Abstract
This mixed methods study evaluated the efficacy of an intervention to increase HIV status disclosure and condom use among 184 women living with HIV/AIDS (WLH/A). Participants were recruited from an HIV clinic and randomly assigned to: (1) a comparison group, who received brief messages from their health care providers (HCPs), or; (2) an intervention group, who received messages from HCPs, a group-level intervention, and peer-led support groups. Participants completed risk surveys at baseline, 6-, 12-, and 18-months. Quantitative analyses using hierarchical generalized linear models within a repeated measures framework indicated that intervention participants had significantly higher odds of reporting condom use with sexual partners in months 6 and 18. Grounded Theory-based qualitative analyses suggested that the opportunity to discuss the social context of their lives in addition to HIV/AIDS, including continued stigma and fear related to disclosure, are also essential components of a prevention strategy for WLH/A.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Women comprise one of the fastest growing populations with HIV/AIDS in the US (CDC 2008). Rates of the virus are alarmingly high among Black and Latina women, who accounted for 24% of US women and 82% of AIDS diagnoses in 2005(CDC 2008). Although many women living with HIV/AIDS (WLH/A) practice safe sex, many also have risky sex, with roughly one-third having reported unprotected sex with their male partners (Aidala et al. 2006; Golden et al. 2007; Wilson et al. 2004). Prevention programs for WLH/A can play an integral role in helping women adopt safer and healthier sex lives to protect their partners from acquiring HIV; protect themselves from acquiring sexually transmitted infections (STIs) or other strains of HIV/AIDS; and obtain emotional support as they cope with difficult intimacy or sexual concerns (Collins et al. 2000; Kalichman 2004).
Engaging in safe sex is difficult and complex. WLH/A in the US are mostly poor and members of racial/ethnic minority communities who report few educational and/or employment opportunities (Barkan et al. 1998; CDC 2008), high rates of relationship violence (Gielen et al. 2007) and AIDS-related stigma (Sandelowski et al. 2004). Often, these cultural, psychosocial, and structural challenges hinder women from protecting themselves from HIV initially, and limit their ability to practice safer sex once they have HIV/AIDS (Amaro 1995; CDC 2008; Zierler and Krieger 1997).
The growing number of WLH/A and the disproportionate rates of HIV/AIDS among marginalized women signal a critical need for empirically validated safer sex strategies that reflect WLH/A’s life challenges and experiences. Although a handful of proven behavioral interventions exist to help both men and women with HIV/AIDS decrease their risky sexual practices (Fisher et al. 2006; Gilbert et al. 2008; The Healthy Living Project Team 2007; Kalichman et al. 2001; Patterson et al. 2003; Richardson et al. 2004; Sikkema et al. 2007), we are aware of few published interventions that are tailored to the specific needs of WLH/A (Fogarty et al. 2001; Wingood et al. 2004). Because women and men face vastly different safer sex challenges, such tailored interventions are necessary.
Thus, this mixed methods study describes key findings from Protect and Respect, an intervention designed to help WLH/A, the majority of whom were Black and Latina, decrease their sexual risk practices. We used quantitative methods to investigate the effect of the intervention on women’s disclosure of their HIV status to partners and unprotected vaginal and anal sex acts (N = 184). We also used qualitative methods to examine how women experienced the group intervention and perceived it to be associated with their safer sex and disclosure skills. Using both quantitative and qualitative methods allowed us to capitalize on the advantages of each method to obtain a more in-depth understanding of the effects of the intervention, as well as women’s experiences within it.
Methods
Participants and Procedures
Participants for Protect and Respect were recruited from the Partnership Comprehensive Care Practice (PCCP) in Philadelphia, PA. The PCCP provides comprehensive and integrated HIV services to more than 1,300 men (68%) and women (32%) annually, and serves people living with HIV/AIDS exclusively. The total Protect and Respect sample included 184 women with HIV/AIDS between the ages of 20 and 70 (M = 39.8, SD = 8.5) at baseline. The majority of the sample identified as Black (n = 158, 85.9%), with relatively low incomes (n = 139, 75.5% reporting annual incomes of $10,000 or less). Participants reported living with HIV for a range of 0.3 (3.6 months) to 20.1 years (M = 8.7, SD = 5.0). Key demographic and behavioral variables for this sample at baseline are presented in Table 1. The qualitative subsample for this study included 18 women who participated in the group-level-intervention (GLI) and Peer groups. This sample size of 18 interviewees is consistent with the “15 ± 10” metric for qualitative studies (Kvale 1996, p. 102). The qualitative participants were similar demographically to the full study sample described above.
The Protect and Respect recruitment team included two peer educators (PEs) (a Black and Latina WLH/A) and three research assistants (RAs). PEs and RAs recruited women from the PCCP’s waiting room from April, 2004 through July, 2006 using flyers to initiate discussions with women who were waiting for their regularly scheduled medical visits. To be eligible to participate, women had to be at least 18-year-old, HIV-positive for at least 6-months, and English-speaking. The PEs or RAs confirmed women’s eligibility after screening for eligibility criteria in discussions with potential participants. Our recruitment team took detailed notes on the recruitment process and recorded that we approached and discussed the project with a little more than twice the number of women that we enrolled. We approached nearly all of the women in the clinic’s waiting room on the days that we recruited (some women were approached more than once) about the study unless they were asleep, visibly intoxicated, or visibly upset (e.g., crying, in an argument with their partner). Most (~85%) of the women that we approached were eligible for the study. The most common exclusion criterion was the inability to speak and read English. Only about 40% of the eligible women were interested in enrolling in the study. The most common refusal reasons included being too ill (e.g., HIV-related fatigue, in recovery) or too busy (e.g., work, parenting demands) to commit to the project.
Next, the RA took the eligible study participant to a private cubicle located on the side of the clinic’s waiting room to explain the project in more detail (i.e., what would be expected of the woman if she enrolled in the project), administer the study’s consent, complete the study’s randomization, explain and administer the baseline demographic and risk assessment survey, and schedule the participants’ next research visit(s).
After the participant signed the consent, the RA opened the next card (concealed in an envelope) from the study’s randomization binder to determine if the participant would be in the study’s comparison or intervention group. The study’s statistician generated the random assignation sequence from a computer generated schedule prior to the study’s start. Neither the study team nor the participants knew the participant’s assignment before the RA chose the next card from the binder. The comparison group received brief messages delivered by health care providers (HCPs) during routine medical visits. The intervention group received messages from providers and a five session GLI, followed by weekly peer-led support groups.
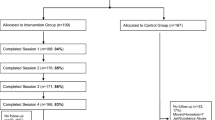
After randomization, the participant completed the study’s assessment, an audio computer-assisted self-interview (ACASI). The ACASI included questions about basic demographics; health; attitudes towards living with HIV/AIDS, the clinic, and prevention for people living with HIV/AIDS; self efficacy to solve problems; sexual behaviors and risk practices; HIV status disclosure practices; and drug and alcohol use. Participants completed the survey in ~30 min at three different time points throughout the project after baseline: 6, 12, and 18 months. The GLI included five consecutive weekly sessions, so the 6 months follow-up occurred ~4–5 months after a participant completed the GLI. Because the peer groups were open and ongoing, it was possible for a participant (i.e., based on how many times or how often she chose to go to group) to attend peer groups throughout all of the follow-up periods. The retention rate for participants across these timeframes was 71.2, 53.3, and 29.9%, respectively. There were no significant differences in attrition rates across intervention and comparison groups during these three follow-up periods (P = 0.14, 0.37 and 0.87 for 6, 12, and 18 months, respectively). The incentive for completing the ACASI was a $10 gift card. After completing the baseline survey the RA scheduled the participant for her next ACASI or for the intervention groups, depending on her study assignment.
Intervention Description
The specific components of the intervention strategies and the intervention’s rationale and development process are described in detail in Teti et al. (2007). We developed the intervention strategies using existing proven prevention strategies for women: tenets of the Transtheoretical Model of the Stages of Change (DiClemente et al. 1985), the Modified AIDS Risk Reduction Model (Ehrhardt et al. 1992), and the Theory of Gender and Power (Wingood and DiClemente 2000); and formative research, including pilot-testing of prevention messages and group activities with WLH/A.
HCPs (nurses or physicians) attended an initial 4-h training and quarterly booster training sessions to learn the intervention’s messages and prevention counseling skills, and discuss how to deliver the messages successfully given the constraints of the clinic (e.g., sick patients, limited time). During women’s regularly scheduled visits, HCPs worked with participants to assess their stage of readiness regarding condom use and/or disclosure, deliver prevention messages or teach skills, and create a follow-up plan.
A health educator with a master’s degree in public health (the first author) delivered the GLI, which included five consecutive, weekly, 1.5 h sessions that focused predominantly on safer sex by addressing sexual risk reduction education and skill-building; women’s challenges and opportunities; HIV/AIDS and STI facts; male and female condom use and condom negotiation; triggers to unsafe sex; HIV status disclosure; problem solving; healthy relationships; social support; and goal setting. Incentives for attending the GLIs included a $10 gift card, transportation tokens, and lunch. The health educator conducted seven full GLI cycles, which included 36 different women. The average attendance rates (women attended/signed up) for each cycle ranged from 22 to 92%. The number of participants in a session ranged from two to seven and on average, each GLI session included four women.
The study’s Peer Educators, one Black and one Latina WLH/A who participated in weekly supervision and training to enhance their HIV/AIDS prevention knowledge and group facilitation skills, conducted weekly 1-h support groups throughout the length of the project. Every woman who completed the GLI was eligible to attend the peer groups, which were designed to help women discuss the skills that they learned in the GLI in the context of their lives and challenges over the long term. Peer group discussions were less structured than the GLI. The GLI facilitator and the Peers collaborated weekly to outline peer sessions. Examples of peer group topics were intimate discussions about how to talk to partners about using condoms, how to make condom use fun and exciting, and how to manage or leave unhealthy relationships. Although we asked the women to attend at least two peer support groups during the project, there was no limit to the number of times participants could attend the weekly group. Incentives for the Peer groups included transportation tokens and lunch. The Peers conducted a total of 156 groups which included 30 different women. Women attended a wide range of peer groups, spanning from one to 135 groups. Most (40%, n = 12) of the women attended two peer groups or less; 27% (n = 8) attended between three and ten groups; 13% (n = 4) attended between 11 and 50 groups; and 20% (n = 6) women attended over 50 groups throughout the project. Attendance in the groups ranged from two to seven and on average, each Peer session included five women.
Quantitative Measures
The main outcomes of interest for the quantitative analysis included (1) partner disclosure of HIV status and (2) condom use with all (i.e., HIV positive, HIV negative, and HIV status unknown) of women’s partners for vaginal and anal sex. All sexual partners were included in this analysis, regardless of HIV status, because the intervention aimed to help women protect their partners and themselves, helping women decrease risks to their own health (e.g., STIs) via unsafe sex with a partner of any HIV status. These outcomes were conditional on respondents being sexually active, and therefore, all analyses were performed only on the subset of women who were sexually active (i.e., if a woman was not sexually active at a given sampling period, her data for that sampling period were excluded from analyses). On average, 61% of the participants were sexually active at any time, and there were no significant differences in the proportion of intervention or comparison women engaging in sexual activity during the study as evidenced by a Chi Square test (P > 0.05 for baseline, 6, 12, and 18).
Partner Disclosure
In order to measure partner disclosure, participants were asked “In the last 6 months, how many of your sexual partners knew you were HIV positive because you told them that you were HIV positive?” Participants were also asked to report the number of sexual partners that they had had in the previous 6 months. The partner disclosure variable was calculated by dividing the number of partners to whom they had disclosed by the total number of partners, thus creating an indicator of the proportion of partners to whom status was disclosed.
Condom Use
Respondents indicated the number of times that they had vaginal or anal sex in the last 6 months, along with the number of times that they had used condoms for vaginal or anal sex during that time period. The proportion of sexual acts where a condom was used served as the outcome of interest for this risk behavior.
Quantitative Analyses
We used hierarchical generalized linear models (HGLM) within a repeated measures framework to establish the effect of the intervention on (1) disclosure of participant’s HIV status to sexual partners; and (2) condom use for vaginal or anal sex. The HGLM method is an appropriate analysis when proportions are dependent variables, and this analysis can account for the non-independence of observations associated with longitudinal data (Raudenbush and Bryk 2002). As it is likely that individuals who disclosed (or used condoms) at a greater rate at baseline were more likely to disclose (or use condoms) at a subsequent time point, there should be a correlation within individual responses over time. The HGLM method accounts for the correlation between observations within an individual at different waves (baseline, 6, 12, 18 months) by incorporating a random effect in the model for each participant. Sensitivity analyses used different specifications for the within-individual correlation matrix and indicate that the reported results are robust (i.e., direction and significance of treatment effects are consistent across models). The parsimonious random intercept model is presented for ease of interpretation. An alpha level of 0.05 was used for all statistical tests.
The HGLM framework is appropriate for determining program impact when there is attrition in the study. HGLM will produce unbiased estimates of program impact if the data are considered to be missing at random (MAR) (Raudenbush and Bryk 2002). This is a reasonable assumption in a longitudinal study, where the probability of missing data is assumed to be related to the observed data (i.e., values for the independent and dependent variables collected during previous waves). This assumption is less conservative than the missing completely at random (MCAR) requirement for unbiased estimates according to generalized estimating equations (Hedeker and Gibbons 1997).
We controlled for a number of variables in each analysis to better understand the causal impact of the Protect and Respect intervention on reported risk behaviors. Participant race/ethnicity, age, years living with HIV/AIDS, HIV/AIDS acquisition route, relationship status, as well as indicators for treatment, wave (for each measurement occasion) and treatment × wave, were included in the analyses. Participant race/ethnicity and HIV/AIDS acquisition route were values calculated at baseline, while the other variables were allowed to change at each time point (i.e., a participant’s age would be higher at subsequent time points). The fixed effects of treatment, wave, and treatment × wave are the parameters of interest for establishing program impact estimates. Least squares means (predicted population margins) of the log odds of the outcome of interest were estimated for each arm of the intervention at each time point, based on the estimated model parameters. These log-odds were then transformed into predicted probabilities of a given event (with corresponding confidence intervals) for ease of interpretation, and the differences between the treatment group and the control group at each time point were compared as evidence of potential program impact.
Qualitative Measures
To gain a more in-depth understanding of the experiences of women who participated in the GLI and Peer groups, we conducted semi-structured interviews with a subsample (n = 18) of participants. Two trained RAs (both Black women) conducted the interviews at the PCCP. Interviews lasted ~1 h and were audio-taped. Interviewees received a $10 cash incentive. Sample questions from the study’s interview guide included: “What was the most important thing that you learned in the groups”?; “How did the groups affect your ability to have safe sex or disclose your HIV status to your sexual partners?” and “What made it hard to use the skills that you learned in the intervention?”
Qualitative Analyses
We transcribed the audio-taped interviews verbatim and edited the transcripts to remove identifiers. The first and fourth authors read the transcripts thoroughly multiple times to become acquainted with the data and developed a code book of key themes to guide analyses. We imported the data into Atlas.ti, a qualitative data analysis software package, and coded and analyzed the data using two strategies derived from Grounded Theory: coding and memo writing (Charmaz 2006). Coding progressed in two stages: initial and focused coding, followed by the discussion of the text that we had interpreted or coded differently until we reached 100% consensus (Charmaz 2006). We assessed the trustworthiness of our analyses as detailed in Bowleg et al. (2004).
Results
Quantitative Results
As indicated in Table 1, there were no statistically significant differences in the intervention and comparison groups at baseline. In Table 2, additional behavioral data are presented for the intervention and comparison groups at baseline, 6, 12, and 18 months. These behavioral indicators were used to create the outcome variables to establish the intervention’s impact. There were no statistically significant differences between the total number of partners or the number of partners to whom status was disclosed across the treatment and control groups at any time point. The intervention group, however, did disclose to a significantly greater number of partners (83.1%) at 6 months than the control group (61.0%, P < 0.05). The intervention group reported more condom use in months 6, 12 and 18, but these differences only approached statistical significance at the 0.05 level. These analyses suggest that there were differences in behavior across the treatment and control groups over time, but these results do not account for the longitudinal nature of the data nor attrition. In order to establish unbiased estimates of the program’s impact on these outcomes, it is necessary to utilize HGLM analysis which appropriately accounts for dropout and the longitudinal design.
The results of the HGLM multivariate analyses are presented in two separate tables for ease of interpretation. Table 3 indicates the parameter estimates for the comparison variables in each regression without presenting the time and treatment effects, along with their interactions, for ease of interpretation. With respect to partner disclosure, none of the covariates were statistically significant at the 0.05 level. Both of the infection route indicator variables approached statistical significance, however.
Some covariates were statistically significantly related to condom use in Table 3. Women who acquired AIDS from a HIV positive man were 94% less likely to use condoms than women who received AIDS from multiple (or other) sources (OR = 0.06; 95% CI = 0.02–0.23; P < 0.01). Women who were single were 73% less likely to use condoms than women who were separated/other (OR = 0.27; 95% CI = 0.13–0.58; P < 0.01). Also pertaining to relationship status, women who were in a committed relationship were 64% less likely to use condoms than women who were separated/other (OR = 0.36; 95% CI = 0.17–0.78; P < 0.01).
Table 4 includes the estimated log-odds and predicted proportions for each group at each time point, along with tests of the differences in these logits. These values were calculated as the least squares means (predicted population margins) for each of the time × treatment predictor variables. While the predicted proportion of disclosure increased at each wave for the treatment group, there was no statistically significant difference in disclosure rates at any point during the study between the intervention and comparison groups. With respect to condom use, the intervention group had significantly greater odds than the comparison group of reporting condom use during vaginal and anal sex in month 6 (adjusted OR = 17.13; 95% CI = 2.96–99.10; P < 0.01) and in month 18 (adjusted OR = 270.04; 95% CI = 24.53–2971.94; P < 0.01).
Qualitative Results
The interviewees’ responses about their intervention experiences stressed the effectiveness and value of the group aspect of the intervention. Below we describe two group-related themes, the importance of two types of groups and the open nature of the peer group, in further detail (see Teti et al. 2008 for a more in depth description of the group intervention experience). Interviewees’ narratives also centered on specific learning activities and/or topics that helped them disclose their HIV status or have safer sex, as well as challenges to changing these behaviors. Table 5 describes key demographics of the participants quoted in this section. Aliases are used to protect women’s confidentiality.
The Importance of Two Types of Groups: “You Can’t do one Without the Other”
Interviewees noted that they benefitted from the aims of each different group: (1) HIV/AIDS skills and education groups (GLI); and (2) peer-led support groups. Many perceived the GLI as an effective means of HIV prevention because it taught women about the clinical manifestations of HIV/AIDS as well as information about sexual risk taking. They noted that this was particularly important because many had entered the intervention with varying levels of education about HIV/AIDS and needed to have an equal knowledge base in order to discuss HIV in a group setting. For example, Paula said that the GLI was integral “because [the GLI sessions] teach you the ABC’s of HIV. You know, they break it down for you.”
Interviewees also described the peer support groups as effective in helping women to decrease their risk behaviors. Most cited the peer group leaders’ ability to empathize and personally relate to being a WLH/A as instrumental to group members’ reflections and critical thinking about their own safer sex behaviors. For example, Marlene said that it was important that the peer leaders “talked from experience” during the groups. Similarly, Leesa said that she valued the peers’ intimate knowledge of living with HIV/AIDS: “It’s all well and good to be a textbook teacher, but if you’ve been there, you can have a little more insight.”
The majority of the interviewees said that the groups in combination were the most effective means of helping them adopt safer sex behaviors. Alexa summarized the complementary aspect of the groups:
They both go together. You can’t do one without the other. You have to have both because I can’t just come into the support [groups because] you haven’t educated me [yet]…One [lady] came and she hadn’t went to [the GLI first] and you could see that she was lost. See, [the GLI] is where she needs to be first. She’s coming to a [bonded] group. We can only reach her so much and then we gonna scare here because she don’t know nothing about nothing. I can’t reach a person like that. You can not do one [group] without the other.
The Groups as the Women’s Space: “The Group is to Hear You”
Glenda summarized the thoughts of several interviewees when she said that being in the groups was the only time that she could be really free to express herself and thoughts. When asked what they liked best about learning in the groups, most women cited the openness of the peer group and acknowledged the importance of including various topics, such as relationships, violence, and mental health, and not just safe sex, in prevention groups for WLH/A. Likewise, the women also recommended that the groups not be limited to specific predetermined topics, but should be sufficiently flexible in design to accommodate concerns that participants brought to the group weekly. This was especially important, they noted, because often they had no other space where their needs were priorities.
The women said that it was important for prevention groups for women to cover “everything”, “nothing specific”, “what ever you feel like [or] whatever you gotta [do to] express yourself”, and “everything about the virus”. As Rochelle noted, it is important for groups to be a place where “everybody can say what they need to say.” Likewise, Alexa described the groups as successful because they were not just about HIV/AIDS but about the women’s lives. She said that a group might be the only place women had to cry, break down emotionally, and get support:
[The] group is to hear you, what you got to say, what you feeling, what you going through… [The group leaders] ask us what we want to learn about, what we want to talk about. Then they make [groups] out of [our input] and that’s good. See it’s not just about [them]. They ask about what we do in life, you know what I’m saying?
Group Facilitators and Social Barriers to HIV Status Disclosure
Many women said that the groups made them feel confident about disclosing their HIV status to others and handling others’ reactions. For example Talia noted that she could not control how others responded to her disclosure, but noted “at least I feel better when I talk about it [in group].” Specifically, sharing disclosure stories amongst themselves gave the group members ideas about how to disclose to others. Rochelle said they got disclosure “advice from each other’s experiences.” Marlene further explained that the group’s role-playing activities were key to her success: “[The group] helps a great deal. It tells you exactly how you go about telling someone, by role playing.”
Learning how to disclose did not always translate to actual disclosure, however. The women noted that they were generally very cautious about disclosure, and feared rejection or retaliating behaviors. Leesa spoke for the group when she said that she was reluctant to disclose because of previous hurtful reactions. For example Daisy explained that she told a family member who pressured her to keep it quiet. After that she said “I went back into my shell. [Now] I don’t be around nobody too much. I stay to myself.” Talia mentioned others’ ignorance and lack of acceptance as a barrier to her and other women’s disclosure success; Brenda agreed that “people just don’t understand.” Edie was so afraid that a partner would leave her that she said, “If I walk down the aisle and say ‘I do’ to [a] man, I’m still not going to tell him.” When asked about how the group affected her disclosure behaviors, Rochelle said that she was getting better at it, but that disclosure remained a challenge:
Disclosure to me is the hardest thing about having this disease. It’s not even that my CD4 count might be low, or [that] my viral load might be real low…The hardest thing for me to deal with is disclosure… I’m hoping to get better [at it].
Learning About and Problem-solving Barriers to Safe Sex
Many of the women conveyed the importance of the opportunity that the group afforded them to talk about sex with other WLH/A. Rita said that she did not realize that she could have sex and be safe before participating in the groups. The women cited role-plays and putting condoms on male and female models as effective and interactive ways to learn safe sex skills. In addition, they specifically described the benefit of sharing safe sex strategies amongst themselves. For example, many interviewees described a participant’s demonstration of how to use one’s mouth to put a condom on a man without his knowledge as the most important thing that they learned in the groups. Glenda said that the minute she saw the skill, she thought, “Oh no, I got to try that [with my boyfriend].” She recounted her success: “I’m getting busy with him. He says, ‘Let me put on a condom.’ I said, ‘You already have one on.’ He didn’t even know it. It works. You learn a lot [in the groups].”
Often, the most important information that women said that they realized in the groups was that prevention was not only about protecting their partners from HIV/AIDS, but was also important for their own health. They realized that STIs or re-infection with another strain of HIV could complicate their illness. For example, when asked if she had learned or thought differently about safe sex as a result of the intervention, Rochelle responded:
Yeah, yeah, yeah, yeah! When they told me I could be re-infected, that changed me a whole lot right there… I was in denial, truly in denial about it …And they was like ‘Hey, you need to take a look at this ‘cause this is real.”
Similarly, Paula captured the sentiments of many group members when she said that she learned that sex was still risky for her even if her partner was also HIV-infected: “[Before participating in the group] I thought, you know, [you’re] HIV positive, your partner’s HIV positive…and there is no way you could make anything worse.” Knowledge about the risks to themselves and not just their partners was another of the group’s important contributions.
The women also said that group helped them manage common barriers to having safe sex, namely their partners’ frequent negative attitudes about or unwillingness to use condoms. A few women discussed the challenge of accurately assessing their partner’s risk behaviors because they often misperceived that they were the only person with whom their partners were sexually active. Lorie recounted that prior to participating in the groups, she was nonchalant about unsafe sex, but now realized that it was prudent to use condoms because she could not be certain that her partner was monogamous. Many women talked about their struggles with how to respond to partners’ condom use resistance. Daisy, for example, opined that most men did not like to use condoms. Brenda said that her participation in the groups emboldened her to avoid partners who refused to use a condom even after her disclosure of her HIV status. Likewise, Tessa recalled that “One guy, he never wanted to use condoms, so I cut him off ‘cause I was scared for myself and him. So [the group helped] me [to do that].” These successful examples notwithstanding, a recurrent theme that most of the women articulated was that it was difficult to consistently integrate condom use into their sexual activities, primarily because they often had to negotiate condom use with reluctant partners.
Discussion
The Protect and Respect intervention included messages from HCPs, a five session GLI, and peer led support groups. Over 90% of participants were Black and Latina WLH/A. In light of the dearth of interventions focused on WLH/A’s specifically, one of the major contributions of this intervention study is its focus on the disclosure and condom use experiences of this population. Women who participated in the intervention (i.e., received safer sex messages from their HCPs, the GLI, and the peer support groups) were significantly more likely than those in the comparison group (i.e., those who received safer sex messages from HCPs only) to report using condoms for vaginal or anal sex in months 6 and 18. Consistent with the results of other interventions for people living with HIV/AIDS (Kalichman et al. 2001; Wingood et al. 2004) our findings suggest that behavioral interventions can help WLH/A adopt safer sex practices.
The ability of the intervention to increase WLH/A’s condom use at months 6 and 18 may have resulted from the intervention’s multiple and reinforcing safer sex messages from HCPs and two types of groups as well as the strong source of emotional support and ongoing education that the groups offered women as they integrated what they learned from the intervention into their lives and relationships. Our qualitative findings elaborated further on how the groups may have helped women to use condoms. First, the women said that the two types of groups provided education (GLI) and a space for the women to discuss what they learned and teach and support each other (peer led support groups). By delivering consistent but varied messages this approach may have given the women sufficient knowledge, support and confidence to change their sexual risk behaviors. Second, the women noted that the opportunity to share strategies in the groups also facilitated behavior change. For example, almost unanimously women cited learning how to use their mouths to put a condom on a man without his knowledge—a skill that the women learned from each other, not the intervention curriculum—as a very useful skill.
Third, the women said that they groups offered WLH/A safer sex strategies in an environment that also acknowledged and addressed the contexts in which their risk behaviors occurred. In other words, the groups provided a forum for women to discuss their lives and devise solutions for their risk practices. As such, these forums countered the common intervention practice of reducing WLH/A’s needs to a single medical diagnosis or risk behavior only (Morrow et al. 2001). Technically, specific behaviors such as unsafe sex transmit HIV. Pragmatically, these behaviors occur within a context of ecological factors (e.g., poverty, substance abuse, relationships with partners, etc.). Thus, interventions that fail to address the context of risk for WHL/A in favor of an individualistic risk behavior approach solely, are doomed to fail. Women bring their painful histories, lack of formal education opportunities, isolation, abusive partnerships, and myriad other life challenges that affect sexual decision making to interventions. They need a space to discuss their lives before they can successfully implement the skills that they have learned in the intervention.
Last, the women said that the groups helped to make them more aware that having safer sex was critical for their own health, not just that of their partners. Specifically, the women learned that having safer sex with partners of all HIV statuses (i.e., negative, positive, unknown) was important to protect them from STIs or other strains of HIV that could further compromise their health. Indeed, many women noted that group setting was the first in which they had learned that they needed to use condoms with their HIV positive partners.
Of note with these findings is also the fact that intervention participants were not only increasing their condom use, but they were increasingly having sex, relative to the comparison group. The comparison group decreased the average number of vaginal and anal sexual acts in the previous 6 month period from 24.10 at baseline to 9.38 by month 18, whereas the intervention participants actually increased their sexual activity from 11.45 acts to 35.75. This increase may have been due to a de-stigmatization of sexual activity, an important tenet of both the GLI and the peer groups, which encouraged women to talk openly about sex and how to make sex safe and fun.
The intervention had no effect on reports of HIV status disclosure to women’s sexual partners, however. While there was a statistically significant difference in the raw disclosure rates at month 6 of the intervention, this difference, and all other differences in disclosure rates were not evidenced as a statistically significant program impact in the HGLM analyses after controlling for other correlated factors. The HGLM results indicated that women in the intervention had increased their model-implied disclosure rate from 73% at baseline to 94% by month 18, whereas the control group had only increased their disclosure from 81% at baseline to 82% in month 18; differences in the disclosure rates were never statistically significant between the two groups at any time. Given the increasing trend in disclosure rates, however, and if additional follow-ups were conducted without an additional sample loss due to attrition, it is likely that a statistically significant difference in disclosure would have been found in future follow-ups.
Another possible reason why the disclosure variable was not associated with statistically significant differences may have been due to the way that the disclosure outcome variable was operationalized. In this study, we focused on partner disclosure in the aggregate, where all partners (i.e., HIV positive, HIV negative, and HIV status unknown) were treated similarly, independent of HIV status. Given our small sample sizes of sexually active women in the late data collection waves, we were unable to disentangle whether or not the intervention was effective in improving disclosure rates for women with certain HIV status partners (i.e., whether or not the intervention was associated with a significant impact for disclosure to HIV negative partners, but not a significant impact for HIV positive partners). Our inability to measure disclosure with sensitivity to partner type may have compromised our ability to detect statistically significant program impacts.
The qualitative findings failed to explain fully why the intervention affected women’s condom use, but not disclosure, although it is also possible that the intervention’s messages may have not been able to counter the risks and barriers associated with disclosing women’s HIV diagnosis. These barriers, which the women touched upon in the qualitative analysis, are significant and include abandonment (Maman and Medley 2004; Simbayi et al. 2007), stigma and discrimination (Maman and Medley 2004; Simbayi et al. 2007), and violence (Gielen et al. 2000).
Despite the study’s contributions to the intervention literature for WLH/A, the study had methodological limitations. We relied on self-reported outcome measures of stigmatized behaviors, and the participants may not have reported their behaviors honestly. Because messaging from HCPs was a standard of care in the clinic, there was no true control group for our intervention, limiting our ability to distinguish which specific part of the intervention was really affecting behavior change. The intervention as well as our data collection measures focused on heterosexual (i.e., condom use for sex with a man) risk behaviors only, even though 30% of the women reported that they were not heterosexual. As a result we missed the opportunity to meet these women’s prevention needs in the intervention and capture their sexual risk behaviors. We conducted qualitative interviews with only a subset (n = 18) of women who attended the group sessions, and their responses may not be representative of the views of all women in the intervention.
The greatest limitation of the study was our high attrition rates. Our efforts to retain women in the study using traditional means such as letters, phone calls, and linking research visits to women’s scheduled doctor visits at the clinic, did not prevent the precipitous decline in follow-up attendance (71% at 6 months to 30% at 18 months). The reasons for high attrition were likely similar to the challenges that we faced to enrolling high numbers of women. Our recruitment notes and records indicated that WLH/A said that they faced multiple challenges to coming into the clinic for medical or research appointments, including illness, fatigue, depression, drug and alcohol use, transportation and childcare barriers, and work conflicts. The decrease in effective sample size may have attenuated statistical power to detect the intervention’s effect on the study’s key outcomes. Given the nature of the intervention, however, and its predominant focus on safer sex, a larger effect was expected in the condom use outcome than in the disclosure outcome. The reduced sample size due to attrition may have been the reason why effects were only observed in the condom use outcome.
These limitations notwithstanding, our findings have important implications for interventions for WLH/A. Our findings suggested that the group intervention discussions allowing women to discuss psycho-social and social-structural issues, including their partners’ attitudes towards condoms, HIV/AIDS stigma, and fears of rejection and abandonment, are important to prevention. These barriers to disclosure and safer sex also highlighted the importance of addressing women’s partners’ and couples’ prevention needs. Our findings indicate that women can reduce their sexual risks, but the fact remains that neither condom use nor disclosure are solely under women’s control. Other socio-structural factors that were not fully addressed in this intervention but that have been suggested elsewhere as barriers to safer sex, such as poverty and/or gender and racial/ethnic inequality, are also important contextual influences to consider and address in HIV prevention programming (Diaz 2007; Dworkin and Ehrhardt 2007;Zierler and Krieger 1997). Our findings about the ability of Protect and Respect to increase protected sex among WLH/A are an important piece of the complex prevention puzzle for women.
References
Aidala, A. A., Lee, G., Garbers, S., & Chiasson, M. A. (2006). Sexual behaviors and sexual risk in a prospective cohort of HIV-positive men and women in New York City, 1994–2002: Implications for prevention. AIDS Education and Prevention, 18(1), 12–32. doi:10.1521/aeap.2006.18.1.12.
Amaro, H. (1995). Love, sex, and power: Considering women’s realities in HIV prevention. The American Psychologist, 50(6), 437–447. doi:10.1037/0003-066X.50.6.437.
Barkan, S. E., Melnick, S. L., Preston-Martin, S., Weber, K., Kalish, L. A., Miotti, P., et al. (1998). The women’s interagency HIV study. Epidemiology (Cambridge, Mass.), 9(2), 117–125. doi:10.1097/00001648-199803000-00004.
Bowleg, L., Lucas, K., & Tschann, J. (2004). “The ball was always in his court”: An exploratory analysis of relationship scripts, sexual scripts, and condom use among African American women. Psychology of Women Quarterly, 28, 70–82. doi:10.1111/j.1471-6402.2004.00124.x.
Centers for Disease Control and Prevention (CDC). (2008). HIV/AIDS among women. Retrieved September 1, 2008, from http://www.cdc.gov/hiv/topics/women/resources/factsheets/women.htm.
Charmaz, K. (2006). Constructing Grounded Theory, a practical guide through qualitative analysis. London: Sage.
Collins, C., Morin, S. F., Shriver, M., & Coates, T. J. (2000). Designing primary prevention for people living with HIV (policy monograph series). University of California, San Francisco: AIDS Policy and Research Center & Center for AIDS Prevention Studies.
Diaz, R. (2007). Impact on communities of color. National HIV Prevention Conference. Atlanta, GA.
DiClemente, R. J., Prochaska, J., & Gilbertini, M. (1985). Self-efficacy and the stages of change of smoking. Cognitive Therapy and Research, 9, 181–200. doi:10.1007/BF01204849.
Dworkin, S. L., & Ehrhardt, A. A. (2007). Going beyond “ABC” to “GEM”: Critical reflections on progress in the HIV/AIDS epidemic. American Journal of Public Health, 97(1), 13–18. doi:10.2105/AJPH.2005.074591.
Ehrhardt, A. A., Exner, T., Miller, S., & Stein, Z. (1992). Sexual risk behavior and behavior change in heterosexual women and men. New York: HIV Center for Clinical and Behavioral Studies at the New York Psychiatric Institute.
Fisher, J. D., Fisher, W. A., Cornman, D. H., Amico, R. K., Bryan, A., & Friedland, G. H. (2006). Clinician-delivered intervention during routine clinical care reduces unprotected sexual behavior among HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes, 41(1), 44–52. doi:10.1097/01.qai.0000192000.15777.5c.
Fogarty, L. A., Heilig, C. M., Armstrong, K., Cabral, R. J., Galavotti, C., Gielen, A. C., et al. (2001). Long-term effectiveness of a peer-based intervention to promote condom and contraceptive use among HIV-positive and at-risk women. Public Health Reports, 116(Supplement 1), S103–S119. doi:10.1093/phr/116.S1.103.
Gielen, A. C., Ghandour, R. M., Burke, J. G., Mahoney, P., McDonnell, K. A., & O’Campo, P. (2007). HIV/AIDS and intimate partner violence: Intersecting women’s health issues in the United States. Trauma, Violence & Abuse, 8(2), 178–198. doi:10.1177/1524838007301476.
Gielen, A. C., McDonnell, K. A., Burke, J. G., & O’Campo, P. (2000). Women’s lives after an HIV-positive diagnosis: Disclosure and violence. Maternal and Child Health Journal, 4(2), 111–120. doi:10.1023/A:1009522321240.
Gilbert, P., Ciccarone, D., Gansky, S. A., Bangsberg, D. R., Clanon, K., McPhee, S. J., et al. (2008). Interactive “video doctor” counseling reduces drug and sexual risk behaviors among HIV-positive patients in diverse outpatient settings. PLoS ONE, 3(4), e1988.
Golden, M., Wood, R. W., Buskin, S. E., Fleming, M., & Harrington, R. D. (2007). Ongoing risk behavior among persons with HIV in medical care. AIDS and Behavior, 11(5), 726–735. doi:10.1007/s10461-007-9244-5.
Hedeker, D., & Gibbons, R. (1997). Application of random effects pattern mixture models for missing data in social sciences. Psychological Methods, 2(1), 64–78. doi:10.1037/1082-989X.2.1.64.
Kalichman, S. C. (2004). Positive prevention, reducing HIV transmission among people living with HIV/AIDS. New York: Kluwer.
Kalichman, S. C., Rompa, D., Cage, M., DiFonzo, K., Simpson, D., Austin, J., et al. (2001). Effectiveness of an intervention to reduce HIV transmission risks in HIV-positive people. American Journal of Preventive Medicine, 21(2), 84–92. doi:10.1016/S0749-3797(01)00324-5.
Kvale, S. (1996). Interviews: An introduction to qualitative research interviewing. Thousand Oaks, CA: Sage.
Maman, S., & Medley, A. (2004). Gender dimensions of HIV status disclosure to sexual partners: Rates, barriers and outcomes. Geneva: World Health Organization.
Morrow, K., Costello, T., & Boland, R. J. (2001). Understanding the psychosocial needs of HIV-positive women: A qualitative study. Psychosomatics, 42(6), 497–503. doi:10.1176/appi.psy.42.6.497.
Patterson, T. L., Shaw, W., & Semple, S. (2003). Reducing the sexual risk behaviors of HIV-positive individuals: Outcomes of a randomized controlled trial. Annals of Behavioral Medicine, 25, 137–145. doi:10.1207/S15324796ABM2502_10.
Raudenbush, S. W., & Bryk, A. S. (2002). Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage.
Richardson, J. L., Milam, J., McCutchan, A., Stoyanoff, S., Boland, R. J., Weiss, J., et al. (2004). Effect of brief safer-sex counseling by medical providers to HIV-1 seropositive patients: A multi-clinic assessment. AIDS (London, England), 18, 1179–1186. doi:10.1097/00002030-200405210-00011.
Sandelowski, M., Lambe, C., & Barroso, J. (2004). Stigma in HIV-positive women. Journal of Nursing Scholarship, 36(2), 122–128. doi:10.1111/j.1547-5069.2004.04024.x.
Sikkema, K. J., Hansen, N. B., Kochman, A., Tarkeshwar, N., Nuefeld, S., Meade, C. S., et al. (2007). Outcomes from a group intervention for coping with HIV/AIDS and childhood sexual abuse: Reductions in traumatic stress. AIDS and Behavior, 11, 49–60. doi:10.1007/s10461-006-9149-8.
Simbayi, L. C., Kalichman, S. C., Strebel, A., Cloete, A., Henda, N., & Mqeketo, A. (2007). Disclosure of HIV status to sex partners and sexual risk behaviors among HIV-positive men and women, Cape Town, South Africa. Sexually Transmitted Infections, 83(1), 29–34. doi:10.1136/sti.2006.019893.
Teti, M., Bowleg, L., & Lloyd, L. (2008). “Don’t ever stop these groups”: The role of group interventions for women living with HIV/AIDS (manuscript submitted for publication).
Teti, M., Rubinstein, S., Lloyd, L., Aaron, E., Merron-Brainerd, J., Spencer, S., et al. (2007). The protect and respect program for women living with HIV/AIDS. AIDS and Behavior, 11(Suppl 1), 106–116. doi:10.1007/s10461-007-9275-y.
The Healthy Living Project Team. (2007). Effects of a behavioral intervention to reduce risk of transmission among people living with HIV: The healthy living project randomized controlled study. Journal of Acquired Immune Deficiency Syndromes, 44(2), 213–221. doi:10.1097/QAI.0b013e31802c0cae.
Wilson, T. E., Gore, M. E., Grange, S. J., Greenblatt, R., Cohen, M. H., Minkoff, H. L., et al. (2004). Changes in sexual behavior among HIV-infected women after initiation of HAART. American Journal of Public Health, 94(7), 1141–1146. doi:10.2105/AJPH.94.7.1141.
Wingood, G. M., & DiClemente, R. J. (2000). Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Education & Behavior, 27(5), 539–565. doi:10.1177/109019810002700502.
Wingood, G. M., DiClemente, R. J., Mikhail, I., Lang, D. L., McCree, D. H., Davis, S., et al. (2004). A randomized controlled trial to reduce HIV transmission risk behaviors and sexually transmitted diseases among women living with HIV. Journal of Acquired Immune Deficiency Syndromes, 37(Suppl 2), S58–S67. doi:10.1097/01.qai.0000140603.57478.a9.
Zierler, S., & Krieger, N. (1997). Reframing women’s risk: Social inequalities and HIV infection. Annual Review of Public Health, 18, 401. doi:10.1146/annurev.publhealth.18.1.401.
Acknowledgments
The authors give special thanks to their supportive collaborators at HRSA, EPPEC, the Partnership Comprehensive Care Practice, and the School of Public Health at Drexel University. We are especially grateful to all of the women who participated in Protect and Respect. This research was supported by grant number 03048 from the Health Resources and Services Administration (HRSA) special projects of national significance (SPNS) program. This publication’s content is solely the responsibility of the authors and do not represent the official view of HRSA or the SPNS program.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Teti, M., Bowleg, L., Cole, R. et al. A Mixed Methods Evaluation of the Effect of the Protect and Respect Intervention on the Condom Use and Disclosure Practices of Women Living with HIV/AIDS. AIDS Behav 14, 567–579 (2010). https://doi.org/10.1007/s10461-009-9562-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-009-9562-x