Abstract
Cribriform-morular variant of papillary thyroid carcinoma (CMV-PTC) is rare and constitutes less than 0.5% of all PTC. CMV-PTC typically affects young adults with a female predominance, showing a female-to-male ratio of 17:1. It is commonly associated with familial adenomatous polyposis and has a germline mutation in the adenomatous polyposis coli (APC) gene. However, sporadic form without FAP has been also reported. Preoperative diagnosis of CMV-PTC is important. As CMV-PTC with FAP usually displays multifocal nodules, total thyroidectomy is required. On the other hand, lobectomy is sufficient for sporadic cases because of solitary nodule and excellent prognosis. In this chapter, we describe the diagnostic clue of CMV-PTC.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
28.1 Introduction
Cribriform-morular variant of papillary thyroid carcinoma (CMV-PTC) is rare and constitutes less than 0.5% of all PTC [1]. CMV-PTC typically affects young adults with a female predominance, showing a female-to-male ratio of 17:1 [1]. It is commonly associated with familial adenomatous polyposis (FAP) and has a germline mutation in the adenomatous polyposis coli (APC) gene [2, 3]. However, sporadic form without FAP has been also reported.
Preoperative diagnosis of CMV-PTC is important. As CMV-PTC with FAP usually displays multifocal nodules, total thyroidectomy is required. On the other hand, lobectomy is sufficient for sporadic cases because of solitary nodule and excellent prognosis. In addition, the fact that colonic polyposis may be detected after the diagnosis of CMV-PTC indicates the necessity of preoperative colonoscopy and/or APC gene analysis [1]. Therefore, aspiration cytology bears an important responsibility in the management of this variant. Herein, we described the diagnostic clue of CMV-PTC.
28.2 Case
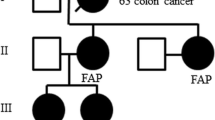
The case was a 21-year-old woman. She was pointed out to have nodules in the anterior neck by a medical checkup. As aspiration cytology was suspicious for malignancy, she was referred to our hospital for surgical therapy. Ultrasonographic examination revealed two nodules in the thyroid. The nodule located in the left lobe measured 8 mm × 5 mm × 7 mm. It was hypoechoic, homogeneous, and not associated with fine strong echoes. The border of the mass was well-defined (Fig. 28.1). Color Doppler ultrasound showed that it was hypovascular. Ultrasonographic interpretation was a malignancy, and CMV-PTC was suspected by aspiration cytology. Another nodule located in the right lobe, measuring 11 mm × 3 mm × 6 mm, was interpreted as a benign nodule by ultrasonographic and cytological examinations. She underwent a left thyroid lobectomy including isthmus with central neck dissection. Colonic examination performed after the microscopic diagnosis of CMV-PTC did not detect any abnormalities. A test for APC gene mutation was not permitted. Her parents had no history of polyposis coli and thyroid tumors.
28.3 Cytological Findings
Aspirated material was cellular. There were a small number of foamy histiocytes in the background. Colloid materials were not seen. Carcinoma cells appeared as papillary or cribriform clusters. The cribriform clusters exhibited slit-like empty spaces and anastomosing bars (Fig. 28.2). Papillary clusters partially showed nuclear palisading (Fig. 28.3). Some clusters contained small hyaline materials. Carcinoma cell nests with eddy formation were scattered (Fig. 28.4). Most of the carcinoma cells were tall columnar and their N/C ratios were low. Isolated carcinoma cells looked like spindle or elongated cells. The cytoplasm was weakly stained with light green, even in the carcinoma cells forming morules. A few carcinoma cells showed vacuolated cytoplasm (cytoplasmic lipid accumulation, CLIA) (Fig. 28.5). Metaplastic cytoplasm showing dense cytoplasm was not observed. Tail-like cytoplasmic elongation was observed at the periphery of the cell clusters (Fig. 28.6). The nuclei were round, oval, or short spindle and exhibited nuclear grooves and intranuclear cytoplasmic inclusions. The nuclear chromatin was not ground glass-like, but granular (Fig. 28.7). Some morular cells showed peculiar nuclear clearing that occupied most of the nuclei and directly surrounded by a nucleoplasm (Fig. 28.8).
28.4 Pathological Findings
The tumor was located in the left lobe of the thyroid and measured 7 mm × 5 mm. On cut surface, it was solid and lobulated (Fig. 28.9). It was well-encapsulated and did not invade the surrounding thyroid tissue. Microscopically, the carcinoma cells showed cribriform (Fig. 28.10), papillary, solid, and follicular pattern. The cribriform pattern was formed by anastomosing bars and arches of carcinoma cells without intervening stroma. There was no colloid in the lumen. The morules were scattered in the solid area. Papillary area was composed of tall columnar carcinoma cells. The cytoplasm was slightly eosinophilic. The nuclei were round to spindle and represented cytoplasmic inclusions (Fig. 28.11). Peculiar nuclear clearing was observed in some of the morular cells (Fig. 28.12). The chromatin pattern was granular. Ground glass pattern consistent with classic papillary carcinoma was not observed. There were no psammoma bodies. Lymph node was not identified. Immunohistochemically, the carcinoma cells showed nuclear and cytoplasmic positivity for beta-catenin (Fig. 28.13). Thyroglobulin was almost negative (Fig. 28.14). Estrogen receptor was positive except for morular cells (Fig. 28.15).
28.5 Discussion
CMV-PTC is considered by some to constitute a distinct category of thyroid carcinoma. It can occur in a sporadic form or as a manifestation of FAP. It occurs almost exclusively in young adult females. A sporadic form occurs in patients who do not carry a germline mutation of APC gene. Sporadic cases are usually solitary, whereas cases associated with FAP are often multifocal [4]. The prognosis is excellent, and nodal metastasis is relatively rare (Table 28.1) [5].
This variant is histologically characterized by an intricate blending of cribriform, follicular, papillary, trabecular, and solid patterns with the morules (Table 28.2). The cribriform pattern is formed by anastomosing bars and arches of carcinoma cells without intervening stroma and resembles ductal carcinoma of the breast. The lumen of the cribriform pattern is usually devoid of colloid. The carcinoma cells showing papillary growth are tall columnar, and the nuclei frequently display pseudostratification. Trabecular arrangement may be reminiscent of hyalinizing trabecular tumor (see Chap. 34). Among thyroid carcinomas, the morules appear limited to this variant. Nuclear chromatin is fine granular and ground glass appearance is obscure. Peculiar nuclear clearing characteristic of this variant tends to be observed in the morules [6]. According to the report by Hirokawa et al., the cytology of CMV-PTC is characterized by (1) hypercellularity, (2) papillary arrangement composed of tall columnar cells, (3) cribriform pattern, (4) morules, (5) spindle cells, (6) obscure ground glass nuclei, (7) pale-staining nuclei with thickened nuclear membranes (peculiar nuclear clearing), (8) foamy or hemosiderin-laden histiocytes, (9) hyaline materials, and (10) no colloid in the background [7].
Papillary arrangement is frequently seen in CMV-PTC. However, the finding is not important to diagnose CMV-PTC, because it is common to conventional PTC. Cribriform structure is characterized by slit-like empty spaces and anastomosing bars within cell clusters [8]. Insular carcinoma and follicular neoplasm may also present cribriform pattern. In such tumors, the spaces are small in size and round and may contain colloid. In contrast, the spaces seen in CMV-PTC are larger in size and not round and do not contain any colloid. Tall columnar cells are easily identified in CMV-PTC as carcinoma cells showing nuclear palisading and low N/C ratio. Tail-like cytoplasmic elongation is also consistent with tall columnar cells [9]. Tall columnar cells are also seen in tall cell variant and columnar cell variant of PTC (see Chaps. 27 and 29). Pseudostratified nuclei, hyperchromasia, and nuclear atypia are helpful in distinguishing columnar cell variant from CMV-PTC. The distinction of columnar cells between CMV-PTC and tall cell variant is difficult. The age of the patient may be useful. The latter occurs in elder persons. Morules are cell clusters with eddy formations [8, 9]. They may mimic squamous metaplasia. Compared with squamous metaplasia, the cytoplasm of carcinoma cells forming the morules is not densely stained. The spindle cells singly appear in the background [10]. Recently, Takada et al. reported that CLIA is a characteristic feature of CMV-PTC [11]. The vacuoles tended to distribute in the subnuclear portion of carcinoma cells showing papillary growth and were positive for oil red O staining and adipophilin (Fig. 28.16).
Similar to conventional PTC, CMV-PTC presents intranuclear cytoplasmic inclusions and nuclear grooves. However, ground glass appearance is obscure (Table 28.3). The chromatin seen in CMV-PTC is granular, and it mimics that of follicular neoplasm or medullary carcinoma. Intranuclear cytoplasmic inclusions are less common than in the conventional PTC (58% of cases) [12]. The presence of peculiar nuclear clearing is very useful for the diagnosis of CMV-PTC [9]. It is identified which as pale staining which is occupying most of the nuclei and usually accompanied by condensed chromatin at the periphery of the nuclei. It is distinguished from cytoplasmic inclusions by cytoplasmic staining and sharp circumscription with the nuclear membrane.
Immunocytochemical staining is very useful in diagnosing CMV-PTC. When this variant is suspected, we routinely stain beta-catenin (Fig. 28.17), estrogen receptor (Fig. 28.18), and progesterone receptor. Beta-catenin reveals nuclear and cytoplasmic immunoreactivity [13, 14]. In contrast, conventional PTC reacts with the cell membrane against the antibody. CMV-PTC shows strong nuclear positivity for estrogen receptor and progesterone receptor, except for morular cells [15]. Conventional PTC is negative for them.
References
Nikiforov YE. Diagnostic pathology and molecular genetics of the thyroid: a comprehensive guide for practicing thyroid pathology. Philadelphia: Lippincott Williams & Wilkins; 2009. p. 191–2.
Harach HR, Williams GT, Williams ED. Familial adenomatous polyposis associated thyroid carcinoma: a distinct type of follicular cell neoplasm. Histopathol. 1994;25:549–61.
Cetta F, Toti P, Petracci M, et al. Thyroid carcinoma associated with familial adenomatous polyposis. Histopathol. 1997;31:231–6.
Rosai J, Albores Saavedra J, Asioli S, et al. Papillary tyroid carcinoma. In: Lloyd RV, Osamura RY, Kloppel G, Rosai J, editors. World Health Organization Classification of tumours of endocrine organs. 4th ed. Lyon: IARC; 2017. p. 87.
Lam AK, Saremi N. Cribriform-morular variant of papillary thyroid carcinoma: a distinctive type of thyroid cancer. Endocr Relat Cancer. 2017;24:R109–21.
Kini SR. Thyroid cytopathology: an Atlas and text. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 163–9.
Hirokawa M, Maekawa M, Kuma S, et al. Cribriform-morular variant of papillary thyroid carcinoma—cytological and immunocytochemical findings of 18 cases. Diagn Cytopathol. 2010;38:890–6.
Koo JS, Jung W, Hong SW. Cytologic characteristics and β-catenin immunocytochemistry on smear slide of cribriform-morular variant of papillary thyroid carcinoma. Acta Cytol. 2011;55:13–8.
Kuma S, Hirokawa M, Xu B, et al. Cribriform-morular variant of papillary thyroid carcinoma. Report of a case showing morules with peculiar nuclear clearing. Acta Cytol. 2004;48:431–6.
Hirokawa M, Kuma S, Miyauchi A, et al. Morules in cribriform-morular variant of papillary thyroid carcinoma: immunohistochemical characteristics and distinction from squamous metaplasia. APMIS. 2004;112:275–82.
Takada N, Hirokawa M, Ito A, et al. Cytoplasmic lipid accumulation characteristic of the cribriform variant of papillary thyroid carcinoma. Pathobiology. 2017;84:251–7.
Pusztaszeri MP, Auger M, Stelow EB, et al. Papillary thyroid carcinoma, variants, and related tumors. In: Ali S, Cibas E, editors. The Bethesda system for reporting thyroid cytopathology: definitions, criteria, and explanatory notes. 2nd ed. New York, NY: Springer; 2018. p. 149–50.
Jung CK, Choi YJ, Lee KY, et al. The cytological, clinical, and pathological features of the cribriform-morular variant of papillary thyroid carcinoma and mutation analysis of CTNNB1 and BRAF genes. Thyroid. 2009;19:905–13.
Boonyaarunnate T, Olson MT, Bishop JA, et al. Cribriform morular variant of papillary thyroid carcinoma: clinical and cytomorphological features on fine-needle aspiration. Acta Cytol. 2013;57:127–33.
Cameselle TJ, Chan JK. Cribriform-morular variant of papillary carcinoma: a distinctive variant representing the sporadic counterpart of familial adenomatous polyposis-associated thyroid carcinoma? Mod Pathol. 1999;12:400–11.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Suzuki, A., Hirokawa, M., Takada, N. (2019). Cribriform-Morular Variant of Papillary Thyroid Carcinoma. In: Kakudo, K. (eds) Thyroid FNA Cytology. Springer, Singapore. https://doi.org/10.1007/978-981-13-1897-9_28
Download citation
DOI: https://doi.org/10.1007/978-981-13-1897-9_28
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-1896-2
Online ISBN: 978-981-13-1897-9
eBook Packages: MedicineMedicine (R0)