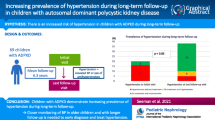
Abstract
Background
In patients with autosomal dominant polycystic kidney disease (ADPKD), renal cysts grow exponentially. Since remaining renal parenchyma has a capacity to compensate for the loss of glomerular filtration, the glomerular filtration rate (GFR) may be sustained until the disease progresses. The purpose of this study was to determine if renal volumetric indices and clinical parameters are associated with renal function in Japanese patients with ADPKD.
Methods
In 73 ADPKD patients (28 men, 45 women), the associations of mean systolic blood pressure, mean diastolic blood pressure, estimated GFR (eGFR), the amount of proteinuria and albuminuria, body mass index (BMI), brachial-ankle pulse wave velocity (baPWV), ankle-brachial index, and total kidney volume (TKV) were retrospectively analyzed.
Results
Multivariate linear regression analysis showed that eGFR was significantly and independently inversely correlated with patients’ age and BMI. The median change in eGFR per year (ΔeGFR/y) was −2.8 ml/min/1.73 m2/year. Multiple linear regression analysis showed that ΔeGFR/y was significantly and independently inversely correlated with the change in TKV per year (ΔTKV/y). Multiple linear regression analysis showed that ΔTKV/y was significantly related to initial TKV and the change in albuminuria per year.
Conclusions
This study demonstrated a significant relationship between the change in renal function and the change in renal volume in Japanese ADPKD patients without renal insufficiency. It is possible that the volume measurements can be used as useful markers for disease progression in Japanese ADPKD patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Autosomal dominant polycystic kidney disease (ADPKD) is the most common progressive hereditary kidney disease affecting all ethnic groups worldwide, with an incidence of 1:500–1:1000. Typically, only a few renal cysts are detected in most affected individuals before 30 years of age; however, by the fifth decade of life, hundreds to thousands of renal cysts are found in the majority of patients. Renal cysts grow exponentially in ADPKD [1]. This continuous growth and expansion of cysts leads to progressive, grotesque, renal enlargement and subsequent loss of renal function [2]. End-stage renal failure requiring renal replacement therapy occurs in approximately 50% of patients and typically develops in the sixth decade of life [3]. However, renal insufficiency is usually not detected until the fifth or sixth decade of life. Since the remaining kidneys have a capacity to compensate for the loss of glomerular filtration in ADPKD patients, the renal function remains stable for many years, but there is a sharp decline in the glomerular filtration rate (GFR) once a critical expansion of renal cysts is reached [4, 5]. GFR, the usual biomarker of renal disease progression, does not decrease substantially until extensive and irreversible damage to noncystic parenchyma occurs. Therefore, it is necessary to identify some reliable biomarkers to follow the progression of this disease [6]. Modeling experiments using prospective clinical data from the Consortium for Radiologic Imaging Studies in Polycystic Kidney Disease (CRISP) cohort have suggested that very high rates of kidney growth must occur during childhood to account for the kidney volumes observed in adults [7]. Recent data from the CRISP study indicate that kidney growth is a critical predictor of progression to renal failure in Caucasian ADPKD patients, playing a more important role than hypertension, proteinuria, age, or sex [1]. Consequently, kidney volume growth is considered the best surrogate marker predicting the decline of renal function in ADPKD [8].
The aim of our study was to investigate the associations among clinical parameters, renal volumetric indices, and renal function in Japanese ADPKD patients.
Materials and methods
The present study enrolled patients who had been diagnosed as having ADPKD, were older than 20 years, and who had magnetic resonance imaging (MRI) examinations with transverse and coronal section images. ADPKD was diagnosed based on the patient’s family history and the results of several imaging studies, such as ultrasonography, computed tomography scanning, and MRI. Patients with end-stage renal disease were excluded. Age of enrollment, mean systolic blood pressure (SBP), mean diastolic blood pressure (DBP), estimated GFR (eGFR), 24-h proteinuria, 24-h albuminuria, body mass index (BMI), brachial-ankle pulse wave velocity (baPWV), ankle-brachial index (ABI), and total kidney volume (TKV) were retrospectively evaluated. Blood pressures were measured at every study visit in the sitting position after a rest of 5 min, using the conventional oscillometric method and mercury manometer in the outpatient clinic. The eGFR was used as a marker of renal function and was calculated using the simplified MDRD equation modified by the appropriate coefficient for Japanese populations by sex as follows [9]:
Arterial stiffness was assessed by measuring baPWV and ABI using an automatic waveform analyzer (Form/ABI; Omron-Colin Co., Ltd., Komaki, Japan). Renal volumes were measured by performing standard abdominal MRI using a 1.5-T scanner. Length, width, and depth were measured in centimeters. TKV was obtained by summing the volumes of both kidneys and then calculating using a standard formula: renal volume = π/6 × length × width × depth [7]. Length and width were obtained from longitudinal images acquired in planes ranging from sagittal to coronal, whereas depth was obtained from transverse images of the mid-kidney acquired in the plane perpendicular to the longitudinal plane. In cases with at least two sequential examinations at least 3 months apart, the changes in variables per year were calculated by comparing values at baseline and the latest data.
Pearson’s correlation coefficients were used to examine the associations among eGFR, the change in eGFR per year (ΔeGFR/y), the change in TKV per year (ΔTKV/y), and selected clinical variables. Multivariate linear regression was used to determine independent predictors of baseline eGFR, ΔeGFR/y, and ΔTKV/y. Two-tailed p values of <0.05 were considered to indicate a statistically significant difference.
Results
Patients’ characteristics
The subjects for this study were 73 patients with ADPKD (28 men and 45 women, median age 48 years, age range 21–72 years). The diagnosis of ADPKD was made using the Japanese criteria of the Ministry of Health, Labor, and Welfare. Table 1 shows the baseline characteristics of the patients in this study. The baseline median eGFR, and TKV were 55.3 ml/min/1.73 m2 (range 7.2–120.6 ml/min/1.73 m2), and 1595.9 ml (range 404.7–9652.0 ml) respectively. The median baseline left TKV and right TKV were 755.3 ml (range 190.0–3629.0 ml) and 786.9 ml (range 176.7–7915.1 ml), respectively. There was no significant difference between the baseline left and right TKVs (p = 0.49).
Of 73 patients, 38 (52.1%) were treated with antihypertensive therapy. In these patients treated with antihypertensive therapy, 36 patients (94.7%) took some kinds of angiotensin receptor blocker (ARB) or angiotensin-converting enzyme inhibitor (ACEI). Compared with patients treated without ARB or ACEI, eGFR was significantly reduced in patients treated with ARB or ACEI (with ARB or ACEI 48.388 ± 23.168 ml/min/1.73 m2, without ARB or ACEI 62.166 ± 25200 ml/min/1.73 m2, p = 0.002). This is partly because blood pressure is significantly low in these patients compared with patients treated without ARB or ACEI (SBP; with ARB or ACEI 138.6 ± 18.6 mmHg, without ARB or ACEI 128.6 ± 15.7 mmHg, p = 0.002: DBP; with ARB or ACEI 83.7 ± 8.7 mmHg, without ARB or ACEI 78.3 ± 11.4 mmHg, p = 0.004). There are no significant differences in albuminuria and TKV between patients with or without ARB or ACEI (albuminuria; with ARB or ACEI 134.9 ± 192.4 mg/day, without ARB or ACEI 162.6 ± 344.4 mg/day, p = 0.735: TKV; with ARB or ACEI 2012.3 ± 1144.6 ml, without ARB or ACEI 1724.4 ± 1338.4 ml, p = 0.207).
The relationship between eGFR and other clinical parameters
eGFR was significantly inversely correlated with age (r = −0.570, p = 0.000), TKV (r = −0.318, p = 0.000), proteinuria (r = −0.246, p = 0.0497), albuminuria (r = −0.278, p = 0.038), SAP (r = −0.350, p = 0.000), DAP (r = −0.345, p = 0.000), BMI (r = −0.338, p = 0.000), and PWV (r = −0.461, p = 0.000) (Table 2). The relationship between eGFR and TKV over the course of the study using all data points for each patient is shown in Fig. 1. eGFR was inversely related with the renal volumetric indices (y = −0.0052x + 64.316, r = −0.313, p = 0.000) (Fig. 1). Compared with the normal renal function group (eGFR ≥60 ml/min/1.73 m2), TKV in deteriorated renal function group (eGFR <60 ml/min/1.73 m2) was significantly large (2306.8 ± 1394.5 vs. 1640.9 ± 1334.5 ml, p = 0.005).
Using the 8 significantly inversely correlated factors identified on univariate analysis, multivariate linear regression analysis was performed to determine the independent predictors of baseline eGFR. Multivariate linear regression showed that eGFR was significantly and independently inversely correlated only with age (p = 0.001) and BMI (p = 0.020) (Table 2).
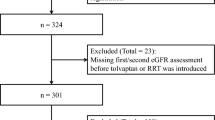
The relationship between the change in eGFR per year (ΔeGFR/y) and other clinical parameters
Thirty-nine patients had at least two sequential examinations. The median follow-up period was 28.5 months (range 3–94 months). During the follow-up period, 111 evaluations were performed (median 2.8 times/patient). The median change in eGFR per year (ΔeGFR/y) was −2.8 ml/min/1.73 m2/year. Figure 2 showed that eGFR decreased in most patients. ΔeGFR/y was significantly inversely correlated with ΔTKV/y (r = −0.674, p = 0.000, Fig. 3), Δu-pro/y (r = −0.663, p = 0.014), and ΔSAP/y (r = −0.473, p = 0.004) (Table 3). Multiple linear regression showed that ΔeGFR/y was significantly and independently inversely correlated with ΔTKV/y (p = 0.039) (Table 3). Consequently, the changes in TKV are a surrogate marker of renal function in ADPKD patients.
The relationship between the change in TKV per year (ΔTKV/y) and other clinical parameters
Assuming an exponential growth kinetic with a constant growth rate, the median change in TKV per year (ΔTKV/y) was 53.9 ml (Fig. 4). Figure 4 shows that TKV increased in most patients but decreased in some. In 8 of 39 patients (20.5%), a substantial reduction of TKV was seen. The ΔTKV/y was significantly correlated with initial TKV (r = 0.915; p = 0.000), initial DAP (r = 0.786; p = 0.007), initial ABI (r = 0.656; p = 0.040), and change in albuminuria per year (Δu-alb/y) (r = 0.902; p = 0.000), and inversely correlated with ΔABI/y (r = −0.770; p = 0.009) (Table 4). Multiple linear regression showed that ΔTKV/y was significantly related to initial TKV (p = 0.025) and Δu-alb/y (p = 0.017) (Table 4). Accordingly, subjects with greater initial renal volume and greater changes in albuminuria had a significantly larger increase in renal volume.
Discussion
In most patients with ADPKD, renal function typically remains within the normal range for several decades, despite progressive renal enlargement. Compensatory hyperfiltration in surviving nephrons initially maintains serum creatinine levels at or near normal values; when levels start to rapidly rise appreciably above baseline, more than 50% of functioning parenchyma has been destroyed. It is only around the age of 40 years that renal function begins to decrease rather rapidly, leading to end-stage failure within about 10 years [5]. To monitor the progression of ADPKD, GFR has several limitations as a biomarker. GFR often does not decline until renal function damage is well established. Accordingly, GFR has no predictive value in the early stages of the disease, and it only becomes a useful indicator of renal function after major, irreversible damage to renal function has occurred [10]. In ADPKD, by the time that GFR has declined, renal volume has already substantially expanded, because renal cysts have already destroyed much of the renal parenchyma [1]. Consequently, measuring GFR alone has not been sufficient for the assessment of disease progression, especially in the early phase [11].
In Caucasian patients with ADPKD, at baseline, GFR decreased by 2.8 ± 2.8 ml/min/1.73 m2/year [12] and 2.4 ± 2.8 ml/min/1.73 m2/year [13] per year. The median ΔeGFR/y in this study was −2.8 ml/min/1.73 m2/year. Accordingly, our data for the changes in GFR in Japanese ADPKD patients were in agreement with published Caucasian data. However, the rate of decline in the GFR of 2–3 ml/min per year in patients with ADPKD is so small that it is difficult to detect the benefit of any therapies. Thus, a tool that detects small changes in ADPKD early enough has been needed. An impressive body of evidence demonstrates that the kidneys of patients with ADPKD increase progressively in size from birth [1, 8, 10, 12–14]. The CRISP study [1] demonstrated that kidney growth occurs in an exponential fashion and that the growth of kidneys in patients with ADPKD is primarily the result of the growth of cysts.
The combined volume of polycystic kidneys in adults commonly exceeds 4000 ml, as compared with normal volumes of 308 ml in women and 404 ml in men [1, 15]. At baseline, TKV amounted to 1076 cm3 [1] and increased at a mean rate of a range from 4.0% [12] to 9.4% [14], 24 ± 22 cm3 [12], 46 ± 55 cm3 [13], and 54 ± 10 cm3 [14] per year in several studies. Assuming an exponential growth kinetic with a constant growth rate, the calculated median annual growth volume was 53.9 ml in our study and, hence, very similar to the CRISP results. Since ADPKD progresses in accordance with the increasing size of a very large number of renal cysts, which cause the whole kidney to enlarge, the sequential measurement of total kidney and cyst volume has been suggested as a surrogate marker of disease progression [1, 16]. According to the recent data, the most objective test to assess and monitor disease progression is MR-based estimation of total renal volume. Several studies revealed that the rates of increase in TKV were highly variable and that the patients with fast rates of growth were likely to exhibit more serious declines in GFR than patients who exhibited slower growth rates [10, 17]. It was reported that inverse correlations existed between TKV and GFR [6, 13], and between the rate of increase in kidney volume and the rate of decrease in GFR [12, 13]. CRISP analyzed the results of serial assessment of the total volume of kidneys and cysts in 232 American patients with ADPKD who had preserved renal function at baseline [1] and demonstrated that renal volume exceeding 1500 ml is associated with a decrease in GFR and rapid progression of the disease [1, 2, 5, 11]. The initial TKV, the initial cyst volume, the initial percent cyst volume, and the changes in TKV were significantly greater in the renal failure group than in the normal renal function group (p < 0.001) [6, 13, 17]. MRI has been shown to be a more sensitive biomarker of disease progression than either serum creatinine or eGFR, and is already being used as a surrogate outcome for increases in creatinine in clinical trials. Multiple linear regressions showed that ΔeGFR/y was significantly inversely correlated with ΔTKV/y independently in this study (Table 3). Consequently, the changes in TKV are considered a surrogate marker of renal function in Japanese ADPKD patients.
To quantify the progression of ADPKD, sufficient sensitivity and reproducibility are required to enable the measurement of relatively small changes in renal and cyst volume [15]. The error in renal volume estimated using MRI is <5% [18]. Currently, the efficacy of various new drugs has been tested in clinical trials, including the mTOR inhibitors sirolimus (rapamycin) [19] and everolimus [20], the vasopressin V2 receptor antagonist tolvaptan [21], and the somatostatin analogue octreotide acetate [22]. In those trials, indices associated with TKV were standard measures in the assessment of ADPKD progression, although their utility in monitoring individual patients has not been established. Consequently, further studies are needed to verify the volumetric indices as an indicator of disease progression.
It is known that albuminuria increases with disease progression. A previous cross-sectional study showed that overt proteinuria (protein >300 mg/day) was associated with larger renal volumes, higher blood pressures, and lower creatinine clearances in patients with ADPKD [23]. The computed tomographic study of King et al. [12] involving nine patients with ADPKD showed that subjects with greater initial proteinuria had a significantly larger increase in renal volume and decline in GFR than those with less proteinuria. In this study, the subjects with greater initial renal volume and greater changes in albuminuria had a significantly larger increase in renal volume. Our results are in line with these previous studies, since TKV at baseline was positively correlated with hypertension, hematuria, and albuminuria, and albuminuria was associated with accelerated volume progression [8].
It has been previously reported that vascular endothelial dysfunction was present in small resistance vessels obtained from ADPKD patients. In this study, although eGFR was significantly inversely correlated with PWV on univariate analysis (Table 2), there are no significant correlations between eGFR and PWV on multivariate analysis. Consequently, we could not conclude the causal relationship between vascular endothelial dysfunction and ADPKD.
It is well established that the control of blood pressure is essential to prevent end-stage renal disease (ESRD) in ADPKD patients. We evaluated the efficacy of ARB or ACEI for ADPKD patients supplementarily. In this study, eGFR was significantly reduced in patients with ARB or ACEI compared with the patients without these drugs, mainly presumably because of significant high blood pressure. Consequently, we could not indicate the efficacy of antihypertensive therapy using ARB or ACEI in this study.
One limitation of this study is that it was a retrospective study, and selection bias may have been present. Another limitation is the technique to quantify TKV. We measured TKV on MRI manually, while other techniques are automatic [15]. Manual operation may have some skewedness and inconsistency. Meanwhile, fully automated segmentation is feasible for normal kidneys. However, this operation is exceedingly difficult when evaluating the kidneys of patients with ADPKD, since ADPKD has high variability in kidney morphology [15]. Moreover, markedly enlarged ADPKD kidneys often compress and distort surrounding healthy anatomical structures, which makes automatic discrimination of the anatomical boundaries of the kidneys challenging. Proper assessment of TKV warrants further studies.
To sum up, this study demonstrates a significant relationship between renal volume and renal function in Japanese ADPKD patients without renal insufficiency. Total renal volume possesses sufficient accuracy and reproducibility to be used to assess disease progression. The volume measurements can be used as useful markers for the progression of disease in Japanese ADPKD patients.
References
Grantham JJ, Torres VE, Chapman AB, Guay-Woodford LM, Bae KT, King BF Jr, et al. Volume progression in polycystic kidney disease. N Engl J Med. 2006;354:2122–30.
Chapman AB, Guay-Woodford LM, Grantham JJ, Torres VE, Bae KT, Baumgarten DA, et al. Renal structure in early autosomal-dominant polycystic kidney disease (ADPKD): the Consortium for Radiologic Imaging Studies of Polycystic Kidney Disease (CRISP) cohort. Kidney Int. 2003;64:1035–45.
Higashihara E, Nutahara K, Kojima M, Tamakoshi A, Yoshiyuki O, Sakai H, et al. Prevalence and renal prognosis of diagnosed autosomal dominant polycystic kidney disease in Japan. Nephron. 1998;80:421–7.
Fick-Brosnahan GM, Tran ZV, Johnson AM, Strain JD, Gabow PA. Progression of autosomal-dominant polycystic kidney disease in children. Kidney Int. 2001;59:1654–62.
Torres VE, Harris PC, Pirson Y. Autosomal dominant polycystic kidney disease. Lancet. 2007;369:1287–301.
Lee YR, Lee KB. Reliability of magnetic resonance imaging for measuring the volumetric indices in autosomal-dominant polycystic kidney disease: correlation with hypertension and renal function. Nephron Clin Pract. 2006;103:c173–80.
Cadnapaphornchai MA, McFann K, Strain JD, Masoumi A, Schrier RW. Prospective change in renal volume and function in children with ADPKD. Clin J Am Soc Nephrol. 2009;4:820–9.
Kistler AD, Poster D, Krauer F, Weishaupt D, Raina S, Senn O, et al. Increases in kidney volume in autosomal dominant polycystic kidney disease can be detected within 6 months. Kidney Int. 2009;75:235–41.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Grantham JJ, Chapman AB, Torres VE. Volume progression in autosomal dominant polycystic kidney disease: the major factor determining clinical outcomes. Clin J Am Soc Nephrol. 2006;1:148–57.
Perrone R. Imaging progression in polycystic kidney disease. N Engl J Med. 2006;354:2181–3.
King BF, Reed JE, Bergstralh EJ, Sheedy PF 2nd, Torres VE. Quantification and longitudinal trends of kidney, renal cyst, and renal parenchyma volumes in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2000;11:1505–11.
Fick-Brosnahan GM, Belz MM, McFann KK, Johnson AM, Schrier RW. Relationship between renal volume growth and renal function in autosomal dominant polycystic kidney disease: a longitudinal study. Am J Kidney Dis. 2002;39:1127–34.
Sise C, Kusaka M, Wetzel LH, Winklhofer F, Cowley BD, Cook LT, et al. Volumetric determination of progression in autosomal dominant polycystic kidney disease by computed tomography. Kidney Int. 2000;58:2492–501.
Bae KT, Grantham JJ. Imaging for the prognosis of autosomal dominant polycystic kidney disease. Nat Rev Nephrol. 2010;6:96–106.
Grantham JJ. Autosomal dominant polycystic kidney disease. N Engl J Med. 2008;359:1477–85.
Gabow PA, Johnson AM, Kaehny WD, Kimberling WJ, Lezotte DC, Duley IT, et al. Factors affecting the progression of renal disease in autosomal-dominant polycystic kidney disease. Kidney Int. 1992;41:1311–9.
Bae KT, Commean PK, Lee J. Volumetric measurement of renal cysts and parenchyma using MRI: phantoms and patients with polycystic kidney disease. J Comput Assist Tomogr. 2000;24:614–9.
Qian Q, Du H, King BF, Kumar S, Dean PG, Cosio FG, et al. Sirolimus reduces polycystic liver volume in ADPKD patients. J Am Soc Nephrol. 2008;19:631–8.
Edelstein CL. Mammalian target of rapamycin and caspase inhibitors in polycystic kidney disease. Clin J Am Soc Nephrol. 2008;3:1219–26.
Torres VE. Role of vasopressin antagonists. Clin J Am Soc Nephrol. 2008;3:1212–8.
Hogan MC, Masyuk TV, Page LJ, Kubly VJ, Bergstralh EJ, Li X, et al. Randomized clinical trial of long-acting somatostatin for autosomal dominant polycystic kidney and liver disease. J Am Soc Nephrol. 2010;21:1052–61.
Chapman AB, Johnson AM, Gabow PA, Schrier RW. Overt proteinuria and microalbuminuria in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 1994;5:1349–54.
Acknowledgments
This work was supported in part by a grant for the Progressive Renal Diseases Research Project from the Ministry of Health, Labour and Welfare of Japan.
Conflict of interest
The authors have declared that no conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Tokiwa, S., Muto, S., China, T. et al. The relationship between renal volume and renal function in autosomal dominant polycystic kidney disease. Clin Exp Nephrol 15, 539–545 (2011). https://doi.org/10.1007/s10157-011-0428-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-011-0428-y