimmerman MB, Podhajsky P et al (1994) Nocturnal arterial hypotension and its role in optic nerve head and ocular ischemic disorders. Am J Ophthalmol 117:603–624
Arnold AC (2003) Pathogenesis of nonarteritic anterior ischemic optic neuropathy. J Neuroophthalmol 23:157–163
Knox DL, Duke JR (1971) Slowly progressive ischemic optic neuropathy: A clinicopathologic case report. Trans Am Acad Ophthalmol Otolaryngol 75(5):1065–1068
Levin LA, Louhab A (1996) Apoptosis of retinal ganglion cells in anterior ischemic optic neuropathy. Arch Ophthalmol 114(4):488–491
Kaup M, Plange N, Arend KO, Remky A (2006) Retrobulbar haemodynamics in non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol 90(11):1350–1353. https://doi.org/10.1136/bjo.2006.093559
Hayreh SS, Zimmerman MB (2017) Ocular arterial occlusive disorders and carotid artery disease. Ophthalmol Retina Jan-Feb 1(1):12–18
Zhu W, Chen T, Jin L et al (2017) Carotid artery intimal medial thickness and carotid artery plaques in hypertensive patients with non-arteritic anterior ischaemic optic neuropathy. Graefes Arch Clin Exp Ophthalmol 255(10):2037–2043
Hayreh SS, Piegors DJ, Heistad DD (1997) Serotonin induced constriction of ocular arteries in atherosclerotic monkeys: Implications for ischemic disorders of retina and optic nerve head. Arch Ophthalmol 115:220–228
Mense L, Reimann M, Rüdiger H et al (2010) Autonomic function and cerebral autoregulation in patients undergoing carotid endarterectomy. Circ J 74:2139–2145
Kitagawa K (2010) Carotid stenosis, baroreceptor sensitivity and cerebral autoregulation – implication for cerebral hyperperfusion syndrome. Circ J 74(10):2058–2059
Acknowledgements
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Istanbul Bakırköy Dr. Sadi Konuk Research and Education Hospital (Date 2020/No 12).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaya, F.S. Carotid disease and retinal optical coherence tomography angiography parameters in patients with non-arteritic anterior ischemic optic neuropathy. Int Ophthalmol 42, 123–131 (2022). https://doi.org/10.1007/s10792-021-02007-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-02007-5