Abstract
Background
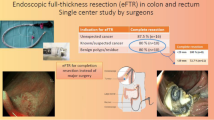
Endoscopic full-thickness resection (EFTR) significantly expands the spectrum of endoscopic colorectal resection methods for lesions that show no lifting sign, submucosal lesions and mucosal carcinomas. The aim of our study was to evaluate the efficacy and safety of EFTR using a commercially available full thickness resection device (FTRD) by assessing the completeness of the full-thickness resection, the technical success, as well as complications in a cohort of patients from three referral centers in Germany. Another aim was to determine which patient subpopulations benefit most in clinical practice.
Methods
This retrospective multicenter study was conducted on consecutive patients who were admitted to three referral centers in Germany between November 2014 and December 2017. The EFTR was conducted according to the standard indications using the FTRD System (OVESCO, Tübingen, Germany). Data were obtained from prospectively maintained institutional databases.
Results
There were 70 patients, 42 males and 25 females with a mean age of 79.5 years (range 25–89 years) who had colonoscopy for EFTR. In three patients EFTR was not feasible because the lesions were too large. Of the remaining 67 patients, 52 had recurrent adenomas, 10 had high-grade intraepithelial neoplasia or mucosal carcinoma and five had a subepithelial lesion. Resection was technically successful in 65 patients (97.0%). Histologically complete resection (R0) was achieved in 59/65 patients (90.8%). The R0 resection rate was lower for lesions > 20 mm (86.5%) versus lesions ≤ 20 mm (92.9%). The total complication rate was 14.9%: there was one major complication (perforation of sigmoid colon), while all other complications were minor.
Conclusions
EFTR yields excellent resection rates for benign recurrent adenomas with non-lifting sign, advanced histopathological findings or submucosal lesions when the procedure is performed in experienced hands and for the correct indication. Thus, surgery can be avoided in many cases. For all lesions the risk of R1 resection goes up with the size of the lesion and careful patient selection is mandatory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Snare-polypectomy, endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) are well-established methods for the endoscopic treatment of colorectal lesions such as colorectal adenomas with low- or high-grade dysplasia and early mucosal cancer [1,2,3,4]. However, subsequent histopathological examination of the resected tissue may show signs of incomplete resection with the necessity for additional treatment. These cases, as well as recurrent adenomas, lesions showing no lifting sign (failure of a lesion to elevate above the surrounding mucosa after submucosal injection), and mucosal T1-carcinomas are a major challenge for endoscopists. Conventional resection techniques may not be applicable here. To overcome these limitations, endoscopic full-thickness resection (EFTR) approaches have been developed. The commercially available full-thickness resection device (FTRD®, Ovesco Endoscopy, Tübingen, Germany) was first described in 2011 by Schurr et al. [5], it is European Conformity (CE)-marked for colorectal EFTR since September 2014 and several reports confirmed the feasibility and safety of this technique [6, 7] when used for therapeutic purposes. Another advantage of EFTR is the possibility of obtaining a better histological evaluation with a concomitant closure of the colon wall defect, avoiding abdominal contamination. EFTR also proved to be effective for endoscopic treatment of small submucosal tumors, for R0-resection of small neuroendocrine tumors (NET) of the rectum and for diagnostic purposes (e.g., for diagnosing Hirschsprung’s disease or chronic al pseudo-obstruction) [8, 9]. One major limitation of this technique is the size of the lesion that can be resected, which corresponds to the amount of tissue that can be grasped in the cap [10, 11]. It may also be difficult to advance the endoscope through the colon with the FTRD-system mounted and thus limiting flexibility and visibility which results in a higher risk of perforation. The aim of our study was to evaluate the efficacy and safety of EFTR with FTRD by assessing the completeness of the full-thickness resection, the technical success, as well as complications in a cohort of patients from three referral centers in and determine which patient group benefits the most from this endoscopic intervention.
Materials and methods
A retrospective multicenter study was conducted patients who were admitted to three reference referral centers in Germany between November 2014 and December 2017. The EFTR was conducted according to the standard indications using the FTRD System (OVESCO, Tübingen, Germany). Data were obtained from prospectively maintained institutional databases.
Inclusion criteria were as follows: patients with colorectal lesions which were difficult or not possible to resect with conventional endoscopic methods like polypectomy, EMR or ESD; patients with an adenoma involving the appendiceal orifice and patients with submucosal lesions. All patients had undergone complete colonoscopy before inclusion. Patients < 18 years of age, pregnant women, patients without a signed informed consent form, or with coagulopathy were excluded from the study. The following parameters were recorded: indication for EFTR, anatomical site of the lesion, technical success (defined as appropriate grasping of the lesion, deployment of the OTSC and en bloc resection), clinical success (histologically proven clear-resection margins = R0 resection) and complications. All patients gave their written informed consent for endoscopy, as well as for the publication of their medical data. The study was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee. All endoscopies were performed in an inpatient setting under moderate-to-deep sedation with propofol (± midazolam or + pethidine). Intravenous butylscopolamine was given at discretion of the operator to reduce bowel peristalsis. All endoscopic procedures were done with CO2 insufflation. Blood pressure, heart rate and oxygen saturation were constantly monitored during the procedure. All patients received prophylactic antibiotic therapy peri-interventionally (broadspectrum coverage for Gram-negative and Gram-positive bacteria). Patients on acetylsalicylic acid were advised to continue the medication; all other anticoagulants (clopidogrel, heparin, warfarin or direct oral anticoagulants) were discontinued. The EFTR was performed with the full-thickness resection device (FTRD, Ovesco Endoscopy, Tübingen, Germany) following a standardized method (Fig. 1). The FTRD consists of an over-the-scope-clip (OTSC) system cap with a 14-mm distally integrated monofilament polypectomy snare. The cap has an inner diameter of 13 mm and a length of 23 mm (measured from the tip of the endoscope). The snare handle runs along the outer surface of the colonoscope, under a plastic sheath that is fixed to the instrument. First resection area limits were marked using coagulation with a delivered probe included in the resection device. Then a forceps (FTRD grasper) is used via the operating channel to grasp and pull the lesion inside the cap. Immediately afterwards, the OTSC is released and the lesion is resected en bloc above the clip using the pre-mounted electrosurgical snare included in the device. After the procedure, patients were monitored for at least one night. Post-polypectomy syndrome was defined as the development of abdominal pain, fever and leukocytosis due to the peritoneal inflammation in the absence of perforation after resection.
Schematic description of the full-thickness resection device (FTRD) technique (www.ovesco.com). a Components of the FTRD: The clip is mounted on the tip of the endoscope. The snare is integrated in the tip of the cap. A grasping forceps is advanced through the working channel of the endoscope. b The target lesion is grasped with the forceps. c The target lesion is pulled into the cap. d The over-the-scope-clip (OTSC) is deployed and creates a full-thickness duplication of the colonic wall. e The pseudopolyp above the clip is resected using the preloaded snare
Results
From November 2014 to December 2017, 70 patients, 42 males and 25 females, with a mean age of 79.5 years (range 25–89 years) had EFTR. Three patients had to be excluded because the lesions were too large (> 4 cm), thus the total study group consisted of 67 patients, Patient and lesion characteristics are shown in Table 1.
The mean size of the resection specimen was 19 × 23 mm (range 5–26 mm for the minor axis and 9–37 mm for the major axis). Lesions were located in the rectum (n = 19), the sigma (n = 14), the descending colon (n = 6), the transverse colon (n = 4), within the right flexure (n = 3), the ascending colon (n = 15) and the cecum (n = 6). Resection was technically successful (macroscopically complete and en bloc) in 65/67 patients (97.0%). No significant differences in resection success were observed between the participating centers. In one case there was a snare dysfunction which led to termination of the intervention (1.4% technical failure). The resection was then completed with a conventional snare. In one other case difficulties of incorporation of the lesion into the cap was reported, which led to termination of the procedure. The median procedure time was 95.5 min (range 48–143 min).
In the total cohort, histologically complete resection (R0) was achieved in 59/65 patients with complete histological assessment (90.8%). The R0 resection rate dropped with increasing lesion size of the neoplastic lesion. R0 resection rate was lower for lesions > 20 mm (86.5%) versus lesions ≤ 20 mm (92.9%, n.s.).
In the subgroup of patients with non-lifting neoplasms (n = 52, see Fig. 2) 6 patients (11.5%) whose lesions had initially been classified as benign had unsuspected cancer on histology. In two cases in this group (3.8%), histology was not obtained due to unsuccessful snare resection.
Final histology of the remaining 44 cases was: adenoma with low-grade dysplasia (n = 28, 63.6%), adenoma with high-grade dysplasia (n = 4, 9.0%), hyperplastic or scar tissue (n = 11, 25%) and one inverted diverticulum (2.2%). The R0 resection rate in this group was 100%. Three-month follow-up data could be obtained from 34 patients in this group showing two cases of recurrent lesions (5.8%) which were then referred to surgery.
Final histology in the subgroup of patients with malignancy (n = 16, see Fig. 2) was: mucosal carcinoma (n = 15, 93.7%) and 1 metastasis of a malignant melanoma (6.2%) (Fig. 3). R0 resection could be verified in 10 cases (10/16; 62.5%), in 6 cases (37.5%) there was R1 or deeper submucosal invasion (sm2/sm3). These cases were referred to surgery. In the group of patients with R0 resection (n = 10) 3-month follow-up data could be obtained from eight patients showing no residual tumor, while unfortunately the remaining two patients were lost to no follow-up.
In patients with subepithelial tumors (n = 5), final histological examination showed neuroendocrine tumor (all well differentiated G1) in all cases. R0 resection was achieved in all patients in this group (100%) and 3-month follow-up data showed no residual tumor in all cases.
Complications
In one case (1.4%) a perforation of the sigmoid colon occurred during the FTRD colonoscopy which resulted in referring the patient to surgery.
In three other cases (4.4%) minor bleeding (with drop in hemoglobin levels < 2 g/l) occurred at the resection site as delayed bleeding (1–3 days after the procedure). Sustained hemostasis was achieved endoscopically after the injection of saline-diluted epinephrine and the application of hemoclips in all three cases.
Six patients (8.9%) developed a post-polypectomy syndrome with abdominal pain, fever and signs of inflammation on blood chemistry tests. Intestinal perforation was ruled out radiologically in all these patients. All patients with post-polypectomy syndrome were managed conservatively with intravenous hydration, antibiotics, and analgesics.
Thus, the overall complication rate was 14.9%, consisting mostly of minor complications. There were no complications associated with sedation. The adverse events were evenly distributed among the participating centers.
Discussion
The study demonstrated a total technical success rate of 97.0% which is in accordance with other studies which report technical success rates ranging from 75 to 100% [7, 11,12,13,14]. In our unselected real-world population from daily clinical practice, a histologically complete resection (R0) was achieved in 90.8% of all our patients (n = 67). Thus, we conclude that EFTR reaches similarly high or even better R0 resection rates when performed by experienced endoscopists as recently described in the WALL RESECT study by Schmidt et al. with a overall R0 rate of 76.9% [18]. In a study by Aepli et al. on a somewhat smaller patient population (33 patients) a R0 resection rate of 80.6% was obtained [19]. However, the success rate for R0 resection depends on several factors, not only on endoscopists’ colonoscopic experience, but also on the site of the neoplastic lesion within the colon, its size and its microscopic invasiveness, and visibility of the lesion when the FTRD cap is fitted on the endoscope.
In our study, the mean size of the resected samples was 19 × 23 mm, in line with data from the literature [7, 12]. According to the literature EFTR is suitable for non-lifting lesions ranging from 5 to 25 mm, but polyps up to 40 mm diameter and even larger have been successfully removed [7, 12]. Notably, the R0 resection rate was lower for lesions > 20 mm (86.5%) than for lesions ≤ 20 mm (92.9%). This again underlines the need for patient selection as bigger lesions are associated with a higher risk for R1 resection prompting further interventions, or an initial surgical approach [17]. With this awareness a new strategy for difficult colonic resections may be the combination of conventional snare-EMR for elevated (polypoid) areas and subsequent EFTR for the remaining (flat) center of the lesions.
The most frequent indications for EFTR in our study were adenomas with a primary non-lifting sign and recurrent adenoma displaying a non-lifting sign after prior polypectomy. While complete histologic resection with R0 was achieved in 90.8% of our cohort, EFTR was found to yield a higher R0 resection rate in the group of recurrent or non-lifting adenoma, reaching 100% when adenoma size was smaller than 4 cm for cap insertion. Thus, EFTR is most helpful in the latter subgroup to avoid surgery: in our preliminary follow-up only 5.8% of the patients developed a recurrence. Furthermore, these cases with recurrence could probably benefit from a second EFTR attempt. If EFTR had not been available in the study period, these patients would have undergone surgery or a somewhat higher risk attempt to resect the lesion by ESD. This is an important issue, as the risk of perforation with conventional techniques like EMR and ESD in such cases of unsuccessful submucosal fluid injection or adenoma recurrence may reach 15% [15, 16].
The FTRD system itself is designed in a way that it allows complete and reliable closure of the colonic wall by applying an OTSC immediately before snare resection of the enclosed specimen. Thus, the risk of colonic perforation is reduced in experienced hands. In our series the only 1 case of perforation (1.4%) occurred (the patient was managed surgically). With regard to cost-effectiveness, in the treatment of patients with non-lifting benign neoplasms of the colon EFTR appears to have clear advantages over EMR and ESR concerning complication rates and recurrence rates [1,2,3, 17] However, the 1- and 5-year recurrence rates after EFTR from all current studies should be published to allow a strict data comparison for the available colonic resection techniques.
Endoscopic resection with EMR or ESD within the cecum and the cecal appendix is considered to be associated with a high risk of perforation [7, 12, 14, 16, 17]; therefore, these lesions have mainly been managed primarily by surgery. EFTR offers an additional approach for therapeutic resection with reduced morbidity and mortality in such cases. In our study we were able to include two patients with difficult adenomas in the appendiceal orifice. Both were safely and efficiently R0 resected with partially endoscopic appendectomy and without complications. However, appendiceal lesions are not an established indication for EFTR unless the detailed location of the lesion, its growth pattern and size have been demonstrated and discussed with the surgeon, because major complications may arise from endoscopic resection in this peculiar region [17].No post-interventional appendicitis or peritonitis occurred in our cohort. Schmidt et al. reported a rate of 8.8% post-interventional appendicitis in their subgroup of 34 patients with adenomas at the appendiceal orifice (total cohort: n = 181) requiring laparoscopic appendectomy [18]. Aepli et al. on the other hand reported an uneventful post-interventional course in two cases where they performed EFTR at the appendiceal orifice [19].
Our median procedure time was 95.5 min, which is somewhat longer than in comparable studies [14,15,16,17]. This may primarily be due to the time-consuming advancement of the FTRD-fitted endoscope to target lesions in more proximal anatomical sites and not to the procedure itself, but may also be due to more efforts to clean the resection site to adequately visualize the neoplastic lesion, or to the time needed to precisely insert the tissue into the FTRD cap. Thus, these technical steps can influence on the R0 resection rate and EFTR should be performed by experienced investigators without time constraints. A quite common side effect of EFTR is the post-polypectomy syndrome, due to a peritoneal reaction after resection, which we observed in 6 patients in our cohort (6/67; 8.9%), which is in line with other published data [7, 12, 14]. Nevertheless, one must be cognizant that EFTR is an invasive method: the endoscopist needs to be highly experienced, capable of treating any adverse events and surgeons should be pre-emptively involved to optimize outcome [16, 17]. Otherwise, EFTR runs into a risk that more adverse events will occur if sufficiently large numbers of procedures are performed.
Limitations of our study include its retrospective design, the small number of patients and the short-term follow-up. Also, we did not assess the overall cost of EFTR procedures. Despite these limitations, based on our data, we conclude that EFTR is a good alternative to ESD or EMR in the resection of recurrent adenomas or no-lifting lesions as well as small submucosal tumors. EFTR is a simpler and less time-consuming procedure than the alternative treatments, such as open or laparoscopic surgery or ESD. The procedure is safe and can be performed under moderate to deep conscious sedation without the need of tracheal intubation. The major limitations of EFTR are the maximum size of the resectable lesions and the possibly limited endoscopic view which aggravates the advancement of the scope through the sigmoid or colonic flexures.
References
Maguire LH, Shellito PC (2014) Endoscopic piecemeal resection of large colorectal polyps with long-term follow up. Surg Endosc 28:2641–2648
Pellise M, Burgess NG, Tutticci N, Hourigan LF, Zanati SA, Brown GJ, Singh R, Williams SJ, Raftopoulos SC, Ormonde D, Moss A, Byth K, P’Ng H, Mahajan H, McLeod D, Bourke MJ (2017) Endoscopic mucosal resection for large serrated lesions in comparison with adenomas: a prospective multicentre study of 2000 lesions. Gut 66:644–653
Kuroki Y, Hoteya S, Mitani T, Yamashita S, Kikuchi D, Fujimoto A, Matsui A, Nakamura M, Nishida N, Iizuka T, Yahagi N (2010) Endoscopic submucosal dissection for residual/locally recurrent lesions after endoscopic therapy for colorectal tumors. J Gastroenterol Hepatol 25:1747–1753
Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH (2015) Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 47:829–854
Schurr MO, Baur F, Ho CN, Anhoeck G, Kratt T, Gottwald T (2011) Endoluminal full-thickness resection of GI lesions: a new device and technique. Minim Invasive Ther Allied Technol 20:189–192
Schmidt A, Bauerfeind P, Gubler C, Damm M, Bauder M, Caca K (2015) Endoscopic full-thickness resection in the colorectum with a novel over-the- scope device: first experience. Endoscopy 47:719–725
Valli PV, Kaufmann M, Vrugt B, Bauerfeind P (2014) Endoscopic resection of a diverticulum-arisen colonic adenoma using a full-thickness resection device. Gastroenterology 147:969–971
Soriani P, Tontini GE, Neumann H, de Nucci G, De Toma D, Bruni B, Vavassori S, Pastorelli L, Vecchi M, Lagoussis P (2017) Endoscopic full-thickness resection for T1 early rectal cancer: a case series and video report. Endosc Int Open 5(11):E1081–E1086
Grauer M, Gschwendtner A, Schäfer C, Neumann H (2016) Resection of rectal carcinoids with the newly introduced endoscopic full-thickness resection device. Endoscopy 48(Suppl 1):E123–E124
Schmidt A, Meier B, Caca K (2015) Endoscopic full-thickness resection: current status. World J Gastroenterol 21:9273–9285
Faehndrich M, Sandmann M (2015) Endoscopic full-thickness resection for gastrointestinal lesions using the over-the-scope clip system: a case series. Endoscopy 47:76–79
Andrisani G, Pizzicannella M, Martino M, Rea R, Pandolfi M, Taffon C, Caricato M, Coppola R, Crescenzi A, Costamagna G, Di Matteo FM et al (2017) Endoscopic full-thickness resection of superficial colorectal neoplasms using a new over-the-scope clip system: a single-centre study. Dig Liver Dis 49:1009–1013
Richter-Schrag HJ, Walker C, Thimme R, Fischer A (2016) Full thickness resection device (FTRD). Experience and outcome for benign neoplasms of the rectum and colon. Chirurg 87:316–325
Vitali F, Naegel A, Siebler J, Neurath MF, Rath T (2018) Endoscopic full-thickness resection with an over-the-scope clip device (FTRD) in the colorectum: results from a university tertiary referral center. Endosc Int Open 6(1):E98–E103
Valli PV, Mertens J, Bauerfeind P (2018) Safe and successful resection of difficult GI lesions using a novel single-step full-thickness resection device (FTRD®). Surg Endosc 32(1):289–299
Hagel AF, Boxberger F, Dauth W, Kessler HP, Neurath MF, Raithel M (2012) Colonoscopy-associated perforations—a 7 year survey on in-hospital examinations: frequency, treatment and outcome in a German university hospital. Colorectal Dis 14(9):1121–1125
Tate DJ, Desomer L, Awadie H, Goodrick K, Hourigan L, Singh R, Williams SJ, Bourke MJ (2018) EMR of laterally spreading lesions around or involving the appendiceal orifice: technique, risk factors for failure, and the outcomes of a tertiary referral cohort. Gastrointest Endosc 87(5):1279–1288
Schmidt A, Beyna T, Schumacher B, Meining A, Richter-Schrag HJ, Messmann H, Neuhaus H, Albers D, Birk M, Thimme R, Probst A, Faehndrich M, Frieling T, Goetz M, Riecken B, Caca K (2018) Colonoscopic full-thickness resection using an over-the-scope device: a prospective multicentre study in various indications. Gut 67(7):1280–1289
Aepli P, Criblez D, Baumeler S, Borovicka J, Frei R (2018) Endoscopic full thickness resection (EFTR) of colorectal neoplasms with the Full Thickness Resection Device (FTRD): clinical experience from two tertiary referral centers in Switzerland. United Eur Gastroenterol J 6(3):463–470
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. H. Albrecht, Prof. Dr. M. Raithel, Mr. A. Braun, Dr. A. Nagel, Dr. A. Stegmaier, Dr. K. Utpatel and Prof. Dr. C. Schäfer have no conflicts of interest or financial ties to disclose.
Ethical approval
The study was conducted according to the declaration of Helsinki.
Informed consent
All participants provided informed consent prior to their participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Albrecht, H., Raithel, M., Braun, A. et al. Endoscopic full-thickness resection (EFTR) in the lower gastrointestinal tract. Tech Coloproctol 23, 957–963 (2019). https://doi.org/10.1007/s10151-019-02043-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-019-02043-5