Abstract
Background
Factors affecting decline in renal function and cyst growth in patients with autosomal polycystic kidney disease (ADPKD) are not fully described, particularly in Japan.
Methods
This was the first multi-facility, prospective, observational cohort study conducted in ADPKD patients at 14 centers in Japan. Patients in the J-PKD registry were assessed from December 2009 to June 2012 (follow-up until June 2017). Patients’ data including estimated glomerular filtration rate (eGFR) and total kidney volume (TKV) were assessed initially and a maximum of five times annually. Contributing factors to eGFR decline and TKV growth were identified using multiple linear regression analysis.
Results
Of the 340 patients in the J-PKD registry, data analysis was performed for 192 patients in whom serial changes for both eGFR and TKV were obtained. eGFR slope, eGFR change, and TKV change values were as follows: − 2.7 (− 4.2 to − 1.5) (ml/min/1.73 m2/year), − 5.0 (− 9.6 to − 2.3) (%/year), and 4.78 (0.86–8.22) (%/year), respectively. Lower high-density lipoprotein (HDL) cholesterol was an independent predictor of eGFR decline, using both eGFR slope and change (P = 0.04, P = 0.02, respectively), whereas lower hemoglobin and higher uric acid were significantly associated with greater eGFR change only (P = 0.02, P = 0.002, respectively). Younger age and higher fasting blood sugar were independent predictors of greater TKV change (P = 0.01, P = 0.02, respectively).
Conclusions
This real-world study in Japan identified risk factors for renal function decline in ADPKD patients. These included lower HDL cholesterol, lower hemoglobin and higher uric acid for eGFR decline, and youth and higher blood sugar levels for TKV growth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autosomal dominant polycystic kidney disease (ADPKD) is a hereditary renal disease marked by the formation of bilateral renal cysts, kidney volume growth, and a gradual decline in kidney function [1]. In Japan, ADPKD is the fourth leading causative disease requiring dialysis treatment [2].
Molecular biological studies have begun to elucidate the pathology of cystogenesis in ADPKD, and numerous risk factors for decline in renal function and renal cyst growth have been reported [3,4,5,6,7]. These include the PKD1 gene, male sex, hypertension, proteinuria, and total kidney volume (TKV); however, findings in the published literature are inconsistent [3,4,5,6,7]. Individuals predisposed to a decline in renal function and cyst growth have, therefore, not been fully described, particularly among the population in Japan [8, 9]. As well as much needed basic research into this disease, clinical studies are essential to clarify risk factors for declining renal function and cyst growth, and to find interventions to prevent these outcomes.
Japan is estimated to have almost 100,000 individuals with polycystic kidney disease (PKD), with approximately 30,000 receiving treatment in hospitals and clinics [10]. In 1994, Japan’s Ministry of Health, Labour, and Welfare funded the Research Program of Progressive Renal Disease; while this program included a longitudinal study of patient treatment at medical institutions [10], it did not include a prospective study of renal function, kidney volume, frequency of complications, or treatment in these patients.
This is the first prospective ADPKD patient cohort study in Japan. The aim of this study was to identify and clarify the relevant risk factors for decline in renal function and renal cyst growth in this population. To achieve this, a Japan PKD registry (J-PKD) for patients with ADPKD or Autosomal Recessive Polycystic Kidney Disease (ARPKD) being treated at medical facilities in Japan was created.
Materials and methods
Study design and study population
This was a joint, multi-facility, prospective, observational cohort study conducted at 14 medical institutions in Japan. Patients being treated for ADPKD or ARPKD at each participating institution during the study period were eligible for inclusion in the J-PKD registry. The registration period was from December 1, 2009 to June 30, 2012, with a follow-up period to June 30, 2017. Exclusion criteria included patients treated with tolvaptan or on renal replacement therapy (RRT) at the time of registration and with only one measurement for estimated glomerular filtration rate (eGFR) and TKV.
Ethics committees from each of the 14 institutions approved the study, and the Japanese Society of Nephrology approved the study (No. 6). Written informed consent was obtained from each participant.
Data collection
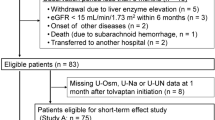
For each case registration, anonymized data were entered into an online system; this format of anonymized data entry is utilized in the Japan Kidney Disease Registry (J-KDR)—the official registry of the Japanese Society of Nephrology. Data were collected and inputted for the following outcomes: eGFR and TKV, as well as principal covariates: age, sex, physical findings, and blood test results (recorded at study start and a maximum of five times annually). If patients received tolvaptan or RRT during the observation period, their eGFR and TKV values preceding tolvaptan initiation or RRT were used (Fig. 1).
The J-PKD registry was created with data collected from 342 patient cases: ADPKD (n = 340), and ARPKD (n = 2).
Outcomes
The primary outcome was decline in renal function. For simplicity, we utilized eGFR slope (ml/min/1.73 m2/year) because it is widely used to define decline in renal function [6, 7, 11], although there are recent reports that eGFR change (%/year) also relates to the development of end-stage renal disease in patients with ADPKD [12,13,14]. The eGFR slope was calculated using the least squares method for secular change.
The secondary outcome was TKV variation, using the common definition of the rate of variability (TKV change [%/year]) [15, 16]. TKV (cm3) was calculated by obtaining the length and width measurements from a magnetic resonance imaging or computerized tomography scan and using either the ellipsoid volume equation or stereology method.
Statistical analysis
Using the Shapiro–Wilk test, normally distributed variables were reported as the mean ± standard deviation (SD), and non-normally distributed variables as median and interquartile range. Categorical variables were determined as a percentage for each level, and variable distribution was also compared by sex. Comparisons were made using the unpaired t test, Mann Whitney U test, or Fisher’s exact test, as appropriate.
First, a correlation analysis was performed using the Spearman’s rank correlation coefficient to clarify the relationship between the objective variable and each explanatory variable. For subgroup analyses, the Mann–Whitney U test was used for comparison between two groups, and the Kruskal–Wallis test for comparison among three or more groups. Second, multiple regression analysis was performed for the primary outcome to investigate related factors. Parameters considered relevant to the renal function decline in patients with ADPKD and chronic kidney disease (CKD) were selected as explanatory variables [3,4,5,6, 15, 17,18,19,20,21,22,23]. Non-normally distributed variables (body mass index [BMI], urinary protein-to-creatinine ratio [UPCR], and height-adjusted TKV [htTKV]) were converted into a natural logarithm (Ln), and TKV change was incorporated in the explanatory variables. Correlation analyses and multivariate analyses were also performed for TKV change,
As TKV growth has been almost universally related to decline in renal function [13, 14], the explanatory variables selected for TKV change were similar to those for the primary outcome.
Using the eGFR slope as an objective variable, regression analysis was calculated within subgroups (by sex, and by TKV cases < 750 ml and ≥ 750 ml). Regression analysis was performed with the adjustment of only baseline eGFR, considering the small number of patients included in the subgroups.
In terms of calculations for the correlation coefficient and multiple regression analyses, missing data for the explanatory variable were presumed to be data missing at random, and calculations were completed using multiple imputation by chained equations (100 imputations). SPSS software for Mac (ver. 25; IBM Corp., Armonk, NY, USA) was used for all statistical analyses, with a significance level of 5%.
Results
Baseline characteristics
Analyses were performed on 192 of the 340 individuals in the J-PKD registry (Fig. 1). The median (range) follow-up was 58.8 (43.8–60.7) months, with a follow-up frequency of assessments of five (4–5) times throughout the study period. Baseline characteristics (Table 1) show mean [SD] age, 49.0 ± 12.8 years, with a predominance of females to males (123:69), and baseline eGFR, 56.7 ± 25.7 ml/min/1.73 m2. Laboratory values, including potassium, alanine aminotransferase (ALT), γ-glutamyltranspeptidase (γ-GTP), and albumin were significantly higher for male versus female participants (P < 0.05). Fasting blood sugars, hemoglobin, hematocrit, uric acid, and serum creatinine values were also significantly higher (P < 0.001), but there was no significant difference in eGFR between males and females (P = 0.4). Higher levels of high-density lipoprotein (HDL) cholesterol were evident in females versus males (P < 0.001). There was also a significantly greater usage of angiotensin converting enzyme inhibitor [ACEi]/angiotensin II receptor blocker [ARB] for male participants (P = 0.04).
Primary outcome: decline in kidney function
The overall eGFR slope was − 2.7 (− 4.2 to − 1.5) ml/min/1.73 m2/year. There were individual significant positive correlations for age, aspartate transaminase (AST), hemoglobin and hematocrit, and individual significant inverse correlations for UPCR, TKV, and htTKV (Table 2, Fig. 2a).
Subgroup analyses for eGFR slope showed significant differences for TKV change (≥ 5%/year vs < 5%/year, P < 0.05), and TKV (≥ 750 ml vs < 750 ml, P ≤ 0.007; Table 3, Fig. 2b–c).
In the multivariate analysis, a significant positive correlation for eGFR slope was shown for HDL cholesterol (P = 0.04), suggesting that a low HDL value is a risk factor for decline in renal function (Table 4). For Ln UPCR, there was a near-significant inverse correlation with eGFR slope (P = 0.08). Inverse correlation trends were also observed for htTKV (P = 0.06) and TKV change (P = 0.07); elevations in TKV and proteinuria are considered risk factors for a decline in renal function.
In instances of TKV < 750 ml (n = 38), there was a significant positive correlation with eGFR slope for hemoglobin (P = 0.03), a significant inverse relationship for Ln UPCR (P = 0.01), and Ln htTKV (P = 0.03; Supplemental Table 1). Similar findings were evident for TKV ≥ 750 ml (n = 154); hemoglobin, age, Ln UPCR, and HDL showed a significant or neared significant relationship with eGFR slope. However, TKV change was found to be a significant risk factor for eGFR slope (P = 0.01), with no significance shown for Ln htTKV. Gender differences were also evident; there was a significant inverse relationship with eGFR slope for ACEi/ARB usage in males (P = 0.001) and TKV change in males (P = 0.001). In females, HDL showed a significant positive correlation (P < 0.05), and Ln UPCR an inverse correlation (P < 0.05; Supplemental Table 2).
Secondary outcome: clinical parameters associated with TKV growth
Overall, TKV change was 4.78 (0.86–8.22) (%/year), and TKV change was significantly higher in males than females [5.86 (2.51–9.87) vs. 3.78 (0.71–7.10); P = 0.02]. Correlation analysis showed a positive correlation with waist circumference, UPCR, and blood sugar (P = 0.04, P < 0.05, P = 0.03, respectively). TKV change also showed a positive correlation with creatinine (P = 0.02), but not with eGFR (P = 0.14; Table 5). While creatinine and eGFR were expected to be inversely associated with TKV change, in addition to males showing higher creatinine than females for similar eGFR, significantly higher TKV change in males than females in this cohort might lead to the stronger positive correlation between serum creatinine and TKV change than the inverse correlation between eGFR and TKV change. Age had a significant inverse correlation with TKV change (P = 0.01), and fasting blood sugar, a positive correlation with TKV change (P = 0.02). Male participants had a tendency toward TKV increase (P = 0.10), with HDL and Ln UPCR showing a trend towards positive correlation with TKV change (P = 0.06 and P = 0.09, respectively; Table 6).
Discussion
This was the first multi-facility, prospective, observational cohort study in Japan to identify risk factors for patients with ADPKD. Increased proteinuria and TKV growth were risk factors for decline in renal function, and lower HDL cholesterol levels were significantly associated with this decline. While several factors contributing to renal function decline in Japanese patients with ADPKD have previously been identified, patient numbers in these studies were limited, leading to insufficient adjustments for covariates [8, 9]. This study used a comparatively large number of participants, enabling robust multivariate analyses on covariates.
A Mendelian randomization study indicated that higher HDL concentration was associated with higher eGFR and lower risk for the development of CKD [24], while the evidence that HDL concentrations are associated with prevalence or incidence of cardiovascular events as well as mortality is quite controversial [25]. In ADPKD patients, the MDRD Study found that low HDL was significantly correlated with a decline in eGFR [17]; however, a 3-year follow-up analysis conducted by The Consortium for Radiologic Imaging Studies of Polycystic Kidney Disease (CRISP) found no such correlation (CRISP I) [6]. In CRISP II, a longer-term, follow-up study examining modifiable factors affecting ADPKD progression, univariate analysis showed that low HDL had a significant correlation with renal function decline, although multivariate analysis (in the final regression model) did not reveal low HDL as a significant correlating factor [7]. In this study, even after adjustment for multiple covariates expected to be associated with ADPKD progression, lower HDL was found to be significantly associated with renal function decline.
Proteinuria was not only to be a known risk factor for general CKD progression, cardiovascular mortality, and all-cause mortality [26, 27], but also was found to be a possible risk factor for a decline in renal function in ADPKD patients [5, 6]. The rate of TKV growth was also found to be an independent risk factor for renal function decline. While large-scale studies have shown that greater baseline htTKV was significantly correlated with renal function decline [5, 6, 13,14,15, 28], multivariate linear regression analyses in this study only showed a tendency toward an inverse correlation with eGFR slope.
The hemoglobin level tended to inversely correlate with eGFR slope, but low hemoglobin did not remain a significant risk factor for eGFR slope by multivariate analysis. The association between hemoglobin and general CKD progression has been also contrasting: a randomized controlled trial in Japan suggested that achieving a higher target hemoglobin level was associated with a greater renoprotective effect [29], while a meta-analysis described that targeting higher hemoglobin levels in CKD might increase the risk for end-stage renal disease [30]. When it comes to ADPKD patients, while hemoglobin was not included as an explanatory variable in the CRISP and MDRD studies [6, 7, 17], in a recent, retrospective Japanese study in patients with ADPKD, low hemoglobin was suggested as an independent contributing factor for decline in renal function [31]. Even though a target hemoglobin value is not known for patients with ADPKD, interventions to increase hemoglobin levels can improve renal survival [29].
Multivariate analyses in CRISP II, and a South Korean study, have also shown that high uric acid levels are an independent risk factor for renal function decline in ADPKD patients [7, 32], although uric acid was not associated with eGFR slope in our study. While febuxostat may have had a renoprotective function in these patients, a randomized controlled trial in patients with Stage 3 CKD in Japan only found a significant renoprotective effect in patients with sub-median renal function, and patients with no observed proteinuria [33]. The ratio of patients with ADPKD in the Stage 3 CKD study is unclear, but one might expect a similar effect among this subset.
Younger age and high fasting blood sugar levels were significant risk factors for TKV growth. Youth is an established significant, independent risk factor for TKV increase (CRISP I and II) [6, 7], while to our knowledge, there are no ADPKD patient studies that correlate high fasting blood sugar levels and TKV growth. Although we could not deny the effect of diabetes itself independent of blood sugar levels, only a small percentage of the patients had fasting blood sugar levels of 126 mg/dl (the level included in the diagnostic criteria for diabetes) or higher (n = 11; 6%), so we believe that the effect of diabetes can be minimized in this cohort. A previous study demonstrated that aerobic glycolysis was enhanced in kidney from ADPKD patients, and glucose deprivation results in decreased proliferation of ADPKD cells, dependent on the extracellular signal-related kinase (ERK) pathway [34]. Additionally, another basic research indicated that the use of a glucose analogue retarded ADPKD progression in different polycystic kidney disease murine models via activation of AMP activated protein kinase (AMPK) [35]. Insulin-like growth factor and AMPK are implicated in cyst growth, and AMPK stimulation inhibits ERK pathway and subsequent mammalian target of rapamycin pathway included in renal cystogenesis in ADPKD [34,35,36,37]. Based on these findings from basic researches, it is likely that high blood sugar levels, or accompanying insulin resistance state, is associated with TKV growth in ADPKD patients via inhibition of AMPK. The association between ADPKD, increase in blood sugar levels, and insulin resistance is controversial, but with the high risk of new onset diabetes after kidney transplantation in patients with ADPKD [38]. Findings from future research, prospective studies, and interventional studies (AMPK-stimulating metformin [which improves insulin resistance]; NCT2903511 and NCT 02656017) are greatly anticipated.
This study found that TKV growth may occur more rapidly in males than females; however, multivariate analysis did not show any significant correlation between male sex and a decline in renal function. While male sex has been reported as a risk factor for decline in renal function when composite outcomes of overall survival and renal survival are used [3, 4, 8], this has not been the case for multivariate analysis [5].
Limitations of this study included that eGFR slope and TKV change might not be entirely clarified by the explanatory variables selected. Other explanatory variables that could have been included are as follows: dyslipidemia medications, anti-hyperuricemic agents, estimated salt intake [6, 7, 39], and genetic information [40]. Although each outcome was adjusted for baseline values in the multiple regression analysis, taking into consideration the large disparity in baseline eGFR and TKV, and variations in the longitudinal follow-up, patient classification may have been helpful. It is also possible that some selection bias may have occurred during patient screening as there was a high percentage of patients in whom eGFR and TKV variation was not obtained.
In conclusion, this was the first multi-facility, prospective, observational cohort study in Japan to identify risk factors for renal function decline in patients with ADPKD. Using the broad ranging inclusion criteria, this was a real-world study. Risk factors identified in this specific population included the following: lower HDL cholesterol levels, higher proteinuria, and greater TKV change for eGFR decline, and youth and higher blood sugar levels for TKV growth.
References
Cornec-Le Gall E, Alam A, Perrone RD. Autosomal dominant polycystic kidney disease. Lancet. 2019;393:919–35.
Nitta K, Masakane I, Hanafusa N, Taniguchi M, Hasegawa T, Nakai S, et al. Annual dialysis data report 2017, JSDT renal data registry. Ren Replace Ther. 2019;5:53.
Gabow PA, Johnson AM, Kaehny WD, Kimberling WJ, Lezotte DC, Duley IT, et al. Factors affecting the progression of renal disease in autosomal-dominant polycystic kidney disease. Kidney Int. 1992;41:1311–9.
Johnson AM, Gabow PA. Identification of patients with autosomal dominant polycystic kidney disease at highest risk for end-stage renal disease. J Am Soc Nephrol. 1997;8:1560–7.
Fick-Brosnahan GM, Belz MM, McFann KK, Johnson AM, Schrier RW. Relationship between renal volume growth and renal function in autosomal dominant polycystic kidney disease: a longitudinal study. Am J Kidney Dis. 2002;39:1127–34.
Torres VE, King BF, Chapman AB, Brummer ME, Bae KT, Glockner JF, et al. Magnetic resonance measurements of renal blood flow and disease progression in autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol. 2007;2:112–20.
Torres VE, Grantham JJ, Chapman AB, Mrug M, Bae KT, King BF Jr, et al. Potentially modifiable factors affecting the progression of autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol. 2011;6:640–7.
Tokiwa S, Muto S, China T, Horie S. The relationship between renal volume and renal function in autosomal dominant polycystic kidney disease. Clin Exp Nephrol. 2011;15:539–45.
Higashihara E, Horie S, Muto S, Mochizuki T, Nishio S, Nutahara K. Renal disease progression in autosomal dominant polycystic kidney disease. Clin Exp Nephrol. 2012;16:622–8.
Higashihara E, Nutahara K, Kojima M, Tamakoshi A, Yoshiyuki O, Sakai H, et al. Prevalence and renal prognosis of diagnosed autosomal dominant polycystic kidney disease in Japan. Nephron. 1998;80:421–7.
Nowak KL, You Z, Gitomer B, Brosnahan G, Torres VE, Chapman AB, et al. Overweight and obesity are predictors of progression in early autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2018;29:571–8.
Coresh J, Turin TC, Matsushita K, Sang Y, Ballew SH, Appel LJ, et al. Decline in estimated glomerular filtration rate and subsequent risk of end-stage renal disease and mortality. JAMA. 2014;311:2518–31.
Yu ASL, Shen C, Landsittel DP, Harris PC, Torres VE, Mrug M, et al. Baseline total kidney volume and the rate of kidney growth are associated with chronic kidney disease progression in Autosomal Dominant Polycystic Kidney Disease. Kidney Int. 2018;93:691–9.
Perrone RD, Mouksassi MS, Romero K, Czerwiec FS, Chapman AB, Gitomer BY, et al. Total kidney volume is a prognostic biomarker of renal function decline and progression to end-stage renal disease in patients with autosomal dominant polycystic kidney disease. Kidney Int Rep. 2017;2:442–50.
Grantham JJ, Torres VE, Chapman AB, Guay-Woodford LM, Bae KT, King BF Jr, et al. Volume progression in polycystic kidney disease. N Engl J Med. 2006;354:2122–30.
Torres VE, Chapman AB, Devuyst O, Gansevoort RT, Grantham JJ, Higashihara E, et al. Tolvaptan in patients with autosomal dominant polycystic kidney disease. N Engl J Med. 2012;367:2407–18.
Klahr S, Breyer JA, Beck GJ, Dennis VW, Hartman JA, Roth D, et al. Dietary protein restriction, blood pressure control, and the progression of polycystic kidney disease. Modification of Diet in Renal Disease Study Group. J Am Soc Nephrol. 1995;5:2037–47.
Nutahara K, Higashihara E, Horie S, Kamura K, Tsuchiya K, Mochizuki T, et al. Calcium channel blocker versus angiotensin II receptor blocker in autosomal dominant polycystic kidney disease. Nephron Clin Pract. 2005;99:c18-23.
Cadnapaphornchai MA, McFann K, Strain JD, Masoumi A, Schrier RW. Prospective change in renal volume and function in children with ADPKD. Clin J Am Soc Nephrol. 2009;4:820–9.
Sarnak MJ, Greene T, Wang X, Beck G, Kusek JW, Collins AJ, et al. The effect of a lower target blood pressure on the progression of kidney disease: long-term follow-up of the modification of diet in renal disease study. Ann Intern Med. 2005;142:342–51.
de Boer IH, Katz R, Fried LF, Ix JH, Luchsinger J, Sarnak MJ, et al. Obesity and change in estimated GFR among older adults. Am J Kidney Dis. 2009;54:1043–51.
Siu YP, Leung KT, Tong MK, Kwan TH. Use of allopurinol in slowing the progression of renal disease through its ability to lower serum uric acid level. Am J Kidney Dis. 2006;47:51–9.
Bash LD, Erlinger TP, Coresh J, Marsh-Manzi J, Folsom AR, Astor BC. Inflammation, hemostasis, and the risk of kidney function decline in the Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis. 2009;53:596–605.
Lanktree MB, Thériault S, Walsh M, Paré G. HDL cholesterol, LDL cholesterol, and triglycerides as risk factors for CKD: a Mendelian randomization study. Am J Kidney Dis. 2018;71:166–72.
Kronenberg F. HDL in CKD—the devil is in the detail. J Am Soc Nephrol. 2018;29:1356–71.
Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375:2073–81.
Hallan SI, Matsushita K, Sang Y, Mahmoodi BK, Black C, Ishani A, et al. Age and association of kidney measures with mortality and end-stage renal disease. JAMA. 2012;308:2349–60.
Irazabal MV, Rangel LJ, Bergstralh EJ, Osborn SL, Harmon AJ, Sundsbak JL, et al. Imaging classification of autosomal dominant polycystic kidney disease: a simple model for selecting patients for clinical trials. J Am Soc Nephrol. 2015;26:160–72.
Tsubakihara Y, Akizawa T, Iwasaki M, Shimazaki R. High hemoglobin levels maintained by an erythropoiesis-stimulating agent improve renal survival in patients with severe renal impairment. Ther Apher Dial. 2015;19:457–65.
Palmer SC, Navaneethan SD, Craig JC, Johnson DW, Tonelli M, Garg AX, et al. Meta-analysis: erythropoiesis-stimulating agents in patients with chronic kidney disease. Ann Intern Med. 2010;153:23–33.
Ushio Y, Kataoka H, Sato MA, Manabe S, Watanabe S, Akihisa T, et al. Association between anemia and renal prognosis in autosomal dominant polycystic kidney disease: a retrospective study. Clin Exp Nephrol. 2020;24:500–8.
Kim H, Koh J, Park SK, Kim YH, Kim Y, Ahn C, et al. Baseline characteristics of the autosomal-dominant polycystic kidney disease sub-cohort of the Korean cohort study for outcomes in patients with chronic kidney disease. Nephrology (Carlton). 2019;24:422–9.
Kimura K, Hosoya T, Uchida S, Inaba M, Makino H, Maruyama S, et al. Febuxostat therapy for patients with stage 3 CKD and asymptomatic hyperuricemia: a randomized trial. Am J Kidney Dis. 2018;72:798–810.
Rowe I, Chiaravalli M, Mannella V, Ulisse V, Quilici G, Pema M, et al. Defective glucose metabolism in polycystic kidney disease identifies a new therapeutic strategy. Nat Med. 2013;19:488–93.
Chiaravalli M, Rowe I, Mannella V, Quilici G, Canu T, Bianchi V, et al. 2-Deoxy-d-glucose ameliorates PKD progression. J Am Soc Nephrol. 2016;27:1958–69.
Liu C, Zhang Y, Yuan L, Fu L, Mei C. Rosiglitazone inhibits insulin-like growth factor-1-induced polycystic kidney disease cell growth and p70S6 kinase activation. Mol Med Rep. 2013;8:861–4.
Takiar V, Nishio S, Seo-Mayer P, King JD Jr, Li H, Zhang L, et al. Activating AMP-activated protein kinase (AMPK) slows renal cystogenesis. Proc Natl Acad Sci USA. 2011;108:2462–7.
Mao Z, Xie G, Ong AC. Metabolic abnormalities in autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2015;30:197–203.
Torres VE, Abebe KZ, Schrier RW, Perrone RD, Chapman AB, Yu AS, et al. Dietary salt restriction is beneficial to the management of autosomal dominant polycystic kidney disease. Kidney Int. 2017;91:493–500.
Harris PC, Bae KT, Rossetti S, Torres VE, Grantham JJ, Chapman AB, et al. Cyst number but not the rate of cystic growth is associated with the mutated gene in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2006;17:3013–9.
Acknowledgements
This study was supported in part by a Grant-in-Aid for Intractable Renal Diseases Research, Research on rare and intractable diseases, Health and Labour Sciences Research Grants from the Ministry of Health, Labour and Welfare of Japan. Medical writing support, in accordance with GPP guidelines, was provided by Mediwrite Asia Inc Pte Ltd and included editorial and proofreading services. We thank all the participants in this registry and the clinicians who referred their patients and contributed to the clinical data acquisition.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Toshio Mochizuki received travel fees and honoraria for lectures from Otsuka Pharmaceutical Co. Toshio Mochizuki and Hiroshi Kataoka belong to an endowed department sponsored by Otsuka Pharmaceutical Co, Chugai Pharmaceutical Co, Kyowa Hakko Kirin Co, and JMS Co. Satoru Muto received travel fees and honoraria for lectures from Otsuka Pharmaceutical Co., Ltd. Shigeo Horie and Satoru Muto belong to an endowed department sponsored by Otsuka Pharmaceutical Co., Ltd., JENESIS Co., Ltd., Nippon Shinyaku Co., Ltd., Shokubunka Co., Ltd., and Rohto Pharmaceutical Co., Ltd..
Ethical approval
The study was conducted in accordance with the guidelines written in the Declaration of Helsinki. Ethics committees from each of the 14 institutions approved the study, and the Japanese Society of Nephrology approved the study (No. 6).
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Uchiyama, K., Mochizuki, T., Shimada, Y. et al. Factors predicting decline in renal function and kidney volume growth in autosomal dominant polycystic kidney disease: a prospective cohort study (Japanese Polycystic Kidney Disease registry: J-PKD). Clin Exp Nephrol 25, 970–980 (2021). https://doi.org/10.1007/s10157-021-02068-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-021-02068-x