Abstract
Purpose
To describe the prevalence and antibiotic resistance profiles of Pseudomonas aeruginosa isolated from the Asia Cornea Society Infectious Keratitis Study (ACSIKS).
Methods
All bacterial isolates from ACSIKS underwent repeat microbiological identification in a central repository in Singapore. Minimum inhibitory concentration (MIC) determination was conducted for isolates of P. aeruginosa against thirteen antibiotics from 6 different classes, and categorized based on Clinical Laboratory Standard Institutes’ reference ranges. The percentage rates of resistance (non-susceptibility) to each antibiotic included isolates of both intermediate and complete resistance. Multi-drug resistance (MDR) was defined as non-susceptibility to at least one agent in three or more antimicrobial classes.
Results
Of the 1493 unique bacterial specimens obtained from ACSIKS, 319 isolates were of P. aeruginosa. The majority of isolates were from centers in India (n = 118, 37%), Singapore (n = 90, 28.2%), Hong Kong (n = 31, 9.7%) and Thailand (n = 30, 9.4%). The cumulative antibiotic resistance rate was the greatest for polymyxin B (100%), ciprofloxacin (17.6%) and moxifloxacin (16.9%), and lowest for cefepime (11.6%) and amikacin (13.5%). Isolates from India demonstrated the highest antibiotic resistance rates of all the centers, and included moxifloxacin (47.5%) and ciprofloxacin (39.8%). Forty-eight of the 59 MDR isolates also originated from India. Antibiotic resistance rates were significantly lower in the other ACSIKS centers, and were typically less than 10%.
Conclusions
The antibiotic resistance profiles of P. aeruginosa varied between different countries. While it was low for most countries, substantial antibiotic resistance and a significant number of multi-drug resistant isolates were noted in the centers from India.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The multi-national, multi-center Asia Cornea Society Infectious Keratitis Study (ACSIKS) established a comparative baseline description of the risk factors, microbiology, and outcomes of infectious keratitis in developed and developing Asian countries [1, 2]. Amongst its objectives was to provide local data on the common pathogens for infection in these countries. The observational study isolated more than 2800 unique microorganisms, of which the most commonly isolated bacterial pathogen was Pseudomonas aeruginosa [1].
P. aeruginosa is an opportunistic gram-negative organism that is a common cause of infectious keratitis worldwide [3,4,5]. Infectious keratitis from P. aeruginosa is strongly linked with contact lens use [2, 4], but it can also be associated with ophthalmic surgery, ocular trauma, and eyes with poor ocular surface health [4]. The virulence of P. aeruginosa can result in severe, progressive infection that rapidly leads to cornea melting, perforation and loss of the eye, unless immediate and effective antibiotic treatment is instituted. The increasing number of reports of multidrug resistant (MDR) strains of P. aeruginosa is thus a great cause for concern [6,7,8].
At the conclusion of the ACSIKS observational study, all bacterial and fungal isolates cultured from study participants were stored in deep freeze and sent to central repositories in Singapore and India for repeat identification and analysis. This paper outlines the antibiotic resistance profiles of isolates of P. aeruginosa analyzed in this laboratory study.
Methods and materials
ACSIKS Phase 1 study design and methodology
The ACSIKS study design and methodology has been previously published [1] and will be summarized here. ACSIKS Phase 1 was a multi-center, prospective observational study of infectious keratitis presenting to study centers in eight countries (India, China, Japan, South Korea, Taiwan, Thailand, the Philippines and Singapore). Each center recruited all cases of infectious keratitis presenting over 12 months and each study patient was observed for 6 months. Phase 1 enrolled 6563 patients between 1 April 2012 and 31 March 2014. The observational study was later expanded, with 3 additional study sites in Hong Kong (where 331 patients were recruited from 21 Nov 2014 to 18 March 2016) and one site in northern India (where an additional 482 patients were enrolled from 1 April 2017 to 30 April 2019). Most sites were dedicated ophthalmology institutes or ophthalmology departments in major hospitals providing tertiary-level ophthalmic care (Appendix 1: ACSIKS Group; Supplemental Material).
During ACSIKS Phase 1, corneal scrapings and/or corneal biopsies were routinely collected to identify the causative organism for the infection, regardless of lesion size and severity. The only exception was for suspected viral infections, as these are typically diagnosed clinically, and identification of viruses (through cell cultures or polymerase chain reaction testing) was not available at every study centers. All specimens were incubated according to a standardized set of conditions (Appendix 2: ACSIKS Phase 1 Standard Microbiological Investigations and Incubation Conditions; Supplemental Material).
All fungal and bacterial organisms isolated from study patients were sub-cultured and transferred into Microbank vials (Pro-Lab Diagnostics, Round Rock, TX, USA) for storage in dedicated ultra-low deep freezers (− 80 °C) at each study center. At least two samples of each isolate were kept, so that by the end of the study each center would retain one sample for their own research, while the second sample would be sent to the central repositories located in Singapore and India for ACSIKS Phase 2.
ACSIKS Phase 2 methodology
ACSIKS Phase 2 is an on-going microbiological initiative to study isolates obtained from ACSIKS Phase 1. All bacterial isolates were sent to the central repository in Singapore, where they were re-identified and had their antibiotic resistance patterns re-evaluated. Similarly, all fungal isolates have been sent to the central repository in India for similar studies.
Between 2015 and 2019, the Diagnostic Bacteriology Laboratory of the Department of Microbiology in the Singapore General Hospital subcultured all bacterial isolates from the Microbank vials onto Trypticase soy agar with 5% sheep blood, and incubated them at 35°C. Identification was then performed using Matrix Assisted Laser Desorption Ionization—Time of Flight (MALDI-ToF), utilizing the MALDI Biotyper (Bruker Daltonics, Bremen, Germany). Additional tests (eg biochemical sugar tests) were done where necessary.
Bacterial isolates were then provided to the Singapore Eye Research Institute for minimum inhibitory concentration (MIC) determination. MIC was determined using the broth microdilution method procedures as per Clinical Laboratory Standard Institutes (CLSI) guidelines. Each glycerol bead from the Microbank vials was isolated and cultures were grown on Tryptic soy agar plates overnight at 35°C. Selected colonies were picked from the overnight growth of bacterial culture, suspended in demineralized water and vigorously vortexed to obtain a homogenous suspension. The turbidity of suspension was adjusted to 0.5 McFarland standard and the precise turbidity confirmed by Nephelometer (Sensititre, Cat. #YV3011, Thermo Fisher Scientific, MA, USA). Fifty microlitres was aliquoted from the adjusted 0.5 McFarland bacterial suspension and subsequently added to the Cation Adjusted Mueller Hinton Broth to a final concentration of 105–106 CFU/mL. Fifty microlitres of inoculation broth were transferred accurately into a customized 96-well plate [(Sensititre, Cat. #YSGCML1F, Thermo Fisher Scientific, MA, USA) plate panel: CML1FASC]. All the 96-well plates were labelled, sealed accordingly and incubated at 35 °C for 24 h. The plates were loaded on to the Sensititre Vizion Plate reader (Thermo Fisher Scientific, MA, USA) for reading. All the growths appeared as turbidity or as deposit of cells at the bottom of a well. Positive growths were read first before proceeding to read the MIC results. Test results were considered to be invalid if the plate showed more than single skipped wells or if mixed cultures were detected on the plates. All the samples were analysed using the SWIN Software System (Sensititre, Cat. #YSW100COMP, Thermo Fisher Scientific, MA, USA).
A total of 13 representative antibiotics from 6 different classes were used for this study on P. aeruginosa (Table 1). The customized plates for P. aeruginosa were designed based on the recommended CLSI reference ranges. This study used P. aeruginosa ATCC 27853 and P. aeruginosa ATCC 9027 strains as the quality control for every batch conducted. These strains achieved MIC within the reference ranges (Table 1) and all the tested P. aeruginosa isolates were categorized as susceptible, intermediate or resistant as recommended by the current CLSI standards [9]. A notable difference between previous CLSI guidelines [10] (which the ACSIKS observational study referenced for susceptibility testing) and the current version is the removal of the “susceptible” category from polymyxin B, such that the antibiotic is deemed to have only intermediate or full resistance against P. aeruginosa. Furthermore, as moxifloxacin and besifloxacin do not have MIC reference ranges listed in the CLSI guidelines, clinical isolates with an MIC that was more than or equal to four times the MIC of the quality control strains were characterised as resistant, following the work of Mei et al. [11].
In accordance with previously-published guidelines, isolates that were categorized with either intermediate or full resistance were considered to be resistant (non-susceptible) to the antibiotic tested [12]. Similarly, multi-drug resistance (MDR) was defined as non-susceptibility to at least one agent, in three or more antimicrobial categories. Extensive drug resistance (XDR) was defined as non-susceptibility to at least one agent in all but two or fewer antimicrobial categories (i.e. bacterial isolates remain susceptible to only one or two categories), and pan drug resistance (PDR) was defined as non-susceptibility to all agents in all antimicrobial categories (i.e. no agents tested as susceptible for that organism).
Ethics
This study adhered to the tenets of the Declaration of Helsinki. Institutional Review Board review was waived for this study as only bacterial isolates with no patient identifiers were provided for this laboratory study.
Results
A total of 1493 unique bacterial specimens were identified; the majority of specimens (80.2%) were from India (n = 606, 40.6%), Hong Kong (n = 232,15.5%), Singapore (n = 185, 12.4%) and Japan (n = 175, 11.7%) (Table 2).
Furthermore, 321 isolates of Pseudomonas species were confirmed, of which 319 isolates were of P. aeruginosa, one of Pseudomonas putida, and one of Pseudomonas otitis.
Cumulative antibiotic resistance rates for Pseudomonas aeruginosa
While isolates of P. aeruginosa were received from all the study centers in ACSIKS, the majority of these isolates were from centers in India (n = 118, 37.0%), Singapore (n = 90, 28.2%), Hong Kong (n = 31, 9.7%) and Thailand (n = 30, 9.4%) (Table 3).
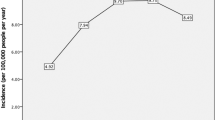
The cumulative antibiotic susceptibility results are presented in Fig. 1. Of the 319 isolates tested, resistance rates were highest for polymyxin B (100%), ciprofloxacin (17.6%) and moxifloxacin (16.9%), while rates were lowest for cefepime (11.6%) and amikacin (13.5%) (Table 4). In the class of fluoroquinolone antibiotics, the resistance rates ranged between 15.4% (besifloxacin and levofloxacin) and 17.6% (ciprofloxacin).
Multidrug resistance was noted in 59 isolates of P. aeruginosa; 48 isolates were from India, 4 from Singapore, 2 from Thailand, and 1 each from China, Japan, Korea, the Philippines and Taiwan. Of these, 31 isolates were found to have extensive drug resistance, and 3 were found to have pan-resistance to all the antibiotics tested.
Antibiotic resistance rates by selected countries
Further analysis of the antibiotic resistance rates was conducted for countries and territories with a total of 30 or more isolates of P. aeruginosa, namely India, Thailand, Hong Kong and Singapore.
Isolates from India were noted to have the highest antibiotic resistance rates of all the ACSIKS study centers (Table 5). Of note was that resistance to the fluoroquinolones was common, such as moxifloxacin (47.5%), ciprofloxacin (39.8%) and besifloxacin/gatifloxacin/levofloxacin (all at 38.1%). In fact, resistance rates to all the antibiotics tested was 30% or greater. Furthermore, 48 of the 59 MDR isolates of P. aeruginosa (and all isolates with XDR and PDR) originated from the centers in India.
Conversely, antibiotic resistance rates in Thailand (Table 6) and Singapore (Table 7) were generally less than 7–8%, with the exception of polymyxin B. Sporadic resistance was seen in the fluoroquinolones, and the antipseudomonal cephalosporins, carbapenems and penicillins. There were 2 MDR isolates from Thailand and 4 MDR isolates from Singapore. All isolates from these two countries were susceptible to the aminoglycosides tested.
Isolates from Hong Kong (Table 8) were susceptible to all the antibiotics tested, with the exception of polymyxin B and a single isolate with intermediate resistance to gatifloxacin. None of the isolates from Hong Kong had multidrug resistance.
Discussion
Over the course of ACSIKS Phase 1, more than 7300 subjects with infectious keratitis were recruited, making this one of the largest prospective observational studies on infectious keratitis ever conducted in Asia. Outside of India and China, bacterial infections are the predominant cause for infectious keratitis, and our Phase 2 results confirm P. aeruginosa to be the most common bacterial pathogen isolated.
MIC testing revealed that the cumulative antibiotic resistance of P aeruginosa ranged between 11.6 and 17.6% for the antibiotics tested (with the exception of 100% non-susceptibility to polymyxin B with current CLSI guidelines). Among the fluoroquinolones with well-defined CLSI breakpoints, ciprofloxacin resistance was slightly higher than levofloxacin and gatifloxacin. Comparing our isolates with those in the ARMOR study [5], MIC90 values for the fluoroquinolones were 4 to 32 times higher in our study. These are all of concern, as topical fluoroquinolones have become the antibiotics of choice for the treatment of infectious keratitis, due to their broad spectrum of activity, low toxicity, and wide-spread commercial availability [13, 14]. Previous randomized controlled trials have also demonstrated the efficacy of fluoroquinolone monotherapy to the use of broad-spectrum fortified antibiotics [15,16,17,18]. The fourth generation fluoroquinolones (such as moxifloxacin and besifloxacin) target both DNA gyrase and topoisomerase IV in bacteria, and at the time that these antibiotics were introduced, it was believed that they would be at lesser risk of encountering antibiotic resistance since two mutations rather than one would be required to develop resistance [19]. However, studies would soon emerge from South India that documented high MIC levels for moxifloxacin in P. aeruginosa and Nocardia spp, [20] as well as a sharp increase in the percentage of P. aeruginosa isolates that were resistant to moxifloxacin between 2007 and 2009 [21]. The resistance results from ACSIKS (with isolates gathered from 2012 to 2019) demonstrates that resistance to moxifloxacin continues to be present in India, and to a lesser extent in other countries.
Ciprofloxacin remains a reasonable choice for the targeted treatment of susceptible P. aeruginosa. However, gatifloxacin and levofloxacin have increased coverage against gram positive bacteria, making them suitable broad-spectrum antibiotics for the empiric treatment of bacterial keratitis. Levofloxacin is also the fluoroquinolone with the highest concentration (1.5%) available in a commercially-prepared eye drop; it has greater bioavailability and intraocular penetration [22, 23] compared to existing fluoroquinolone eye drops, and this may further increase its potency given that fluoroquinolones are concentration-dependent agents. Experimental studies have even suggested that levofloxacin 1.5% may be effective against resistant strains of P. aeruginosa, [24, 25] although further clinical studies will be needed to clarify this.
Beyond fluoroquinolone resistance, ACSIKS Phase 2 has also identified multiple MDR and even PDR isolates of P. aeruginosa. Antibiotic drug resistance is an increasing concern globally [12, 26], and emergence of MDR bacteria has affected all disciplines in medicine, including ophthalmology. Drug resistant bacterial keratitis may render first or second line antibiotics ineffective, and ophthalmologists may have little choice but to use more toxic and/or more expensive antibiotics to treat these cornea infections. Resistant infections can also lead to prolonged treatment, or result in treatment failure with complications such as cornea perforation and endophthalmitis [6, 7]. P. aeruginosa is part of the ESKAPE group of pathogens commonly associated with increases in antimicrobial resistance [27]. It has also been identified by the World Health Organization as one of the top three “priority 1” pathogens urgently requiring development of new antibiotics for effective treatment of infection [28].
The centers in India had isolates with the highest antibiotic resistance rates of all the ACSIKS study centers (more than 30% on average), and also contributed the majority of the MDR isolates from the Phase 1 study. Outside of India, antibiotic resistance was typically 10% or less in the other ACSIKS centers. A survey of global antibiotic resistance performed prior to 2008 noted the higher incidence of resistance to ciprofloxacin in P. aeruginosa isolates from India (greater than 20%), as compared to other countries such as Australia and North America [29]. Similarly, the ARMOR studies in the USA demonstrated low and stable levels of antibiotic resistance in P. aeruginosa isolates from ocular and cornea samples between 2009 and 2019 [5]. Possible reasons for this increasing antibiotic resistance in India include the misuse or overuse of antibiotics [26]. Indian regulation of antibiotic prescription is weak and medications can be sold over the counter without prescription, which encourages widespread misuse [30]. Counterfeit and substandard antibiotics have also been reported [30]. Extensive use of antibiotics in agriculture (prevalent in India, but also in countries such as the United States), is also contributing to antibiotic resistance in environmental bacteria, which may in turn result in more virulent infections in humans [26].
We acknowledge the potential limitations to this study. Firstly, given the wide differences between Asian countries in terms of population demographics, economic development and access to healthcare, bacterial specimens isolated by the individual ACSIKS study centers may not be representative of the entire country. Secondly, the ASCIKS study centers are tertiary eyecare referral centers, thus infections encountered are possibly more severe and there may be an over-representation of drug resistant isolates of P. aeruginosa. Thirdly, there is also a wide variation in the number of P. aeruginosa isolates contributed by each country, with a large percentage of drug-resistant samples from India. The cumulative resistance rates described here will need to be interpreted with this in mind, although it this does reflect the real-world situation of infectious keratitis in Asia. Finally, the use of systemic break points for the interpretation of bacterial resistance of ocular isolates may not be absolute, as topical antibiotics may result in higher concentrations on the ocular surface and so resistance rates may actually be lower in clinical practice. This may be particularly relevant to polymyxin B, as the antibiotic is now deemed to have only intermediate or full resistance against P. aeruginosa; and moxifloxacin and besifloxacin, for which there were no established MIC ranges in the CLSI guidelines for susceptibility. Nonetheless, in the absence of eye-specific criteria, the adoption of systemic break points for ocular isolates remains a useful standard for comparison of bacterial resistance rates across countries and centers. In spite of these limitations, it is hoped that the data presented here will serve as a baseline for describing and understanding the antibiotic resistance profiles of P. aeruginosa in this region, and help ophthalmologists in making informed and prudent antibiotic choices in the management of infectious keratitis.
Data availability
The data that support the findings of this study are available from the authors but restrictions apply to the availability of these data, which was supplied by the Asia Cornea Society. The data are available upon reasonable request with written permission by the Asia Cornea Society.
References
Khor WB, Prajna VN, Garg P et al (2018) The Asia Cornea Society Infectious Keratitis Study: a prospective multicenter study of infectious keratitis in Asia. Am J Ophthalmol 195(11):161–170. https://doi.org/10.1016/j.ajo.2018.07.040
Stapleton F, Lim CHL, Kweon S, Tan D, Mehta JS, ACSIKS group (2021) Cosmetic contact lens-related corneal infections in Asia. Am J Ophthalmol 229(9):176–183. https://doi.org/10.1016/j.ajo.2021.03.005
Ung L, Bispo PJM, Shanbhag SS, Gilmore MS, Chodosh J (2019) The persistent dilemma of microbial keratitis: global burden, diagnosis, and antimicrobial resistance. Surv Ophthalmol 64(3):255–271. https://doi.org/10.1016/j.survophthal.2018.12.003
Hilliam Y, Kaye S, Winstanley C (2020) Pseudomonas aeruginosa and microbial keratitis. J Med Microbiol 69(1):3–13. https://doi.org/10.1099/jmm.0.001110
Thomas RK, Melton R, Vollmer PM, Asbell PA (2021) In vitro antibiotic resistance among bacteria from the cornea in the antibiotic resistance monitoring in ocular microorganisms surveillance study. Optom Vis Sci 98(9):1113–1121. https://doi.org/10.1097/OPX.0000000000001768
Vazirani J, Wurity S, Ali MH (2015) Multidrug-resistant Pseudomonas aeruginosa keratitis: risk factors, clinical characteristics, and outcomes. Ophthalmology 122(10):2110–2114. https://doi.org/10.1016/j.ophtha.2015.06.007
Fernandes M, Vira D, Medikonda R, Kumar N (2016) Extensively and pan-drug resistant Pseudomonas aeruginosa keratitis: clinical features, risk factors, and outcome. Graefes Arch Clin Exp Ophthalmol 254(2):315–322. https://doi.org/10.1007/s00417-015-3208-7
Khan M, Stapleton F, Summers S, Rice SA, Willcox MDP (2020) Antibiotic resistance characteristics of pseudomonas aeruginosa isolated from keratitis in Australia and India. Antibiotics (Basel) 9(9):600. https://doi.org/10.3390/antibiotics9090600
Performance standards for antimicrobial susceptibility testing. 30th ed. CLSI supplement M100. Wayne, PA: Clinical and Laboratory Standard Institute; 2020.
Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; Approved Standard. 7th Edition, CLSI Document M7-A7. Clinical and Laboratory Standards Institute; 2006.
Mei JA, Johnson W, Kinn B et al (2022) Antimicrobial activity of a triple antibiotic combination toward ocular Pseudomonas aeruginosa clinical isolates. Transl Vis Sci Technol 11(5):26. https://doi.org/10.1167/tvst.11.5.26
Magiorakos AP, Srinivasan A, Carey RB et al (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18(3):268–281. https://doi.org/10.1111/j.1469-0691.2011.03570.x
Lin A, Rhee MK, Akpek EK et al (2019) American Academy of ophthalmology preferred practice pattern cornea and external disease panel. Bacterial keratitis preferred practice pattern. Ophthalmology 126(1):P1–P55. https://doi.org/10.1016/j.ophtha.2018.10.018
Cabrera-Aguas M, Khoo P, Watson SL (2022) Infectious keratitis: a review. Clin Exp Ophthalmol 50(5):543–562. https://doi.org/10.1111/ceo.14113
Hyndiuk RA, Eiferman RA, Caldwell DR et al (1996) Comparison of ciprofloxacin ophthalmic solution 0.3% to fortified tobramycin-cefazolin in treating bacterial corneal ulcers. Ciprofloxacin Bacterial Keratitis Study Group. Ophthalmology 103(11):1854–1862. https://doi.org/10.1016/s0161-6420(96)30416-8
Constantinou M, Daniell M, Snibson GR, Vu HT, Taylor HR (2007) Clinical efficacy of moxifloxacin in the treatment of bacterial keratitis: a randomized clinical trial. Ophthalmology 114(9):1622–1629. https://doi.org/10.1016/j.ophtha.2006.12.011
Shah VM, Tandon R, Satpathy G et al (2010) Randomized clinical study for comparative evaluation of fourth generation fluoroquinolones with the combination of fortified antibiotics in the treatment of bacterial corneal ulcers. Cornea 29(7):751–757. https://doi.org/10.1097/ICO.0b013e3181ca2ba3
Sharma N, Arora T, Jain V et al (2016) Gatifloxacin 0.3% versus Fortified Tobramycin-cefazolin in treating nonperforated bacterial corneal ulcers: randomized controlled trial. Cornea 35(1):56–61. https://doi.org/10.1097/ICO.0000000000000664
Mah FS (2004) Fourth-generation fluoroquinolones: new topical agents in the war on ocular bacterial infections. Curr Opin Ophthalmol 15(4):316–320. https://doi.org/10.1097/00055735-200408000-00007
Lalitha P, Srinivasan M, Manikandan P et al (2012) Relationship of in vitro susceptibility to moxifloxacin and in vivo clinical outcome in bacterial keratitis. Clin Infect Dis 54(10):1381–1387. https://doi.org/10.1093/cid/cis189
Oldenburg CE, Lalitha P, Srinivasan M et al (2013) Emerging moxifloxacin resistance in Pseudomonas aeruginosa keratitis isolates in South India. Ophthalmic Epidemiol 20(3):155–158. https://doi.org/10.3109/09286586.2013.790978
Bucci FA Jr, Nguimfack IT, Fluet AT (2016) Pharmacokinetics and aqueous humor penetration of levofloxacin 1.5% and moxifloxacin 0.5% in patients undergoing cataract surgery. Clin Ophthalmol 2:783–789. https://doi.org/10.2147/OPTH.S91286
Chung JL, Lim EH, Song SW et al (2013) Comparative intraocular penetration of 4 fluoroquinolones after topical instillation. Cornea 32(7):1046–1051. https://doi.org/10.1097/ICO.0b013e31828d6d9e
Kowalski RP, Romanowski EG, Mah FS, Shanks RM, Gordon YJ (2010) Topical levofloxacin 1.5% overcomes in vitro resistance in rabbit keratitis models. Acta Ophthalmol 88(4):e120–e125. https://doi.org/10.1111/j.1755-3768.2010.01897.x
Tajima K, Miyake T, Koike N et al (2015) Two different concentrations of topical levofloxacin for the treatment of multidrug-resistant Pseudomonas aeruginosa keratitis. J Ocul Pharmacol Ther 31(10):636–641. https://doi.org/10.1089/jop.2015.0026
Ventola CL (2015) The antibiotic resistance crisis: part 1: causes and threats. P T 40(4):277–283
Pendleton JN, Gorman SP, Gilmore BF (2013) Clinical relevance of the ESKAPE pathogens. Expert Rev Anti Infect Ther 11(3):297–308. https://doi.org/10.1586/eri.13.12
World Health Organization (2017) WHO publishes list of bacteria for which new antibiotics are urgently needed [Internet]. https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed. Accessed 21 Aug 2023
Willcox MD (2011) Review of resistance of ocular isolates of Pseudomonas aeruginosa and staphylococci from keratitis to ciprofloxacin, gentamicin and cephalosporins. Clin Exp Optom 94(2):161–168. https://doi.org/10.1111/j.1444-0938.2010.00536.x
Porter G, Grills N (2016) Medication misuse in India: a major public health issue in India. J Public Health (Oxf) 38(2):e150–e157. https://doi.org/10.1093/pubmed/fdv072
Funding
The original Asia Cornea Society Infectious Keratitis Study was funded by the following organizations: Asia Cornea Foundation, Singapore; Alcon, TX, USA; Allergan, Ireland; Bausch & Lomb, NY, USA; Santen Pharmaceutical, Japan; Project Orbis, NY, USA. None of the sponsors or funding organizations had a role in this study’s design; in the collection, analysis and interpretation of data; in the writing of the report; nor in the decision to submit the article for publication.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by WBK, RL, MHP and DTHT. The first draft of the manuscript was written by WBK and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Wei-Boon Khor has received honorarium by Santen Pharmaceuticals for presentations; and received support by the Asia Cornea Society for meetings. Jodhbir S. Mehta and Donald TH Tan are co-inventors of the EndoGlide, and have financial interests in the device (AngioTech, Reading, Pennsylvania, USA/Network Medical Products, North Yorkshire, UK). Ai Ling Tan has received honorarium for lectures from the Singapore Association of Pharmaceutical Industries. The following authors have no relevant financial or non-financial interests to disclose.: Rajamani Lakshminarayanan, Venkatesh Prajna, Prashant Garg, Namrata Sharma, Alvin Young, Panida Goseyarakwong, Vilavun Puangsricharern, Mercy Halleluyah Periayah, Roger Beuerman.
Ethical approval
This study adhered to the tenets of the Declaration of Helsinki. Ethics review was waived for this study by the SingHealth Institutional Review Board as only bacterial isolates with no patient identifiers were provided for this laboratory study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Khor, WB., Lakshminarayanan, R., Periayah, M.H. et al. The antibiotic resistance profiles of Pseudomonas aeruginosa in the Asia Cornea Society Infectious Keratitis Study. Int Ophthalmol 44, 361 (2024). https://doi.org/10.1007/s10792-024-03270-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10792-024-03270-y