Abstract
Cribriform morular variant of papillary thyroid carcinoma (CMV-PTC) is a rare variant. It is commonly associated with familial adenomatous polyposis. It is mostly seen in females below 30 years of age. We describe a male patient in his fourth decade of life, who presented with a solitary thyroid nodule and was evaluated and treated. The histopathology of the thyroid nodule was reported as CMV-PTC. In light of this finding, the patient was further investigated and treated for familial adenomatous polyposis (FAP), for which he was asymptomatic. Any patient diagnosed with CMV-PTC must also undergo colonoscopy to rule out FAP and receive appropriate treatment. Clinicians must be aware that this variant can be seen in men too.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Papillary thyroid carcinoma (PTC) is the most common type of thyroid carcinoma. There are many histological variants of PTC; the cribriform-morular variant (CMV) is one among them constituting 0.2% of PTC [1]. It is known that CMV-PTC may be associated with familial adenomatous polyposis (FAP). A majority (95%) of them belong to the non-syndromic type and in young female patients [1]. However, it is important to note that this rare disease entity may not only be difficult to diagnose but may also show deviation from the most anticipated presentation.
Case Presentation
A 39-year-old male was referred to our department for an anterior neck swelling of 3 months duration. He was evaluated with an ultrasonography of the neck, which showed a 3.7 × 2.7 cm hetero-echoic nodule in the right lobe of the thyroid and suspicious extrathyroidal extension. The thyroid function tests were normal. The fine needle aspiration cytology (FNAC) was suggestive of a papillary thyroid carcinoma (Bethesda category V). Contrast-enhanced computed tomography showed that the mass was encroaching the right tracheo-oesophageal groove with indeterminate central and lateral compartment nodes. In view of the above findings, the patient underwent total thyroidectomy with right central compartment clearance and a right selective neck dissection (SND II-IV), (in view of the indeterminate node reported on imaging in the right side of the neck as per our institutional policy). The histopathological report showed a complex papillary architecture, fusion of papillae and vague cribriform arrangement. Many morules of thyroid follicular cells were noted with extensive lymphovascular invasion. Immunohistochemical analysis showed nuclear positivity for beta-catenin and cytoplasmic strong positivity for CD10. In addition, there was strong nuclear positivity for CK7 and TTF1 (Fig. 1b, c).
a Colonoscopy pictures showing the entire colon studded with multiple polyps. b Histomorphological features of cribriform-morular variant of papillary thyroid carcinoma. Low-power (× 40) view to show the cribriform architecture. c High-power view (× 400) showing follicular architecture of arrangement, lack of classical nuclear features of PTC, and scattered non-squamous morules. Inset shows nuclear (pathognomonic) and cytoplasmic positivity for beta-catenin immunohistochemistry
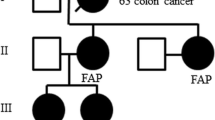
In view of its known association with FAP, a colonoscopy was advised. The patients had no GI-related symptoms but did give a history of carcinoma colon in a relative (details unknown). As anticipated, it showed multiple sessile polyps seen from the anal verge until the caecum (Fig. 1a). Biopsy from the ascending colon revealed high-grade dysplasia. Therefore, the patient underwent a total proctocolectomy + ileostomy. The patient also received 160 mCi of radioactive iodine therapy in view of extensive lymphovascular invasion subsequently. The patient’s family was counselled, and their family is currently under surveillance. The patient is alive and free of disease at 20 months following treatment completion.
Discussion
The earliest reported case of cribriform morular variant of papillary carcinoma of thyroid was by Crail in 1949 [1] and its association with FAP was made in the 1960s in a case report of two sisters with Gardener’s syndrome and thyroid carcinoma [2].
The cribriform-morular variant of papillary carcinoma is relatively rare with a reported incidence of 0.4–6.1% [1]. They are mostly seen at a younger age group (less than 30 years) with a female preponderance (31:1) [1]. The thyroid carcinoma is often multifocal and is associated with FAP. In patients with FAP, the estimated risk of thyroid carcinoma is considered to be 160 times higher than that of the general population [2]; about 30% of patients may manifest a thyroid carcinoma 4–12 years before the development of polyposis [3].
FAP is a hereditary autosomal dominant syndrome involving the APC gene (5q21) mutation [4]. The mutations may be sporadic (20–25%) or germline [4]. The cumulative risk of developing colorectal carcinoma in patients with FAP is considered to be 100% [2, 3]. It can be said that every patient with FAP should be screened for thyroid carcinoma and vice versa [3].
The diagnosis is mostly based on the histopathological findings [5]. Further confirmation to a diagnosis can be assisted by immunohistochemistry. The tumour cells are always positive for thyroid transcription factor-1 (TTF-1). One of the hallmark of this variant is its strong nuclear and cytoplasmic staining for β-catenin (Fig. 1c) [5]. On confirmation of the diagnosis, the management mostly entails only total thyroidectomy with central compartment clearance if necessary [2, 6, 7], due to the multifocal nature of the disease in a majority of the cases. Patients diagnosed with FAP-associated thyroid carcinoma must undergo a prophylactic proctocolectomy with or without ileostomy [6].
The overall prognosis is similar to that of classical PTC. The 5- and 20-year survivals of FAP-associated CMV have been reported to be at 90% and 77%, respectively, and the long-term prognosis is excellent if the patients undergo therapy for FAP [2]. Only 4 cases of male patients have been reported [1]. It is important to consider colonoscopy with the diagnosis of CMV-PTC and also screening of thyroid with FAP.
Conclusions
In this case report, we would like to highlight the importance of reporting the type/variant of papillary thyroid carcinoma in the histopathology report and to be aware of its possible associations with other systemic conditions and their appropriate management as reported in our case.
References
Lam AK, Saremi N (2017) Cribriform-morular variant of papillary thyroid carcinoma: a distinctive type of thyroid cancer. Endocr Relat Cancer 24(4):R109–R121
Tomoda C, Miyauchi A, Uruno T, Takamura Y, Ito Y, Miya A, Kobayashi K, Matsuzuka F, Kuma S, Kuma K, Kakudo K (2004) Cribriform-morular variant of papillary thyroid carcinoma: clue to early detection of familial adenomatous polyposis-associated colon cancer. World J Surg 28:886–839
Plail R, Bussey H, Glazer G, Thomson J (1987) Adenomatous polyposis: an association with carcinoma of the thyroid. Br J Surg 74(5):377–380
Kinzler K, Nilbert M, Su L, Vogelstein B, Bryan T, Levy D, Smith K, Preisinger A, Hedge P, McKechnie D et al (1991) Identification of FAP locus genes from chromosome 5q21. Science. 253(5020):661–665
Cameselle-Teijeiro JM, Peteiro-González D, Caneiro-Gómez J, Sánchez-Ares M, Abdulkader I, Eloy C, Melo M, Amendoeira I, Soares P, Sobrinho-Simões M (2018) Cribriform-morular variant of thyroid carcinoma: a neoplasm with distinctive phenotype associated with the activation of the WNT/β-catenin pathway. Mod Pathol 31(8):1168–1179
Ito Y, Miyauchi A, Ishikawa H, Hirokawa M, Kudo T, Tomoda C, Miya A (2011) Our experience of treatment of cribriform morular variant of papillary thyroid carcinoma; difference in clinicopathological features of FAP-associated and sporadic patients. Endocr J 58(8):685–689
Akaishi J, Kondo T, Sugino K, Ogimi Y, Masaki C, Hames KY, Yabuta T, Tomoda C, Suzuki A, Matsuzu K, Uruno T, Ohkuwa K, Kitagawa W, Nagahama M, Katoh R, Ito K (2018 Nov) Cribriform-morular variant of papillary thyroid carcinoma: clinical and pathological features of 30 cases. World J Surg 42(11):3616–3623
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chakraborthy, A., Mittal, N. & Thiagarajan, S. Cribriform-Morular Variant of Papillary Thyroid Carcinoma: a Clinical Surprise in a Routine Case. Indian J Surg 82, 1268–1270 (2020). https://doi.org/10.1007/s12262-020-02199-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-020-02199-7