Abstract
Objectives
To compare the diagnostic accuracy between low-kilovolt peak (kVp) (≤ 100) and high-kVp (> 100) third-generation dual-source coronary CT angiography (CCTA) using a kVp-tailored contrast media injection protocol.
Methods
One hundred twenty patients (mean age = 62.6 years, BMI = 29.0 kg/m2) who underwent catheter angiography and CCTA with automated kVp selection were separated into two cohorts (each n = 60, mean kVp = 84 and 117). Contrast media dose was tailored to the kVp level: 70 = 40 ml, 80 = 50 ml, 90 = 60 ml, 100 = 70 ml, 110 = 80 ml, and 120 = 90 ml. Contrast-to-noise ratio (CNR) was measured. Two observers evaluated image quality and the presence of significant coronary stenosis (> 50% luminal narrowing).
Results
Diagnostic accuracy (sensitivity/specificity) with ≤ 100 vs. > 100 kVp CCTA was comparable: per patient = 93.9/92.6% vs. 90.9/92.6%, per vessel = 91.5/97.8% vs. 94.0/96.8%, and per segment = 90.0/96.7% vs. 90.7/95.2% (all P > 0.64). CNR was similar (P > 0.18) in the low-kVp vs. high-kVp group (12.0 vs. 11.1), as ws subjective image quality (P = 0.38). Contrast media requirements were reduced by 38.1% in the low- vs. high-kVp cohort (53.6 vs. 86.6 ml, P < 0.001) and radiation dose by 59.6% (4.3 vs. 10.6 mSv, P < 0.001).
Conclusions
Automated tube voltage selection with a tailored contrast media injection protocol allows CCTA to be performed at ≤ 100 kVp with substantial dose reductions and equivalent diagnostic accuracy for coronary stenosis detection compared to acquisitions at > 100 kVp.
Key points
• Low-kVp coronary CT angiography (CCTA) enables reduced contrast and radiation dose.
• Diagnostic accuracy is comparable between ≤ 100 and > 100 kVp CCTA.
• Image quality is similar for low- and high-kVp CCTA.
• Low-kVp image acquisition is facilitated by automated tube voltage selection.
• Tailoring contrast injection protocols to the automatically selected kVp-level is feasible.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The increased utilisation of coronary CT angiography (CCTA) has prompted efforts to reduce the associated ionising radiation and contrast media dose via a number of approaches, such as prospective ECG triggering and anatomy-based tube current modulation [1,2,3]. Lowering the x-ray tube potential [peak voltage in kilovolts (kVp)] is another attractive strategy that decreases the radiation dose while increasing iodine attenuation, indirectly leading to a reduction in intravenous contrast media requirements [2, 4,5,6,7]. However, the advantages of low-kVp acquisitions must be weighed against a concomitant increase in image noise. In previous investigations that used prior CT platforms, a decrease in both image quality and diagnostic accuracy was observed for low-kVp examinations when compared to CCTA using 110 and standard 120 kVp settings [8,9,10,11]. This negative effect is even more apparent in overweight and obese patients, in whom high image noise is an inherent limitation [12]. Therefore, the application of tube voltages < 90 kVp has been traditionally limited to patients with a slim to normal build [5, 8, 13,14,15].
Hard- and software advancements used in the most recent “third generation” of dual-source CT scanners have been reported to maintain image quality when using lower tube voltages. These features include increased x-ray tube power [5, 16], refined iterative reconstruction techniques [5, 16, 17], and individual automated tube voltage selection based on topogram-derived patient anatomy, which is performed prior to image acquisition [9, 18]. Results from a sub-analysis in a prior study suggest that diagnostic accuracy of CCTA for the detection of coronary artery stenosis may be similar at both low- and high-kVp levels using current state-of-the-art dual-source CT equipment with simultaneously reduced radiation and contrast dose [9]. In addition, based on prior investigations, we further modified a kVp-tailored contrast media injection protocol to fit the scope of the current study [9, 18].
Thus, we aimed to compare the diagnostic accuracy between low- (≤ 100) and high-kVp (> 100) third-generation dual-source CCTA using a kVp-tailored contrast media injection protocol with invasive catheter angiography (ICA) as the reference standard.
Material and methods
Patients
This retrospective study was approved by our local IRB with a waiver of informed consent and was conducted in HIPAA compliance. We investigated 120 patients with known or suspected coronary artery disease who had undergone CCTA and ICA within a 21-day period between January 2014–November 2016. Radiology and patient information databases were randomly screened to build two cohorts of patients having undergone CCTA examinations of different tube potential (each n = 60), specifically either low (≤ 100) or high kVp (> 100). Patients were consecutively identified and included until the maximum enrolment for each group was obtained. Coronary segments with stents or communicating coronary artery bypass grafts were excluded. Patient characteristics are summarised in Table 1.
Image acquisition
All CCTA data were acquired using a third-generation dual-source CT scanner (Somatom Force, Siemens Healthineers, Forchheim, Germany) with a maximum x-ray tube current power of 1300 mAs [5].
ECG-triggered unenhanced images at 70% of the cardiac cycle were acquired to determine the Agatston scores. Reference tube current was 80 mAs, and tube voltage was 120 kVp.
Prospective adaptive-sequential contrast-enhanced scan data were acquired during 30-90% of the RR-interval with a full nominal tube current applied over 10% of the RR interval in either end diastole (heart rate ≤ 80 beats per minute) or end systole (heart rate > 80 beats per minute). No anxiolytics were administered during CCTA acquisition. The current was reduced to 20% of the default tube output value over the remaining cardiac cycle. The z-axis coverage extended from the carina to the cardiac base. Automated tube current modulation (CareDose4D, Siemens) and automated tube voltage selection (ATVS, Siemens) were used. Thus, individualised kVp settings were automatically selected based on the patient’s body habitus, and contrast media volume was adjusted according to the applied kVp level: 70 kVp = 40 ml, 80 kVp = 50 ml, 90 kVp = 60 ml, 100 kVp = 70 ml, 110 kVp = 80 ml, and 120 kVp = 90 ml. Image acquisition was guided using the bolus-tracking technique and initiated after a threshold of 100 Hounsfield units (HU) was reached in a region of interest (ROI) in the descending aorta. Contrast agent (370 mgI/ml iopromide, Ultravist, Bayer, Wayne, NJ) was administered through an antecubital vein with a flow rate of 4 and 5 ml/s for low- and high-kVp examinations, respectively. Contrast administration was followed by a 50-ml saline chaser bolus.
Further settings of image acquisition were as follows: adaptive detector collimation varying in 96-192 steps of 8 × 0.6 mm, gantry rotation time = 0.25/s, and matrix size = 512 × 512 pixels.
Image data were reconstructed using iterative reconstruction (Admire, Siemens, strength level = 3) and a semi-sharp reconstruction kernel algorithm (Bv36). Section-thickness and increment were set to 0.6 mm and 0.4 mm, respectively. The phase with the least cardiac motion was automatically selected (BestPhase, Siemens).
ICA (Axiom Artis, Siemens) was performed within 21 days after CCTA image acquisition using the conventional Judkins approach. ICA interpretation by two cardiologists with >5 years of experience served as the reference standard. Each coronary artery segment was analysed from at least two perpendicular planes and luminal narrowing >50% was regarded as significant stenosis [3, 10].
Quantitative analysis
Further evaluation was performed using a dedicated 3D workstation (syngo.via VB10B, Siemens). A radiologist with 3 years of experience in cardiovascular imaging performed the quantitative CCTA analysis. Attenuation was measured in HU by placing an ROI in the following coronary arteries: left main (LM), left anterior descending (LAD), left circumflex (LCX), and right coronary artery (RCA). ROIs were drawn as large as possible while carefully avoiding inclusion of the vessel wall or atherosclerotic plaque. Measurements were performed three times and averaged to minimise measuring inaccuracies. Attenuation in the LM was determined in one location, as opposed to the LAD, LCX, and RCA, which were measured in both the proximal and distal portions. To define vessel contrast, attenuation was measured in an ROI placed in the adjacent pericardial fat tissue (size, 50 mm2). Image noise was defined as the standard deviation (SD) in an ROI in the left-ventricular blood pool (size, 200 mm2). The following formulas were used to quantify image quality: signal-to-noise ratio (SNR) = HU artery/noise and contrast-to-noise ratio (CNR) = (HU artery – HU fat)/ noise [9, 19].
The dose-length-product (DLP) specified in the examination protocols was multiplied with a conversion factor of k = 0.014 mSv/ mGy*cm to estimate effective radiation dose values [2].
Qualitative analysis
Two independent radiologists with 5 and 4 years of experience in cardiovascular imaging, respectively, analysed the CCTA data sets in a randomised order. Observers were blinded to patient demographics, scan indication, and findings. Standard 3D multi-planar reformats (MPR), maximum intensity projections (MIP), and curved MPRs could be freely modified and reoriented. Preset window settings (width 800, level 200) could be adjusted according to each reader’s preference to optimise contrast and reduce blooming artefacts.
Reviewers assessed overall image quality (ranging from 1 = non-diagnostic to 5 = excellent image quality), image sharpness (ranging from 1 = noticeable blurring to 5 = excellent sharpness) and contrast (ranging from 1 = poor to 5 = excellent contrast) in consensus interpretation sessions. For the evaluation of coronary arteries, the coronary artery tree was divided into 16 segments using a modified 18-segment model of the American Heart Association [9, 20]. Segments 1-14 were coronary artery segments of the RCA, LAD, and LCX. Segment 15 combined the left posterior descending artery (PDA) and posterolateral branch, and segment 16 represented the ramus intermedius. Initially, visualisation of all coronary segments was classified as either diagnostic or non-diagnostic (due to motion artefacts, poor contrast, or extensive noise) to evaluate coronary artery stenosis. Non-diagnostic segments were excluded from the analysis. Subsequently, readers rated each coronary segment as negative (score = 0) or positive (score = 1) for the presence of significant coronary artery stenosis (> 50% luminal narrowing). When multiple lesions were found in a coronary segment, the lesion with the highest grade of stenosis was used for analysis.
Statistical evaluation
Statistical assessments were performed using commercially available software (MedCalc Statistical Software, V12.7.5.0, MedCalc bvba, Ostend, Belgium and Stata IC/14.2; StataCorp, College Station, TX, USA). Continuous variables were expressed as mean ± SD.
After the Kolmogorov-Smirnov test was performed, data were assessed using either a paired Student’s t-test (normal distribution) or Wilcoxon-matched pairs test (non-normal distribution).
Using ICA as the reference standard, sensitivity, specificity, positive- (PPV) and negative predictive values (NPV), and accuracy were calculated for low- and high-kVp CCTA examinations. Per-patient estimates were compared using an unpaired chi-squared test. In addition, the per-vessel and per-segment estimates were compared using logistic regression and variance adjustment by sandwich estimator to account for multiple segments and vessels per patient [21].
A P-value <0.05 was considered statistically significant for the tests that were performed.
Results
The mean tube voltages for the two patient cohorts were 83.6 ± 10.6 and 116.5 ± 4.7 kVp, respectively (P < 0.001). Average patient age for the low- and high-kVp group was 65.0 ± 10.8 and 60.2 ± 9.0 years (P = 0.02). Mean BMI was 28.2 ± 4.0 and 29.9 ± 4.3 kg/m2 in the low- and high-kVp cohorts (P = 0.04). Agatston scores were comparable (P = 0.25) for the low- (809.4 ± 1069.2) vs. high-kVp group (728.8 ± 1137.3). Significant coronary artery stenosis was present in 33/60 (55%) patients in each cohort. Further information is summarised in Table 1.
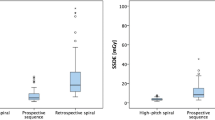
Contrast and radiation dose
On average, 53.6 ± 10.5 and 86.6 ± 4.7 ml of contrast media were administered in the low- and high-kVp cohorts, respectively. The mean DLP was 307.8 ± 387.1 and 763.7 ± 528.1 mGy*cm for the low- and high-kVp groups (P < 0.001), resulting in an effective dose of 4.3 ± 5.4 and 10.6 ± 7.3 mSv (P < 0.001) (Table 1).
Quantitative image quality analysis
Results for the analyses of image quality are shown in Table 2. Attenuation was increased using lower tube voltages compared to high-kVp scans in all measured coronary artery segments (P < 0.001). However, image noise was significantly higher in low-kVp examinations (P < 0.001).
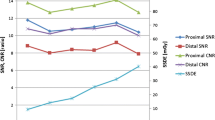
Comparable CNR and SNR values (P > 0.18) were found for low- and high-kVp CCTA studies (proximal CNR, 12.7 ± 5.0 vs. 11.8±4.1; distal CNR, 11.3 ± 4.7 vs. 10.4 ± 3.9; proximal SNR, 10.5 ± 4.2 vs. 9.6 ± 3.4; distal SNR, 9.1 ± 4.0 vs. 8.2 ± 3.3, respectively).
Qualitative image quality
Attenuation was rated higher for the low-kVp cohort in both the proximal and distal coronary arteries (P < 0.05). Neither image sharpness (P = 0.54) nor subjective image quality (P = 0.38) were significantly different between the groups (Table 2).
Diagnostic accuracy
Of the 1920 possible coronary artery segments, 183 were excluded because of motion artefact (n = 13), prior stent placement (n = 14), previous CABG (n = 3), or anatomic variants (n = 153). Thus, 1737 segments were evaluated for the presence of significant coronary stenosis.
Indices of diagnostic accuracy for both cohorts were comparable (P > 0.36). In detail, sensitivity and specificity for significant stenosis detection for the low- vs. high-kVp cohort, respectively, were: per patient = 93.9 and 92.6% vs. 90.9 and 92.6%, per vessel = 91.5 and 97.8% vs. 94.0 vs. 96.8%, and per segment = 90.0 and 96.7 vs. 90.7 and 95.2%. Accuracy values for the low- and high-kVp groups were: per patient = 93.3 vs. 91.7%, per vessel = 96.3 vs. 96.3%, and per segment = 96.0 vs. 94.7%, respectively. Further details are summarised in Table 3 and illustrated in Fig. 1.
Discussion
This investigation aimed to compare the diagnostic accuracy of CCTA examinations using either ≤ 100 kVp or > 100 kVp settings combined with a kVp-tailored contrast medium injection protocol. Our results demonstrate that, when using the most recent and advanced CT technology, specifically automated tube voltage selection, ≤ 100 kVp CCTA protocols can be employed without any detrimental effect on diagnostic accuracy for the detection of coronary stenosis. Furthermore, substantial reductions in radiation dose and contrast media volume can be achieved using this low-kVp scan protocol compared to the standard > 100 kVp image acquisition.
We found comparable quantitative and qualitative image quality for the low- vs. high-kVp CCTA cohorts (Fig. 2), which is in accordance with prior studies using the same CT technology [5, 9]. Our data suggest that the image quality achieved using low-kVp CCTA protocols with tailored contrast administration translates into comparable diagnostic accuracy for the detection of coronary artery stenosis, with sensitivity and specificity values similar to those reported in previous studies using standard (i.e., ordinarily 120) kVp acquisitions. In the current investigation, values for sensitivity and specificity ranged from 91–98% in all patient-, vessel-, and segment-based analyses [9, 22,23,24]. Notably, we found that low-kVp examinations with a substantially decreased tube potential (mean decrease: 28.3%) compared to standard kVp examinations were associated with a distinct reduction in radiation and contrast media requirements (Fig. 3). Specifically, effective radiation dose and contrast media volume were decreased by 6.3 mSv (59.6%) and 33 ml (38.1%), respectively. Thus, our data support the feasibility and clinical usefulness of ≤100 kVp tube potentials and the implementation of a kVp-tailored contrast injection protocol for CCTA image acquisition. While a prior study with the same CT technology used a kVp-adapted injection approach for tube voltages between 70-100 kVp, the current study further refined this strategy by tailoring contrast injections to a greater range of tube potentials, specifically 70-120 kVp [9]. Thus, our data may help to further support and elucidate the utility of kVp-tailored contrast injection.
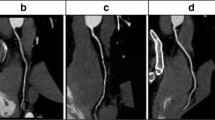
Contrast conditions of the right coronary arteries without significant stenoses at low (A = 70 kVp) and high tube potentials (B = 120 kVp). The low-kVp image acquisition allows for sufficient iodine attenuation, despite lower contrast media doses (40 ml) compared to the high-kVp examination (90 ml). Subjective ratings regarding image quality, sharpness, and contrast were equivalent (all scores = 5). BMI values were 28 and 29 kg/m2 for low and high CCTA. Window settings were: level = 400, width = 1100 Hounsfield units
This 73-year-old male patient (BMI = 29.5) showed significant stenosis of the mid LAD on invasive catheter angiography (A, arrow) and 70-kVp CCTA images (B, arrowhead). A total of 40 ml contrast media volume was administered for CCTA image acquisition according to the kVp-tailored injection protocol. Image quality and contrast of CCTA reconstructions were rated as excellent. The lesion was treated with stent placement, effectively restoring coronary blood flow (C). BMI body mass index; LAD left anterior descending coronary artery
A reduction of effective radiation dose by means of decreasing kVp while increasing mAs is technically feasible, because radiation is altered by approximately the square of the change in tube voltage, whereas the relationship of radiation dose to tube current is linear [25]. Furthermore, with reduced tube voltages, the x-ray spectrum moves closer to the k-edge of iodine (33.2 keV), providing increased photon attenuation (and consequently higher CT numbers) of contrast-enhanced coronary lumina. Consequently, our data demonstrate slightly greater coronary artery attenuation in the low-kVp cohort. These potentials for radiation and contrast dose reductions, however, could not be fully exploited using previous generations of CT technology. This limitation was predominantly due to considerably increased noise and subsequent decreases in both image quality and diagnostic accuracy when using lower tube voltage settings for CCTA in normal-sized or obese patients [10, 11, 16]. As previously noted, third-generation dual-source CT technology helps counteract the higher image noise that was traditionally observed at low-kVp levels. This is accomplished through increased x-ray tube power, which is able to generate higher currents to avoid excessive noise [5, 16], routine implementation of noise-reducing iterative reconstruction techniques [16, 17], and automated tube voltage selection based on patient body habitus [18]. We believe that all of these features contributed to the comparable image quality and diagnostic accuracy observed between low- and high-kVp cohorts in our study.
Overweight patients so far were mostly excluded from the benefits of low-kVp CCTA due to increased image noise. Consequently, low tube voltage levels (kVp < 90) were predominantly applied to children and patients with a slighter body habitus (BMI 18.5–25) [5, 13,14,15, 26]. However, the present study demonstrates that the diagnostic accuracy of CCTA is not adversely affected by applying lower tube voltages despite our generally overweight patient population (mean BMI = 28.2, Fig. 4) and the presence of heavily calcified coronary atherosclerosis (mean Agatston score = 809.4). This finding is in agreement with the results of a prior phantom experiment [16] and a sub-group analysis of an in-vivo study [9] suggesting that current radiation and contrast-saving strategies such as low-kVp scanning can be routinely applied using the most recent dual-source CT technology, particularly through the use of automated tube voltage selection based on patient body habitus. By including more patients (120 vs. 76 individuals), using a lower tube voltage in the ≤ 100 kVp study group (mean kVp = 83.6 vs. 91.1), and implementing a refined kVp-tailored contrast media injection protocol, we have effectively strengthened these previous notions.
Several limitations of our study deserve additional consideration beyond the retrospective single-centre design. The injection volume of the kVp-tailored contrast media protocol was empirically estimated based on both previous investigations [9, 18] and our clinical experience; thus, our protocol should be further optimised. In addition, we only used two different injection flow velocities for low- and high-kVp examinations and therefore did not tailor the iodine delivery rate to each kVp level as suggested in a more recent study [27]. Moreover, our tailored contrast injection protocol requires further refinement when applied to patient populations with a greater proportion of lithe, normal-sized, or morbidly obese individuals, as our study was predominantly conducted in overweight individuals. Likewise, the algorithm that was used for automated tube voltage selection needs to be re-evaluated in patients within a normal weight range. Another noteworthy limitation to the study is that the kVp level was automatically selected by the scanner, independent of technologist and radiologist direction. Accordingly, based on the current data, it remains unknown whether tube potentials ≤ 100 kVp can be applied to a general population without compromising diagnostic accuracy for coronary stenosis detection. Lastly, although we had ICA as the reference standard and included 120 patients, our study was not performed in the same individuals. An additional intra-individual comparison of low- and high-kVp settings would therefore be desirable to confirm our findings.
In conclusion, this study demonstrates that third-generation dual-source CCTA using a kVp-tailored contrast injection protocol and automated tube voltage selection can be safely performed at ≤ 100 kVp in a population of mostly overweight individuals. Diagnostic accuracy for coronary stenosis detection is maintained compared to acquisition at > 100 kVp and the protocol enables substantial reductions in both radiation and contrast dose.
This obese 74-year-old female patient (BMI = 32.8) showed severe stenosis (arrow) of the mid LAD artery on both invasive catheterisation (A) and 80 kVp CCTA using 50 ml of contrast material. The CCTA curved (B) and standard (C) multi-planar reformats reveal distinct calcified and non-calcified composition of the plaque, which is substantially narrowing the coronary lumen (arrowheads). Cinematic rendering reconstructions (not approved for clinical use) reveal irregularity of the affected segment (D)
References
De Cecco CN, Meinel FG, Chiaramida SA et al (2014) Coronary artery computed tomography scanning. Circulation 129:1341–1345
Hausleiter J, Meyer TS, Martuscelli E et al (2012) Image quality and radiation exposure with prospectively ECG-triggered axial scanning for coronary CT angiography. JACC Cardiovasc Imaging 5:484–493
Moscariello A, Takx RAP, Schoepf UJ et al (2011) Coronary CT angiography: image quality, diagnostic accuracy, and potential for radiation dose reduction using a novel iterative image reconstruction technique—comparison with traditional filtered back projection. Eur Radiol 21:2130–2138
Jun BR, Yong HS, Kang E-Y et al (2012) 64-slice coronary computed tomography angiography using low tube voltage of 80 kV in subjects with normal body mass indices: comparative study using 120 kV. Acta Radiol Stockh Swed 1987 53:1099–1106
Meyer M, Haubenreisser H, Schoepf UJ et al (2014) Closing in on the K edge: Coronary CT angiography at 100, 80, and 70 kV—Initial comparison of a second- versus a third-generation dual-source CT system. Radiology 273:373–382
Zhang LJ, Wang Y, Schoepf UJ et al (2016) Image quality, radiation dose, and diagnostic accuracy of prospectively ECG-triggered high-pitch coronary CT angiography at 70 kVp in a clinical setting: comparison with invasive coronary angiography. Eur Radiol 26:797–806
Spearman JV, Schoepf UJ, Rottenkolber M et al (2016) Effect of automated attenuation-based tube voltage selection on radiation dose at CT: An observational study on a global scale. Radiology 279:167–174
Wang D, Hu X, Zhang S et al (2012) Image quality and dose performance of 80 kV low dose scan protocol in high-pitch spiral coronary CT angiography: feasibility study. Int J Cardiovasc Imaging 28:415–423
Mangold S, Wichmann JL, Schoepf UJ et al (2016) Diagnostic accuracy of coronary CT angiography using 3rd-generation dual-source CT and automated tube voltage selection: Clinical application in a non-obese and obese patient population. Eur Radiol. 27:2298–2308
Stehli J, Fuchs TA, Bull S et al (2014) Accuracy of coronary CT angiography using a submilliSievert fraction of radiation exposure: comparison with invasive coronary angiography. J Am Coll Cardiol 64:772–780
Layritz C, Schmid J, Achenbach S et al (2014) Accuracy of prospectively ECG-triggered very low-dose coronary dual-source CT angiography using iterative reconstruction for the detection of coronary artery stenosis: comparison with invasive catheterization. Eur Heart J Cardiovasc Imaging 15:1238–1245
Modica MJ, Kanal KM, Gunn ML (2011) The obese emergency patient: imaging challenges and solutions. Radiogr Rev Publ Radiol Soc N Am Inc 31:811–823
Yin W-H, Lu B, Li N et al (2013) Iterative reconstruction to preserve image quality and diagnostic accuracy at reduced radiation dose in coronary CT angiography: an intraindividual comparison. JACC Cardiovasc Imaging 6:1239–1249
Schuhbaeck A, Achenbach S, Layritz C et al (2013) Image quality of ultra-low radiation exposure coronary CT angiography with an effective dose <0.1 mSv using high-pitch spiral acquisition and raw data-based iterative reconstruction. Eur Radiol 23:597–606
LaBounty TM, Leipsic J, Poulter R et al (2011) Coronary CT angiography of patients with a normal body mass index using 80 kVp versus 100 kVp: a prospective, multicenter, multivendor randomized trial. AJR Am J Roentgenol 197:W860–W867
Meinel FG, Canstein C, Schoepf UJ et al (2014) Image quality and radiation dose of low tube voltage 3rd generation dual-source coronary CT angiography in obese patients: a phantom study. Eur Radiol 24:1643–1650
Geyer LL, Schoepf UJ, Meinel FG et al (2015) State of the art: Iterative CT reconstruction techniques. Radiology 276:339–357
Mangold S, Wichmann JL, Schoepf UJ et al (2016) Automated tube voltage selection for radiation dose and contrast medium reduction at coronary CT angiography using 3rd generation dual-source CT. Eur Radiol. 86:276–283
Albrecht MH, Trommer J, Wichmann JL et al (2016) Comprehensive comparison of virtual monoenergetic and linearly blended reconstruction techniques in third-generation dual-source dual-energy computed tomography angiography of the thorax and abdomen. Invest Radiol. 51:582–590
Leipsic J, Abbara S, Achenbach S et al (2014) SCCT guidelines for the interpretation and reporting of coronary CT angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 8:342–358
Genders TSS, Spronk S, Stijnen T et al (2012) Methods for calculating sensitivity and specificity of clustered data: a tutorial. Radiology 265:910–916
Menke J, Unterberg-Buchwald C, Staab W, et al (2013) Head-to-head comparison of prospectively triggered vs retrospectively gated coronary computed tomography angiography: Meta-analysis of diagnostic accuracy, image quality, and radiation dose. Am Heart J 165:154–163.e3.
Meijer AB, Ying OL, Geleijns J, Kroft LJM (2008) Meta-analysis of 40- and 64-MDCT angiography for assessing coronary artery stenosis. Am J Roentgenol 191:1667–1675
Ruzsics B, Lee H, Zwerner PL et al (2008) Dual-energy CT of the heart for diagnosing coronary artery stenosis and myocardial ischemia-initial experience. Eur Radiol 18:2414–2424
Kalra MK, Maher MM, Toth TL et al (2004) Strategies for CT radiation dose optimization. Radiology 230:619–628
Cao J, Wang Y, Lu J et al (2014) Radiation and contrast agent doses reductions by using 80-kV tube voltage in coronary computed tomographic angiography: A comparative study. Eur J Radiol 83:309–314
Lell MM, Fleischmann U, Pietsch H et al (2017) Relationship between low tube voltage (70 kV) and the iodine delivery rate (IDR) in CT angiography: An experimental in-vivo study. PLOS ONE 12:e0173592
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is U. Joseph Schoepf, MD.
Conflict of interest
The authors of this manuscript declare relationships with the following companies: U. Joseph Schoepf is a consultant for and/or receives research support from Astellas, Bayer, Bracco, GE, Guerbet, Medrad, and Siemens. Katharina Otani is an employee of Siemens. Akos Varga-Szemes is a consultant for and/or receives research support from Guerbet and Siemens. Carlo N. De Cecco is a consultant for and/or receives research support from Guerbet and Siemens.
Funding
The authors state that this work has not received any funding.
Statistics and biometry
Katharina Otani, PhD, kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Rights and permissions
About this article
Cite this article
Albrecht, M.H., Nance, J.W., Schoepf, U.J. et al. Diagnostic accuracy of low and high tube voltage coronary CT angiography using an X-ray tube potential-tailored contrast medium injection protocol. Eur Radiol 28, 2134–2142 (2018). https://doi.org/10.1007/s00330-017-5150-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5150-z