Summary
Background AT-101 is a BH3 mimetic that inhibits the heterodimerization of Bcl-2, Bcl-xL, Bcl-W, and Mcl-1 with pro-apoptotic proteins, thereby lowering the threshold for apoptosis. This phase I trial investigated the MTD of AT-101 in combination with paclitaxel and carboplatin in patients with advanced solid tumors. Methods Patients were treated with AT-101 (40 mg) every 12 h on days 1, 2 and 3 of each cycle combined with varying dose levels (DL) of paclitaxel and carboplatin [DL1: paclitaxel (150 mg/m2) and carboplatin (AUC 5) on day 1 of each cycle; DL2: paclitaxel (175 mg/m2) and carboplatin (AUC 6) on day 1 of each cycle]. Secondary objectives included characterizing toxicity, efficacy, pharmacokinetics, and pharmacodynamics of the combination. Results Twenty-four patients were treated across two DLs with a planned expansion cohort. The most common tumor type was prostate (N = 11). Two patients experienced DLTs: grade 3 abdominal pain at DL1 and grade 3 ALT increase at DL2; however, the MTD was not determined. Moderate hematologic toxicity was observed. One CR was seen in a patient with esophageal cancer and 4 patients achieved PRs (1 NSCLC, 3 prostate). PD studies did not yield statistically significant decreases in Bcl-2 and caspase 3 protein levels, or increased apoptotic activity induced by AT-101. Conclusion The combination of AT-101 at 40 mg every 12 h on days 1, 2 and 3 combined with paclitaxel and carboplatin was safe and tolerable. Based on the modest clinical efficacy seen in this trial, this combination will not be further investigated. Clinical Trial Registration: NCT00891072, CTEP#: 8016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Defective regulation of apoptosis appears important to cancer pathogenesis and progression, and has been associated with resistance to standard therapy [1]. Many members of the Bcl-2 family of apoptosis-related genes are differentially expressed in various malignancies, and correlation between the overexpression of the protein products of some Bcl-2 genes and adverse prognosis has been reported in certain malignancies [2]. The Bcl-2 family of proteins includes proapoptotic members (e.g., Bax, Bak, Bad, Bid, Bim) as well as those that act to suppress apoptosis (e.g., Bcl-2, Bcl-xL, Bcl-W, Mcl-1) [3]. The ratios and interactions of these anti- and pro-apoptotic proteins determine the sensitivity or resistance of cells to various apoptotic stimuli. Alterations in the amounts of these proteins have been associated with a variety of pathologic conditions characterized by either too much or too little cell death [4]. Previous research efforts indicate that Bcl-2 (and Bcl-xL) bind to the BH3 domains of pro-apoptotic family members, sequestering them and thereby inhibiting their ability to promote cell death [5]. Peptide and non-peptide BH3 mimetics have been shown in laboratory studies to inhibit the heterodimerization of Bcl-2 or Bcl-xL to pro-apoptotic BH3 family members with the expected effects of increasing mitochondrial permeability and cytochrome-c release and activating effector caspases and apoptosis [6].
AT-101 [R-(−)-gossypol acetic acid)] is a BH3 mimetic that inhibits the heterodimerization of Bcl-2, Bcl-xL, Bcl-W, and Mcl-1 with pro-apoptotic members, Bax and Bak, at submicromolar affinity, and therefore, lowers the threshold for apoptosis [7,8,9]. Pre-clinical data has demonstrated the anti-tumor effects of AT-101; however, AT-101 has shown only modest clinical efficacy as a single agent with no objective responses were observed [10,11,12,13,14]. Evidence of AT-101 single-agent clinical activity was limited to declines of prostate-specific antigen [10] and stable disease [14]. However, unlike the BH3 mimetic navitoclax, in which Bcl-xL induced thrombocytopenia is often a dose limiting toxicity, there was little to no evidence of thrombocytopenia. While a clear explanation is not apparent for the difference between AT-101 and navitoclax in causing thrombocytopenia, it is notable that AT-101 demonstrated no consistent induction of caspase-dependent apoptosis in limited correlative analyses [14]. AT-101 toxicities primarily included nausea, vomiting, and anorexia were seen [10, 14,15,16].
The combination of carboplatin and paclitaxel has wide applicability to many solid tumor types, including lung [17], bladder [18], head/neck [19], breast [20], and ovarian cancers [21]. Paclitaxel treatment results in prolonged mitotic arrest, elevated levels of mitotic kinase activity, hyperphosphorylation of Bcl-2, and subsequent cell death in epithelial tumor cells by reducing heterodimer formation of Bcl-2 with Bax [22,23,24]. Paclitaxel also induces Bim accumulation antagonizing both Bcl-2 and Mcl-1 [25]. Cytotoxic chemotherapy is known to promote apoptosis through p53 and BH3-only proteins, which in turn bind to Bcl-2 [9]. The rationale for combining AT-101 with cytotoxic chemotherapy, such as carboplatin and paclitaxel, derives from the hypothesis that the combination may be more apoptogenic [26].
The primary aim of this phase I study was to determine to the maximum tolerated dose (MTD) of AT-101 in combination with paclitaxel and carboplatin in patients with advanced solid tumors.
Methods
Patients
Eligible patients were > 18 years of age with histologically or cytologically confirmed metastatic and/or unresectable malignancies, and for which standard curative or palliative measures no longer exist or are no longer effective. Other inclusion criteria included: an ECOG performance status ≤2, life expectancy of ≥3 months, and adequate organ function including: absolute neutrophil count of >1500/μL and platelets >100,000/μL without hematopoietic growth factor support (such as granulocyte colony stimulating factor, granulocyte macrophage colony stimulating factor, or interleukin-11), or platelet transfusions, creatinine within normal institutional limits (or a measured, 24 h, creatinine clearance greater than 60 mL/min), total bilirubin within normal limits, and aspartate transaminase and alanine transaminase ≤2.5 times the upper limit of normal). Patients were excluded if they received more than nine months of previous marrow damaging cytotoxic chemotherapy, or if they received prior racemic gossypol or AT-101 treatment. Patients with clinically and radiographically stable, previously treated, brain metastases, or those who clinically improved at least four weeks after completion of radiation therapy and were off steroids were considered eligible. This study was reviewed and approved by the Institutional Review Board of the Rutgers, The State University of New Jersey (Biomedical and Health Sciences)/ Rutgers Cancer Institute of New Jersey and all patients signed written informed consent.
Study design and treatment
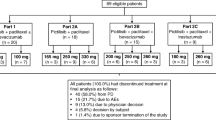
This was an open-label, dose-escalating, nonrandomized, single-center phase I study of AT-101 (R-(−)-gossypol acetic acid; NSC726190) combined with varying doses of paclitaxel and carboplatin administered on a 21-day cycle (NCT00891072). AT-101 was provided by the Cancer Therapy Evaluation Program (CTEP), National Cancer Institute (NCI), NIH under cooperative research and development agreement (CRADA). The recommended full dose of AT-101 (40 mg orally every 12 h on days 1, 2 and 3 of each cycle) was combined with either a lower dose of paclitaxel (150 mg/m2 on day 1 of each cycle) and carboplatin (AUC 5 on day 1 of each cycle) on dose level 1, or a higher dose of paclitaxel (175 mg/m2 on day 1 of each cycle) and carboplatin (AUC 6 on day 1 of each cycle) on dose level 2. AT-101 was dosed orally 1 h prior to IV paclitaxel, which was administered as an intravenous (IV) infusion over 3 h following standard intravenous H-1 and H-2 antagonists and oral dexamethasone. Carboplatin was administered following paclitaxel as an IV infusion over 30 min. AT-101 was omitted the morning of Cycle 1 Day1 or Cycle 2 Day 1 in the expansion cohort to assess apoptotic markers during paclitaxel and carboplatin chemotherapy with and without AT-101.
Study participants were enrolled in a standard 3 + 3 cohort design. If 1 of 3 patients in a dose group experienced a dose limiting toxicity (DLT) during the first cycle, 3 more patients were added to that dose group. The MTD was defined as the highest dose at which no more than 1 of 6 patients experienced a DLT in the first treatment course. Intrapatient dose escalations were not permitted. Patients who received less than 1 cycle of therapy were replaced in the cohort. Treatment was continued for a maximum of eight cycles, in the setting of no disease progression and treatment tolerability. Patients exhibiting response or benefiting from therapy, as determined by the treating physician were allowed to continue on single agent AT-101 therapy.
Primary and secondary endpoints
The primary endpoint was to determine the MTD of AT-101 combined with paclitaxel and carboplatin. Secondary endpoints included: describing the toxicities of the combination, evaluating the human pharmacokinetic disposition of AT-101 in the context of escalating doses, describing the pharmacokinetics of paclitaxel when given concurrently with AT-101, and evaluating evidence of clinical activity.
Clinical assessments
Medical history and demographic data were collected at screening (days −28 to 0). A physical examination and laboratory tests (including a complete blood count with differential, chemistry, and urinalysis) were performed at screening (days −14 to 0), on day 1 of every cycle, and at least 30 days after the last dose of study medication. An electrocardiogram and troponin I levels were obtained at baseline, 24 h following the completion of 3 days of dosing of AT-101, and at the completion of the study. Imaging of involved cancer sites was performed within 4 weeks of enrollment and after every 2 cycles. Responses were assessed using Response Evaluation Criteria in Solid Tumors Version 1.0 (RECIST 1.0) [27].
Adverse events were monitored and graded according to the National Cancer Institute Common Toxicity Criteria version 3.0 (before August 2010) or version 4.0 (after August 2010). A DLT was defined as ≥ grade 3 non-hematological toxicity excluding nausea, vomiting, or diarrhea; grade 3 nausea, vomiting, or diarrhea uncontrolled by maximal antiemetic/antidiarrheal therapy; grade 4 neutropenia of ≥7 days duration or with fever >38.5 °C, grade 3 neutropenia with > grade 3 infection; elevated serum troponin of any grade; grade 4 carboplatin/paclitaxel infusion related events; thrombocytopenia of any grade if associated with clinically significant bleeding, or grade 4 thrombocytopenia. For purposes of dose escalation and determination of MTD, only toxicities observed during cycle 1 were evaluated for DLTs.
Pharmacokinetic sampling and analysis
Data available in the literature delineating the bioavailability or metabolic fate of AT-101 remain limited [28, 29] and suggest that the drug may demonstrate variable bioavailability, or perhaps be subject to conjugative pathways [30, 31]. Overall, while the data do not support a high level of suspicion for a pharmacokinetic interaction between paclitaxel and AT-101, unsuspected effects (e.g. competition for plasma protein binding) warrant surveillance of paclitaxel disposition, given its toxicity profile. Thus, this study assessed the pharmacokinetics of AT-101 and any acute effect of paclitaxel administration on such (cycle 1 day 1) in addition to paclitaxel pharmacokinetics.
Blood samples were collected on Cycle 1 Day1 from patients enrolled on the dose escalation cohorts. Patients enrolled to the dose expansion cohort omitted the morning dose of AT-101 on Day 1 of either Cycle 1 or Cycle 2. Blood samples were collected on Day 1 of both cycles from expansion cohort patients in order to evaluate any acute effect of AT-101 on the pharmacokinetics of paclitaxel.
Since AT-101 was given one hour before starting the paclitaxel infusions, we used a combined sampling schedule to allow for determination of both paclitaxel and AT-101 pharmacokinetics. We thus obtained blood samples pre AT-101 treatment, and at 1 h, 2 h, 3 h, 4 h (end of paclitaxel infusion), 4.5 h, 5 h, 5.5 h, 6 h, 8 h, 10 h, and 24 h post AT-101 treatment. When AT-101 a.m. dose was omitted, the blood samples were obtained at pre- paclitaxel, 1 h, 2 h, 3 h (end of paclitaxel infusion), 3.5 h, 4 h, 4.5 h, 5 h, 6 h, 7 h, 9 h, and 24 h post the beginning of paclitaxel infusion.
Plasma concentrations of AT-101 were assessed using a validated high performance liquid chromatography HPLC assay [31]. Briefly, plasma samples were stabilized with reduced glutathione and maleic anhydride. Subsequent extraction procedures included addition of R-(−)-gossypol-diamino-propanol as an internal standard, precipitation with acetonitrile and centrifugation at 4 °C. Samples were injected into a HPLC system equipped with a Zorbax Eclipse XDB C18 column (4.6 × 150 mm, Agilent, Santa Clara, CA) at 30 °C using a isocratic elution with mobile phase (10 mM potassium monophosphate pH 3.0, and acetonitrile (20:80) at 30 °C. The method was applicable for measuring concentrations ranging from 28 ng/mL to 3.58 μg/mL using 300 μL of stabilized human plasma for extraction. Plasma concentrations of paclitaxel were determined by a validated HPLC method using a solid phase extraction. The method was applicable for measuring concentrations ranging from 0.039 to 10.0 μg/mL using 500 μL of human plasma sample for extraction.
The pharmacokinetic parameters, including the terminal half-life (t1/2), Cmax, Tmax, AUC0-10h, AUClast and apparent clearance (Cl/F) were estimated using a noncompartmental model with WinNonlin 2.1 software (Pharsight Corp, Palo Alto, CA). Descriptive statistics of pharmacokinetics parameters included are arithmetic means, standard deviation (SD), standard error (SE), and coefficient of variation (CV). Student t-test of mean pharmacokinetic parameters was used for the statistics evaluation (p < 0.05).
Pharmacodynamics
Peripheral blood mononuclear cells were isolated from blood at baseline and 1, 2, 4, and 8 h after paclitaxel infusion for both cycle 1 and cycle 2. All samples were stored at −80 °C, and analyzed for apoptosis using semi-quantitative immunoblot analysis of activated caspase 3 and PPAR-gamma cleavage. Comparisons were made in the change in apoptosis with and without the addition of AT-101 to carboplatin and paclitaxel.
Results
Patient characteristics
Twenty-four patients were enrolled and received one or more cycles of treatment. Patient demographics and baseline disease characteristics are shown in Table 1. The most common tumor type was prostate (N = 11; 46%). Twenty-two (92%) of the 24 patients had received prior chemotherapy, with 10 patients (42%) receiving two or more prior chemotherapy regimens. Of the 22 patients who received prior chemotherapy, 15 received prior taxane therapy and 9 received prior platinum therapy. The number of patients treated at each dose level and number of cycles administered are shown in Table 2. Six (25%) of the 24 patients remained on study for at least 8 cycles.
Patient enrollment and toxicities
Of the first 3 patients enrolled on dose level 1, one experienced grade 3 abdominal pain, which was considered a DLT. The patient presented with severe abdominal pain secondary to nausea, vomiting, and constipation following the first dose of AT-101. Due to the proximity to AT-101 dosing and the severity of the pain, the event was declared as possibly related to study drug. The patient continued on study following a dose reduction.
As a result of the DLT, 3 more patients were enrolled at dose level 1 and were cleared without any DLTs. Dose escalation continued to dose level 2 and 1 patient experienced a DLT (grade 3 ALT elevation). The patient presented to the hospital with grade 2 fatigue and fevers, grade 2 anorexia and grade 3 ALT elevation the day following his third dose of AT-101 during cycle 1. The patient recovered and continued on study with a dose reduction and the event was deemed as probably related to AT-101. Subsequently, three more patients were enrolled on dose level 2, and none experienced any DLTs. An expansion cohort (EC) of 12 patients was opened at dose level 2.
A summary of the non-hematologic toxicities attributed to treatment is provided in Table 3. The most common non-hematologic toxicities for all cycles attributed to treatment were: fatigue (N = 20; 83%), nausea (N = 13; 54%), metabolism and nutrition disorders (N = 13; 54%), and anorexia (N = 12; 50%). Most of the toxicities were grade 1 or 2. The most common non-hematologic toxicity at dose level 2 was grade 1/2 fatigue (N = 17; 71%) .
We observed moderate hematologic toxicity as outlined in Supplemental Table 1. Grade 3 or 4 anemia, thrombocytopenia, neutropenia, and leukopenia were reported in one patient (4%), one patient (4%), five patients (21%), and three patients (13%), respectively. Grade 1/2 thrombocytopenia was observed in 1 patient in DL1 and in 5 patients in DL2. Twelve (50%) patients received filgrastim or pegfilgrastim therapy, and 2 patients (8%) received erythropoietin therapy while also being treated with filgrastim or pegfilgrastim. There were no other serious hematologic adverse events. Two patients discontinued carboplatin on cycle 7 due to an adverse reaction. Dose reductions for both paclitaxel and carboplatin were administered in one patient on dose level 2 during cycle 5. Dose escalation cohorts proceeded through both dose levels without the determination of the MTD. AT-101 at the pre-specified dose level was tolerable at standard doses of chemotherapy.
Antitumor activity
Among the 24 treated patients, 1 patient with esophageal adenocarcinoma achieved a complete response (CR), and remained in a CR for 7 cycles. Prior therapy for this patient included paclitaxel175 mg/m2 and carboplatin, starting AUC of 6, and pazopanib. Four patients (17%), 1 with non-small cell lung cancer (NSCLC) and 3 with prostate cancer, achieved a partial response (PR)—three of the which were confirmed PRs. The 3 prostate patients with PRs received a median of 3 prior lines of therapy (range 2–4) and a median of 1 prior line of cytotoxic chemotherapy (range 1–2). All 3 PRs had prior treatment with docetaxel and no prior platinum therapy. The PR with NSCLC was chemotherapy naïve. Eight patients (33%) experienced stable disease (SD), including 1 small cell neuroendocrine bladder/prostate carcinoma patient, 1 breast cancer patient, and 6 patients with prostate cancer. Nine of the 11 patients with prostate cancer were evaluable for response: 3 experienced PR (EC9, 7 12) at dose level 2 and 6 experienced SD (Fig. 1a). The median duration of stable disease was 6 cycles (range 4–12 cycles). All prostate patients had received previous docetaxel therapy. The median duration of response was 10 cycles (range 9–10 cycles). Four out of 11 patients (36%) with prostate cancer exhibited more than a 50% reduction in PSA (Fig. 1b). Supplemental Table 2 includes details relating to each patient’s response on trial, including prior type and number of therapies, dose levels, duration of best response, and PSA levels for prostate patients.
Pharmacokinetics
The pharmacokinetic (PK) parameters of AT-101 are summarized in Table 4 and (Fig. 2a-f). The plasma concentration-time profiles of AT-101, obtained from 18 patients, are shown in Table 4. The concentration-time profiles showed large inter-patient variation, with Tmax and Cmax ranging from 2 h – 10 h and from 0.12–0.92 μg/mL, respectively, suggesting that the absorption rate of AT-101 varies between patients. In this study, the estimated PK parameters apparent clearance, t1/2, and AUC also showed large inter-patient variation (Fig. 2c-e). In 4 of 22 patients, plasma AT-101 levels either remained constant or kept rising for as long as 10 h (Fig. 2b), suggesting abnormal absorption and elimination of AT-101. The Cmax occurred at 10 h (Tmax) for Pt-11, while the AT-101 levels in plasma remained plateau from 5 h to 10 h in three other patients (Pt-EC-3, EC-7, EC-10), suggesting slow absorption from GI tract, and no significant elimination phase with a longer t1/2 (>15 h). Excluding those patients with abnormal absorption, we summerized the PK parameters of 18 patients’ data. The average Tmax and Cmax were 3.83 ± 1.14 h (range 2–6 h), and 0.60 ± 0.21 μg/mL (range 0.24–0.92 μg/mL), respectively. The average AUC0-10h (μg/mL*hr) was 3.20 ± 1.07 (range 1.42–5.12 μg/mL*hr). The mean apparent oral clearance (CL/F) was 11.08 ± 4.28 L/h (range 6.06–21.2 L/h). Since the bioavailability (F) of AT-101 remains unknown, the PK parameter clearance represents only apparent clearance. The plasma t1/2 of AT-101 was 3.27 ± 1.0 h (range 2.2–6.2 h). We observed that following the second dose, AT-101 levels increased over the first dose at 12 h levels in almost every patient. In this study, there were no significant changes in AT-101 PK parameters (AUC0-10h and apparent clearance), suggesting that the combination of AT-101 with paclitaxel and carboplatin demonstrates no significant drug interaction.
a Plasma concentration-time plot of AT-101 in patients (Mean ± SE). b Plasma concentration-time plot of patient Pt-11, Pt EC-3, Pt EC-7 and Pt EC-10 (abnormal absorption of AT-101). c-f AT-101 pharmacokinetics parameters in different chemotherapy regimens. g Plasma concentration-time plot of paclitaxel in patients with oral administration of AT-101 (Mean ± SD)
The estimated PK parameters of paclitaxel in combination with/without AT-101 in this study are presented in Table 5, and Fig. 2g). The average plasma concentration-time plots of paclitaxel are shown in Fig. 2g (with AT-101), and Fig. 2h (without AT-101). The PK parameters Cmax, AUCinf and CL were not significantly different between the groups with or without AT-101 in cycle 1 and cycle 2. The Cmax, AUCinf and CL values for paclitaxel were comparable in the odd number patients treated with A + P + C in cycle 1 and treated with P + C in cycle 2 in the extended cohort. Student t-test showed no significant difference in these treatment groups including paclitaxel pharmacokinetic parameters (t1/2, AUCinf, clearance) with and without AT-101.
Pharmacodynamics
In this study, pharmacodynamic studies we evaluated Bcl-2 protein level change in response to cytotoxic chemotherapy alone and in the combination of chemotherapy with AT-101, using PBMCs collected at different time points within the first 12 h after chemotherapy infusion. We also evaluated caspase 3 protein levels as a maker of apoptotic activities (data not shown). Although detection of Bcl-2 level alteration in PBMCs in response to modulating agents was shown as feasible in Phase II studies [32], we detected no statistically significant decrease of Bcl-2 protein level or increased apoptotic activities induced by AT-101.
Discussion
The purpose of this phase I study was to determine the MTD of the combination of AT-101 administered ag 40 mg orally every 12 h on days 1, 2 and 3 in combination with two dose levels paclitaxel and carboplatin on a 21-day cycle in patients with advanced solid tumors. Dose escalation occurred through both planned dose levels without sufficient DLTs to constitute the MTD, indicating that AT-101 given with either a higher or lower dose of paclitaxel and carboplatin was safe and relatively well tolerated.
The DLTs observed in this study were alanine aminotransferase (ALT) elevation and abdominal pain. No ALT elevations were observed in the monotherapy phase I/II study, in which AT-101 was given at 30 mg/day for 21 of 28 days; however significant gastrointestinal toxicities were observed, consistent with previous studies [10]. No small bowel obstructions were observed in this study with intermittent AT-101 dosing, which was often seen in studies involving continuous daily doing of AT-101 [10]. ALT elevations and gastrointestinal toxicities were observed in a phase II study of AT-101 in patients initiating androgen deprivation therapy (ADT) and in a phase I study of AT-101 in combination with cisplatin and etoposide [33, 34]. The most common non-hematologic adverse event was fatigue, and the most common hematologic adverse event was anemia. This side effect profile is comparable with what has been reported Phase I/II study with the same dose schedule of AT-101 plus docetaxel [35]. The lack of prominent thrombocytopenia observed in this study is unusual for Bcl-2 mimetics targeting Bcl-xL. Notably, navitoclax (ABT-263) a Bcl-2 mimetic, is typically associated with Bcl-xL induced thrombocytopenia as a single agent [15]. Moreover, thrombocytopenia resulting from navitoclax in combination with carboplatin and paclitaxel was observed in 36.8% of patients and was a dose limiting toxicity in 1/5 patients with DLTs [36]. The lack of the Bcl-xL induced thrombocytopenia as a result of AT-101 suggests that AT-101 may not be inhibiting these pro-apoptotic targets as selectively as other agents developed to modulate apoptosis.
In the pharmacokinetic studies, the estimated parameters t1/2, AUC, and clearance of AT-101 showed large interpatient variation, in 4 out of 22 patients’ plasma gossypol levels remaining constant or continually rising for as long as 10 h, indicating abnormal absorption and elimination of AT-101. This could possibly contribute to the discrepancies of the DLTs observed in this study versus the previous monotherapy study. AT-101 PK data could not be compared with previous studies carried out in limited number patients and the differences in dose and formulations. The pharmacokinetic parameters of paclitaxel were comparable to the previous report of a 3 h IV infusion as a single agent [37] and we conclude that the oral administration of AT-101 did not alter paclitaxel pharmacokinetics.
In the pharmacodymanic studies, we did not detect statistically significant decreases of Bcl-2 and Caspase 3 protein levels or increased apoptotic activities induced by AT-101 as demonstrated in VCaP prostate cancer cells in preclinical studies [38]. The lack of statistically meaningful change of Bcl-2 protein levels in PBMCs in our study may relate to the small sample size, time point selection, or insufficient effects, especially if AT-101 exhibits less selective modulation of BCL-2 family proteins targets.
In this study, designed to identify the MTD of the triplet, it is not possible to discern with certainty the contribution of AT-101 to treatment response in these patients. Evidence of efficacy was seen in 5 patients that achieved durable objective responses. One patient with esophageal cancer and prior carboplatin/paclitaxel therapy achieved a complete response and maintained a CR for 7 cycles (28 weeks), and 4 patients, all naïve to the carboplatin/paclitaxel treatment backbone achieved partial responses (1 NSCLC and 3 prostate). Twelve patients with varying tumor types experienced stable disease for a median of 6 cycles (range 4–12 cycles). Of the 11 prostate cancer patients, 3 (all chemotherapy naïve) experienced a partial response, and 6 experienced stable disease for a disease control rate of 82%. The median cycles of previous docetaxel in patients who experienced PR and SD was 3 (range 1–3) and 3.5 (range 1–6) cycles, respectively. Decline in PSA appeared consistent with previous studies [10]. While others have reported objective responses in patients with esophageal, prostate and NSCLC treated with AT-101 and chemotherapy [34, 35, 39]. randomized studies of docetaxel with or without AT-101 in patients with NSCLC as second line therapy, or as first line therapy for metastatic castrate-resistant prostate cancer, did not improve clinical outcomes [35, 39]. While disease control was achieved in docetaxel refractory prostate cancer patients, we are unable to conclude that that the treatment responses were AT-101 dependent. Taken together, the clinical benefit seen from this and other phase 1 studies [40, 41] is modest.
In conclusion, AT-101 in combination with carboplatin and paclitaxel appeared generally well tolerated in this patient population. Due to the limited clinical activity, in this and in other studies, further evaluation of this combination is not recommended.
References
Pistritto G, Trisciuoglio D, Ceci C, Garufi A, D'Orazi G (2016) Apoptosis as anticancer mechanism: function and dysfunction of its modulators and targeted therapeutic strategies. Aging. 8(4):603–619
Li L, Li Y, Que X, Gao X, Gao Q, Yu M, Ma K, Xi Y, Wang T (2018) Prognostic significances of overexpression MYC and/or BCL2 in R-CHOP-treated diffuse large B-cell lymphoma: a systematic review and meta-analysis. Sci Rep 8(1):6267
Chipuk JE, Moldoveanu T, Llambi F, Parsons MJ, Green DR (2010) The BCL-2 family Reunion. Mol Cell 37(3):299–310
Czabotar PE, Lessene G, Strasser A, Adams JM (2014) Control of apoptosis by the BCL-2 protein family: implications for physiology and therapy. Nat Rev Mol Cell Biol 15(1):49–63
Shamas-Din A, Kale J, Leber B, Andrews DW (2013) Mechanisms of action of Bcl-2 family proteins. Cold Spring Harb Perspect Biol 5(4):a008714–a00871a
S. Soderquist R, Eastman A (2016) BCL2 inhibitors as anticancer drugs: a plethora of misleading BH3 mimetics. Mol Cancer Ther 15(9):2011–2017
Vela L, Marzo I (2015) Bcl-2 family of proteins as drug targets for cancer chemotherapy: the long way of BH3 mimetics from bench to bedside. Curr Opin Pharmacol 23:74–81
Opydo-Chanek M, Gonzalo O, Marzo I (2017) Multifaceted anticancer activity of BH3 mimetics: current evidence and future prospects. Biochem Pharmacol 136:12–23
Adams JM, Cory S (2007) The Bcl-2 apoptotic switch in cancer development and therapy. Oncogene. 26(9):1324–1337
Liu G, Kelly WK, Wilding G, Leopold L, Brill K, Somer B (2009) An open-label, multicenter, phase I/II study of single-agent AT-101 in men with castrate-resistant prostate cancer. Clin Cancer Res 15(9):3172–3176
Meng Y, Tang W, Dai Y, Wu X, Liu M, Ji Q, Ji M, Pienta K, Lawrence T, Xu L (2008) Natural BH3 mimetic (−)-gossypol chemosensitizes human prostate cancer via Bcl-xL inhibition accompanied by increase of Puma and Noxa. Mol Cancer Ther 7(7):2192–2202
Balakrishnan K, Wierda WG, Keating MJ, Gandhi V (2008) Gossypol, a BH3 mimetic, induces apoptosis in chronic lymphocytic leukemia cells. Blood. 112(5):1971–1980
Kline MP, Rajkumar SV, Timm MM, Kimlinger TK, Haug JL, Lust JA, Greipp PR, Kumar S (2008) R-(−)-gossypol (AT-101) activates programmed cell death in multiple myeloma cells. Exp Hematol 36(5):568–576
Baggstrom MQ, Qi Y, Koczywas M, Argiris A, Johnson EA, Millward MJ, Murphy SC, Erlichman C, Rudin CM, Govindan R, Mayo Phase 2 Consortium, California Consortium (2011) A phase II study of AT-101 (gossypol) in chemotherapy-sensitive recurrent extensive-stage small cell lung cancer. J Thorac Oncol 6(10):1757–1760
Tse C, Shoemaker AR, Adickes J, Anderson MG, Chen J, Jin S, Johnson EF, Marsh KC, Mitten MJ, Nimmer P, Roberts L, Tahir SK, Xiao Y, Yang X, Zhang H, Fesik S, Rosenberg SH, Elmore SW (2008) ABT-263: a potent and orally bioavailable Bcl-2 family inhibitor. Cancer Res 68(9):3421–3428
Zhang H, Nimmer PM, Tahir SK, Chen J, Fryer RM, Hahn KR, Iciek LA, Morgan SJ, Nasarre MC, Nelson R, Preusser LC, Reinhart GA, Smith ML, Rosenberg SH, Elmore SW, Tse C (2007) Bcl-2 family proteins are essential for platelet survival. Cell Death Differ 14(5):943–951
Schiller JH, Harrington D, Belani CP, Langer C, Sandler A, Krook J, Zhu J, Johnson DH (2002) Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med 346(2):92–98
Vaughn DJ (2000) Paclitaxel and carboplatin in bladder cancer: recent developments. Eur J Cancer (Oxford, England : 1990) 36(Suppl 2):7–12
Vokes EE, Stenson K, Rosen FR, Kies MS, Rademaker AW, Witt ME, Brockstein BE, List MA, Fung BB, Portugal L, Mittal BB, Pelzer H, Weichselbaum RR, Haraf DJ (2003) Weekly carboplatin and paclitaxel followed by concomitant paclitaxel, fluorouracil, and hydroxyurea chemoradiotherapy: curative and organ-preserving therapy for advanced head and neck cancer. J Clin Oncol 21(2):320–326
Adamski V, Hempelmann A, Fluh C, Lucius R, Synowitz M, Hattermann K et al (2017) Dormant glioblastoma cells acquire stem cell characteristics and are differentially affected by Temozolomide and AT101 treatment. Oncotarget. 8(64):108064–108078
Kyrgiou M, Salanti G, Pavlidis N, Paraskevaidis E, Ioannidis JP (2006) Survival benefits with diverse chemotherapy regimens for ovarian cancer: meta-analysis of multiple treatments. J Natl Cancer Inst 98(22):1655–1663
Scatena CD, Stewart ZA, Mays D, Tang LJ, Keefer CJ, Leach SD, Pietenpol JA (1998) Mitotic phosphorylation of Bcl-2 during normal cell cycle progression and Taxol-induced growth arrest. J Biol Chem 273(46):30777–30784
Haldar S, Chintapalli J, Croce CM (1996) Taxol induces bcl-2 phosphorylation and death of prostate cancer cells. Cancer Res 56(6):1253–1255
Ito T, Deng X, Carr B, May WS (1997) Bcl-2 phosphorylation required for anti-apoptosis function. J Biol Chem 272(18):11671–11673
Tan TT, Degenhardt K, Nelson DA, Beaudoin B, Nieves-Neira W, Bouillet P, Villunger A, Adams JM, White E (2005) Key roles of BIM-driven apoptosis in epithelial tumors and rational chemotherapy. Cancer Cell 7(3):227–238
Macoska JA, Adsule S, Tantivejkul K, Wang S, Pienta KJ, Lee CT. 2008, -(-)Gossypol promotes the apoptosis of bladder cancer cells in vitro. Pharmacol Res 58(5–6):323–31
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, van Glabbeke M, van Oosterom A, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92(3):205–216
Othman MA, Abou-Donia MB (1988) Pharmacokinetic profile of (+/−)-gossypol in male Sprague-Dawley rats following single intravenous and oral and subchronic oral administration. Proc Soc Exp Biol Med 188(1):17–22
Jia L, Coward LC, Kerstner-Wood CD, Cork RL, Gorman GS, Noker PE et al (2008) Comparison of pharmacokinetic and metabolic profiling among gossypol, apogossypol and apogossypol hexaacetate. Cancer Chemother Pharmacol 61(1):63–73
Liu H, Sun H, Lu D, Zhang Y, Zhang X, Ma Z, Wu B (2014) Identification of glucuronidation and biliary excretion as the main mechanisms for gossypol clearance: in vivo and in vitro evidence. Xenobiotica. 44(8):696–707
Lin H, Gounder MK, Bertino JR, Kong AN, DiPaola RS, Stein MN (2012) A validated HPLC assay for the determination of R-(−)-gossypol in human plasma and its application in clinical pharmacokinetic studies. J Pharm Biomed Anal 66:371–375
DiPaola RS, Chen YH, Stein M, Vaughn D, Patrick-Miller L, Carducci M et al (2010) A randomized phase II trial of mitoxantrone, estramustine and vinorelbine or bcl-2 modulation with 13-cis retinoic acid, interferon and paclitaxel in patients with metastatic castrate-resistant prostate cancer: ECOG 3899. J Transl Med 8:20
Stein MN, Hussain M, Stadler WM, Liu G, Tereshchenko IV, Goodin S, Jeyamohan C, Kaufman HL, Mehnert J, DiPaola RS (2016) A phase II study of AT-101 to overcome Bcl-2--mediated resistance to androgen deprivation therapy in patients with newly diagnosed castration-sensitive metastatic prostate Cancer. Clin Genitourin Cancer 14(1):22–27
Schelman WR, Mohammed TA, Traynor AM, Kolesar JM, Marnocha RM, Eickhoff J, Keppen M, Alberti DB, Wilding G, Takebe N, Liu G (2014) A phase I study of AT-101 with cisplatin and etoposide in patients with advanced solid tumors with an expanded cohort in extensive-stage small cell lung cancer. Investig New Drugs 32(2):295–302
Ready N, Karaseva NA, Orlov SV, Luft AV, Popovych O, Holmlund JT, Wood BA, Leopold L (2011) Double-blind, placebo-controlled, randomized phase 2 study of the proapoptotic agent AT-101 plus docetaxel, in second-line non-small cell lung cancer. J Thora Oncol 6(4):781–785
Vlahovic G, Karantza V, Wang D, Cosgrove D, Rudersdorf N, Yang J, Xiong H, Busman T, Mabry M (2014) A phase I safety and pharmacokinetic study of ABT-263 in combination with carboplatin/paclitaxel in the treatment of patients with solid tumors. Investig New Drugs 32(5):976–984
Gianni L, Kearns CM, Giani A, Capri G, Vigano L, Lacatelli A et al (1995) Nonlinear pharmacokinetics and metabolism of paclitaxel and its pharmacokinetic/pharmacodynamic relationships in humans. J Clin Oncol 13(1):180–190
Loberg RD, McGregor N, Ying C, Sargent E, Pienta KJ (2007) In vivo evaluation of AT-101 (R-(−)-gossypol acetic acid) in androgen-independent growth of VCaP prostate cancer cells in combination with surgical castration. Neoplasia 9(12):1030–1037
Sonpavde G, Matveev V, Burke JM, Caton JR, Fleming MT, Hutson TE, Galsky MD, Berry WR, Karlov P, Holmlund JT, Wood BA, Brookes M, Leopold L (2012) Randomized phase II trial of docetaxel plus prednisone in combination with placebo or AT-101, an oral small molecule Bcl-2 family antagonist, as first-line therapy for metastatic castration-resistant prostate cancer. Ann Oncol 23(7):1803–1808
Heist RS, Fain J, Chinnasami B, Khan W, Molina JR, Sequist LV et al (2010) Phase I/II study of AT-101 with topotecan in relapsed and refractory small cell lung cancer. J Thorac Oncol 5(10):1637–1643
Swiecicki PL, Bellile E, Sacco AG, Pearson AT, Taylor JM, Jackson TL et al (2016) A phase II trial of the BCL-2 homolog domain 3 mimetic AT-101 in combination with docetaxel for recurrent, locally advanced, or metastatic head and neck cancer. Investig New Drugs 34(4):481–489
Funding
This trial was sponsored by the Cancer Therapy Evaluation Program of the National Cancer Institute (NCI/CTEP#8016) and was supported by the following grants: NCI CCSG 72720 and U01CA132194.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
NR reports advisory/consultation for ABBVIE, Celgene, BMS, Novartis, Merck, Astra zeneca, Genentech/Roche. RM is owns stock and is employed by Bristol-Myers Squibb. SG receives salary support from Janssen Pharmaceuticals. JMM reports consultancy for Amgen, Boehringer Ingelheim, and Array BioPharma travel, accommodations, or expenses from EMD Serono, Merck Sharp & Dohme, Array BioPharma, and Bristol-Myers Squibb; honoraria from Pfizer and EMD Serono; research funding from Merck, Sanofi, Novartis, Polynoma, Immunocore, Amgen, AstraZeneca, Incyte, Bristol Myers Squibb, and MacroGenics; and other relationships with Amgen, EMD Serono, Merck, Array BioPharma and Boehringer Ingelheim. AT declares no relevant disclosures for this manuscript. MNS reports consultancy for Merck Sharp & Dohme and Exelixis and research funding from Oncoceutics, Merck Sharp & Dohme, Janssen Oncology, Medivation/Astellas, Advaxis, Suzhou Kintor Pharmaceuticals, Harpoon, Bristol-Myers, Squibb, Genocea Biosciences, Lilly, Nektar, Seattle Genetics and Xencor. SG is employed by Janssen Pharmaceuticals. The remaining authors declare no conflicts of interest. None of the following disclosures influenced the results of this clinical trial.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from all participants included in this clinical study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 100 kb)
Rights and permissions
About this article
Cite this article
Stein, M.N., Goodin, S., Gounder, M. et al. A phase I study of AT-101, a BH3 mimetic, in combination with paclitaxel and carboplatin in solid tumors. Invest New Drugs 38, 855–865 (2020). https://doi.org/10.1007/s10637-019-00807-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10637-019-00807-2