Abstract
We evaluated the determinants of vessel contrast in prospectively ECG-triggered CT coronary angiography (CTCA). Seventy patients underwent low-dose CTCA using Body Mass Index (BMI)-adapted tube parameters and a fixed contrast material bolus. Contrast to noise ratio (CNR) was calculated from contrast (between coronaries and perivascular tissue) and image noise (standard deviation of aortic attenuation). Cardiac output (CO) was calculated from gated 99mTc-tetrofosmin-SPECT. Mean radiation dose was 2.13 ± 0.69 mSv. Image noise was not affected by BMI (r = 0.1, P = 0.36), while CNR was inversely related to body surface area (BSA) (r = −0.5, P < 0.001) and CO (r = −0.45, P < 0.001). After successfully overcoming the impact of BMI on image noise by adapting tube parameters, CNR mainly depends on coronary vessel contrast. The latter reflects the dilution of the contrast material by blood volume and CO, which are both correlated to BSA. Therefore, BSA adapted contrast administration may help to compensate for this effect.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since the implementation of computed tomography coronary angiography (CTCA) with 64 slices, CTCA is an accurate method for non-invasive detection of coronary artery disease [1–4].
However, radiation exposure to patients and non-diagnostic image quality still remain issues of concern. Radiation exposure to patients can be reduced tremendously with prospective ECG-triggering as a new scanning protocol [5]. The use of this CTCA protocol allows to reduce radiation dose from about 15 mSv in spiral scanning with ECG-modulated tube current down to about 2 mSv [5] by administering radiation dose only at one predefined end-diastolic time point instead of during a whole phase of the cardiac cycle [6].
Image quality is primarily affected by coronary calcification [1, 4, 7], motion artifacts [1–3, 8], body related factors (i.e., body mass index (BMI), body surface area (BSA)) [9–11] or by contrast bolus dilution depending on cardiac output (CO) [12–14]. Coronary calcifications are known to influence image quality by their blooming and beam-hardening artifacts [1, 4, 7]. Motion artifacts could be reduced by technical advances in new scanner generations such as subsecond rotation time and 64 [1–3] or more slices [15, 16], but image quality is still affected by individual body- and hemodynamic-related parameters. According to previous studies, an increase in BMI induces higher image noise [9–11] while an increase in CO is associated with a decrease in coronary artery contrast [13]. The latter is most probably caused by more contrast dilution in coronary arteries.
In the present study we have adapted tube voltage and current to patients’ BMI in order to minimize the interference of BMI with image noise and, thus, contrast to noise ratio (CNR). With this we aimed at assessing the impact of CO as an index of contrast bolus dilution on coronary artery attenuation and CNR.
Methods
Patients
Seventy consecutive patients (Table 1) underwent low dose CTCA using prospective ECG-triggering and gated 99mTc-tetrofosmin myocardial perfusion imaging (MPI). Exclusion criteria were hypersensitivity to iodinated contrast agent, renal insufficiency (creatinine level >150 μmol/l or >1.7 mg/dl), non-sinus rhythm, or hemodynamic instability.
Patients were referred because of suspected CAD (n = 64) based on at least one of the following symptoms such as dyspnoe (n = 11), typical angina pectoris (n = 10), atypical chest pain (n = 42), pathological exercise test or ECG (n = 20) or high cardiovascular risk factors (n = 2). Six patients with known CAD were referred for stent-control (n = 2) or follow-up after myocardial infarction (n = 4).
CT coronary angiography
All patients received a single dose of 2.5 mg isosorbiddinitrate sublingual (Isoket, Schwarz Pharma, Monheim, Germany) 2 min prior to the scan. In addition, intravenous metoprolol (2–20 mg) (Beloc, AstraZeneca, London, UK) was administered, if necessary to achieve a target heart rate under 65 bpm prior to the start of the scan. Heart rate was monitored. A fixed contrast material protocol was used in all patients, administering a bolus of 80 ml of iodixanol (Visipaque 320, 320 mg/ml, GE Healthcare) followed by 50 ml saline solution, which was continuously injected into an antecubital vein via an 18-gauge catheter at a flow rate of 5 ml/s. Bolus tracking was performed with a region of interest (ROI) placed into the ascending aorta. All CTCA examinations were performed on a LightSpeed VCT XT scanner (GE Healthcare) with prospective ECG-triggering [6], using a commercially available protocol (SnapShot Pulse, GE Healthcare) and the following scanning parameters: slice acquisition 64 × 0.625 mm, smallest X-ray window (only 75% of the RR-cycle), z-coverage value of 40 mm with an increment of 35 mm and gantry rotation time 350 ms. Tube voltage and effective tube-current were adapted to BMI (100 kV: BMI < 25 kg/m2, 120 kV: BMI ≥ 25 kg/m2; 450 mA: BMI < 22.5 kg/m2, 500 mA: BMI 22.5–25 kg/m2, 550 mA: BMI 25–27.5 kg/m2, 600 mA: BMI 27.5–30 kg/m2, 650 mA: BMI > 30 kg/m2). The effective radiation dose of CTCA was calculated as the product of the dose-length product (DLP) times a conversion coefficient for the chest (k = 0.017 mSv/mGycm) [17]. Axial images for attenuation calculations were reconstructed with a slice thickness of 0.6 mm, using a standard medium soft-tissue convolution kernel. All images were transferred to an external workstation (AW 4.4, GE Healthcare).
We performed the calculations of the CNR in the left main artery (LMA) as previously reported [13, 18]. Briefly, we first determined image noise by placing a ROI (2 × 2 cm) and measured the standard deviation of the attenuation value (in Hounsfield units, HU) in the ascending aorta. Second, ROIs were drawn as large as possible to measure attenuation in the proximal LMA and in the perivascular tissue, carefully avoiding calcifications, plaques, and stenoses. Vessel contrast was calculated as the difference in mean attenuation between the contrast enhanced vessel lumen and the adjacent perivascular tissue. Finally we calculated CNR as the ratio of vessel contrast over noise.
Myocardial perfusion imaging
MPI data acquisition was performed on a dual-head detector camera with the Hawkeye facility (Ventri, GE Healthcare), using a 1-day stress (0.14 mg/kg/min adenosine i.v.)/rest protocol with a dose of approximately 300 and 900 MBq of 99mTc tetrofosmin, respectively. Emission data were acquired with a parallel-hole, low-energy, high resolution collimator with a 20% symmetric window centered at 140 keV. Further acquisition parameters were 3° rotation per stop, 180° each head, and 25 s per projection. Acquisitions were gated for 16 frames per R–R cycle with an acceptance window of 50%. A low-dose, unenhanced CT for attenuation correction was acquired on a Light speed VCT XT scanner (GE Healthcare) and also used for coronary calcium socring, as previously reported in detail [19].
Statistical analysis
Quantitative variables were expressed as mean ± SD and categorical variables as frequencies, or percentages. SPSS software (SPSS 15.0, Chicago, IL, USA) was used for statistical testing. The BSA was calculated with the common standard, i.e. Mosteller formula. Pearson correlation analyses were performed to compare image noise of the ascending aorta with BMI. Similarly attenuation and CNR in the LMA was compared with cardiac output and BSA. The 95% confidence intervals (CI) were plotted for the regression lines and were calculated for the slopes of regression line. A P value of <0.05 was considered to indicate a statistical significance. The study protocol was approved by the institutional review board and written informed consent was obtained.
Results
CTCA and MPI were successfully performed in all 70 patients on the same day. Intravenous betablocker was administered for heart rate control prior to CTCA in 46 patients (10.27 ± 5.58 mg, range 2.50–20.00 mg). The mean DLP from CTCA was 125.46 ± 40.68 mGycm (range: 58.39–189.36 mGycm) resulting in an estimated mean applied radiation dose of 2.13 ± 0.69 mSv (range: 0.99–3.22 mSv). This does not include the radiation dose of 64.91 ± 7.76 DLP (0.90 ± 0.45 mSv) from the unenhanced CT.
Image noise
Image noise (i.e. standard deviation of the attenuation in the ascending aorta) (mean: 33.42 ± 6.56, range: 20.8–46.60) was not correlated to BMI over a wide range (mean: 26.35 ± 4.41 kg/m2, range: 17.51–38.75 kg/m2).
Coronary attenuation
In the LMA the mean attenuation was 400.46 ± 120.98 HU (range: 139.70–676.50 HU) and the mean attenuation of the perivascular tissue adjacent to the LMA was -60.40 ± 19.73 HU (range: −98.60–(−13.70) HU). The mean CNR in the LMA was 14.12 ± 4.08 (range: 6.53–29.78).
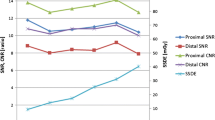
The BMI was inversely correlated to attenuation (r = −0.41, P < 0.001, standard error of estimate (SEE) = 73.31) and CNR (r = −0.42, P < 0.001, SEE = 71.36). Similarly the BSA (mean: 1.91 ± 0.22 m2, range: 1.49–2.37 m2) was inversely correlated to attenuation (r = −0.56, P < 0.001, SEE = 70.16) and CNR (r = −0.50, P < 0.001, SEE = 68.11) (Fig. 1).
The mean stroke volume was 56.23 ± 11.24 ml (range: 35.00–87.00 ml) and the mean heart rate during CT scanning 57.92 ± 7.22 bpm (range: 39.85–80.13 bpm). The calculated CO ranged from 1.84 to 4.45 ml/min and was inversely correlated to attenuation (LMA r = −0.50, P < 0.001, SEE = 74.61) and CNR (r = −0.45, P < 0.001, SEE = 72.71) (Fig. 2). Moreover, CO was correlated to BSA (r = 0.58, P < 0.001, SEE = 34.94). Figure 3 shows the impact of contrast bolus dilution in patients with different BSA and CO. There was no correlation between CNR and calcium score (P = non significant).
Axial slices of CT coronary angiography in two patients with different body mass index (BMI), but similar image noise. The vessel attenuation is lower in the more obese patient (a) than in the slim patient (b). a Patient with BMI 32.3 kg/m2. Contrast enhanced image (left panel) obtained at 120 kV/600 mA (image noise: 31.3, vessel attenuation: 139.7 HU, CNR: 7.3, CO: 3.2 ml/min). Right image: native CT. b Patient with BMI 24.8 kg/m2. Contrast enhanced image (left panel) obtained at 100 kV/500 mA (image noise: 29.7, vessel attenuation: 421.6 HU, CNR: 15.1, CO: 1.58 ml/min). Right image: native CT
Discussion
CTCA image quality is impaired in patients with high BMI due to increased image noise and decreased coronary attenuation [9–11, 13]. In the present study we have minimized the impact of BMI on image noise, supporting that the adjustment of tube voltage and current was appropriate. As a consequence CNR mainly depended on coronary vessel attenuation. Despite BMI-adaption of the parameters above for noise reduction, vessel attenuation remained inversely correlated to BMI. The latter reflects that BMI is generally linked with blood volume and cardiac output, resulting in more contrast bolus dilution with higher BMI. Adjusting contrast administration to blood volume and cardiac output may compensate for this influence of dilution. As in daily clinical practice these parameters are often difficult to obtain, easily available alternatives would be more convenient. BSA is known to be a good indicator of metabolic active mass and therefore to be correlated to blood volume and CO. For this reason BSA is generally used for dosing of intravenous drugs, rather than BMI, which is more related to body fat. This may explain why BSA, reflecting CO and blood volume was slightly closer correlated to attenuation than CO alone. It has therefore been theoretically suggested that contrast medium should be adjusted to BSA [9]. Our study confirms a close relationship between BSA and attenuation.
The use of a BMI-adapted scanning protocol allows the reduction of BMI-interference on image noise as evidenced by similar noise values over a large range of BMI. As mentioned above BSA is much closer related to blood volume and CO than BMI. In fact our results show that BSA is slightly stronger related to attenuation than BMI. Therefore, we conclude that the effect of dilution with decreased attenuation and CNR caused by an increasing blood volume and CO may be best compensated for by adaptation of contrast administration to BSA.
We acknowledge the following limitations. First, the amount of contrast material was not BMI-adapted in concordance with a large body of literature [1–4, 6, 8], although suggested by a few previous reports [9, 10]. However, only the use of a fixed amount of contrast material enabled us to specifically evaluate the influence of BMI on image noise and coronary vessel attenuation. Second, coronary attenuation and CNR were selectively evaluated in the LMA, while distal segments were not evaluated, as the small diameters of distal segments do not allow reliably placing a ROI without including parts of the vessel wall and adjacent tissue thus causing partial volume effects.
Conclusion
Our results have shown that a BMI adapted protocol widely reduces the impact of BMI on image noise, while vessel contrast remains subject to large variations, depending on bolus dilution by blood volume and CO. Our study has identified BSA as the most promising parameter to be of potential value for adjusting the contrast bolus in future protocols.
References
Leber AW, Knez A, von Ziegler F et al (2005) Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 46:147–154
Leschka S, Alkadhi H, Plass A et al (2005) Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart 26:1482–1487
Mollet NR, Cademartiri F, van Mieghem CA et al (2005) High-resolution spiral computed tomography coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation 112:2318–2323
Raff GL, Gallagher MJ, O’Neill WW et al (2005) Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol 46:552–557
Husmann L, Valenta I, Gaemperli O et al (2008) Feasibility of low-dose coronary CT angiography: first experience with prospective ECG-gating. Eur Heart J 29:191–197
Hsieh J, Londt J, Vass M et al (2006) Step-and-shoot data acquisition and reconstruction for cardiac X-ray computed tomography. Med Phys 33:4236–4248
Hoffmann MH, Shi H, Manzke R et al (2005) Noninvasive coronary angiography with 16-detector row CT: effect of heart rate. Radiology 234:86–97
Pugliese F, Mollet NR, Runza G et al (2006) Diagnostic accuracy of non-invasive 64-slice CT coronary angiography in patients with stable angina pectoris. Eur Radiol 16:575–582
Bae KT, Seeck BA, Hildebolt CF et al (2008) Contrast enhancement in cardiovascular MDCT: effect of body weight, height, body surface area, body mass index, and obesity. AJR Am J Roentgenol 190:777–784
Husmann L, Leschka S, Boehm T et al (2006) Influence of body mass index on coronary artery opacification in 64-slice CT angiography. Rofo. 178:1007–1013
Stanford W, Burns TL, Thompson BH et al (2004) Influence of body size and section level on calcium phantom measurements at coronary artery calcium CT scanning. Radiology 230:198–205
Bae KT, Heiken JP, Brink JA (1998) Aortic and hepatic contrast medium enhancement at CT. Part II. Effect of reduced cardiac output in a porcine model. Radiology 207:657–662
Husmann L, Alkadhi H, Boehm T et al (2006) Influence of cardiac hemodynamic parameters on coronary artery opacification with 64-slice computed tomography. Eur Radiol 16:1111–1116
Sivit CJ, Taylor GA, Bulas DI et al (1992) Posttraumatic shock in children: CT findings associated with hemodynamic instability. Radiology 182:723–726
Motoyama S, Anno H, Sarai M et al (2008) Noninvasive coronary angiography with a prototype 256-row area detector computed tomography system: comparison with conventional invasive coronary angiography. J Am Coll Cardiol 51:773–775
Rybicki FJ, Otero HJ, Steigner ML et al (2008) Initial evaluation of coronary images from 320-detector row computed tomography. Int J Cardiovasc Imaging 24:535–546
Einstein AJ, Moser KW, Thompson RC et al (2007) Radiation dose to patients from cardiac diagnostic imaging. Circulation 116:1290–1305
Achenbach S, Giesler T, Ropers D et al (2003) Comparison of image quality in contrast-enhanced coronary-artery visualization by electron beam tomography and retrospectively electrocardiogram-gated multislice spiral computed tomography. Invest Radiol 38:119–128
Schepis T, Gaemperli O, Koepfli P et al (2007) Use of coronary calcium score scans from stand-alone multislice computed tomography for attenuation correction of myocardial perfusion SPECT. Eur J Nucl Med Mol Imaging 34:11–19
Acknowledgments
The study was supported by a grant from the Swiss National Science Foundation (SNSF-professorship grant No. PP00A-114706) and by the ZIHP (Zurich Center for Integrative Human Physiology, University of Zurich, Switzerland).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Herzog, B.A., Husmann, L., Valenta, I. et al. Determinants of vessel contrast in BMI-adapted low dose CT coronary angiography with prospective ECG-triggering. Int J Cardiovasc Imaging 25, 625–630 (2009). https://doi.org/10.1007/s10554-009-9460-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-009-9460-3