Abstract
It was the objective of this report to present a case of recurrent aneurysmal subarachnoid hemorrhage (SAH) and intracerebral hemorrhage (ICH) in which an MCA aneurysm was detected by 3D rotational fluoroscopy in an emergency situation. A 44-year-old woman was admitted from an external department after repeated SAH and temporal ICH. Due to progressive anisocoria and cardiocirculatory instability, she was transferred to the operating room without angiography. After a 3D rotational fluoroscopy baseline scan, another scan with 50 ml of iodine contrast agent was performed. The Digital Imaging and Communications in Medicine (DICOM) data sets were subtracted and reconstructed using the OsiriX® free imaging software. No adverse effect was observed during and after the administration of the contrast agent. The entire procedure from positioning of the fluoroscope to the production of utilizable 3D images was completely integrated into the surgical workflow with an image acquisition time of 2 × 24 s. The configuration of the aneurysm, the aneurysm-carrying vessel, and the distal vessel anatomy were well assessable. This technique quickly supplies images at adequate quality to assess the configuration of an intracranial aneurysm and is a useful diagnostic tool if the patient’s critical condition prohibits aneurysm diagnostics by angiography or CT angiography.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Today, digital subtraction angiography (DSA) is the standard diagnostic procedure for the majority of cerebrovascular pathologies [2, 10]. It carries the advantage of high spatial resolution and good image quality. However, DSA is time-consuming. In cases of emergency, like subarachnoid hemorrhage (SAH) with space-occupying intracerebral hematoma, the time may be too short to perform DSA. Therefore, CT angiography (CTA) has become the procedure of choice to search for an intracranial aneurysm in these situations [3, 9]. In cases of ongoing brainstem herniation, however, even CTA may delay surgery too long if it has to be performed as a separate procedure and not in immediate connection to a native CT. In these cases, surgery has to be performed without information about the exact location and configuration of the aneurysm.
3D fluoroscopy is available in many neurosurgical centers and mainly used for spine surgery. It is easy and quick to handle. In this article, we report about the attempt to depict an intracranial aneurysm by intraoperative 3D rotational fluoroscopy and intravenous contrast administration in a case of emergency in a patient who suffered intracerebral hemorrhage (ICH) from a ruptured intracranial aneurysm.
Case description
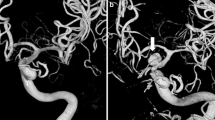
A 44-year-old woman experienced an episode of acute headache and neck pain and was admitted to an external hospital. An initial CT scan detected SAH with a small left temporal intracerebral hemorrhage (ICH) (Fig. 1a). Two hours later, she rapidly deteriorated to a GCS of 7 and had to be analgosedated and intubated. A follow-up CT scan performed at the external hospital showed an increase of the temporal lobe hematoma, a new left frontotemporal subdural hematoma, and an increased midline shift (Fig. 1b). Thereafter, she was transferred to our hospital. Upon arrival at our department, another hour later, the patient had signs of rapidly progressive herniation with cardiocirculatory problems and progressive anisocoria. It was decided to transfer the patient directly into the operating room without obtaining a DSA or another CT combined with a CTA in order to provide rapid decompression and clipping of the aneurysm which was the presumable cause of the recurrent temporal lobe bleeding. In order to possibly obtain additional information about the source of hemorrhage without a delay of surgery, it was decided to attempt imaging of the cerebral vessels for detection of an aneurysm by the use of an available 3D fluoroscope.
Patient positioning and preparation
The head was fixed in a carbon Mayfield clamp and the patient positioned in a supine position on a carbon table. During the hair shave and surgical disinfection, the 3D fluoroscope (O-arm®, Medtronic GmbH, Meerbusch, Germany) was positioned. The appropriate positioning was verified by anteroposterior and lateral fluoroscopy. During the surgeon’s hand disinfection, a 3D rotational fluoroscopy scan was performed. Hereby, 750 images were acquired during a 24-s period without administration of contrast agent. Thereafter, a contrast-enhanced 3D rotational fluoroscopy scan was acquired within the same positions of the table and the 3D fluoroscope. Over 25 s, 50 ml of iodine contrast agent was administered via a 16 gauge central venous catheter. The second 3D rotational scan was started with a delay of 12 s after the beginning of the contrast administration using the same image acquisition parameters. The two Digital Imaging and Communications in Medicine (DICOM) data sets were transferred to an Apple Power Mac® workstation and post-processed by freely available OsiriX® imaging software.
Post-processing of the DICOM data
The data sets were subtracted using the automated subtraction function of the OsiriX® software for sliced DICOM images. From the subtracted data set, a 3D reconstruction was produced, again using an automated function (“Volume Rendering”) of the OsiriX® software. The skull bone was virtually removed from the reconstructed image and the intensity adjusted in order to selectively demonstrate the contrast-filled cerebral vessels. During image processing, sterile draping was attached to the patient. Image processing was performed by the assistant while the surgeon continued the preparations and started surgery.
Imaging
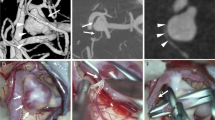
The image reconstruction revealed a complex middle cerebral artery (MCA) aneurysm with both M2 branches originating from a broad aneurysm base on the MCA trunk (Fig. 2).
An axial contrast-enhanced fluoroscopy scan shows a further increase of the temporal ICH (upper left). After subtraction of contrast-enhanced images from baseline images, a reconstruction of the intracranial vessel trunk and relation to the skull base can be evaluated (upper right). After subtraction of bone, the vessel trunk can be rotated in any direction (lateral view = lower left, surgeon’s view = lower right)
Operative course
Skin incision was performed 15 min after arrival in the operating room. After a standard pterional craniotomy, opening of the dura mater, and removal of the subdural hematoma, a re-rupture of the aneurysm occurred. The MCA trunk was temporarily clipped and the aneurysm located and prepared. It showed a broad site of rupture at the temporal face of the aneurysm dome, which was partly occluded only by a firm clot. After removal of the clot, moderate arterial hemorrhage was restarted, indicating a retrograde cross-flow. One of two MCA branches originated close to the rupture site. The aneurysm was occluded by a reconstruction of the MCA bifurcation with three clips. Indocyanine green-enhanced near-infrared angiography showed no more filling of the aneurysm, a rapid filling of the frontal MCA branch, and a delayed filling of the temporal MCA branch, which originated close to the rupture site. The patient developed a minor infarction of the lateral temporal lobe, posterior to the former location of the evacuated temporal lobe hematoma.
Discussion
To our knowledge, this is the first report about the use of intraoperative contrast-enhanced 3D fluoroscopy for imaging of intracranial aneurysms. It was used as an emergency diagnostic tool in a young and otherwise healthy patient, who was admitted in a state of rapidly progressive signs of temporal herniation. In this situation, we supposed that there was not enough time for angiography or even acquisition of another CT followed by a CTA and immediately transferred the patient into the operating room for evacuation of the hematoma and clipping of the suspected aneurysm. If the procedure had not been successful, we would have searched and occluded the aneurysm without additional information about the source of hemorrhage. However, after three supposed re-bleedings, we considered information about the aneurysm to be helpful for the operation, especially in the case of another, intraoperative, re-rupture. This consideration was confirmed as the aneurysm actually ruptured in a very early stage of the operation without visualization of the proximal control. To obtain information about its location and configuration before surgery and still not lose valuable time, we attempted an angiography by the use of a 3D rotational fluoroscope, intravenous contrast agent, and reconstruction of the images by the OsiriX® free software. The image acquisition took approximately 2 min and was performed during the surgeon’s hand disinfection. The image reconstruction lasted 5 min and was performed during sterile draping and skin incision. Altogether, the transfer into the operating room, positioning of the patient, skin disinfection, and draping required 15 min. The imaging procedure could be integrated into the surgical workflow and did not cause any delay of surgical decompression.
To date, DSA is still considered the gold standard in the imaging of cerebrovascular pathologies, although this point of view has been challenged in the recent years. CTA has demonstrated a similar diagnostic precision [6] and comparable depiction of the vessel anatomy and morphology of the aneurysm by advanced image processing technologies [10]. Magnetic resonance angiography (MRA) as a radiation-free examination has been focussed in the recent years and tested for its diagnostic value to depict the vessel anatomy and configuration of intracranial aneurysms [8]. It has shown a good correlation with DSA findings regarding the detection of aneurysms [4], aneurysm size [7], and its use for follow-up after endovascular treatment [5].
For the diagnosis of intracranial aneurysms, DSA is still the standard examination. In cases of emergency, CTA is the most widely used kind of examination. In departments with experience in diagnosis and treatment of cerebrovascular emergencies, CTA would be more or less self-evident. Coming from an external department, however, the patient reported here only received plain CT scans, one at the time of admission and one due to neurological deterioration. Since angiography facilities, CT and MR scanners, are, in most departments, not localized in the operating room or, if they are indeed available there, require an interruption of the surgical workflow, with progressive signs of herniation like in our patient, we supposed that conducting another CT scan followed by CTA would be a situation in which the delay of surgery would have been harmful for the patient. Fluoroscopy scanners are mobile devices which can be positioned by choice. Combined with adequate post-processing software, subtracted images can be generated, bone virtually removed, and the reconstructed images rotated in any direction. The procedure is quick, and, in the presented case, we found that it can be completely integrated into the preoperative workflow—even in a case of emergency.
The images presented in this report were obtained within an acquisition time of 2 min and a processing time of 5 min. The images were acquired by a 3D fluoroscope which is available in many neurosurgical departments today and processed by freely available software. The acquisition of DICOM images by O-arm fluoroscopy followed by OsiriX image was first described by Cardinale et al. who used selective catheter angiography intraoperatively during an epilepsy surgery [1]. The subtraction technique finally leaves contrast-filled vessels in subtracted images. Intracerebral hematomas and thick subarachnoid blood clots are also subtracted by data processing. Placement of an angiography catheter and selective contrast administration into brain-supplying vessels was not indicated in the presented case due to the emergency situation in which a delay of surgery was irresponsible. For this reason, we attempted intravenous contrast administration. The use of an intraoperative 3D fluoroscope with intravenous contrast administration for cerebral angiography is an extension of its technology. Appropriately used, it produces acceptable images of intracranial aneurysms. The data processing was achieved by the use of the OsiriX® software. The advantage of this software is that it is available for free. However, for other computers and operating systems, comparable software is commercially available, too. We only used basic automated tools of the OsiriX® software and no advanced functions, so we believe that this technique can be readily reproduced anywhere and at any time. Although the occasion to take advantage of this technique may be rare, it may be exceedingly helpful in particular cases. It certainly requires further evaluation regarding its diagnostic sensitivity and accuracy. However, the possibility to use this technique may be kept in mind for exceptional cases of emergency.
References
Cardinale F, Moscato A, Cossu M, Castana L, Schiariti MP, Gozzo F, Pero G, Quilici L, Citterio A, Torresin A, LoRusso G (2012) Talairach methodology in the multimodal imaging and robotics era. In: Scarabin JM (ed) Stereotaxy and epilepsy surgery. John Libbey Eurotext, pp 245-272
Fischer G, Stadie A, Oertel JM (2010) Near-infrared indocyanine green videoangiography versus microvascular Doppler sonography in aneurysm surgery. Acta Neurochir (Wien) 152:1519–1525
Kobata H, Sugie A, Yoritsune E, Miyata T, Toho T (2013) Intracranial extravasation of contrast medium during diagnostic CT angiography in the initial evaluation of subarachnoid hemorrhage: report of 16 cases and review of the literature. Springerplus 2:413
Li MH, Li YD, Tan HQ, Gu BX, Chen YC, Wang W, Chen SW, Hu DJ (2011) Contrast-free MRA at 3.0 T for the detection of intracranial aneurysms. Neurology 77:667–676
Lubicz B, Neugroschl C, Collignon L, Francois O, Baleriaux D (2008) Is digital subtraction angiography still needed for the follow-up of intracranial aneurysms treated by embolisation with detachable coils? Neuroradiology 50:841–848
Sun G, Ding J, Lu Y, Li M, Li L, Li GY, Zhang XP (2012) Comparison of standard- and low-tube voltage 320-detector row volume CT angiography in detection of intracranial aneurysms with digital subtraction angiography as gold standard. Acad Radiol 19:281–288
Thines L, Gauvrit JY, Leclerc X, Le Gars D, Delmaire C, Pruvo JP, Lejeune JP (2008) Usefulness of MR imaging for the assessment of nonophthalmic paraclinoid aneurysms. AJNR Am J Neuroradiol 29:125–129
Westerlaan HE, van der Vliet AM, Hew JM, Metzemaekers JD, Mooij JJ, Oudkerk M (2004) Magnetic resonance angiography in the selection of patients suitable for neurosurgical intervention of ruptured intracranial aneurysms. Neuroradiology 46:867–875
Wu TC, Tsui YK, Chen TY, Lin CJ, Tzeng WS (2012) Rebleeding of aneurysmal subarachnoid hemorrhage in computed tomography angiography: risk factor, rebleeding pattern, and outcome analysis. J Comput Assist Tomogr 36:103–108
Zhang H, Hou C, Zhou Z, Zhou G, Zhang G (2012) Evaluating of small intracranial aneurysms by 64-detector CT Angiography: a comparison with 3-dimensional rotation DSA or surgical findings. J Neuroimaging 10-6569
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
A 360° rotational view of the cerebral vessels. A 3D rotational fluoroscopy scan and image post-processing using the automated subtraction and reconstruction functions of the OsiriX® free software served for acquisition of this image (AVI 8008 kb)
Rights and permissions
About this article
Cite this article
Westermaier, T., Willner, N., Vince, G.H. et al. Intraoperative 3D rotational angiography: an emergency tool for the diagnosis of intracranial aneurysms. Emerg Radiol 22, 97–100 (2015). https://doi.org/10.1007/s10140-014-1252-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-014-1252-y