Abstract
We surveyed randomly selected patients in the largest HIV clinic in Seattle, WA in 2005 and 2006. A total of 397 patients completed usable surveys. Twenty-seven percent of men who have sex with men (MSM) and 22% of women or heterosexual men reported having non-concordant unprotected anal or vaginal intercourse in the preceding year. Compared to 2005, more MSM in 2006 reported meeting a sex partner via the Internet (15% vs. 33%), and fewer met partners in bathhouses (23% vs. 13%). Twenty-four percent of MSM reported deciding not to have sex with a potential partner because he was HIV negative, and 31% of MSM reported that another man had decided not to have sex with them because they were HIV positive. Among all participants, 22% had told a sex partner they were HIV negative since their HIV diagnosis. These findings demonstrate the persistence of high-risk behavior among persons with HIV, a rapid increase in the use of the Internet among MSM to find sex partners, and provide direct evidence for serosorting among MSM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Beginning in the late 1980s and early 1990s, studies conducted in sexually transmitted disease (STD) clinics began to draw attention to ongoing high risk sexual behavior and high rates of STDs among persons known to be HIV infected (Golden et al., 1996; Lee, Branan, Hoff, Datwyler, & Bayer, 1990; Osewe, Peterman, Ransom, Zaidi, & Wroten, 1996; Otten, Zaidi, Wroten, Witte, & Peterman, 1993; Zenilman, Erickson, Fox, Reichart, & Hook, 1992). More recently, the US Centers for Disease Control and Prevention (CDC) has emphasized the importance of integrating HIV prevention measures into routine HIV care (CDC, 2003; CDC 2004). Studies and behavioral surveillance programs have sought to define the magnitude of ongoing risk among persons previously diagnosed with HIV (Brewer, Golden, & Handsfield, 2006; CDC, 2004; Morin et al., 2005; Sullivan et al., 2005; Weinhardt et al., 2004; Wolitski, Parsons, & Gomez, 2004), and randomized controlled trials involving HIV infected persons have evaluated behavioral interventions designed to reduce HIV transmission (Crepaz et al., 2006; Gordon, Forsyth, Stall, & Cheever, 2005; Johnson, Carey, Chaudoir, & Reid, 2006).
However, to date, few prevention interventions for HIV infected persons have been widely implemented, and public health behavioral surveillance programs focusing on persons with HIV have been limited. Among HIV infected men who have sex with men (MSM), these efforts occur in the context of a rapidly changing sexual market place in which meeting sex partners over the Internet has become commonplace (Liau, Millett, & Marks, 2006), and serosorting, the practice of choosing partners or adopting different sexual behaviors based on a potential partner’s HIV status, may be increasing (Elford, Bolding, Sherr, & Hart, 2005).
Beginning in 2005, Public Health–Seattle & King County (PHSKC) initiated an on-going behavioral surveillance effort in the largest HIV clinic in the Pacific Northwest to assess the clinic’s ongoing prevention activities and to monitor sexual risk taking in the clinic’s patients. This program was envisioned as the first step in developing a wider prevention program for persons with HIV. In this paper, we present data from the first two years of this program.
Methods
Study Population
The study population was comprised of randomly selected patients with scheduled visits at the Harborview Medical Center (HMC) “Madison” (HIV) Clinic in Seattle, WA. HMC is a public hospital in King County, WA. The clinic provides HIV care to approximately 2,000 of the estimated 8,400 HIV infected persons in King County, WA.
We recruited two populations of 200 study participants, one during a 2-week time period in April 2005, and a second during a 2-week period in May 2006. Potential study participants were selected at the beginning of each day by enumerating all persons with scheduled appointments, and then using a random number table to select 50% of patients as potential recruits. We excluded persons who could not speak English as well as persons that clinic staff judged to be too ill to complete the survey. We also excluded persons if they had previously been seen in the clinic for a scheduled visit during the same year’s study period; this was done to avoid over-sampling persons with multiple visits during the 2-week study period.
Study Procedures
The study instrument was a three page, single-sided, self-administered survey composed of questions with multiple-choice and yes/no responses. Most questions were asked in an identical manner during both 2005 and 2006, however some questions related to serosorting and the Internet were asked only in 2006.
Although the survey instrument was designed to be self-administered, a small number of persons asked study staff to read the survey to them. The number of surveys that staff read to subjects was not specifically recorded, but staff believed this was done in fewer than 10 (5%) instances per year. To assure the anonymity of responses, participants were asked to seal completed surveys in a blank envelope and place them in a sealed box. Staff informed participants that envelopes would only be opened in groups of 10. We paid participants $5 for completing the survey, which took approximately 10 min.
Data Analysis
We conducted descriptive analyses of participants’ sexual behavior, substance use, and prevention-related interactions with clinic providers in the preceding year. Because all sexual history questions referred to the previous 12-month time period, we excluded 26 persons diagnosed with HIV in the preceding year to avoid the inclusion of behaviors that might have occurred prior to a subject’s HIV diagnosis. These persons were included in an analysis of a question that asked participants if they had ever misrepresented their HIV status to a partner; this question read, “Since you were diagnosed with HIV, have you ever told a sex partner that you were HIV negative?”
Analyses of sexual behavior focused on non-concordant unprotected anal intercourse (UAI) for MSM, and non-concordant unprotected anal or vaginal intercourse (UAVI) for heterosexuals. We defined non-concordant UAI and non-concordant UAVI as any unprotected anal or vaginal intercourse with an HIV negative partner or partner of unknown HIV status.
To assess the representativeness of the study population, we compared the study population’s age distribution, gender and sexual orientation to similar data included in a clinical database of all clinic patients in 2005 derived from hospital records. We compared the demographic characteristics of the populations recruited in 2005 and in 2006 to assure their similarity, and compared the sexual behaviors of these two populations to assess how sexual behavior might be changing over time. Because the sexual behavior of MSM and heterosexuals is often different, the sexual networks of these populations are substantially distinct, and interventions designed to control HIV in these populations may differ, we stratified our analysis of sexual behavior by gender and sexual orientation. We evaluated binary outcomes using logisitic regression and the χ 2 test, medians using a two-tailed Wilcoxon/Mann–Whitney test, and means using the t-test. We used logistic regression to develop a multivariate model using non-concordant UAI as an outcome. This model initially included all variables included in both the 2005 and 2006 surveys that were significantly associated with having non-concordant UAI on bivariate analysis; the final multivariate model was limited to variables found to have independent significant associations with non-concordant UAI (P < .05). We conducted all analyses using SAS.
Results
Study Population
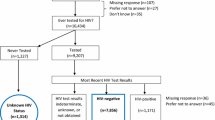
A total of 721 patients were selected for potential study participation, of whom 228 (32%) missed their appointment, 10 (1%) attended their appointment but were not approached by study staff, and five (0.5%) were too sick to participate. Of the remaining 478 potential participants, 78 (16%) declined to participate. Thus, the study enrolled 84% of approached patients, but only 56% of all persons defined as potential participants. Three participants left a question about their gender blank. These persons were excluded from further analysis.
The population was predominantly male (85%) and white (68%) (Table 1). The median age was 42 (range 20–67). Most participants had a high school education or less (61%) and earned <$15,000 per year (74%). Seventy-one percent of the entire clinic population, and 81% of male population identified as being gay or bisexual men. Almost half (48%) were infected with HIV for more than 10 years and nearly three quarters (74%) were taking antiretroviral medication. Comparing the populations recruited in 2005 and 2006, there were no statistically significant differences in any of the demographic characteristics presented in Table 1. Based on a comparison to data in a database of all clinic patients seen in 2005, the study population did not significantly differ from the overall clinic population with respect age, gender, or the proportion of the population composed of MSM (data not shown).
Sexual Behavior
Table 2 presents data on the sexual behavior and substance use of the 363 participants diagnosed with HIV more than 12 months prior to study participation, dividing the population into MSM (including bisexual men), heterosexual men, and women. (These data exclude 26 persons diagnosed with HIV within the preceding 12 months and three transgender persons.) Overall, 63% of MSM, 49% of heterosexual men, and 54% of women reported having any vaginal or anal sex in the preceding 12 months. Compared to women and to heterosexual men, MSM more often had multiple partners, and more often reported having unprotected anal or vaginal intercourse (UAVI) with an HIV-positive partner. On multivariate analysis, persons who reported engaging in any anal or vaginal sex were younger (OR 0.96, 95% CI 0.93–0.99 per year), more often Hispanic (OR 6.2, 95% CI 1.5–30.2), and more often reported using poppers (OR 8.6, 95% CI 3.3–22.7). Engaging in any anal or vaginal sex was not independently significantly associated with gender, sexual orientation, time since HIV diagnosis, race, use of antiretrovirals, or use of methamphetamine, heroin, crack, or cocaine.
Twenty-seven percent of MSM, 20% of heterosexual men, and 24% of women reported having non-concordant unprotected anal or vaginal intercourse (UAVI). These percentages were not significantly different, and similar proportions of MSM, heterosexual men and women reported always telling their partners their own HIV status and always knowing their partners’ status. However, among persons who reported any non-concordant UAVI, 9 (45%) of 20 heterosexual men and women vs. 10 (15%) of 66 MSM had only a single primary sex partner in the preceding year (OR 4.8, 95% CI 1.6–14.4). Regardless of gender or sexual orientation, among the 141 persons who reported having a primary partner, 138 (98%) indicated that their primary partner knew they were HIV positive. On bivariate analysis restricted to MSM who reported having anal sex in the preceding 12 months, non-concordant UAI was significantly associated with use of methamphetamine, cocaine, poppers, heroin, and drugs used to treat erectile dysfunction (ED); number of sex partners; and meeting a partner via the Internet or in a bathhouse (Table 3). Persons on antiretroviral drugs and those who reported always telling partners that they were HIV infected were less likely to report having non-concordant UAI. On multivariate analysis of data on MSM, having non-concordant UAI was associated with using poppers (OR 2.6, 95% CI 1.2–5.3), and inversely associated with always telling partners their HIV status (OR 0.36, 95% CI 0.17–0.74). Comparing the 2005 and 2006 samples of MSM, there were no significant differences in the percentage of patients who reported always telling partners their HIV status (63% vs. 65%, OR 1.1, 95% CI 0.63–1.8) or the percentage of persons who had non-concordant UAI (29% vs. 25%, OR 0.82, 95% CI 0.47–1.4) (Table 4).
Serosorting and Disclosure
Twenty-four percent of MSM reported that they had decided not to have sex with one or more potential partner in the preceding year because that potential partner was HIV negative, and 31% reported that a potential partner had decided not to have sex with them because they were HIV positive. These percentages were lower for heterosexual men and women, though differences were not statistically significant. Across all groups, 39 (22%) of 180 persons indicated that they had told a sex partner that they were HIV negative since being diagnosed with HIV. Compared to persons who reported never misrepresenting their HIV status to a sex partner, participants who misrepresented their HIV status less often reported always telling their partners their HIV status (OR 0.37, 95% CI 0.18–0.80), and more often reported that a partner had decided not to have sex with them because they were HIV positive (OR 2.2, 95% CI 0.96–5.0), though this later difference was not statistically significant. Misrepresenting one’s status to a partner was not significantly associated with participants’ number of partners, gender or sexual orientation, use of illegal drugs or drugs to treat erectile dysfunction, or time since the participant’s HIV diagnosis.
The Internet and Bathhouses as Venues to Meet Sex Partners
Among 180 MSM who reported having any anal sex in the preceding 12 months, 43 (24%) reported meeting a partner via the Internet and 37 (21%) met a partner in a bathhouse or sex club. Comparing the 2005 and 2006 populations, meeting partners via the Internet was significantly more common in 2006 (15% vs. 33%, OR 2.7 95% CI 1.3–5.6) and meeting partners in a bathhouse or sex club was significantly less common in 2006 (23% vs. 13%, OR 0.42 95% CI 0.20–0.91). The percentage of MSM who met partners through friends or family was similar during the two time periods (36% vs. 28%, OR 0.71, 95% CI 0.39–1.3). Participants in the 2006 survey were asked about home Internet access. Compared to 32 MSM without Internet access at home, the 55 MSM with home Internet access were more likely to meet partners over the Internet (49% vs. 6%, OR 14.5, 95% CI 3.1–66.5) and had more sex partners (median 3 vs. 1, P < 0.05, Wilcoxon/Mann–Whitney test), but were not significantly more likely to report having non-concordant UAI (51% vs. 37%, OR 1.8, 95% CI 0.89–3.6) or to say that they always told partners their HIV status (61% vs. 65%, OR 0.84, 95% CI 0.41–1.7). MSM with home Internet access were somewhat less likely to meet partners in a bathhouse or sex club (9% vs. 22%, OR 0.36 95% CI 0.10–1.2), though this difference was not significant. On multivariate analysis controlling for numbers of anal sex partners, MSM with home Internet access were significantly less likely to have met partners in a bathhouse (OR 0.09, 95% CI 0.02–0.55).
MSM subjects who met partners via the Internet were significantly more likely than those who did not meet partners via the Internet to have a potential partner decide not to have sex with them because of their HIV status (59% vs. 25%, OR 4.4, 95% CI 1.6–11.6), but not significantly more likely to report deciding not to have sex with a potential partner because that potential partner was HIV negative (39% vs. 29%, OR 1.6, 95% CI 0.61–4.1). The significant association between meeting partners via the Internet and having those potential partners decline sex with the participant persisted after adjustment for the participant’s number of sex partners. Among 62 MSM with home Internet access, only 6 (10%) thought the Internet prompted them to have more sex partners, while 41 (66%) thought it had no effect on their number of partners, and 15 (24%) thought it led them to have fewer partners.
Substance Use
Use of illegal drugs was common among all groups of patients, though patterns of substance use varied by sexual orientation. Methamphetamine was the most commonly used drug among MSM, heroin the most commonly used drug among heterosexual men, and crack cocaine the most commonly used drug among women. A total of 66 (25%) of 267 MSM reported using a drug to treat erectile dysfunction (ED) in the preceding year; only 22 (33%) of these men reported obtaining the ED medication from their HIV clinic provider, while an additional eight (12%) received the ED drug from another medical provider. Non-medical sources of ED drugs included friends (n = 21), sex partners (n = 20), the street (n = 5), and the Internet (n = 5). Eleven men (17%) of the 66 MSM who reported using ED drugs obtained from a non-medical source were also taking a protease inhibitor. Comparing 2005 and 2006, there was no significant change in the proportions of MSM who reported using an ED drug (23% vs. 27%, OR 1.2, 95% CI 0.71–2.2) or methamphetamine (30% vs. 34%, OR 1.2 95% CI 0.7–2.0).
Clinicians Discussions with Patients about Risk
Regardless of gender or sexual orientation, over half of patients reported that their provider had asked them about their sex life in the preceding year, and over 90% indicated that they were comfortable talking about sex and would bring concerns about sex up with their provider. Among the 268 persons who reported having any oral, anal or vaginal sex in the preceding year, 198 (79%) reported that their provider had asked them about sex (data were missing on 18), 168 (64%) reported that they had been tested for STDs (data were missing on six), and 67 (25%) indicated they had been treated for at least one STD. Questions regarding the content of clinicians’ discussions of sex and substance use were asked only in 2006. Although fewer than half of participants reported talking to their clinicians specifically about condom use, their partners’ HIV status, or their number of sex partners, persons who reported non-concordant UAI were more likely to indicate that they had spoken to their providers about condoms (54% vs. 28%, OR 3.1, 95% CI 1.6–6.3), numbers of sex partners (54% vs. 26%, OR 3.4, 95% CI 1.7–6.8), and their partner’s HIV status (50% vs. 26%, OR 2.9, 95% CI 1.4–5.9) than those who denied having non-concordant UAI.
Discussion
We serially surveyed patients in the largest HIV clinic in the Pacific Northwest of the United States to assess their ongoing sexual risk behaviors, and to gauge the extent to which clinicians talk to patients about these risks. We found that 25% of clinic patients had engaged in non-concordant UAI in the preceding year, with different patterns of risk behavior among MSM and heterosexuals. As in previous studies, we found that many clinicians did not discuss specific aspects with risk with patients (Marks et al., 2002; Morin et al., 2004), though clinicians appear to discuss sexual risks more often with patients who engaged in the highest risk.
Several of our epidemiologic observations merit comment. First, our findings provide new evidence regarding serosorting. Studies conducted since the early 1990s have consistently demonstrated that MSM preferentially have sex with men of the same HIV status (Dawson et al., 1994; Golden, Brewer, Kurth, Holmes, & Handsfield, 2004; Hoff et al., 1997; Koblin et al., 2003; Marks & Crepaz, 2001), a finding confirmed by analyses comparing observed mixing patterns to those anticipated if mixing were random with respect to HIV status(Cowen, Haff, & Smith, 2006; Golden, 2006). We found that approximately a quarter of MSM in our clinic had decided not to have sex with a potential partner in the last year because that potential partner was HIV negative; 31% had a potential partner decide not to have sex with them because they were HIV positive. Unfortunately, we also found that some HIV infected persons inaccurately told partners that they were HIV negative. We do not know how often this misreporting occurred in the context of unprotected sex, and this subject merits further study. However, our observation may partially explain previous observations that 15–30% of MSM with newly diagnosed HIV report having anal sex only with men who they believe to be HIV negative (Buchbinder et al., 2005; Golden, 2006; Koblin et al., 2006), and again illustrates the limits of serosorting as a prevention strategy.
Second, our findings demonstrate the dynamic nature of sexual behavior among MSM, and highlight the importance of the Internet as a factor that may be affecting MSM sexual behavior. Previous studies have shown that MSM who meet partners via the Internet have more partners (Benotsch, Kalichman, & Cage, 2002; Bolding, Davis, Hart, Sherr, & Elford, 2005; McFarlane, Bull, & Rietmeijer, 2000), but also suggested that partnerships formed via the Internet may be less risky (Bolding et al., 2005). Although our study populations in 2005 and 2006 were very similar in most respects, we observed a significant increase in the proportion of MSM who met partners via the Internet, and a decline in the proportion who met partners in bathhouses. The net impact of this change on the population’s risk profile is uncertain. Compared to MSM without home Internet access, MSM with such access were much more likely to meet partners online and had significantly more partners. Men who met partners via the Internet were not more likely to report always telling partners their HIV status than men who did not meet partners via the Internet. These factors suggest that the Internet could have increased the population’s risk. On the other hand, MSM who met partners via the Internet were less likely to meet partners in bathhouses, and were more likely to report that potential partners had elected not to have sex with them because of their HIV status. When specifically asked, men who met partners via the Internet did not believe the Internet had increased their number of partners. Overall, we observed no association between the occurrence of non-concordant UAI and having Internet access or meeting partners via the Internet. Thus, our findings provide somewhat conflicting evidence on how the Internet may affect serosorting and risk, and highlight the need for additional research on this complex topic.
Consistent with previous studies, we found that while the proportion of HIV positive persons who reported non-concordant UAI was similar for MSM and heterosexuals (Richardson et al., 2004; Weinhardt et al., 2004), the context of risk was very different. Among heterosexuals, almost half of persons who reported non-concordant UAI had only a single primary partner who was aware of their HIV status while only 15% of MSM who engaged in non-concordant UAI had a single primary partner. Knowing the different settings in which risky sexual practices occur should help clinicians to frame their discussions of risk reduction appropriately.
Most patients in our clinic reported that they were comfortable talking to their providers about sex, and over 80% of sexually active patients had done so in the preceding year. This is consistent with a study which found that 80% of Ryan White funded clinics, like ours, provide some type of risk reduction counseling (Valverde et al., 2004). However, as in previous studies (Marks et al., 2002; Morin et al., 2004; Myers et al., 2004), only a minority of patients reported discussing topics such as HIV status disclosure with providers. Our findings suggest that providers more frequently discuss sexual risks with persons who take more risk, but also demonstrate that there is a need for improvement in this area. We plan to use our observations regarding the frequency and content of provider/patient discussions of sexual behaviors as a benchmark to measure our clinic’s progress in implementing HIV prevention efforts.
Finally, our data demonstrate that a local public health department can conduct low-cost behavioral surveillance among persons with HIV. Similar behavioral data have previously been collected as part of research studies (Morin et al., 2005; Weinhardt et al., 2004), and CDC has developed a national behavioral surveillance system involving persons with HIV (CDC 2004; Sullivan et al., 2005). While this national effort will provide useful information, it will survey a relatively small number of metropolitan areas, the findings may be slow to reach local health departments and clinical providers, and the scale of such an effort may make it relatively inflexible. We believe that our approach complements this national surveillance system by providing locally accessible, timely data to guide and evaluate prevention efforts focusing on persons with HIV, and to monitor the dynamic sexual behavioral risks taken by HIV infected patients. Moreover, our approach is simple and inexpensive; all surveys were distributed by a single public health worker over a 1–2 week period per year and survey development, analysis and data management were provided by existing HIV clinic and STD program staff. The self-administered questionnaire was highly acceptable to patients, easily incorporated new questions, and preliminary results were available within weeks of the survey being completed.
The generlizability of our findings may be limited by our study’s small size and inclusion of patients from only a single HIV clinic that is more likely to see the uninsured and socially disadvantaged. However, the overall level of non-concordant UAI we observed among MSM (28%), is very similar to that observed in a 2003 random digit dial study of Seattle MSM (32%) (Brewer et al., 2006), suggesting that at least one of our central findings is representative of the larger local MSM population. Moreover, the patterns of risk we observed comparing heterosexuals and MSM are comparable to those found in much larger studies (Richardson et al., 2004). Since our survey did not include questions about behavior with specific partners or about specific sexual events, we could not compare partnerships or conduct event level analyses. Our findings were further limited by missing data, particularly regarding drug use. Instruments collecting egocentric sexual network data via computer self-interviews would improve the collected data, but would entail additional costs, added complexity and a potential loss in flexibility. Finally, we relied on patient self-reports, and some of the information participants provided may be inaccurate.
In summary, we found that 25% of HIV infected patients in the largest HIV clinic in the Pacific Northwest of the US engaged in non-concordant UAVI in the preceding year, and that patterns of risk observed in heterosexuals and MSM varied. MSM had more partners and displayed substantial serosorting, while heterosexuals were more likely to expose partners to HIV in the context of primary monogamous relationships. Over a single year, we observed a significant increase in MSM’s use of the Internet to find sex partners, though the implications of that change remain uncertain. Clinicians frequently discussed ongoing sexual risk behaviors with patients, but the content of those discussions often omitted key aspects of risk. Although prevention programs focusing on persons with HIV are not yet widespread, our experience demonstrates that locally conducted surveillance among HIV infected persons is feasible, and that data from such efforts may be useful in informing public health programs and in alerting clinicians to the need to devote additional energy to prevention.
References
Benotsch, E. G., Kalichman, S., & Cage, M. (2002). Men who have met sex partners via the Internet: Prevalence, predictors, and implications for HIV prevention. Archives of Sexual Behavior, 31(2), 177–183.
Bolding, G., Davis, M., Hart, G., Sherr, L., & Elford, J. (2005). Gay men who look for sex on the Internet: Is there more HIV/STI risk with online partners? AIDS, 19(9), 961–968.
Brewer, D. D., Golden, M. R., & Handsfield, H. H. (2006). Unsafe sexual behavior and correlates of risk in a probability sample of men who have sex with men in the era of highly active antiretroviral therapy. Sexually Transmitted Diseases, 33(4), 250–255.
Buchbinder, S. P., Vittinghoff, E., Heagerty, P. J., Celum, C. L., Seage, G. R. 3rd, Judson, F. N., et al. (2005). Sexual risk, nitrite inhalant use, and lack of circumcision associated with HIV seroconversion in men who have sex with men in the United States. Journal of the Acquired Immune Deficiency Syndrome, 39(1), 82–89.
CDC. (2003). Advancing HIV prevention: New strategies for a changing epidemic. Morbidity and Mortality Weekly Report, 52(15), 1–4.
CDC. (2004). Recommendations for incorporating human immunodeficiency virus (HIV) prevention into the medical care of persons living with HIV. Clinical Infectious Diseases, 38(1), 104–121.
CDC. (2004). High-risk sexual behavior by HIV-positive men who have sex with men-16 sites, United States, 2000–2002. Morbidity and Mortality Weekly Report, 53(38), 891–894.
Cowen, S., Haff, J., & Smith, E. (2006). Serosorting–On Purpose or By Chance. Paper presented at the XVI International AIDS Conference, Toronto, Canada.
Crepaz, N., Horn, A. K., Rama, S. M., Griffin, T., Deluca, J. B., Mullins, M. M. et al. (2006). The efficacy of behavioral interventions in reducing hiv risk sex behaviors and incident sexually transmitted disease in black and hispanic sexually transmitted disease clinic patients in the United States: A meta-analytic review. Sexually Transmitted Diseases.
Dawson, J. M., Fitzpatrick, R. M., Reeves, G., Boulton, M., McLean, J., Hart, G. J., et al. (1994). Awareness of sexual partners’ HIV status as an influence upon high-risk sexual behaviour among gay men. AIDS, 8(6), 837–841.
Elford, J., Bolding, G., Sherr, L., & Hart, G. (2005). High-risk sexual behaviour among London gay men: No longer increasing. AIDS, 19(18), 2171–2174.
Golden, M. R. (2006). HIV Serosorting Among Men Who Have Sex with Men: Implications for Prevention. Paper presented at the 13th Conference on Retroviruses and Opportunistic Infections 2006, Denver, CO.
Golden, M. R., Brewer, D. D., Kurth, A., Holmes, K. K., & Handsfield, H. H. (2004). Importance of sex partner HIV status in HIV risk assessment among men who have sex with men. Journal of the Acquired Immune Deficiency Syndrome, 36(2), 734–742.
Golden, M. R., Rompalo, A. M., Fantry, L., Bein, M., Perkins, T., Hoover, D. R., et al. (1996). Early intervention for human immunodeficiency virus in Baltimore Sexually Transmitted Diseases Clinics. Impact on gonorrhea incidence in patients infected with HIV. Sexually Transmitted Diseases, 23(5), 370–377.
Gordon, C. M., Forsyth, A. D., Stall, R., & Cheever, L. W. (2005). Prevention interventions with persons living with HIV/AIDS: State of the science and future directions. AIDS Education and Prevention, 17(1 Suppl A), 6–20.
Hoff, C. C., Stall, R., Paul, J., Acree, M., Daigle, D., Phillips, K., et al. (1997). Differences in sexual behavior among HIV discordant and concordant gay men in primary relationships. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology, 14(1), 72–78.
Johnson, B. T., Carey, M. P., Chaudoir, S. R., & Reid, A. E. (2006). Sexual risk reduction for persons living with HIV: Research synthesis of randomized controlled trials, 1993 to 2004. Journal of the Acquired Immune Deficiency Syndrome, 41(5), 642–650.
Koblin, B. A., Chesney, M. A., Husnik, M. J., Bozeman, S., Celum, C. L., Buchbinder, S., et al. (2003). High-risk behaviors among men who have sex with men in 6 US cities: Baseline data from the EXPLORE Study. Amican Journal of Public Health, 93(6), 926–932.
Koblin, B. A., Husnik, M. J., Colfax, G., Huang, Y., Madison, M., Mayer, K., et al. (2006). Risk factors for HIV infection among men who have sex with men. AIDS, 20(5), 731–739.
Lee, J. H., Branan, L., Hoff, G. L., Datwyler, M. L., & Bayer, W. L. (1990). Voluntary human immunodeficiency virus testing, recidivism, partner notification, and sero-prevalence in a sexually transmitted disease clinic: A need for mandatory testing. Sexually Transmitted Diseases, 17(4), 169–174.
Liau, A., Millett, G., & Marks, G. (2006). Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sexually Transmitted Diseases, 33(9), 576–584.
Marks, G., & Crepaz, N. (2001). HIV-positive men’s sexual practices in the context of self-disclosure of HIV status. Journal of the Acquired Immune Deficiency Syndrome, 27(1), 79–85.
Marks, G., Richardson, J. L., Crepaz, N., Stoyanoff, S., Milam, J., Kemper, C., et al. (2002). Are HIV care providers talking with patients about safer sex and disclosure?: A multi-clinic assessment. AIDS, 16(14), 1953–1957.
McFarlane, M., Bull, S. S., & Rietmeijer, C. A. (2000). The Internet as a newly emerging risk environment for sexually transmitted diseases. Journal of the American Medical Association, 284(4), 443–446.
Morin, S. F., Koester, K. A., Steward, W. T., Maiorana, A., McLaughlin, M., Myers, J. J., et al. (2004). Missed opportunities: Prevention with HIV-infected patients in clinical care settings. Journal of the Acquired Immune Deficiency Syndrome, 36(4), 960–966.
Morin, S. F., Steward, W. T., Charlebois, E. D., Remien, R. H., Pinkerton, S. D., Johnson, M. O., et al. (2005). Predicting HIV transmission risk among HIV-infected men who have sex with men: Findings from the healthy living project. Journal of the Acquired Immune Deficiency Syndrome, 40(2), 226–235.
Myers, J. J., Steward, W. T., Charlebois, E., Koester, K. A., Maiorana, A., & Morin, S. F. (2004). Written clinic procedures enhance delivery of HIV “prevention with positives” counseling in primary health care settings. Journal of the Acquired Immune Deficiency Syndrome, 37(Suppl 2), S95–S100.
Osewe, P. L., Peterman, T. A., Ransom, R. L., Zaidi, A. A., & Wroten, J. E. (1996). Trends in the acquisition of sexually transmitted diseases among HIV-positive patients at STD clinics, Miami 1988–1992. Sexually Transmitted Diseases, 23(3), 230–233.
Otten, M. W., Jr., Zaidi, A. A., Wroten, J. E., Witte, J. J., & Peterman, T. A. (1993). Changes in sexually transmitted disease rates after HIV testing and posttest counseling, Miami, 1988 to 1989. American Journal of Public Health, 83(4), 529–533.
Richardson, J. L., Milam, J., Stoyanoff, S., Kemper, C., Bolan, R., Larsen, R. A., et al. (2004). Using patient risk indicators to plan prevention strategies in the clinical care setting. Journal of the Acquired Immune Deficiency Syndrome, 37(Suppl 2), S88–S94.
Sullivan, P. S., Karon, J. M., Malitz, F. E., Broyles, S., Mokotoff, E. D., Buskin, S. E., et al. (2005). A two-stage sampling method for clinical surveillance of individuals in care for HIV infection in the United States. Public Health Reports, 120(3), 230–239.
Valverde, E., Del Rio, C., Metsch, L., Anderson-Mahoney, P., Krawczyk, C. S., Gooden, L., et al. (2004). Characteristics of Ryan White and non-Ryan White funded HIV medical care facilities across four metropolitan areas: Results from the Antiretroviral Treatment and Access Studies site survey. AIDS Care, 16(7), 841–850.
Weinhardt, L. S., Kelly, J. A., Brondino, M. J., Rotheram-Borus, M. J., Kirshenbaum, S. B., Chesney, M. A., et al. (2004). HIV transmission risk behavior among men and women living with HIV in 4 cities in the United States. Journal of the Acquired Immune Deficiency Syndrome, 36(5), 1057–1066.
Wolitski, R. J., Parsons, J. T., & Gomez, C. A. (2004). Prevention with HIV-seropositive men who have sex with men: Lessons from the Seropositive Urban Men’s Study (SUMS) and the Seropositive Urban Men’s Intervention Trial (SUMIT). Journal of the Acquired Immune Deficiency Syndrome, 37( Suppl 2), S101–109.
Zenilman, J. M., Erickson, B., Fox, R., Reichart, C. A., & Hook, E. W. 3rd. (1992). Effect of HIV posttest counseling on STD incidence. Journal of the American Medical Association, 267(6), 843–845.
Acknowledgements
The authors thank Carol Glen for assistance recruiting study participants. Dr. Golden was supported by NIH K23 AI01846.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Golden, M.R., Wood, R.W., Buskin, S.E. et al. Ongoing Risk Behavior Among Persons With HIV in Medical Care. AIDS Behav 11, 726–735 (2007). https://doi.org/10.1007/s10461-007-9244-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-007-9244-5