Abstract
Women experiencing homelessness are at heightened risk for HIV, yet risk reduction interventions specifically designed for this population are lacking. This study reports on a pilot efficacy trial of a brief evidence-based intervention, Sister To Sister (STS), that we specifically adapted for homeless women in the temporary/emergency settings where they typically seek services. Seventy-nine women, recruited from three service sites in Los Angeles County, were assigned to the 40-min adapted STS intervention or an information-only control group. At 30-day follow-up, intervention participants reported significantly greater condom use, intentions to use condoms, and sexual impulse control (as well as marginally higher positive condom beliefs and condom self-efficacy) compared to control participants. Results provide preliminary evidence that HIV risk reduction can be achieved for homeless women through a brief skill-based intervention. A randomized controlled trial employing a longer follow-up period to monitor outcomes will be necessary to determine efficacy of the adapted intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Eighty-four percent of new HIV infections among women in the USA are attributable to unprotected heterosexual intercourse (Centers for Disease Control [CDC] 2014a, b). Other than complete abstinence, correct and consistent condom use remains the most effective means of preventing the sexual transmission of HIV to women (DiClemente et al. 2008); thus, sexual risk reduction remains a priority in reducing incidence of HIV as well as other sexually transmitted infections (STIs) (US Department of Health and Human Services 2010). HIV disproportionately impacts persons who are poor. In a recent study involving 23 US cities, poverty level and homelessness emerged as significant predictors of HIV prevalence (Dennin and DiNenno 2014).
Homeless women face health risks including HIV and drug use (Caton et al. 2013; Cederbaum et al. 2013; Wenzel et al. 2004). Homeless women are more likely to engage in sexual risk behaviors and are at greater risk of contracting HIV than poor, housed women (Caton et al. 2013; Riley et al. 2007), and more likely to have multiple partners and less likely to use condoms with casual partners (German and Latkin 2012; Wenzel et al. 2004).
Behavioral HIV Risk Reduction Intervention is Effective
A meta-analytic synthesis of behavioral intervention studies highlights the long-term effectiveness of interventions for increasing condom use and subsequently reducing incidence of HIV and other STIs, especially of those tailored for and delivered to women (Scott-Sheldon et al. 2011). Program characteristics associated with effective HIV sexual risk reduction for women include gender specificity, skill-building demonstrations and exercises, and sufficient program intensity (i.e. multiple sessions; Campbell et al. 2011). Woman-focused HIV interventions have also been effective in reducing substance use, specifically crack use (Wechsberg et al. 2004). Gender specificity and skill-building components may be desirable and relevant for homeless women, but multiple session-interventions may be challenging for women who are transient.
Behavioral HIV Risk Reduction for Homeless Women
Although behavioral interventions have been found to reduce HIV risk among vulnerable populations such as Black women (Crepaz et al. 2009; Scott-Sheldon et al. 2011), no HIV risk reduction intervention has focused specifically on unique needs of women experiencing homelessness and the attendant challenges of transiency, pre-occupation with satisfying subsistence needs, limited access to health service providers, higher rates of drug use, and health risks (Thomas et al. 2006). The Diffusion of Effective Behavioral Interventions (DEBI) initiative (CDC 2009) has been the major means through which the CDC has attempted to disseminate interventions to affected communities across the USA. None of these interventions, however, is specifically designed for homeless women and, to the best of our knowledge, existing interventions have not been adapted for this population and translated into routine practice in settings frequented by these women.
Interventions may need to be modified and adapted for different populations and settings to maximize effectiveness (Barrera et al. 2013; Cederbaum et al. 2014). Consideration must be given to delivering HIV prevention services in non-traditional settings frequented by homeless women. Implementation of evidence-based interventions in community settings is also affected by providers’ resource capabilities and limitations and the match between researcher and provider preferences (Cunningham and Card 2014). Both the target population and providers should be involved in selection of an intervention and adaptation to ensure relevance, feasibility, and sustainability (Durlak and DuPre 2008; McKleroy et al. 2006).
Adaptation of Sister to Sister for Homeless Women
As reported elsewhere (Cederbaum et al. 2014), using the CDC MAP (McKleroy et al. 2006) and ADAPT-ITT (Wingood and DiClemente 2008) models for adapting HIV prevention EBIs for new target populations and settings, we collaboratively and systematically engaged service providers and homeless women in selecting and adapting an EBI available through DEBI. The EBI selected for adaption was Sister To Sister, a brief, one-on-one skill-based HIV/STI risk reduction intervention (Jemmott et al. 2007; O’Leary et al. 2008). The intervention was designed to increase condom negotiation and condom use with sex partners and to enhance women’s understanding of their risk, as well as influence their beliefs, motivation, and self-efficacy in making behavioral changes (Jemmott et al. 2007). The intervention was demonstrated to be efficacious in increasing condom use for women through 12-month follow-up, relative to a brief information-only condition, and 200-min group interventions that were either information-only or skill-based (Jemmott et al. 2007). One highlighted advantage of Sister To Sister was brevity, an advantageous characteristic for a transitory population receiving intermittent and largely subsistence services at shelters and drop-in centers (Cederbaum et al. 2014).
Sister To Sister is grounded in health behavior theories (Ajzen and Fishbein 2005; Jemmott et al. 2008). Specifically, in terms of social cognitive theory (McAliser et al. 2008), attitudinal changes or proximal outcomes of an intervention are posited to explain behavioral changes achieved through the intervention. Self-efficacy in condom use (i.e., putting a condom on a partner, persuading a partner to use a condom) is considered an important path through which Sister To Sister accomplishes behavioral change from a social cognitive perspective, and was the most important mediator explaining the effect of Sister To Sister on condom use (O’Leary et al. 2008). Given that homeless women are particularly affected by substance use, efficacy in negotiating condom use under the influence may be valuable. In accordance with health behavior theories, specifically the theory of reasoned action (Ajzen et al. 2007), intention to use condoms has been a consistent predictor of use (Crosby et al. 2013; Webb and Sheeran 2006) and is reflected in Sister To Sister (Jemmott et al. 2008). Sexual impulse control and hedonistic beliefs about condoms have also been investigated as attitudinal mechanisms through which Sister To Sister may affect behavioral change in condom use (O’Leary et al. 2008). Because theory-based mechanisms of change guide the specific activities of interventions (Jemmott et al. 2008), these elements were preserved in our adaptation.
Present Study
The present study reports on results of a pilot efficacy trial of the adapted Sister To Sister intervention for homeless women. Women participating in the intervention were hypothesized to engage in more condom use relative to women in an information-only control condition during a 30-day follow-up period. We also hypothesized that women participating in the intervention would report greater self-efficacy regarding condom use, more favorable beliefs about condoms, greater sexual impulse control, and greater intentions to use condoms compared to women in the information-only control condition. We also report on the feasibility and acceptability of the adapted intervention. To our knowledge, this is the first test of the efficacy of an HIV/STI risk reduction intervention that has been adapted for women experiencing homelessness.
Methods
Study Design
We pilot tested the adapted HIV risk reduction intervention in three organizations that provide temporary (emergency) shelter, drop-in, and meal services to homeless women in Los Angeles County between February 2014 and May 2014. Sites were located in South Los Angeles, downtown Los Angeles, and Pasadena, thus providing reasonable generalizability of findings for this small pilot test. Although the randomized controlled trial is the gold standard in achieving internal validity and causal inference regarding treatment effects, we determined that a quasi-experimental design was the most feasible approach for this pilot study due to limitations in project staffing and initial concerns about contamination across study conditions in an individually randomized trial. In this design, both the intervention and control conditions were offered in each of the three sites. We first recruited participants for the control condition at each of the three sites. Once enrollment for the control condition was completed, and after a 30-day “clean out” period to allow for client turnover, we recruited participants for the intervention condition at each site. Any given participant, therefore, was “assigned” to either the comparison or intervention condition by virtue of where and when she happened to be seeking services.
Participants and Procedures
Eligibility criteria for the study were as follows: (1) age 18 or older, (2) having had either vaginal or anal sex with a man in the past 30 days, (3) having had any unprotected sex (i.e., without a condom) in the past 30 days, (4) an expectation of having sex with a man at least once in the next 30 days, and (5) English speaking ability. Eligibility screening was completed with a total of 121 women. The major reason for ineligibility and thus exclusion from the study was not having had sex with a man in the past 30 days (N = 27; 22.3 %).
Participants were 79 women (N = 40 in intervention; N = 39 in control) who were determined to be eligible, consented to participate, and completed the baseline (pre-test) interview. Women were recruited on a voluntary basis. In coordination with staff at each site, the study team determined days and times during which study team members would visit the site to recruit and screen women for eligibility. One day prior to the appointed day of the study at each site, study staff posted a descriptive flyer about the study and a sign-up sheet. Upon arrival the next day, study staff took the sign-up sheet, announced their presence, and began screening in the order indicated on the sign-up sheet. Screening, consent, baseline survey, and intervention or control activities all occurred on the same day. Screening, consent, and surveys were administered by different study team members than those who served as intervention facilitators.
All activities involving participants, starting with eligibility screening and through the 30-day follow-up survey, were conducted one-on-one with a study team member. After administering the paper-and-pencil survey, a study member assisted each woman in completing a “contact and locator form” to assist the team in contacting the woman for the 30-day follow-up survey. Women were paid US$30 for participation in the baseline survey and were then escorted to a private space where a trained facilitator completed the intervention or control condition protocol. Finally, each woman was provided with a packet of information including a follow-up reminder card with a study coordinator’s phone number, male and female condoms, a one-page HIV information sheet, and a two-page resource guide containing information on local services (HIV testing, condom distribution, substance use treatment, needle exchanges, and intimate partner violence service organizations). Approximately 3 weeks from date of baseline, a study member attempted to contact the woman to schedule the follow-up survey. The majority of follow-up surveys were conducted at the site at which the baseline was conducted; other sites included nearby coffee shops and homeless service agencies. Women were paid US$35 for participation in the follow-up survey. Trained study staff conducted all study activities. All procedures were approved by the University of Southern California and RAND Corporation institutional review boards. A Certificate of Confidentiality was obtained.
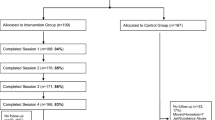
A CONSORT diagram is provided in Fig. 1. A total of 79 women out of 81 eligible completed the baseline interview, with 1 woman in each of the two study arms unable to complete the baseline due to cognitive impairment. Retention at 30 days post-baseline was 84.6 % (N = 33) in the control condition and 77.5 % (N = 31) in the intervention condition; an overall 30-day retention rate and follow-up survey completion rate of 79 % (N = 64). The primary reason for attrition in both conditions was the inability to contact women for follow-up despite our efforts to collect detailed contact and locator information from all women at baseline.
Study Conditions
Control Condition
The control condition was an information-only condition. Women who participated in the control condition received a 10-min, one-on-one intervention in which the facilitator provided the participant with a two-page resource guide that included information on where to access (1) free condoms, (2) free HIV testing, (3) substance use treatment services, (4) needle exchanges, (5) domestic violence services, and (6) HIV education/prevention hotlines. Women were also provided with an information sheet on how HIV is transmitted and ways to prevent acquiring HIV. A standardized script was used to guide the facilitator’s presentation and description of the resource guide and HIV information sheet. For example, the facilitator was instructed to open the resource guide and point out the kinds of services available and of potential interest for use to women. In reviewing the HIV information sheet, the facilitator named some of the ways in which HIV could be transmitted (e.g., unprotected sex), and some of the ways in which HIV transmission could be prevented (e.g., use of condoms). Last, women were provided with male and female condoms and a reminder card for the follow-up survey.
Intervention Condition
As detailed elsewhere (Cederbaum et al. 2014), the study team used structured techniques (i.e., focus groups, consensus groups, and interviews) to engage homeless women and service providers in the selection and adaptation of Sister To Sister, an evidence-based, woman-specific intervention from the Center for Disease Control’s DEBI website. Intervention facilitators were trained on the original Sister To Sister curriculum by master trainers; these trainers also provided advice and input on integrating and implementing adaptations to the established curriculum.
Sister To Sister is a brief, one-on-one skill-based HIV/STI risk reduction intervention originally designed for sexually active Black women to be delivered in health care settings (e.g., STI clinics) by nurses, health educators, or social workers (Jemmott et al. 2007). The intervention was designed to increase skills in condom use and negotiating condom use with sex partners, and to enhance women’s understanding of their risk, as well as their beliefs, motivations, and confidence in making behavioral changes (Jemmott et al. 2007). Materials and activities include an informational brochure, video clips, condom use demonstration, condom application practice opportunity with an anatomical model, and role plays (Jemmott et al. 2007).
In the current study, women who participated in the intervention engaged in a 40-min, one-on-one adapted version of Sister To Sister (Jemmott et al. 2007). Adaptations were based on interaction and feedback received from homeless women and providers (Cederbaum et al. 2014). We made no changes to the original theory-driven core elements; for example, we retained building confidence and behavioral skills in male condom use and in negotiating condom use.
Major modifications to Sister To Sister that we had made in collaboration with homeless women and providers included the following: (1) addition of female condom discussion, video clip, demonstration, and skill-building opportunity using an anatomical model; (2) emphasis on woman’s safety throughout the curriculum (e.g., “You are the best person to judge your own situation, and your physical safety should be the first priority. It is not a personal failure if you cannot use condoms when facing a serious risk to your personal safety”) and inclusion of information on resources (e.g., hotlines) for women experiencing intimate partner violence; (3) inclusion of information on substance use and sexual risk (in addition to IDU), including information on substance use treatment resources in Los Angeles; (4) updating and tailoring of information on HIV statistics to the Los Angeles area, and including information on HIV testing resources in Los Angeles; and (5) inclusion of information on locations to access free male and female condoms in Los Angeles. The curriculum was also thoroughly edited, for example, to remove references to the clinic setting as the site of intervention delivery, and to ensure that words and sentences were accessible and respectful of women experiencing homelessness.
Finally, we provided the following: (1) a separate resource guide inclusive of services available at no-cost or low-cost to women experiencing homelessness in Los Angeles (e.g., substance use treatment, condoms, HIV testing); (2) an information sheet regarding HIV transmission and protection; (3) male and female condoms; and (4) a reminder card for the follow-up survey.
Measures
Participants in the intervention and control conditions completed structured baseline and 30-day follow-up surveys administered by study staff. Each survey was 30 min in length. Participants in the intervention condition additionally completed a post-intervention feedback questionnaire as a measure of feasibility and acceptability of the intervention.
Demographic and Background Characteristics at Baseline
These included questions used in previous studies involving homeless women (Kennedy et al. 2010). Demographics included age, race\ and ethnicity, education (highest year or grade in school), current marital status, employment status, and past 30-day income. We additionally asked how much time women had spent homeless in the past 6 months and whether women had ever previously attended an HIV or AIDS education program.
Behavioral Outcomes
Outcomes included proportion of vaginal or anal sex acts in the past 30 days in which a male or female condom was used, and whether a male or female condom was used the last time women had vaginal or anal sex in the past 30 days (Jemmott et al. 2007; O’Leary et al. 2008). Condom use was self-reported. The first outcome was derived from three items referencing the past 30 days: (1) how many times the woman had vaginal or anal sex, (2) how many times a male condom was used when she had sex, and (3) how many times a female condom was used. Proportion was calculated by dividing number of times a condom was used (male + female) by number of times one had sex.
Attitudinal Outcomes
Condom self-efficacy was assessed with the 15-item Condom Self-Efficacy Scale (CUSES) (Barkley and Burns 2000), which includes efficacy in the mechanics of putting on a condom (e.g., “confident in my ability to put on a condom”), in the face of partner disapproval (e.g., “feel afraid that he would reject me” (reversed)), in persuading a partner to use a condom (e.g., “confident in my ability to suggest using a condom”), and in using a condom while under the influence of substances (e.g., “confident that I could stop to put a condom on my partner”). The 5-point Likert scale ranges from strongly disagree to strongly agree. Scale scores could range from 15 to 75 in the overall measure (α = .90).
Condom beliefs were measured with Bogart and Thorburn’s 8-item scale (Bogart and Thorburn 2005) including questions related to hedonistic beliefs (e.g., “condoms ruin sex,” “condoms are too much trouble”). The 4-point Likert scale ranges from “strongly disagree” to “strongly agree,” with scores ranging from 8 to 40 (α = .81).
Intentions to use condoms was measured with a single item (1 = “not at all likely” to 7 = “extremely likely”): “In the next 6 months, how likely is it that you will use a condom every time you have vaginal or anal sex with your partner?”
Sexual impulse control was measured with a single item (1 = “strongly disagree” to 4 = “strongly agree”) to understand women’s willingness to refuse sex if a condom is not at hand: “If a condom is not handy, I will have sex anyway” (Wingood and Diclemente 1998).
Feasibility and Acceptability
Stakeholder input is necessary to ensure feasibility and acceptability of an intervention (McKleroy et al. 2006). Final program content was informed by feedback obtained during the adaptation process through focus groups, consensus groups, and interviews with homeless women and service providers (Cederbaum et al. 2014). In the pilot efficacy trial reported here, we obtained feedback from women in the intervention condition through a one-page, anonymous self-administered form that women completed in privacy immediately after the intervention and returned in a sealed envelope upon departing. We sought to understand women’s acceptance of the program and facilitator, and to understand the extent to which they perceived that facilitators discussed all content. Women responded to eight items inquiring about the program on a scale ranging from “strongly agree” to “strongly disagree.” Items included, “The counselor was respectful of me,” “The program made me feel more able to protect myself from HIV,” and “I would recommend this program to a friend.” Women also responded to 12 “yes/no” items to indicate whether the counselor had addressed fundamental aspects of the program, including, “showed me how to put on a male condom,” and “gave me the opportunity to practice putting on a male condom.”
Analyses
Analyses were focused on understanding the effect of the adapted Sister To Sister intervention on behavioral outcomes (i.e., proportion of times a condom was used during sex, condom use at last sex) and attitudinal outcomes (i.e., self-efficacy, condom beliefs, condom use intentions, sexual impulse control). Because of the small sample, we did not test the attitudinal outcomes as mediators of associations between the intervention and behavioral outcomes.
We first examined baseline differences between intervention and control conditions on demographic, background, and outcome variables. We then conducted bivariate analyses (t test or linear regression) to examine the association of each demographic and background characteristic at baseline with (1) each of the outcome variables at 30-day follow-up, and (2) study condition. Results of these two sets of analyses informed selection of covariates entered into multivariate regression models to test the effect of the intervention on each outcome measured at follow-up, controlling for the same outcome variable at baseline. Additionally, we included three variables in each model regardless of their association with study condition or outcomes: age, race/ethnicity (coded as Black or other), and a dummy variable to represent study site. We used logistic regression to model intervention effects on condom use at last intercourse; for the outcomes, we used linear regression. As p value correction is a matter of debate (Miles and Banyard 2007; Perneger 1998), we did not correct for multiple testing. Bonferroni correction alters p values and power in ways dependent on number of tests performed, is highly conservative, and may lead to a high rate of false negatives (Miles and Banyard 2007; Perneger 1998). The underlying assumption for applying Bonferroni correction on multiple comparison is that all null hypotheses are true, which is rare in intervention or psychological studies (Perneger 1998; Gelman et al. 2012). For a pilot evaluation such as the current study, it is important to reduce the probability of missing real differences (i.e., making a type II error). To understand potential bias due to attrition, we tested for differences at baseline between study participants who completed the 30-day follow-up and those who did not. Feasibility and acceptability analyses consisted of simple descriptive tabulations of responses to the participant feedback form.
Results
Descriptives
As shown in Table 1, the majority of women who completed the baseline survey identified as African-American or Black (57.0 %). Few women (6 %) were currently married. Mean monthly income was limited (US$517) and only 15.2 % had been employed part-time or full-time in the past 6 months. Sixty-two percent of all women had been homeless at least three of the past 6 months. Overall, 40 % of women reported previous participation in an HIV or AIDS education program.
In terms of baseline differences between participants in the intervention and control conditions, women in the intervention condition were less likely to have reported previous participation in an HIV or AIDS education program than women in the control condition (27.5 vs. 53.8 %, p = .02). Participants also differed on several outcomes measured at baseline. In terms of behavioral outcomes, women in the comparison condition were more likely to have self-reported use of condoms (male or female) at last sex (38.5 vs. 15.4 %, p = .02). Mean self-efficacy scores were greater among women in the control group than among women in the intervention group (49.0 vs. 38.4; p = .001). Women in the control group also reported more positive condom beliefs (mean 22.9 vs. mean 19.5; p = .02) and greater mean intention to use condoms (3.8 vs. 2.7, p = .02) than women in the intervention group. There were no significant differences at baseline in behavioral or attitudinal outcomes or in demographic and background characteristics between participants who completed the follow-up survey and those who did not.
Multivariate
Multivariate regression models included the following independent variables to predict attitudinal and behavioral outcomes: intervention vs. control condition, the corresponding outcome measured at baseline, age, race/ethnicity (Black vs. other), income, employment, education, homeless at least three of the past 6 months, previous HIV education, and study site. Results of models are depicted in Table 2.
Behavioral Outcomes
At follow-up, the proportion of times women had protected vaginal or anal sex was significantly and positively associated with women’s participation in the intervention (b = .21, SE = .10, t = 2.16, p = .036). Women who participated in the intervention were also significantly more likely to have self-reported either male or female condom use at last sex, such that a woman who participated in the intervention had four times the odds of having used a condom in the past 30 days than a woman in the control condition (OR = 4.28, 95 % CI = 1.07, 17.16, p = .04).
Attitudinal Outcomes
Among the attitudinal variables, participants in the intervention expressed significantly greater intentions to use condoms at follow-up, relative to those in the comparison condition (b = 1.53, SE = .55, t = 2.78, p = .008). The intervention effect was also significant for sexual impulse control, such that women who participated in the intervention expressed greater control at follow-up than women in the comparison condition (b = .60, SE = .26, t = 2.31, p = .025). Among intervention participants, more positive condom beliefs (b = 2.50, SE = 1.49, t = 1.68, p = .098) and greater overall condom self-efficacy (b = 3.88, SE = 2.20, t = 1.76, p = .084) trended towards significance in the expected direction at follow-up.
Feasibility and Acceptability
Participant Feedback
Among 37 of 39 women who completed the feedback form, all women indicated either strong agreement (N = 33; 89.2 % of 37) or agreement (N = 4; 10.8 % of 37) with each of the eight items that reflected satisfaction and acceptance of the intervention. Two women did not complete the form due to their time constraints. Regarding the 12 “yes/no” items that indicated whether the facilitators addressed fundamental aspects of the program, all women (N = 37; 100 %) expressed agreement that the counselor had addressed 10 of the 12 fundamental aspects. Nearly all women (N = 34; 91.9 %) indicated that the counselor had addressed the other two aspects (i.e., presented statistics on HIV in the Los Angeles area, discussed reducing HIV risk when using injection drugs).
Discussion
Results from this pilot efficacy trial of an adapted Sister To Sister intervention for homeless women are encouraging. Consistent with health behavior theories which posit that behavioral changes are likely to occur when attitudes are influenced and skills are enhanced (Ajzen and Fishbein 2005), we expected that participants in the intervention condition would show more positive change in condom use attitudes and beliefs and related behaviors over a 30-day period compared to participants in the information-only condition (Jemmott et al. 2008). Our hypothesis was confirmed in that we detected statistically significant differences between the intervention and control conditions in both the proportion of protected sex acts during the follow-up period, as well as whether a condom was used the last time women had sexual intercourse.
Our expectations regarding attitudinal change were also confirmed, in that intervention participants showed significantly greater positive change in condom use intentions and sexual impulse control over time compared to control group participants. Intention to engage in a behavior, in this case condom use, is central to the theory of reasoned action (Fishbein and Ajzen 2010) and has been associated with condom use behavior in previous studies (Webb and Sheeran 2006). Condom beliefs and self-efficacy were marginally associated with intervention participation in the expected direction. It is somewhat surprising that stronger effects were not found for condom use self-efficacy, as this was found to be the most important predictor and mediator of intervention effects in the randomized controlled trial of the original Sister To Sister intervention (O’Leary et al. 2008). Sister To Sister’s emphasis on social cognitive theory (O’Leary et al. 2008; Jemmott et al. 2008) is evident in the intervention’s focus on building skills in condom use and partner negotiation. The significance of condom use intentions and the marginal effect for self-efficacy in the present study might suggest greater relevance for the theory of reasoned action (Fishbein and Ajzen 2010) than for social cognitive theory (McAliser et al. 2008) in explaining how the intervention influences homeless women’s protective behaviors. This possibility awaits examination in an efficacy trial through formal testing of these theory-based mechanisms of behavioral change in mediation models.
That the intervention significantly influenced sexual impulse control is an especially important finding for homeless women. Women who experience homelessness may be more inclined to have unprotected sex because of gender-based power imbalances arising from past and current intimate partner violence (Wenzel et al. 2006). Homeless women may also engage in sex trade activities to meet subsistence needs for housing and food, and other needs such as drugs (Weiser et al. 2006). The adapted Sister To Sister intervention may have helped the women in this study feel more empowered to resist having sex when a condom was not available. While this is a positive outcome in terms of protection against HIV and other STIs, it does not directly address women’s unmet subsistence needs, a need for drug treatment, or previous trauma experiences. The brevity of the intervention (40 min), however, would enable its integration and delivery in the context of other programming at sites to address homeless women’s needs. Brevity was a desirable feature highlighted by service providers in the formative stages of this work (Cederbaum et al. 2014).
A major limitation of this study is that we used a quasi-experimental design rather than a true experiment to evaluate the efficacy of the intervention on attitudinal and behavioral factors for HIV. Although differences in baseline demographic/background, behavioral, and attitudinal characteristics were controlled in regression analyses, selection bias, the primary threat to internal validity, cannot be ruled out except through a meticulously executed randomized controlled trial. Nonetheless, with limited power due to small sample size, we were able to detect statistically significant effects for both of the behavioral outcomes and for two of the four attitudinal outcomes we examined. We did not correct for multiple testing because p value correction is a matter of debate, and Bonferroni correction is highly conservative (Miles and Banyard 2007; Perneger 1998). For this pilot study, we decided it was important to reduce the probability of missing real differences (i.e., making a Type II error). We nevertheless acknowledge a potential for error. The limited number of study sites, the small sample size, and use of a single post-intervention follow-up survey are additional limitations inherent to a small pilot study that will be addressed in the next phase of this research.
There is a call for approaches that go beyond behavioral risk reduction interventions to address the larger set of circumstances surrounding vulnerable populations and that influence risk for HIV and other poor health outcomes (Adimora et al. 2013). Safe and stable housing, for example, may be among the most important tools for reducing women’s risk for HIV and related threats to health (Wenzel et al. 2007). Yet, housing that is affordable and accessible to the extremely poor in the USA remains limited (National Low Income Housing Coalition 2013), and significant numbers of women continue to experience homelessness (Mental Health Services Administration 2011; US Department of Housing and Urban Development [HUD] 2010). Women homeless now and in the future therefore continue to face elevated levels of risk for HIV and other threats. Further, HIV continues to disproportionately impact Black women in the USA (CDC 2014a, b). Due to long-standing disparities in socioeconomic status, Black women also represent the majority of women experiencing homelessness (HUD 2010).
In the face of multi-faceted risks and a call for structural interventions to prevent HIV, what, then, is the role of a brief behavioral skill-based intervention in reducing the sexual transmission of HIV and other STIs among homeless women? Effective HIV sexual risk reduction interventions focused on women experiencing homelessness continue to be urgently needed. This small pilot study provides preliminary evidence that behavioral change—namely, condom use—can be achieved for homeless women through a brief skill-based intervention that is viewed positively by program participants and is feasible to deliver in the busy settings where homeless women typically seek services. A randomized controlled trial employing a longer follow-up period to monitor outcomes will be necessary to determine efficacy of the adapted intervention.
References
Adimora, A. A., Ramirez, C., Auerbach, J. D., Aral, S. O., Hodder, S., et al. (2013). Preventing HIV infection in women. Journal of Acquired Immune Deficiency Syndromes, 63, S168–S173.
Ajzen, I., & Fishbein, M. (2005). The influence of attitudes on behavior. In D. Albarracín, B. T. Johnson, & M. P. Zanna (Eds.), The handbook of attitudes (pp. 173–221). Mahwah: Lawrence Erlbaum Associates Publishers.
Ajzen, I., Albarracín, D., & Hornik, R. (2007). Prediction and change of health behavior: Applying the theory of reasoned action approach. Mahwah: Lawrence Erlbaum.
Barkley, T. W., & Burns, J. L. (2000). Factor analysis of the Condom Use Self-Efficacy Scale among multicultural college students. Health Education Research, 15, 485–489. doi:10.1093/her/15.4.485.
Barrera, M., Jr., Castro, F. G., Strycker, L. A., & Toobert, D. J. (2013). Cultural adaptations of behavioral health interventions: A progress report. Journal of Consulting and Clinical Psychology, 81, 196–205.
Bogart, L., & Thorburn, S. (2005). Are HIV/AIDS conspiracy beliefs a barrier to HIV prevention among African Americans? Journal of Acquired Immune Deficiency Syndromes, 38, 213–218.
Campbell, A. N. C., Tross, S., Hu, M., Pavlicova, M., Kenney, J., & Nunes, E. V. (2011). Female condom skill and attitude: Results from a NIDA Clinical Trials Network gender-specific HIV risk reduction study. AIDS Education and Prevention, 23, 329–340.
Caton, C. L. M., El-Bassel, N., Gelman, A., Barrow, S., Herman, D., Hsu, E., Tochterman, A. Z., Johnson, K., & Felix, A. (2013). Rates and correlates of HIV and STI infection among homeless women. AIDS Behavior, 17, 856–864.
Cederbaum, J. A., Wenzel, S. L., Gilbert, M. L., & Chereji, E. (2013). The HIV risk reduction needs of homeless women in Los Angeles. Women's Health Issues, 23, 17–172.
Cederbaum, J. A., Song, A., Hsu, H., Tucker, J., & Wenzel, S. (2014). Adopting an EBI for homeless women: Engaging the community in shared decision-making. Journal for the Health Care for the Poor and Underserved, 25, 1552–1570.
Centers for Disease Control and Prevention (2009). Compendium of evidence-based HIV prevention interventions. Retrieved from http://www.cdc.gov.libproxy.usc.edu/HIV/topics/research/prs/evidence-based-interventions.htm.
Centers for Disease Control and Prevention (2014). HIV among women: Fact sheet. Atlanta: Author. Retrieved from http://www.cdc.gov/hiv/pdf/risk_women.pdf.
Centers for Disease Control and Prevention (2014). HIV among African Americans. Fact sheet. Atlanta: Author. Retrieved from http://www.cdc.gov/nchhstp/newsroom/docs/CDC-HIV-AA-508.pdf.
Crepaz, N., Marshall, K. J., Aupont, L. W., et al. (2009). The efficacy of HIV/STI behavioral health interventions for African American females in the United States: A meta-analysis. American Journal of Public Health, 99, 2069–2078.
Crosby, R. A., DiClemente, R. J., Salazar, L. F., Wingood, G. M., McDermott-Sales, J., Young, A. M., & Rose, E. (2013). Predictors of consistent condom use among young African American women. AIDS Behavior, 17, 865–871.
Cunningham, S. D., & Card, J. J. (2014). Realities of replication: Implementation of evidence-based interventions for HIV prevention in real-world settings. Implementation Science, 9, 1–9.
Dennin, P., & DiNenno, E. (2014). Communities in crisis: Is there a generalized HIV epidemic in impoverished areas of the United States? http://www.cdc.gov/hiv/risk/other/poverty.html. Accessed 29 June 2014.
DiClemente, R. J., Wingood, G. M., Blank, M. B., & Metzger, D. S. (2008). Future directions for HIV prevention research: Charting a prevention science research agenda. Journal of Acquired Immune Deficiency Syndromes, 47, S47–S48.
Durlak, J. A., & DuPre, E. P. (2008). Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affection implementation. American Journal of Community Psychology, 41, 327–350.
Fishbein, M., & Ajzen, I. (2010). Predicting and changing behavior: The reasoned action approach. New York: Psychology Press (Taylor & Francis).
Gelman, A., Hill, J., & Yajima, M. (2012). Why we (usually) don't have to worry about multiple comparisons. Journal of Research on Educational Effectiveness, 5, 189–211.
German, D., & Latkin, C. A. (2012). Social stability and HIV risk behavior: Evaluating the role of accumulated vulnerability. AIDS Behavior, 16, 168–178.
Jemmott, L. S., Jemmott, J. B., & O’Leary, A. (2007). Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary care settings. American Journal of Public Health, 97, 1034–1040. doi:10.2105/AJPH.2003.020271.
Jemmott, L. S., Jemmott, J. B., Hutchinson, M. K., Cederbaum, J. A., & O’Leary, A. (2008). Sexually transmitted infection/HIV risk reduction interventions in clinical settings. Journal of Obstetrics, Gynecologic, and Neonatal Nursing, 37, 137–145. doi:10.1111/j.1552-6909.2008.00221.x.
Kennedy, D. P., Wenzel, S. L., Tucker, J. S., et al. (2010). Unprotected sex of homeless women living in Los Angeles County: an investigation of the multiple levels of risk. AIDS and Behavior, 14, 960–973.
McAliser, A. L., Perry, C. L., & Parcel, G. S. (2008). How individuals, environments, and health behaviors interact: Social cognitive theory. In K. Glanz, B. K. Rimer, & K. Viswanath (Eds.), Health behavior and health education (4th ed., pp. 169–188). San Francisco: Jossey-Bass.
McKleroy, V. S., Galbraith, J. S., Cummings, B., Jones, P., Harshbarger, C., et al. (2006). Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Education and Prevention, 18, 59–74.
Miles, J., & Banyard, P. (2007). Applying statistics in psychology: A practical introduction. London: Sage.
National Low Income Housing Coalition (2013). Housing spotlight-America’s affordable housing shortage, and how to end it. Washington, DC. Retrieved from http://nlihc.org/sites/default/files/HS_3-1.pdf.
O’Leary, A., Jemmott, L. S., & Jemmott, J. B. (2008). Mediation analysis of an effective sexual risk-reduction intervention for women: The importance of self-efficacy. Health Psychology, 27, S180–S184. doi:10.1037/0278-6133.27.2(Suppl.).S180.
Perneger, T. V. (1998). What’s wrong with Bonferroni adjustments. British Medical Journal, 316, 1236–1238.
Riley, E. D., Gandhi, M., Hare, C. B., Cohen, J., & Hwang, S. W. (2007). Poverty, unstable housing, and HIV infection among women living in the United States. Current HIV/AIDS Reports, 4, 181–186.
Substance Abuse and Mental Health Services Administration (2011). Current statistics on the prevalence and characteristics of people experiencing homelessness in the United States. Rockville, MD. http://homeless.samhsa.gov/ResourceFiles/hrc_factsheet.pdf.
Scott-Sheldon, L. A., Huedo-Medina, T. B., Warren, M. R., Johnson, B. T., & Carey, M. P. (2011). Efficacy of behavioral interventions to increase condom use and reduce sexually transmitted infections: A meta-analysis, 1991 to 2010. Journal of Acquired Immune Deficiency Syndromes, 58, 489–498.
Thomas, S. B., Benjamin, G. C., Almario, D., & Lathan, M. J. (2006). Historical and current policy efforts to eliminate racial and ethnic health disparities in the United States: Future opportunities for public health education research. Health Promotion Practice, 7, 324–330.
United States Department of Health and Human Services. (2010). Healthy People 2020. Washington, DC: United States Government Printing Office.
United States Department of Housing and Urban Development. (2010). The 2009 Annual Homeless Assessment Report to Congress. Washington, DC: U.S. Government Printing Office.
Webb, T. L., & Sheeran, P. (2006). Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychological Bulletin, 132, 249–268. doi:10.1037/0033-2909.132.2.249.
Wechsberg, W. M., Lam, K. K., Zule, W. A., & Bobashez, G. (2004). Efficacy of a woman-focused intervention to reduce HIV risk and increase self-sufficiency among African American crack abusers. American Journal of Public Health, 94, 1165–1173.
Weiser, S. D., Dilworth, S. E., Neilands, T. B., Cohen, J., Bangsberg, D. R., & Riley, E. D. (2006). Gender-specific correlates of sex trade among homeless and marginally housed individuals in San Francisco. Journal of Urban Health, 83, 736–740.
Wenzel, S. L., Tucker, J. S., Elliott, M. N., et al. (2004). Prevalence and co-occurrence of violence, substance use and disorder, and HIV risk behavior: A comparison of sheltered and low-income housed women in Los Angeles County. Preventive Medicine, 39, 617–624.
Wenzel, S. L., Tucker, J. S., Hambarsoomian, K., & Elliott, M. N. (2006). Toward a more comprehensive understanding of violence against impoverished women. Journal of Interpersonal Violence, 21, 820–839.
Wenzel, S.L., Tucker, J.S., Elliott, M.N., & Hambarsoomian, K. (2007). Sexual risk among impoverished women: Understanding the role of housing status. AIDS and Behavior, (Suppl 6), S9–S20.
Wingood, G. M., & DiClemente, R. (1998). Partner influences and gender-related factors associated with non-condom use among young adult African American women. American Journal of Community Psychology, 26, 29–51.
Wingood, G. M., & DiClemente, R. J. (2008). The ADAPT-ITT model: A novel method of adapting evidence-based HIV interventions. Journal of Acquired Immune Deficiency Syndromes, 47, 40–46.
Acknowledgements
This research was funded by a grant from the National Institute of Drug Abuse (R21 DA031610-01; PI: Wenzel).
Conflict of Interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wenzel, S.L., Cederbaum, J.A., Song, A. et al. Pilot Test of an Adapted, Evidence-Based HIV Sexual Risk Reduction Intervention for Homeless Women. Prev Sci 17, 112–121 (2016). https://doi.org/10.1007/s11121-015-0575-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11121-015-0575-6