Abstract
To analyze the invasiveness and image quality of coronary CT angiography (CCTA) with 80 kV. We enrolled 181 patients with low body weight and low calcium level. Of these, 154 patients were randomly assigned to 1 of 3 groups: 280 HU/80 kV (n = 51); 350 HU/80 kV (n = 51); or 350 HU/120 kV (n = 52). The amount of contrast media (CM) was decided with a CT number–controlling system. Twenty-seven patients were excluded because of an invalid time density curve by timing bolus. The predicted amount of CM, volume CT dose index, dose-length product, effective dose, image noise, and 5-point image quality were measured. The amounts of CM for the 80 kV/280 HU, 80 kV/350 HU, and 120 kV/350 HU groups were 10 ± 4 mL, 15 ± 7 mL, and 30 ± 6 mL, respectively. Although image noise was greater at 80 than 120 kV, there was no significant difference in image quality between 80 kV/350 HU and 120 kV/350 HU (p = 0.390). There was no significant difference in image quality between 80 kV/280 HU and 80 kV/350 HU (4.4 ± 0.7 vs. 4.7 ± 0.4, p = 0.056). The amount of CM and effective dose was lower for 80 kV CCTA than for 120 kV CCTA. CCTA at 80 kV/280 HU may decrease the amount of CM and radiation dose necessary while maintaining image quality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary CT angiography (CCTA) is a noninvasive alternative to conventional invasive coronary angiography for detecting coronary artery stenoses [1] and plaques [2]. One of the major concerns with CCTA is the amount of contrast media (CM) injected. Preventing contrast-induced nephropathy involves reducing the amount of CM [3]. Despite the improvement of multidetector CT (MDCT), the amount of CM required for CT imaging with 64 rows or more has not decreased. Even prospective electrocardiography (ECG)-gated wide-area detector single-heartbeat CCTA has involved the use of approximately 60 mL of CM [4].
Another concern with CCTA is the radiation dose. CCTA using high tube potential significantly reduces patient exposure. In smaller patients and children without extensive calcium deposits, reduction of the tube potential to 100 or 80 kV will lower radiation while maintaining adequate contrast-to-noise ratio [5, 6]. Thus, the Society of Cardiovascular Computed Tomography guideline [7] recommend 100 kV CCTA when the patient’s weight is less than 85 kg and the body mass index is less than 30 kg/m2. However, dose reduction of CM in 80-kV CCTA has not been fully elucidated.
The CT number of CM increases as tube potential decreases. The CT number of CM injected by the standard method was approximately 500 Hounsfield units (HU) when 100 kV was selected [8]. A recent report demonstrated an intracoronary CT number of more than 800 HU in 80-kV CCTA. [9] A superhigh CT number decreases the detectability of stenosis in smaller vessels. The optimal vascular CT number for detection of coronary artery stenosis on CCTA is approximately 350 HU [10]. In general, a high intraarterial opacification of more than 250 HU is recommended for optimal images [7]. Contrast volume may be reduced with CCTA using low tube potential.
We have developed a system for controlling intracoronary CT number in CCTA with small amounts of CM [11]. Using this technique, we evaluated the radiation dose and the image quality of CCTA performed according to a protocol calling for a low dose of CM and the following combinations of tube potentials and intracoronary CT numbers: 80 kV/280 HU, 80 kV/350 HU, and 120 kV/350 HU.
Methods
Study sample
We enrolled 181 subjects with low body weight (<65 kg), low body mass index (<26 kg/m2), and low coronary artery calcium (CAC ≤ 200 and calcified plaque size less than half the diameter of the vessel). Patients were referred because coronary artery disease was suspected (n = 126) or diagnosed (n = 55). CCTA was indicated according to the guideline of the Society of Cardiovascular Computed Tomography [7].
The CT number–controlling system can be applied when the time-density curve (TDC) is valid, or in other words, when the TDC is a unimodal curve in which the peak time and peak CT number are measurable [10]. Of the enrolled subjects, a randomized, open-label study was done for 154 who had a valid TDC by timing bolus. Patients were randomly assigned to CCTA targeting 280 HU with 80 kV, 350 HU using 80 kV, or 350 HU using 120 kV (Fig. 1). Twenty-seven patients with an invalid TDC underwent CCTA using 0.7–1 mL CM/kg body weight but were excluded from the analysis.
The minimum required CT number was 280 HU. Two hundred and fifty HU was recommended as the minimum for standard intracoronary CT [7]. We analyzed differences in patient parameters, radiation dose, and image quality between the 80 kV/280 HU group and the 80 kV/350 HU group to demonstrate the feasibility of a lower intracoronary CT number with a tube potential of 80 kV. These parameters were also compared between the 80 kV/350 HU and 120 kV/350 HU groups to demonstrate the feasibility of low tube potential with the same intracoronary CT number.
This study was approved by the local ethics committee, and all patients gave written, informed consent. Clinical exclusion criteria for CCTA were atrial fibrillation, allergy to CM, renal insufficiency (glomerular filtration rate <60 mL/min/1.73 mm2), pregnancy, congenital heart disease, low left ventricular function (ejection fraction <50 %), and coronary artery bypass graft.
Patients were administered an oral beta-blocker (25 mg Atenolol, AstraZeneca, Osaka, Japan) 120 min before CCTA and 0.3 mg of sublingual nitroglycerine 5 min before CCTA. Heart rate was maintained between 55 and 65 bpm by administering additional intravenous beta-blocker (2–10 mg Propranolol, AstraZeneca).
Scanning protocol
We used a 64-detector CT scanner with ECG gating (Lightspeed VCT, GE Healthcare, Milwaukee, USA) and Advantage Workstation 4.3 software. The scan sequence included scanogram, scout, timing bolus, and CCTA.
Coronary CT angiography was performed with prospective ECG triggered axial scan (Snapshot Pulse) with the following parameters: slice acquisition, 64 × 0.625 mm (40-mm volume coverage); 75 % of the RR interval with 0–50 ms of padding; rotation time, 350 ms; temporal resolution, 175 ms; tube potential, 120 kV; tube current, 450–680 mA; and total scan time 5 s.
Contrast media (350 mg I/mL; Omnipaque 350; Daiichi Sankyo Pharmaceutical Co, Ltd, Japan) was injected in a right antecubital vein using a dual-headed injector system (Dual Shot GX, Nemoto Kyorindo Co, Ltd, Tokyo, Japan) during the timing bolus and CCTA. Five milliliters of CM with 40 mL of saline chaser (injection rate 4 mL/s) was used as a timing bolus for determining the circulation time of the enhanced scan. Sequential scans were obtained every 2 s, from 10 to 40 s after the timing bolus. The region of interest was located in the ascending aorta, and a TDC was determined. The peak time was identified, and the absolute value of the CT number of the ascending aorta at the peak time was measured at the region of interest. Scan delay was defined as 2 s after peak enhancement. The amount of CM was decided with the CT number–controlling system, using body surface area, peak time, and peak CT number of the timing bolus (10). Saline chaser was 40 mL and injection rate was 4 mL/s. Because the CT number of CM increases 1.5-fold when using 80 kV rather than 120 kV (data not shown), we used the amount of CM needed to target 167 HU or 233 HU with 120 kV when we performed CCTA in the 80 kV/280 HU and 80 kV/350 HU groups.
Calculation of radiation dose estimates
Radiation dose was calculated from the volume CT dose index (CTDIvol) and the dose-length product (DLP) [12]. The CTDI value is calculated as a mathematic integral under the radiation dose profile of a single rotation scan that would produce 1 tomographic image at a fixed table position [13]. CTDIvol is the average radiation dose over a specific investigated volume. The DLP was calculated by multiplying CTDIvol by the respective scan length [14]. The DLP is an estimation of the radiation exposure for the entire CT examination. The CTDIvol and DLP were recorded as direct data output from prospective ECG-triggered axial scan. The CT scanner provided a protocol summary containing the DLP for each image series. The effective radiation dose was then estimated by multiplying the dose-length product (mGy × cm) by the conversion coefficient of the chest (k = 0.014 mSv/mGy × cm) [15].
Assessment of image quality
Image quality was measured according to image noise. The image noise was defined as the standard deviation of the region-of-interest measurement at the aorta. The region of interest was on the ascending aorta at the level of the proximal portion of the left main trunk and right coronary artery.
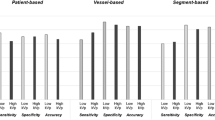
Axial and multiplanar reformatted images were used for analysis. The patient-based image quality of the coronary vessels was subjectively assessed by 2 well-trained, independent, blinded cardiologists who had read the CCTA results of at least 300 patients. The evaluation was patient based after screening the image quality of the 16-segment model of vessel disease proposed by the American Heart Association [16]. All patients were analyzed in a randomized manner, and all segments were evaluated using a 5-point scale: 5, excellent and easily assessable, no artifact in any coronary segment; 4, good, mild artifacts at 1 segment and assessable; 3, evaluable, moderate artifacts on a few segments; 2, evaluable, diagnostic combined with axial images; and 1, not assessable, because of severe artifacts. Reviewers closely reevaluated discordant image quality scores, and if the discordance persisted after a second evaluation, they further evaluated the images individually until they reached a consensus.
Statistical analysis
Statistical analysis was performed using SPSS 17.0 (SPSS Inc, Chicago, IL). Data are expressed as means with standard deviations. Differences in patients parameters, radiation dose, and image quality between the 80 kV/280 HU and 80 kV/350 HU groups were analyzed with t test. These parameters were also compared between the 80 kV/350 HU and 120 kV/350 HU groups. Interobserver agreement was calculated by the κ test. A p value of 0.05 was considered statistically significant.
Results
Patient characteristics and parameters
Patient characteristics are summarized in Table 1. All patients successfully underwent CCTA with prospective ECG-triggered axial scan, probably because we excluded patients with low ventricular function, which causes a relatively high heart rate, and patients with high coronary calcium, which causes artifacts. Mean body mass index of 80 kV/280 HU, 80 kV/350 HU and 120 kV/350 HU groups were 20.0 ± 3.5 kg/m2 (16.9–25.9 kg/m2), 21.0 ± 3.5 kg/m2 (15.4–25.9 kg/m2), and 20.4 ± 3.2 kg/m2 (14.5–25.9 kg/m2), respectively. Mean serum creatinine in all patients was 0.84 ± 0.26 mg/dL. No patients showed 25 % increase in or an absolute elevation in serum creatinine (SCr) of 0.5 mg/dL, 48–72 h after parenteral contrast exposure. The mean age of the 80 k/350 HU group was less than that of the 120 kV/350 HU group. There were no significant differences between the 80 kV/280 HU and 80 kV/350 HU groups in the distribution of sex, height, body weight, heart rate, test peak time, or peak CT number. There were no significant differences between the 80 kV/350 HU and 120 kV/350 HU groups in the distribution of sex, height, body weight, heart rate, test peak time, or peak CT number. A representative 80 kV/350 HU case is shown in Fig. 2.
Representative coronary computed tomography angiography (80 kV/280 HU) with 8 mL of contrast media. Age, 65 years; sex, female; height, 145 cm, weight, 41 kg; body mass index, 19.5 kg/m2; effective dose, 0.48 mSv, intracoronary CT number, 328 ± 18 HU, image quality, 5. a Volume rendering images. Curved multiplanar reconstruction images of the left anterior descending artery (b), left circumflex artery (c), and right coronary artery (d)
Contrast volume and image quality
Table 2 compares CM amount and image quality between the 3 groups. The volume of CM used in the 80 kV/280 HU, 80 kV/350 HU, and 120 kV/350 HU groups was 10 ± 4 mL, 15 ± 7 mL, and 30 ± 6 mL, respectively. Significantly less CM was used for 80 kV/280 HU compared to 80 kV/350 HU (p < 0.001). Significantly less CM was used for 80 kV/350 HU compared to 120 kV/350 HU (p < 0.001). The representative case of 80 kV/280 HU using 8 mL of CM was shown in Fig. 2. The intracoronary CT number was 328 ± 18 HU, and the image quality of the patient was 5. Intracoronary CT numbers for 80 kV/280 HU, 80 kV/350 HU, and 120 kV/350 HU were 278 ± 24 HU, 348 ± 23 HU, and 359 ± 33 HU, respectively.
Although image noise was higher for 80 kV/350 HU than for 120 kV/350 HU, there was no significant difference in image quality (4.7 ± 0.4 vs. 4.6 ± 0.6, p = 0.390). Neither was there a significant difference in image quality between 80 kV/280 HU and 80 kV/350 HU (4.4 ± 0.7 vs. 4.7 ± 0.4, p = 0.056). Interobserver agreement on image quality was excellent (κ = 0.85).
Discussion
We found that, in patients with low body weight and low CAC, CCTA with 80 kV had the same image quality as CCTA with 120 kV and required a lower radiation dose, and 80 kV/280 HU CCTA had the same image quality as 80 kV/350 HU CCTA. Many studies have used a reduced radiation dose [19]; few have tried to reduce both contrast volume and radiation dose. We found that the volume of contrast required for 80 kV/280 HU CCTA was only one-third of that required for 120 kV/350 HU CCTA (Table 2). CCTA with both a low dose of contrast and reduced radiation exposure may have extended applications, such as screening for early stage atherosclerosis [20], imaging in patients with high-risk chronic kidney disease and diabetic nephropathy.
The amount of CM has generally been decided based on body weight, body mass index, or body surface area [17, 18]. Controlling the amount of CM has been difficult with this approach. It is reported that CCTA with low tube potential reduces radiation dose; however, it also drastically increases the intracoronary CT number [9], perhaps hindering diagnostic accuracy [10]. Therefore, the volume of contrast should be reduced for 80-kV CCTA. We have developed a CT number–controlling system for CCTA [11]. This system can be applied for approximately 85 % of patients with a valid TDC after a timing bolus with 5 mL of CM [11]. In addition, the system may be applicable with different tube potentials if the CT number is corrected. The average intracoronary CT numbers for 80 kV/280 HU, 80 kV/350 HU, and 120 kV/350 HU were 278 ± 24 HU, 348 ± 23 HU, and 358 ± 33 HU, respectively.
The value of two hundred and fifty Hounsfield units does not seem to be the absolute standard intracoronary CT number. Our data of lowest amount contrast media is CCTA using 4 mL of CM with 40 mL of saline chaser (Fig. 3), though the patient was not included in the study. Peak intracoronary CT number depends on body mass index and the circulation of CM in the patient [11]. The intracoronary CT number was 200 ± 21 HU. The images clearly excluded significant stenosis in all coronary arteries.
Coronary CT angiography using 80 kV and 4 mL of contrast media. Age, 73 years; sex, female; height, 148 cm; weight, 43 kg; body mass index, 19.6 kg/m2; effective dose, 0.72 mSv; intracoronary CT number, 200 ± 21 HU; image quality, 5. A Volume rendering images (a) Curved multiplanar reconstruction images of the left anterior descending artery (b), left circumflex artery (c), and right coronary artery (d)
The main artifact is blurring in the right coronary artery. It is especially difficult to obtain still images of the right coronary artery with calcification disposition, even if heart rate is fully controlled at 55–65 bpm. Because patients with heavy calcification were excluded from this study, all participants were eligible for prospective ECG-triggered helical scan.
A generally acceptable level of image noise has not yet been defined; however, image noise may be improved by using adaptive statistical iterative reconstruction [21].
Limitations
The feasibility of 80-kV CCTA should be assessed based on coronary calcium deposition after scanogram. The CT number–controlling system might be applied to other machines with shorter scan times than 64-row CT, but it has not yet been validated for other CT apparatuses. The CT number–controlling system has been verified only with 350 mg I/mL of CM.
Abbreviations
- CCTA:
-
Coronary computed tomography angiography
- CM:
-
Contrast media
- HU:
-
Hounsfield units
- TDC:
-
Time-density curve
- CTDIvol:
-
Volume CT dose index
- DLP:
-
Dose-length product
- ED:
-
Effective radiation dose
References
Achenbach S, Ropers U, Kuettner A, Anders K, Pflederer T, Komatsu S, Bautz W, Daniel WG, Ropers D (2008) Randomized comparison of 64-slice single- and dual-source computed tomography coronary angiography for the detection of coronary artery disease. JACC Cardiovasc Imaging 1(2):177–186
Komatsu S, Imai A, Kodama K (2011) MDCT may accurately estimate plaque vulnerability. Circ J 75(6):1515–1521
Vercellino M, Bezante GP, Balbi M (2009) Contrast medium induced nephropathy: new insights into prevention and risk management. Cardiovasc Hematol Agents Med Chem 7(2):166–180
Kumamaru KK, Steigner ML, Soga S, Signorelli J, Bedayat A, Adams K, Mitsouras D, Rybicki FJ (2011) Coronary enhancement for prospective ECG-gated single R–R axial 320-MDCT angiography: comparison of 60- and 80-mL iopamidol 370 injection. AJR Am J Roentgenol 197(4):844–850
Hausleiter J, Meyer T, Hadamitzky M, Huber E, Zankl M, Martinoff S, Kastrati A, Schomig A (2006) Radiation dose estimates from cardiac multislice computed tomography in daily practice: impact of different scanning protocols on effective dose estimates. Circulation 113(10):1305–1310
Siegel MJ, Schmidt B, Bradley D, Suess C, Hildebolt C (2004) Radiation dose and image quality in pediatric CT: effect of technical factors and phantom size and shape. Radiology 233(2):515–522
Abbara S, Arbab-Zadeh A, Callister TQ, Desai MY, Mamuya W, Thomson L, Weigold WG (2009) SCCT guidelines for performance of coronary computed tomographic angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 3(3):190–204
Durmus T, Rogalla P, Lembcke A, Mühler MR, Hamm B, Hein PA (2011) Low-dose triple-rule-out using 320-row-detector volume MDCT–less contrast medium and lower radiation exposure. Eur Radiol 21(7):1416–1423
Wang D, Hu XH, Zhang SZ, Wu RZ, Xie SS, Chen B, Zhang QW (2012) Image quality and dose performance of 80 kV low dose scan protocol in high-pitch spiral coronary CT angiography: feasibility study. Int J Cardiovasc Imaging 28(2):415–423
Fei X, Du X, Yang Q, Shen Y, Li P, Liao J, Li K (2008) 64-MDCT coronary angiography: phantom study of effects of vascular attenuation on detection of coronary stenosis. AJR Am J Roentgenol 191(1):43–49
Komatsu S, Kamata T, Imai A, Ohara T, Takewa M, Miyaji K, Yoshida J, Kodama K (2013) Controlling intracoronary CT number for coronary CT angiography. J Cardiol 61(2):155–161
Morin RL, Gerber TC, McCollough CH (2003) Radiation dose in computed tomography of the heart. Circulation 107(6):917–922
McCollough CH (2008) CT dose: how to measure, how to reduce. Health Phys 95(5):508–517
Jung B, Mahnken AH, Stargardt A, Simon J, Flohr TG, Schaller S, Koos R, Günther RW, Wildberger JE (2003) Individually weight-adapted examination protocol in retrospectively ECG-gated MSCT of the heart. Eur Radiol 12(13):2560–2566
(2007) The 2007 recommendations of the international commission on radiological protection: ICRP publication 103. Ann ICRP 37(2–4):1–332
Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB (1975) A reporting system on patients evaluated for coronary artery disease: report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery. American Heart Association. Circulation. 51(4 Suppl):5–40
Herzog BA, Husmann L, Valenta I, Tay FM, Burkhard N, Gaemperli O, Wyss CA, Landmesser U, Kaufmann PA (2009) Determinants of vessel contrast in BMI-adapted low dose CT coronary angiography with prospective ECG-triggering. Int J Cardiovasc Imaging 25(6):625–630
Pazhenkottil AP, Husmann L, Buechel RR, Herzog BA, Nkoulou R, Burger IA, Vetterli A, Valenta I, Ghadri JR, von Schulthess P, Kaufmann PA (2010) Validation of a new contrast material protocol adapted to body surface area for optimized low-dose CT coronary angiography with prospective ECG-triggering. Int J Cardiovasc Imaging 26(5):591–597
Buechel RR, Husmann L, Herzog BA, Pazhenkottil AP, Nkoulou R, Ghadri JR, Treyer V, von Schulthess P, Kaufmann PA (2011) Low-dose computed tomography coronary angiography with prospective electrocardiogram triggering: feasibility in a large population. J Am Coll Cardiol 57(3):332–336
Imai A, Komatsu S, Ohara T, Kamata T, Yoshida J, Miyaji K, Shimizu Y, Takewa M, Hirayama A, Deshpande GA, Takahashi O, Kodama K (2011) Serum cystatin C is associated with early stage coronary atherosclerotic plaque morphology on multidetector computed tomography. Atherosclerosis. 218(2):350–355
Leipsic J, Labounty TM, Heilbron B, Min JK, Mancini GB, Lin FY, Taylor C, Dunning A, Earls JP (2010) Estimated radiation dose reduction using adaptive statistical iterative reconstruction in coronary CT angiography: the ERASIR study. AJR Am J Roentgenol 195(3):655–660
Conflict of interest
Dr Komatsu is a technical consultant for Nemoto Kyorin-do Co., LTD.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Komatsu, S., Kamata, T., Imai, A. et al. Coronary computed tomography angiography using ultra-low-dose contrast media: radiation dose and image quality. Int J Cardiovasc Imaging 29, 1335–1340 (2013). https://doi.org/10.1007/s10554-013-0201-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-013-0201-2