Abstract
We aimed to present our experience regarding infections caused by Serratia spp. in a region with relatively high antimicrobial resistance rates. We retrospectively reviewed the databases of the microbiological laboratory of the University Hospital of Heraklion, Crete (2/2004–12/2009). A total of 77 patients [67.5% men, mean age ± standard deviation (SD) = 56.9 ± 24.5 years) were identified; 37.7% were outpatients. Sixty-five (84.4%) of the 77 included patients had a Serratia marcescens isolate; the remaining 12 patients had a non-marcescens Serratia spp. The most frequently observed infections were respiratory tract infection (32.5%) and keratitis/endophthalmitis (20.8%). Seventy-three (94.9%) patients were cured. Four deaths were observed; three of them were considered as attributed to the Serratia infection. No difference was found regarding the characteristics and outcomes between patients with Serratia marcescens and non-marcescens infections. In addition, antipseudomonal penicillins and their combinations with beta-lactamase inhibitors, as well as carbapenemes, and fluoroquinolones exhibited high antimicrobial activity against both the tested Serratia marcescens and non-marcescens isolates. Our study adds useful information regarding the characteristics and outcomes of patients with Serratia infection, as well as the susceptibilities of the respective Serratia marcescens and non-marcescens isolates, in a region with relatively high levels of antimicrobial resistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Serratia spp, particularly Serratia marcescens, are mainly encountered as causative pathogens of nosocomial infections and nosocomial outbreaks [1, 2]. Specifically, Serratia spp. are incriminated for outbreaks in neonatal intensive care units (NICUs) [3–5]. In addition, due to their ability of biofilm formation and the production of enzymes including gelatinase, elastase and alkaline protease, Serratia spp. manage to invade human corneal epithelial cells and cause keratitis, and particularly contact lens-related keratitis [6, 7].
Even though Serratia spp. are mainly considered nosocomial pathogens, recently published population-based studies suggested that a considerable percentage of the identified Serratia infections is community-acquired [6, 8]. Even though Serratia marcescens constitutes the majority of the identified Serratia isolates, many reports regarding infections and outbreaks caused from Serratia spp. other than Serratia marcescens have also appeared in the literature [7, 9–12]. In addition, another issue that intensified the importance of Serratia infections is the emergence of multi-drug resistant Serratia isolates, and particularly extended spectrum beta-lactamase-producing (ESBLs) Serratia isolates [13–15].
In this regard, the aim of our study was to present our experience regarding the characteristics and outcomes of patients with infections caused from Serratia spp. at a university hospital of a region with relatively high levels of antimicrobial resistance [16–20].
Methods
Study design and patient population
We present a descriptive study based on the retrospective evaluation of a case series. Specifically, we retrospectively reviewed the databases of the microbiological laboratory of the University Hospital of Heraklion, Crete in order to identify patients from whom Serratia spp. were isolated, during a 5-year period (February 2004–December 2009). The University Hospital of Heraklion, Crete is a 650-bed tertiary care centre, serving a population of approximately 650,000 individuals, with approximately 65,000–70,000 admitted patients per year. The following data were retrieved from the available medical records of the respective patients: sex, age, department of hospitalization, potential risk factors for acquisition of nosocomial infections (including immunosuppression, treatment with corticosteroids, malnutrition, trauma, surgery, and presence of a urinary catheter), type of Serratia infection, antibiotic treatment administered for the infection, duration of hospitalization, as well as the outcome of the infection.
With regard to the evaluated potential risk factors in particular, the objective criteria of malnutrition were a BMI < 18.5, or unintentional weight loss of more than 5% in the last month, or more than 10% in the last 6 months, whereas trauma was defined as any injury or wound infection. When more than one Serratia isolates were identified from a patient, we selected the first isolate for inclusion in our study. Moreover, data regarding any other pathogen that was simultaneously identified from the same clinical specimen were also retrieved.
Microbiological testing
Identification of the isolates was performed with the use of standard biochemical methods—the API 20 E system and the Vitek2 automated system (BioMérieux, Marcy l’ Etoile, France) [21]. The antimicrobial susceptibility of the tested isolates to the evaluated antibiotic agents was determined by using the Vitek2 system and the results were interpreted according to CLSI criteria [22].
Statistical analysis
We performed comparisons regarding demographic, clinical characteristics, and outcomes between the included patients with a clinical specimen that yielded a Serratia marcescens isolate and those with a clinical specimen that yielded a Serratia spp. isolate (other than Serratia marcescens). The χ2 test or the Fisher exact tests were used, when appropriate, in the comparisons regarding categorical variables, whereas the t-test was used in the comparisons regarding continuous variables. For non-normally distributed continuous variables, the Mann-Whitney signed-rank test was used. A p value of <0.05 was regarded as indicative of statistical significance. The comparisons were performed with the use of the OpenEpi Software [23] and the SPSS software version 13.0 (SPPS Inc, Chicago, Illinois, USA).
Results
Patient characteristics
A total of 77 patients were identified as having a clinical specimen that yielded a Serratia spp. isolate during the study period. Detailed data regarding the demographic, clinical characteristics and outcomes of the patients are presented in Table 1. Specifically, the mean age ± standard deviation (SD) of the included patients was 56.9 ± 24.5 years. Two of the 77 patients were infants (7 and 8 months, respectively). The majority (67.5%) of the patients were men. Regarding the department of hospitalization, the majority (59.7%) were admitted in medical wards, whereas 37.7% were outpatients. Seventeen (22.1%) of the 77 patients did not have any comorbidity. Regarding the remaining 60 patients, cardiac diseases were reported most frequently (50%). A total of 32.5% of the patients were immunosuppressed, 24.7% were treated with corticosteroids, 19.5% had undergone surgery, 13% had a urinary catheter, 9.1% were trauma patients, and 7.8% were malnourished. In addition, ten of the evaluated patients were admitted in the ICU; two of them were on mechanical ventilation. None of the evaluated patients had a central venous catheter.
Infections and outcomes
A total of 32.5% of the patients had a respiratory tract infection, followed by 20.8% that had keratitis/endophthalmitis. None of the latter ocular infections was hospital-acquired. Other types of infections observed were skin and soft tissue infections (16.9%), urinary tract infections (13.0%), sepsis (6.5%), and cholecystitis (3.9%). In addition, eight (10.4%) of the patients were considered as colonized with Serratia spp. With regard to the patients’ outcomes, 73 (94.9%) of the 77 patients were cured. Four deaths were observed during hospitalization in our case series. Three of the four deceased patients had monomicrobial Serratia infections, whereas the remaining one patient also had an infection from Citrobacter freundii. The four deaths were evaluated by the clinicians that took care of the specific patients as well as the study investigators. Three of these four deaths were considered attributable to the Serratia infection and one to other causes.
Comparisons regarding patient subpopulations
Comparative data regarding the patients providing a clinical specimen that yielded a Serratia marcescens isolate and those with a clinical specimen that yielded a Serratia spp. isolate, other than Serratia marcescens, are also presented in Table 1. No difference was found between the compared patient sub-populations regarding the analyzed characteristics and outcomes.
Microbiological characteristics
Types of isolates and sites of isolation
In Table 2 we present data regarding the isolated Serratia spp, the respective sites of isolation, as well as any other simultaneously isolated non-Serratia species. Specifically, 65 (84.4%) of the 77 patients had a Serratia marcescens isolate, whereas the remaining 12 patients had a non-marcescens Serratia spp. isolate. These were Serratia liquefaciens in five patients, Serratia rubidaea in three, Serratia fonticola in two, Serratia plymuthica in one, and Serratia ficaria in one patient. Detailed data regarding the respective sites of isolation are presented in Table 2. Other isolates, including P. aeruginosa, K. pneumoniae, and Candida spp., were identified concurrently to the isolation of the Serratia spp. Detailed data regarding the distribution of the concurrently isolated species are also presented in Table 2.
Antimicrobial susceptibility of the tested isolates
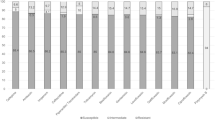
The susceptibility rates of the isolated Serratia spp. to the 30 analyzed antimicrobial agents are presented in Table 3. Regarding the isolated Serratia marcescens that constituted the majority (65/77 [84.4%]) of the identified Serratia isolates, the following antibiotic agents exhibited substantial antimicrobial activity against the tested isolates (89.2–100%): antipseudomonal penicillins (specifically, ticarcillin, piperacillin, and ceftazidime), ticarcillin-clavulanic acid, piperacillin-tazobactam, third generation cephalosporins (cefotaxime and ceftriaxone), carbapenems (imipenem and meropenem), aztreonam, tobramycin, netilmicin, nitrofurantoin trimethoprim-sulfonamides, and quinolones (specifically, pefloxacin, ofloxacin, norfloxacin, and ciprofloxacin).
Regarding the 12 tested non-marcescens Serratia spp., all of them were found susceptible to the following antimicrobial agents: ticarcillin, piperacillin, ticarcillin-clavulanic acid, piperacillin-tazobactam, ceftazidime, ceftriaxone, cefotaxime, imipenem, meropenem, aztreonam, tobramycin, netilmicin, nitrofurantoin trimethoprim-sulfonamides, pefloxacin, ofloxacin, norfloxacin, and ciprofloxacin. In addition, amikacin, gentamicin, and chloramphenicol exhibited substantial antimicrobial activity against the 12 tested isolates (83.3% each).
Discussion
A total of 77 patients providing a clinical specimen that yielded a Serratia spp. isolate were identified in a 650-bed tertiary care hospital during a 5-year period. The majority of the Serratia isolates were identified in male patients. This observation is in accordance with the findings of recent population-based studies in which males were considered to be at higher risk for the acquisition of a Serratia isolate [8]. In addition, ICU patients were represented by rather low percentages (13%) in this cohort, whereas a considerable percentage (38%) were outpatients. Indeed, population-based studies also reported that the majority of the isolated Serratia species [8], including a considerable percentage of Serratia bacteremic episodes, were community-acquired [24].
With regard to the observed Serratia infections, these were mostly respiratory tract infections, followed by ocular infections, including keratitis and/or endophthalmitis, skin and soft tissue infections, and urinary tract infections. Indeed, due to their ability for biofilm formation, based on the interaction of quorum sensing system and nutrient factors [25, 26], Serratia spp frequently colonize medical devices, such as bronchoscopes [27], urinary catheters [28] and water supplies [29], whereas long-term carriage in the hands of healthcare workers has been reported as well [30]. Consequently, Serratia spp are frequently incriminated for hospital-acquired bacteremias, nosocomial respiratory and urinary tract infections, and nosocomial outbreaks [31–34]. Specifically, 13% of the included included patients had a urinary catheter. In addition, due to the production of specific enzymes such as gelatinase, elastase and alkaline protease, Serratia spp. cause ocular infections including ulcerative keratitis, particularly contact lens-related keratitis [6, 35] and endophthalmitis [36, 37]. Moreover, immunocompromised patients are considered more prone to Serratia infections. Of note, a considerable percentage of 32.5% of the included patients were immunosuppressed, and an additional 24.7% received corticosteroids.
Serratia marcescens is the most frequently isolated Serratia spp. However, other Serratia spp. including Serratia liquefaciens, Serratia plymuthica, and Serratia rubidaea, have been recently identified as the cause of Serratia nosocomial infections and outbreaks [10, 12, 38, 39]. Furthermore, non-marcescens Serratia spp are also incriminated for community-acquired infections [40]. A possible explanation that has been proposed for the relative scarcity of published evidence regarding non-marcescens Serratia spp. compared to Serratia marcescens is the misidentification of these specific strains by commercially available identification systems [41]. In our study, 12 (15.5%) of the 77 patients provided a clinical specimen of non-marcescens Serratia spp (specifically, Serratia liquefaciens, Serratia rubidaea, Serratia fonticola, Serratia plymuthica, and Serratia ficaria). The majority of the respective infections were respiratory tract infections. It is worth to note that in the comparisons between the patient subpopulations with S. marcescens infection and those with non-marcescens Serratia infection, no difference was found regarding the demographic characteristics, comorbidity, risk-factors, types of infections, as well as infection outcomes.
As far as mortality is concerned, four of the 77 patients died. Three of these four deaths were considered to have been probably attributed to the Serratia infection, after a meticulous evaluation of the respective clinical data from the clinicians as well as the study investigators. Regarding mortality from Serratia infections, published evidence report percentages of 5% and 37% for Serratia bacteremia 7-day and 6-months mortality, respectively [24]. However, mortality can occur even in less severe Serratia infections, such as urinary tract infections. Specifically, female gender and the development of secondary S. marcescens bacteremia have been identified as risk factors independently associated with fatality in patients with urinary tract infection due to S. marcescens [42]. Moreover, the emergence of ESBL-producing Serratia spp. intensifies the importance of the issue of Serratia infection-related mortality. Specifically, a 30-day mortality rate of 33% has been reported for nosocomial patients with ESBL-producing S. marcescens infections [43].
Serratia spp. exhibit considerable antimicrobial resistance to penicillins and cephalosporins. This is mainly attributed to the fact that AmpC beta-lactamases are encoded in the chromosome of Serratia spp. The expression of these genes is inducible in most cases [44, 45]. In our study all the 65 tested Serratia marcescens isolates were found resistant to amoxicillin and amoxicillin/clavulanic acid. Similarly, one of the 12 non-marcescens Serratia spp was susceptible to the above drugs. This observation was consistent regarding cefalothin, a first generation cephalosporin, whereas with regard to cefuroxime, lower susceptibility rates were observed for the tested Serratia marcescens compared to the non-marcescens isolates. Additionally, 35% of the tested Serratia marcescens isolates and 50% of the non-marcescens isolates were found susceptible to cefoxitin. Finally, third generation cephalosporins (ceftazidime and cefotaxime) and ceftriaxone exhibited high susceptibility rates regarding the Serratia marcescens and non-marcescens tested isolates (95.4% and 100%, respectively).
Other beta-lactamases, including CTX-M3, IMP-type, as well as TEM-type have also been identified in Serratia spp [14, 46–48]. Specifically, the issue of the emergence of carbapenem resistance Serratia strains is of major importance. In our study, both imipenem and meropenem exhibited high antimicrobial activity rates against the tested Serratia marcescens and non-marcescens isolates. In addition, among the evaluated antimicrobial agents, tobramycin, netilmicin, nitrofurantoin, as well as the combination of trimethoprim with sulfonamides were also found highly active against the tested Serratia marcescens and non-marcescens isolates. On the contrary, amikacin and gentamicin were found to be more active against the tested non-marcescens isolates compared to the tested Serratia marcescens isolates. Finally, fluoroquinolones were also highly active against the tested Serratia marcescens and non-marcescens isolates. However, evidence regarding the chromosome-encoded resistance to fluoroquinolones of Serratia marcescens has appeared in the literature [49–51].
Our study has specific limitations that should be considered. Firstly, one should bear in mind the intrinsic methodological limitations of retrospective cohort studies before the extrapolation of the study findings. In addition, our findings derive from the evaluation of the clinical and microbiological data of a rather limited number of 77 patients that provided a clinical specimen that yielded a Serratia spp. isolate. Moreover, since Serratia spp. are often incriminated for nosocomial epidemics, one may consider that the Serratia strains included in this study are epidemic strains. Yet, even though genetic identification techniques were not used in this study, the 5-year study period is rather contradictory to the potential of a concurrent nosocomial epidemic. However, one may consider that a proportion of the tested Serratia isolates might have been of the same clonal origin. Finally, even though the emergence of ESBL-producing Serratia spp. appears to be an issue of increasing importance, microbiological methods for the identification of ESBL-producing isolates, among the evaluated Serratia isolates, were also not implemented in this study.
In conclusion, our study aids in the clarification of issues regarding the characteristics and outcomes of patients with Serratia infections, as well as the susceptibility patterns of the respective isolates. In the era of alarmingly high antimicrobial resistance, and particularly in the era of ESBL-producing enterobacteriaceae [52], our findings may provide useful information regarding the infections caused from this specific pathogen, as they derive from a clinical setting with relatively high levels of antimicrobial resistance.
References
Chemaly RF, Rathod DB, Raad II (2009) A tertiary care cancer center experience of the 2007 outbreak of Serratia marcescens bloodstream infection due to prefilled syringes. Infect Control Hosp Epidemiol 30:1237–1238
Kim JH, Choi WH, Yun SW, Chae SA, Yoo BH (2010) An outbreak of Serratia marcescens Sepsis in a pediatric ward. Clin Pediatr (Phila) 49(10):1000–1002
Arslan U, Erayman I, Kirdar S et al (2010) Serratia marcescens sepsis outbreak in a neonatal intensive care unit. Pediatr Int 52:208–212
Dessi A, Puddu M, Testa M, Marcialis MA, Pintus MC, Fanos V (2009) Serratia marcescens infections and outbreaks in neonatal intensive care units. J Chemother 21:493–499
Voelz A, Muller A, Gillen J et al (2010) Outbreaks of Serratia marcescens in neonatal and pediatric intensive care units: clinical aspects, risk factors and management. Int J Hyg Environ Health 213:79–87
Pinna A, Usai D, Sechi LA, Carta A, Zanetti S (2009) Detection of virulence factors in Serratia strains isolated from contact lens-associated corneal ulcers. Acta Ophthalmol [Epub ahead of print]
Szczotka-Flynn LB, Imamura Y, Chandra J et al (2009) Increased resistance of contact lens-related bacterial biofilms to antimicrobial activity of soft contact lens care solutions. Cornea 28:918–926
Laupland KB, Parkins MD, Gregson DB, Church DL, Ross T, Pitout JD (2008) Population-based laboratory surveillance for Serratia species isolates in a large Canadian health region. Eur J Clin Microbiol Infect Dis 27:89–95
Dalamaga M, Pantelaki M, Karmaniolas K, Matekovits A, Daskalopoulou K (2008) Cutaneous abscess and bacteremia due to Serratia ficaria. J Eur Acad Dermatol Venereol 22:1388–1389
Dubouix A, Roques C, Segonds C et al (2005) Epidemiological investigation of a Serratia liquefaciens outbreak in a neurosurgery department. J Hosp Infect 60:8–13
Grohskopf LA, Roth VR, Feikin DR et al (2001) Serratia liquefaciens bloodstream infections from contamination of epoetin alfa at a hemodialysis center. N Engl J Med 344:1491–1497
Mostafa E, Mohammed F, Abdelhamid Z, Tahar B, Sakina E, Belkacem C (2008) Septic pseudarthrosis caused by Serratia plymuthica. Joint Bone Spine 75:506–507
Crivaro V, Bagattini M, Salza MF et al (2007) Risk factors for extended-spectrum beta-lactamase-producing Serratia marcescens and Klebsiella pneumoniae acquisition in a neonatal intensive care unit. J Hosp Infect 67:135–141
Mlynarczyk A, Szymanek K, Sawicka-Grzelak A et al (2009) CTX-M and TEM as predominant types of extended spectrum beta-lactamases among Serratia marcescens isolated from solid organ recipients. Transplant Proc 41:3253–3255
Rizvi M, Fatima N, Shukla I, Malik A (2010) Epidemiology of extended spectrum beta-lactamases in Serratia and Citrobacter species in North India. Indian J Pathol Microbiol 53:193–194
Falagas ME, Maraki S, Karageorgopoulos DE, Kastoris AC, Kapaskelis A, Samonis G (2010) Antimicrobial susceptibility of Gram-positive non-urinary isolates to fosfomycin. Int J Antimicrob Agents 35:497–499
Falagas ME, Maraki S, Karageorgopoulos DE, Kastoris AC, Mavromanolakis E, Samonis G (2010) Antimicrobial susceptibility of multidrug-resistant (MDR) and extensively drug-resistant (XDR) Enterobacteriaceae isolates to fosfomycin. Int J Antimicrob Agents 35:240–243
Maraki S, Samonis G, Rafailidis PI, Vouloumanou EK, Mavromanolakis E, Falagas ME (2009) Susceptibility of urinary tract bacteria to fosfomycin. Antimicrob Agents Chemother 53:4508–4510
Samonis G, Maraki S, Rafailidis PI, Kapaskelis A, Kastoris AC, Falagas ME (2010) Antimicrobial susceptibility of Gram-negative nonurinary bacteria to fosfomycin and other antimicrobials. Future Microbiol 5:961–970
Samonis G, Matthaiou DK, Kofteridis D, Maraki S, Falagas ME (2010) In vitro susceptibility to various antibiotics of colistin-resistant gram-negative bacterial isolates in a general tertiary hospital in Crete, Greece. Clin Infect Dis 50:1689–1691
Farmer JJ III, Boatwright KD, Janda JM (2007) Enterobacteriaceae: Introduction and identification. In: Murray P, Baron EJ, Jorgensen JH, Landry ML, Pfaller MA (eds) Manual of clinical microbiology, vol 1, 9th edn. American Society for Microbiology, Washington, pp 649–669
Clinical and Laboratory Standards Institute (2009) Performance standards for antimicrobial susceptibility testing; Nineteenth informational supplement. CLSI Document M100-S19, Wayne, PA, USA
Dean A, Sullivan K, Soe M (2008) OpenEpi: open source epidemiologic statistics for public health, version 2.2.1. Updated 2008/04/06. Available from: www.OpenEpi.com. Cited 18 September 2008
Engel HJ, Collignon PJ, Whiting PT, Kennedy KJ (2009) Serratia sp. bacteremia in Canberra, Australia: a population-based study over 10 years. Eur J Clin Microbiol Infect Dis 28:821–824
Rice SA, Koh KS, Queck SY, Labbate M, Lam KW, Kjelleberg S (2005) Biofilm formation and sloughing in Serratia marcescens are controlled by quorum sensing and nutrient cues. J Bacteriol 187:3477–3485
Van Houdt R, Givskov M, Michiels CW (2007) Quorum sensing in Serratia. FEMS Microbiol Rev 31:407–424
Molina-Cabrillana J, Rodriguez-Bermejo JC, del Rosario-Quintana C, Bolanos-Rivero M (2007) Rapid detection of an outbreak of bronchoscopy-associated colonization by Serratia marcescens. Enferm Infecc Microbiol Clín 25:222–224
Jones GL, Muller CT, O'Reilly M, Stickler DJ (2006) Effect of triclosan on the development of bacterial biofilms by urinary tract pathogens on urinary catheters. J Antimicrob Chemother 57:266–272
Horcajada JP, Martinez JA, Alcon A et al (2006) Acquisition of multidrug-resistant Serratia marcescens by critically ill patients who consumed tap water during receipt of oral medication. Infect Control Hosp Epidemiol 27:774–777
de Vries JJ, Baas WH, van der Ploeg K, Heesink A, Degener JE, Arends JP (2006) Outbreak of Serratia marcescens colonization and infection traced to a healthcare worker with long-term carriage on the hands. Infect Control Hosp Epidemiol 27:1153–1158
Casolari C, Pecorari M, Fabio G et al (2005) A simultaneous outbreak of Serratia marcescens and Klebsiella pneumoniae in a neonatal intensive care unit. J Hosp Infect 61:312–320
Johnson JS, Croall J, Power JS, Armstrong GR (1998) Fatal Serratia marcescens meningitis and myocarditis in a patient with an indwelling urinary catheter. J Clin Pathol 51:789–790
Kim BN, Choi SI, Ryoo NH (2006) Three-year follow-up of an outbreak of Serratia marcescens bacteriuria in a neurosurgical intensive care unit. J Korean Med Sci 21:973–978
Yu WL, Lin CW, Wang DY (1998) Serratia marcescens bacteremia: clinical features and antimicrobial susceptibilities of the isolates. J Microbiol Immunol Infect 31:171–179
Parment PA (1997) The role of Serratia marcescens in soft contact lens associated ocular infections. A review. Acta Ophthalmol Scand 75:67–71
Latorre G (2008) Endogenous Serratia marcescens endophthalmitis in a preterm infant. Indian J Pediatr 75:410
Mah-Sadorra JH, Najjar DM, Rapuano CJ, Laibson PR, Cohen EJ (2005) Serratia corneal ulcers: a retrospective clinical study. Cornea 24:793–800
Chuang TY, Chuang CP, Cheng HH, Hsueh PR (2007) Aortic valve infective endocarditis caused by Serratia liquefaciens. J Infect 54:e161–e163
Sekhsokh Y, Arsalane L, El Ouenass M, Doublali T, Bajjou T, Lahlou Amine I (2007) Serratia rubidaea bacteremia. Méd Mal Infect 37:287–289
Okada T, Yokota E, Matsumoto I (2002) Community acquired sepsis by Serratia rubidaea. Kansenshogaku Zasshi 76:109–112
Anahory T, Darbas H, Ongaro O, Jean-Pierre H, Mion P (1998) Serratia ficaria: a misidentified or unidentified rare cause of human infections in fig tree culture zones. J Clin Microbiol 36:3266–3272
Liu J-W, Hsu Y-M, Huang Y-F (2004) Independent prognostic factors for fatality in patients with urinary tract infection caused by Serratia marcescens. Infect Control Hosp Epidemiol 25:80–82
Cheng K-C, Chuang Y-C, Wu L-T, Huang G-C, Yu W-L (2006) Clinical experiences of the infections caused by extended-spectrum beta-lactamase-producing Serratia marcescens at a medical center in Taiwan. Jpn J Infect Dis 59:147–152
Park YJ, Park SY, Oh EJ et al (2005) Occurrence of extended-spectrum beta-lactamases among chromosomal AmpC-producing Enterobacter cloacae, Citrobacter freundii, and Serratia marcescens in Korea and investigation of screening criteria. Diagn Microbiol Infect Dis 51:265–269
Rizvi M, Fatima N, Rashid M et al (2009) Extended spectrum AmpC and metallo-beta-lactamases in Serratia and Citrobacter spp. in a disc approximation assay. J Infect Dev Ctries 3:285–294
Kumamoto Y, Tsukamoto T, Matsukawa M et al (2005) Comparative studies on activities of antimicrobial agents against causative organisms isolated from patients with urinary tract infections (2003). I. Susceptibility distribution. Jpn J Antibiot 58:518–543
Tsou MF, Yu WL, Hung SW et al (2004) Detection of cefotaxime-resistant CTX-M-3 in clinical isolates of Serratia marcescens. Folia Microbiol (Praha) 49:452–456
Zhao WH, Hu ZQ, Chen G, Matsushita K, Fukuchi K, Shimamura T (2007) Characterization of imipenem-resistant Serratia marcescens producing IMP-type and TEM-type beta-lactamases encoded on a single plasmid. Microbiol Res 162:46–52
Sheng WH, Chen YC, Wang JT, Chang SC, Luh KT, Hsieh WC (2002) Emerging fluoroquinolone-resistance for common clinically important gram-negative bacteria in Taiwan. Diagn Microbiol Infect Dis 43:141–147
Acar JF, O'Brien TF, Goldstein FW, Jones RN (1993) The epidemiology of bacterial resistance to quinolones. Drugs 45(Suppl 3):24–28
Velasco C, Rodriguez-Martinez JM, Briales A, Diaz de Alba P, Calvo J, Pascual A (2010) Smaqnr, a new chromosome-encoded quinolone resistance determinant in Serratia marcescens. J Antimicrob Chemother 65:239–242
Falagas ME, Karageorgopoulos DE (2009) Extended-spectrum beta-lactamase-producing organisms. J Hosp Infect 73:345–354
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Samonis, G., Vouloumanou, E.K., Christofaki, M. et al. Serratia infections in a general hospital: characteristics and outcomes. Eur J Clin Microbiol Infect Dis 30, 653–660 (2011). https://doi.org/10.1007/s10096-010-1135-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-010-1135-4