Abstract
Cribriform-morular variant (CMV) is a rare subtype of papillary thyroid carcinoma (PTC) that is associated with familial adenomatous polyposis (FAP). Given the high likelihood for multi-organ malignancies in FAP patients, this study explores the yield of diagnosing occult FAP among CMV-PTC patients. Institutional database was searched in order to identify patients with pathologically-confirmed CMV-PTC from 2000 to 2012. Medical records were reviewed, and clinical and pathological features were analyzed. Eleven cases of CMV were identified from 6,901 patients with PTC, for a prevalence of 0.16 %. All 11 patients were female. The median age at CMV-PTC diagnosis was 36 years (range 18–46). Two patients had pre-existing FAP at the time of PTC diagnosis. The other nine patients were referred for colonoscopy and/or genetic testing. Six patients underwent colonoscopy and one (17 %) was diagnosed with FAP based on polyposis phenotype and genetic testing. The mean age of patients at the time of CMV-PTC diagnosis was younger in the FAP group (23 years, range 18–34) than in the sporadic group (37 years, range 25–46). All three patients with FAP-associated CMV-PTC had multicentric tumors, while all five sporadic patients did not. Our study found that approximately one-sixth of patients with CMV-PTC may have occult FAP. Patients with FAP-associated CMV-PTC appear to be younger and more likely to have multicentric tumors than those with sporadic CMV-PTC. Due to the increased risk of malignancy in patients with FAP, patients with CMV-PTC should be referred for colonoscopy and/or genetic evaluation for FAP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cribriform-morular variant (CMV) is a rare subtype of papillary thyroid carcinoma (PTC) that is often associated with familial adenomatous polyposis (FAP) [1, 2]. Since FAP, which is inherited in an autosomal dominant fashion, is characterized by multiple adenomatous polyps in the colon and rectum and a near certainty of developing colorectal cancer unless a risk-reducing prophylactic colectomy is performed, early identification and intervention in FAP patients is essential. FAP is also associated with several extracolonic malignancies, including malignancies of the upper gastrointestinal tract, hepatobiliary tract, central nervous system, and endocrine system [3]. While many individuals are diagnosed with FAP due to the discovery of colorectal polyps, the identification of CMV histology in patients with PTC provides clinicians with a unique opportunity to diagnose occult cases of FAP.
The prevalence of PTC among individuals with FAP has been reported to be 0.4–12 % [1, 4–11], and several institutions have recently implemented prospective thyroid ultrasound (US) screening programs to increase early detection of thyroid abnormalities in the FAP population [10, 12, 13]. Forty-five years after the relationship between FAP and PTC was first identified [14]. Harach et al. discovered that many cases of FAP-associated PTC had distinct pathological features, including a cribriform pattern [2]. Although CMV accounts for only approximately 0.16 % of all PTC cases [15], reports suggest that up to 90 % of FAP-associated PTC have CMV histology [4]. One of seven (14.3 %) FAP patients with PTC in our institution’s Hereditary Colorectal Cancer Family Registry has CMV morphology [13].
The purpose of this study is to evaluate the yield of diagnosing occult cases of FAP among patients with CMV-PTC at a specialized cancer care center over a 12-year period, and to enhance the small body of literature on this topic by further clarifying any clinical or pathological features that could possibly distinguish FAP-associated CMV-PTC from sporadic CMV-PTC.
Methods
The medical records of patients with pathologically-confirmed diagnoses of CMV-PTC between 2000 and 2012 were retrospectively reviewed within a specialized cancer care center. Demographic and clinical data including age, sex, and personal and family history of polyps and/or thyroid disease were extracted. Pathology reports were analyzed for clinical features of CMV-PTC. Referrals for colonoscopy and/or genetic testing for FAP and subsequent test results were recorded. Fisher’s exact and the Mann–Whitney U tests were used to detect statistical differences for categorical and continuous variables, respectively.
Results
Eleven pathologically-confirmed cases of CMV-PTC were identified from a total of 6,901 patients with PTC who were treated at our institution during the study period, for an estimated prevalence of 0.16 %. All 11 (100 %) patients with CMV-PTC were female. The median age at diagnosis of CMV-PTC was 36 years (range 18–46). One (9 %) patient had a personal history of benign thyroid disease. Five (46 %) patients had personal or family histories of colonic polyps. The patients in the study cohort underwent thyroid evaluation for various reasons. Five (46 %) patients were found to have an enlarged thyroid on routine physical examination. Three (27 %) patients sought medical workup due to symptoms of lethargy, neck pain, dizziness and vertigo. One (9 %) patient self-detected a thyroid mass, while the reasons for thyroid evaluation of two (18 %) patients are unknown.
The clinical and pathological features and treatment of the 11 cases of CMV-PTC are summarized in Table 1. Photomicrographs of PTC and CMV-PTC are displayed in Fig. 1. To the best of our knowledge, no patient has had PTC recurrence. One patient, who also had FAP, died 1.9 years after CMV-PTC diagnosis due to progressive peritoneal carcinomatosis from an ovarian cancer.
Histology of PTC versus CMV-PTC. Hematoxylin and eosin sections of PTC and CMV-PTC cases, courtesy of Nora Katabi, MD. PTC-classical type is characterized by papillary architecture (a), while CMV-PTC shows focal papillary architecture and is characterized by cribriform pattern (b) and squamoid morules (c)
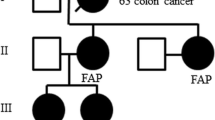
Two of the 11 (18 %) patients had pre-existing diagnoses of FAP at the time of PTC diagnosis. The other nine patients were all referred for colonoscopy and/or genetic testing by their physicians because of a CMV-PTC diagnosis. Three of the nine referred patients were lost to follow up and did not, according to available records, undergo a colonoscopy or genetic testing. Of the six patients who did undergo colonoscopy, one (17 %) was diagnosed with FAP based on polyposis phenotype and subsequent confirmation with genetic testing. The remaining five patients had negative colonoscopies; two of those patients also underwent genetic counseling due to a family history of colorectal polyps. Of these two patients, one underwent genetic testing which was negative for an APC gene mutation, while the other was precluded from testing due to insurance issues. A schematic of the referral of patients with CMV-PTC for genetic workup is displayed in Fig. 2. In sum, the overall prevalence of FAP among patients with CMV-PTC in our institution is 27 % (3 of the 11).
Our cohort contains three patients with FAP-associated CMV and five patients with sporadic CMV-PTC, as determined by colonoscopy and/or genetic testing (excluding the three patients who were lost to follow up from either group). The mean age of patients in the FAP group at the time of CMV-PTC diagnosis was 23 years (range 18–34), while the mean age of patients in the sporadic group was 37 years (range 25–46) (p = 0.03). In addition, all three patients with FAP-associated CMV-PTC had multicentric tumors, while the five patients without FAP did not (p = 0.04). All three patients with FAP had PTC located in both the right and left lobes, while four of the five patients without FAP had PTC located in only one lobe, though no statistical significance was noted. Though no other striking differences between the two groups were identified, all patients with FAP had aberrant B-catenin staining, consistent with the theory that the loss of function of the adenomatous polyposis coli (APC) gene causes B-catenin to accumulate in the nuclei of syndrome-related carcinomas (Table 2) [16, 17].
Discussion
In our study, one of six (17 %) patients with CMV-PTC who underwent colonoscopy was found to have occult FAP. This incidence is slightly lower than that of a Japanese study in which two of six (33 %) patients with CMV-PTC were found to have colonic polyps and a mutation of the APC gene [15]. However, the overall prevalence of FAP in our CMV-PTC cohort is three of 11 (27 %). Other studies include a few case reports of patients who were screened for FAP after being diagnosed with CMV-PTC, and are therefore not able to comment on incidence or prevalence [18–20].
Several recent studies have tried to determine clinical or pathological features that may distinguish FAP-associated CMV-PTC from sporadic CMV-PTC. The Japanese group found that patients with FAP-associated CMV-PTC tended to have multiple tumors compared to the sporadic group. Patient age and tumor size were not statistically different between the two groups [21]. Another retrospective study describes 11 female patients with CMV-PTC and one male with typical PTC histology and noted trends toward young age (average 23.5 years for CMV-PTC), multicentricity (66 %), and bilateral tumors (42 %) [4]. Our data confirms these observations and suggests that patients with FAP-associated CMV-PTC are more likely to be younger and have bilateral and multicentric tumors than patients with sporadic CMV-PTC. While some studies have found that CMV-PTC is generally indolent regardless of whether or not it is associated with FAP [4, 18, 21–23], several of our cases had aggressive histological findings such as lymph node metastases, capsular invasion, and extrathyroid extension.
A major limitation of our study is the small cohort, particularly in the FAP-associated CMV group. However, since FAP and CMV are both rare, amassing a large cohort of patients is challenging for a single institution. In a recent analysis of characteristics that may be associated with FAP-associated versus sporadic CMV-PTC, the Japanese group reported only 12 patients with FAP-associated CMV-PTC in 19 years. However, their cohort of patients may have been enhanced due to their relatively loose inclusion criteria. Patients in their study were considered to have FAP if they had family histories of colonic polyposis or colorectal cancer, regardless of whether they themselves underwent evaluation for FAP. Our study did not consider a family history alone to be sufficient for a diagnosis of FAP, since individuals with FAP transmit the condition to only 50 % of their offspring. In addition, it is possible that some cases of colonic polyposis from the Japanese group may be attributed to other forms of adenomatous polyposis, such as attenuated FAP (AFAP) or MYH-associated polyposis (MAP), which has an autosomal recessive hereditary pattern with variations in penetrance and presumably differences in cancer risks. It is unknown whether patients with other polyposis syndromes are also at risk for CMV-PTC [21].
The Japanese study also designated patients who did not undergo workup for FAP as part of the sporadic group, even though up to 30 % of FAP cases can be attributed to de novo mutations and will not have a family history of polyposis or colorectal cancer [24–27]. Therefore, some cases of FAP may have been missed in the Japanese study CMV-PTC cohort. In contrast, our study was fairly conservative and excluded patients without colonoscopic and/or genetic evaluation from the analyses.
Given the rarity of both CMV-PTC and FAP, further studies are required to determine the prevalence of FAP among patients with CMV-PTC and to investigate whether clinical and/or pathological features, such as a younger age and/or multicentric tumors, can distinguish FAP-associated from sporadic CMV-PTC. Until then, we believe that since a significant proportion of patients with CMV-PTC may potentially harbor occult FAP, these patients should be referred for colonoscopy and/or genetic evaluation for FAP.
References
Cetta F, Pelizzo MR, Curia MC, Barbarisi A (1999) Genetics and clinicopathological findings in thyroid carcinomas associated with familial adenomatous polyposis. Am J Pathol 155(1):7–9. doi:10.1016/S0002-9440(10)65091-2
Harach HR, Williams GT, Williams ED (1994) Familial adenomatous polyposis associated thyroid carcinoma: a distinct type of follicular cell neoplasm. Histopathology 25(6):549–561
Gibbons DC, Sinha A, Phillips RK, Clark SK (2011) Colorectal cancer: no longer the issue in familial adenomatous polyposis? Fam Cancer 10(1):11–20. doi:10.1007/s10689-010-9394-x
Perrier ND, van Heerden JA, Goellner JR, Williams ED, Gharib H, Marchesa P, Church JM, Fazio VW, Larson DR (1998) Thyroid cancer in patients with familial adenomatous polyposis. World J Surg 22(7):738–742 discussion 743
Giardiello FM, Offerhaus GJ, Lee DH, Krush AJ, Tersmette AC, Booker SV, Kelley NC, Hamilton SR (1993) Increased risk of thyroid and pancreatic carcinoma in familial adenomatous polyposis. Gut 34(10):1394–1396
Bulow S, Holm NV, Mellemgaard A (1988) Papillary thyroid carcinoma in Danish patients with familial adenomatous polyposis. Int J Colorectal Dis 3(1):29–31
Bulow C, Bulow S (1997) Is screening for thyroid carcinoma indicated in familial adenomatous polyposis? The Leeds Castle polyposis group. Int J Colorectal Dis 12(4):240–242
van der Linde K, Vasen HF, van Vliet AC (1998) Occurrence of thyroid carcinoma in Dutch patients with familial adenomatous polyposis. An epidemiological study and report of new cases. Eur J Gastroenterol Hepatol 10(9):777–781
Plail RO, Bussey HJ, Glazer G, Thomson JP (1987) Adenomatous polyposis: an association with carcinoma of the thyroid. Br J Surg 74(5):377–380
Herraiz M, Barbesino G, Faquin W, Chan-Smutko G, Patel D, Shannon KM, Daniels GH, Chung DC (2007) Prevalence of thyroid cancer in familial adenomatous polyposis syndrome and the role of screening ultrasound examinations. Clin Gastroenterol Hepatol 5(3):367–373. doi:10.1016/j.cgh.2006.10.019
Steinhagen E, Guillem JG, Chang G, Salo-Mullen EE, Shia J, Fish S, Stadler ZK, Markowitz AJ (2012) The prevalence of thyroid cancer and benign thyroid disease in patients with familial adenomatous polyposis may be higher than previously recognized. Clin Colorectal Cancer 11(4):304–308. doi:10.1016/j.clcc.2012.01.006
Jarrar AM, Milas M, Mitchell J, Laguardia L, O’Malley M, Berber E, Siperstein A, Burke C, Church JM (2011) Screening for thyroid cancer in patients with familial adenomatous polyposis. Ann Surg 253(3):515–521. doi:10.1097/SLA.0b013e3181fcba8a
Steinhagen E, Hui VW, Levy RA, Markowitz AJ, Fish S, Wong RJ, Sood R, Ochman SM, Guillem JG (In press) Results of a prospective thyroid utrasound screening program in adenomatous polyposis patients. Am J Surg
Crail HW (1949) Multiple primary malignancies arising in the rectum, brain, and thyroid; report of a case. US Nav Med Bull 49(1):123–128
Tomoda C, Miyauchi A, Uruno T, Takamura Y, Ito Y, Miya A, Kobayashi K, Matsuzuka F, Kuma S, Kuma K, Kakudo K (2004) Cribriform-morular variant of papillary thyroid carcinoma: clue to early detection of familial adenomatous polyposis-associated colon cancer. World J Surg 28(9):886–889
Kurihara K, Shimizu S, Chong J, Hishima T, Funata N, Kashiwagi H, Nagai H, Miyaki M, Fukayama M (2000) Nuclear localization of immunoreactive beta-catenin is specific to familial adenomatous polyposis in papillary thyroid carcinoma. Jpn J Cancer Res 91(11):1100–1102
Boonyaarunnate T, Olson MT, Bishop JA, Yang GC, Ali SZ (2013) Cribriform morular variant of papillary thyroid carcinoma: clinical and cytomorphological features on fine-needle aspiration. Acta Cytol 57(2):127–133. doi:10.1159/000345879
Cameselle-Teijeiro J, Chan JK (1999) Cribriform-morular variant of papillary carcinoma: a distinctive variant representing the sporadic counterpart of familial adenomatous polyposis-associated thyroid carcinoma? Mod Pathol 12(4):400–411
Chikkamuniyappa S, Jagirdar J (2004) Cribriform-morular variant of papillary carcinoma: association with familial adenomatous polyposis—report of three cases and review of literature. Int J Med Sci 1(1):43–49
Schaeffer DF, Yoshida EM, Owen DA, Berean KW (2011) Familial adenomatous polyposis-rendering a diagnosis based on recognition of an unusual primary thyroid neoplasm. Case Rep Med 2011:767610. doi:10.1155/2011/767610
Ito Y, Miyauchi A, Ishikawa H, Hirokawa M, Kudo T, Tomoda C, Miya A (2011) Our experience of treatment of cribriform morular variant of papillary thyroid carcinoma; difference in clinicopathological features of FAP-associated and sporadic patients. Endocr J 58(8):685–689
Ng SB, Sittampalam K, Goh YH, Eu KW (2003) Cribriform-morular variant of papillary carcinoma: the sporadic counterpart of familial adenomatous polyposis-associated thyroid carcinoma. A case report with clinical and molecular genetic correlation. Pathology 35(1):42–46
Xu B, Yoshimoto K, Miyauchi A, Kuma S, Mizusawa N, Hirokawa M, Sano T (2003) Cribriform-morular variant of papillary thyroid carcinoma: a pathological and molecular genetic study with evidence of frequent somatic mutations in exon 3 of the beta-catenin gene. J Pathol 199(1):58–67. doi:10.1002/path.1225
Evans DG, Howard E, Giblin C, Clancy T, Spencer H, Huson SM, Lalloo F (2010) Birth incidence and prevalence of tumor-prone syndromes: estimates from a UK family genetic register service. Am J Med Genet Part A 152A(2):327–332. doi:10.1002/ajmg.a.33139
Patel SG, Ahnen DJ (2012) Familial colon cancer syndromes: an update of a rapidly evolving field. Curr Gastroenterol Rep 14(5):428–438. doi:10.1007/s11894-012-0280-6
Newton KF, Mallinson EK, Bowen J, Lalloo F, Clancy T, Hill J, Evans DG (2012) Genotype-phenotype correlation in colorectal polyposis. Clin Genet 81(6):521–531. doi:10.1111/j.1399-0004.2011.01740.x
Sinha A, Tekkis PP, Rashid S, Phillips RK, Clark SK (2010) Risk factors for secondary proctectomy in patients with familial adenomatous polyposis. Br J Surg 97(11):1710–1715. doi:10.1002/bjs.7202
Conflict of interest
The authors declare no conflicts of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Levy, R.A., Hui, V.W., Sood, R. et al. Cribriform-morular variant of papillary thyroid carcinoma: an indication to screen for occult FAP. Familial Cancer 13, 547–551 (2014). https://doi.org/10.1007/s10689-014-9732-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-014-9732-5