Abstract
Purpose
To study the prevalence, antibiotic susceptibility profile, clinical outcomes and plasmid-mediated transfer of colistin resistance (CLR) among Gram-negative bacilli (GNB) isolates from different ocular infections.
Design
Prospective case–control study in eastern India.
Methods
Consecutive ocular samples with GNB isolates from clinically diagnosed cases of microbial keratitis, infectious endophthalmitis and orbital infections were included. Inclusion criteria were significant GNB growth from ocular samples and > 6 weeks follow-up. Clinical outcomes were determined by disease-specific criteria for each clinical group. Antibiotic susceptibility was tested by broth microdilution for colistin and Kirby–Bauer disc diffusion method for others. Plasmid detection for CLR genes mcr-1 and mcr-2 genes was done by standard protocols.
Results
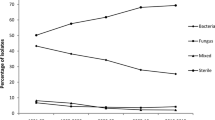
Sixty GNB isolates were studied. Overall prevalence of CLR (intrinsic plus acquired) was 40% (n = 24), acquired being 37.5% of CLR isolates (n = 9). The prevalence varied from 45.5% (10/22) and 45% (9/20) in microbial keratitis and infectious endophthalmitis, respectively, to 26.3% (5/19) in orbital infections. Clinical outcomes in CLR patients were significantly worse in microbial keratitis (p = 0.018) and orbital infections (p = 0.018), and comparable to colistin-susceptible ones (p = 0.77) in infectious endophthalmitis. CLR isolates had significantly higher resistance to Amikacin, Gentamicin and Ceftazidime but were susceptible to Piperacillin, Carbapenems and fluoroquinolones. Plasmids mcr-1 and mcr-2 were detected in 6.25% (n = 1) and 25%(n = 4), respectively, of the 16 tested isolates.
Conclusions
CLR is highly prevalent in ocular isolates and affects clinical outcomes. CLR isolates may still remain susceptible to Carbapenems, Piperacillin and fluoroquinolones. Plasmid mcr-1- and mcr-2-mediated CLR remains low in ocular infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antimicrobial resistance is a major challenge in modern medicine, especially with few new molecules in the pipeline. As in systemic infections, antimicrobial resistance in ocular isolates has been on the rise over the past two decades [1]. This led to increased chances of ocular morbidity with vision-threatening conditions like microbial keratitis, infectious endophthalmitis and infections of the orbit and lacrimal apparatus [1].
Among bacterial pathogens, Gram-negative bacilli (GNB) infections, though less common than Gram-positive organisms, are more often associated with fulminant infections and poorer outcomes [2,3,4]. There is also an increasing trend towards antimicrobial resistance in GNB infections, especially in Asian countries [2, 3]. Multidrug resistant (MDR) GNB were till recently, uniformly susceptible to Carbapenem group of drugs such as Imipenem and Meropenem. But with emergence of Carbapenem resistance, there has been an increasing need for newer antibiotics to which such GNB would be susceptible. Colistin, a Polymyxin antibiotic (Polymyxin E), discovered in 1940’s, that had been discontinued due to severe renal and neurological side-effects due to high doses being used [5], has now emerged as the last line of defence against such MDR-GNB infections [6]. Though colistin is a reserve drug for GNB infections, it is now being increasingly used as a stand-alone antibiotic for treatment of MDR-GNB infections resistant to first line antibiotics, both in systemic and ocular infections such as keratitis and endophthalmitis [7,8,9,10]. Expectedly, there has been an emergence of resistance to colistin as well [11].
Colistin resistance is of serious concern as there are no new drugs in the pipeline for GNB infections [11,12,13,14]. It may be intrinsic (inherent) or acquired. Intrinsic resistance to colistin is seen in Burkholderia cepacia and members of Enterobacteriaceae like Serratia marcescens, Proteus species, Morganella species and Providencia species and is mainly due to chromosomal mutation, which is transmitted vertically during multiplication of microbes. All other GNB have acquired resistance to colistin, which is plasmid mediated and transferred horizontally and hence carries a threat for rapid spread in same or different GNB species [11,12,13,14]. The acceptable range for colistin resistance is less than 10% of GNB infections, in most countries [15]. There are ongoing surveillance mechanisms in place for detection and determination of colistin resistance in systemic infections (e.g. European antimicrobial surveillance report or EARS-Net) [16, 17]. These surveillances have revealed increasing trends in colistin resistance in GNB infections [16,17,18].
Several case reports are available on the use of local (topical or intravitreal) colistin in the treatment of MDR-GNB keratitis or endophthalmitis [7,8,9,10]. These studies have described the dosage and frequency of colistin administration for effective management of MDR-GNB infections [7,8,9,10]. However, no extensive data are available on the prevalence and clinical outcomes in colistin-resistant ocular GNB infections [19, 20].
In the current study, we have analysed the prevalence of colistin-resistant (CLR) and colistin-susceptible (CLS) Gram-negative isolates from different ocular infections at a tertiary eye care centre in eastern India. In addition, we analysed the overall antibiogram profile of CLR and CLS infections and the correlation between CLR and clinical outcomes in different ocular infections. In a smaller subset of our isolates, we also investigated the prevalence of mcr-1 and mcr-2 plasmids as these could account for horizontal transfer of CLR.
Methods
A prospective case–control study was conducted on consecutive samples from clinically diagnosed ocular infections with significant Gram-negative bacterial growth, at L V Prasad Eye Institute, Bhubaneswar, India. Institutional ethics committee approval (2017-91-IM-17) was taken, and tenets of Declaration of Helsinki were adhered to. Electronic medical records (EMR) of the patients were referred to for collection of relevant clinical data. The CLR isolates were designated as cases and the CLS as controls. The ocular infections were divided into 3 clinical groups: microbial keratitis, infectious endophthalmitis and orbital infections. The following inclusion and exclusion criteria were followed during collection of clinical and microbiological data:
Inclusion criteria
-
1.
Clinically diagnosed cases of microbial keratitis, infectious endophthalmitis, panophthalmitis and orbital infections.
-
2.
Significant growth of Gram-negative bacteria, as per Jones criteria for significant bacterial growth from ocular samples [21].
-
3.
Patients with ≥ 6 weeks of follow-up, after initial intervention.
Exclusion criteria
-
1.
Patients with significant growth of organisms other than GNB, such as Gram-positive or anaerobic organisms.
-
2.
Follow-up ≤ 6 weeks.
-
3.
Patients with any recent serious illness for which they had been hospitalized or treated.
The primary aim of the study was to determine prevalence of CLR in ocular GNB isolates in different ocular infections. Secondary aims were to correlate CLR with clinical outcomes and to compare susceptibility of CLR isolates to non-colistin antibiotics with that of CLS isolates.
Microbiological processing
Samples of corneal scraping, half corneal buttons, vitreous biopsy, anterior chamber exudates, intraocular lens, eviscerated contents, abscess pus, lacrimal sac, nasolacrimal duct implants, or canalicular contents were inoculated into solid media (Blood and Chocolate agars, Sabouraud dextrose and Potato dextrose agars) and liquid media (Brain–heart infusion broth, Robertson’s cooked meat media, Thioglycollate broth) and incubated at 37 °C. Any significant growth obtained was then processed and identified by standard microbiological procedures and confirmed by Vitek 2 Compact identification system. Antibiotic susceptibility of the isolates was tested by Kirby–Bauer disc diffusion method (discs supplied by HiMedia, India), for all antibiotics except colistin, as part of routine microbiology, according to Clinical and Laboratory Standard Institute (CLSI) guidelines. The antibiotic panel tested for the significant Gram-negative isolates were Chloramphenicol, Amikacin, Gentamicin, Gatifloxacin, Ofloxacin, Ciprofloxacin, Moxifloxacin, Ceftazidime, Imipenem, and Piperacillin–Tazobactam. Organisms were marked as susceptible or resistant (intermediately susceptible were also considered as resistant) to any of these antibiotics as per the zone of inhibition standard chart provided by HiMedia.
Colistin susceptibility was tested by Broth Microdilution test with colistin sulphate powder (Sisco Research Laboratory, Maharashtra), since Kirby–Bauer disc diffusion, E-test or Vitek-AST is not currently acceptable for colistin, as per EUCAST (European Committee for Antimicrobial Susceptibility Testing) and CLSI subcommittee on colistin resistance guidelines [22]. Isolates were marked as susceptible or resistant to colistin as per this subcommittee’s guidelines [22]. Screening for plasmid-mediated CLR was done in microbiologically proven resistant isolates by plasmid DNA extraction and PCR with mcr-1 (309 bp) and mcr-2 (567 bp) probes, according to standard EUCAST protocol [23].
Clinical data collection
The clinical data collected for the 3 clinical groups were presenting symptoms, visual acuity, duration of illness, interventions following which the present complaint occurred, history of hospital admission, recent colistin use, provisional diagnosis, medical and surgical interventions, and treatment outcomes. The criteria for good or poor clinical outcome of the patients in the 3 clinical groups of microbial keratitis, infectious endophthalmitis and orbital infections are given in Table 1. Clinical data as obtained from EMR were matched with these criteria for assessing the outcome.
Statistical analysis
Data were arranged on Excel spread sheet. Relevant statistical analysis was done using Medcalc’s statistical software version 18.11 for statistical analysis. CLR and CLS data were compared using paired t test for clinical outcome in the 3 clinical groups and for antibiotic susceptibility results. Relative risk (RR) and confidence interval (CI) were calculated, and a p-value of < 0.05 was taken as statistically significant.
Results
Of a total of 60 GNB isolates in the study, 40% (n = 24) were CLR; among the CLR isolates, 62.5% (n = 15/24) were intrinsically resistant to colistin and 37.5% (n = 9/24) had acquired resistance. Thus, isolates with confirmed acquired resistance to colistin constituted 15% (n = 9/60) of all GNB isolates tested in our study. The overall prevalence of colistin resistance in the 3 clinical groups of microbial keratitis, infectious endophthalmitis and orbital infections and the individual isolates in each group is shown in Table 2. Though overall prevalence of CLR was higher in microbial keratitis and infectious endophthalmitis (nearly equal), acquired resistance was the highest for orbital infections (80%) as compared to 30% and 22.2% for keratitis and endophthalmitis, respectively (Table 2).
Clinical outcomes in different ocular infections
The clinical outcomes in each of the 3 clinical groups, as per criteria defined in the study, are given in Table 1. Significantly poorer outcome was noted in the microbial keratitis (95% CI = 1.2–6.2, RR = 2.7, p = 0.02) and orbital infection (95% CI = 1.3–11.2, RR = 3.8, p = 0.02) groups among CLR isolates, while the outcomes were comparable between CLR and CLS isolates in the infectious endophthalmitis group (95% CI = 0.51–1.64, RR = 0.91, p = 0.77) (Table 3).
Antibiotic susceptibility in CLR and CLS isolates
Significant difference in antibiotic susceptibility between CLR and CLS isolates was seen for Amikacin (95% CI = 1.07–6.1, RR = 2.5, p = 0.03), Gentamicin (95% CI = 1.02–4.9, RR = 2.2, p = 0.05) and Ceftazidime (95% CI = 0.05–0.88, RR = 0.22, p = 0.03) (Table 4). The susceptibility pattern to other non-colistin antibiotics for the intrinsic and acquired resistant isolates in the CLR group is as shown in Table 5. Multidrug resistance (resistance to 3 or more antimicrobials from different antimicrobial groups) was similar between CLR and CLS isolates [62.5% CLR (n = 15/24) versus 61.1% CLS (n = 22/36) (p = 0.91)]. The isolates with intrinsic CLR showed higher resistance to all the antibiotics in the panel compared to the acquired CLR group, except for Ceftazidime and Piperacillin–Tazobactum, for which the acquired CLR isolates were more commonly resistant. Among CLR isolates, 25% (n = 4/16) of intrinsic CLR and 12.5% (n = 1/8) of acquired CLR were also resistant to Imipenem (Table 6).
Plasmid-mediated resistance in CLR isolates
Plasmid-mediated colistin resistance (mcr-1 and mcr-2) was tested in 16 of the 24 CLR isolates. Plasmid mcr-1 was amplified in 1 isolate of Enterobacter cloacae (microbial keratitis isolate) that also had good clinical outcome. Plasmid mcr-2 was amplified in 3 isolates of Burkholderia cepacia (1 microbial keratitis isolate and 2 endophthalmitis isolates) all of which had good clinical outcomes, and 1 Pseudomonas aeruginosa (microbial keratitis) that had poor outcome. Thus, mcr-2 plasmid was found in 25% (n = 4) of the 16 tested isolates. Notably, Burkholderia is considered to have intrinsic CLR, while Enterobacter and Pseudomonas have acquired CLR.
Discussion
Our study highlights the high prevalence of CLR in ocular GNB infections and its association with poor clinical outcomes in microbial keratitis and orbital infections. We found a high overall prevalence of CLR (40%), a significant proportion (37.5%) of which was acquired. Acquired resistant isolates to colistin constituted 15% of all GNB isolates tested, which is much higher than the reported prevalence from western countries [14, 24, 25] and from one study in our country [26], but lower than that reported from another study in our country [27]. We have also described the overall antibiotic susceptibility profile in CLR infections and the impact of CLR on clinical outcomes in different types of ocular infections. Significantly, we tested CLR in our isolates by Broth microdilution method, as per the recommendations of EUCAST and CLSI subcommittee on colistin resistance guidelines [22]. Colistin is a large molecule which does not diffuse uniformly in media for antibiotic susceptibility testing by Kirby–Bauer disc diffusion method, while the Vitek method shows major errors while testing for colistin susceptibility. Hence, Broth microdilution is currently the only acceptable method for confirming colistin resistance [22]. The acceptable cut-off for CLR in GNB infections is 10%, though incidence is steadily rising in Mediterranean and South-East Asia [15]. In European countries, the prevalence of CLR was found to vary from a low of 0.67% in Enterobacteriaceae to a high of 6.2% and 7.7% in Klebsiella pneumoniae and Enterobacter cloacae isolates, respectively [16, 24]. In the USA, CLR has been reported to vary between 3 and 4% [25]. Our finding of 15% acquired resistance to colistin in ocular isolates is higher than all the above reports. In India itself, one study reported CLR prevalence to be less than 10% (i.e. > 90% isolates are CLS) [26], while another study reported CLR prevalence in systemic infections as a high of 28.7% (n = 27/94) [27], by Broth microdilution method. To our knowledge, this is the first comprehensive report of CLR infections in the eye. The earlier reports of ocular CLR infections were isolated case reports [19, 20] and did not provide an overall perspective of CLR in ocular infections. Several factors could account for the high prevalence of CLR in our isolates. Colistin use, till now, is not very tightly regulated, leading to frequent use of the drug, occasionally in suboptimal doses, in infections still susceptible to lower antibiotics. Colistin is also widely used commercially for prophylaxis and better yield in agriculture, farm and dairy animals and in pisciculture [28]. This leads to leaching of colistin into the environment in low doses, thereby inducing CLR in environmental saprophytes, which later find their way to human bodies [28]. Incidentally, none of our CLR patients had any history of prior administration of colistin on recall, in contrast to the reports in systemic CLR infections [16]. Thus, CLR may exist in the environment even in the absence of prior exposure to colistin [24]. The impact of CLR on clinical outcomes in different types of ocular infections, however, remains ambiguous. We found poorer clinical outcomes among CLR patients with microbial keratitis and orbital infections but not in endophthalmitis. Patients with CLR microbial keratitis had higher requirement for TPK (therapeutic penetrating keratoplasty), poorer final visual outcome (final BCVA < 20/400), corneal perforations, endophthalmitis and even evisceration or phthisis. Those with orbital CLR infections had higher associations with delayed wound healing (> 2 weeks), and partially patent tube or nasolacrimal duct post-intervention. However, in infectious endophthalmitis, the clinical outcomes were similar for both CLR and CLS infections. We speculate that the lack of difference in clinical outcomes between CLR and CLS isolates in endophthalmitis could be due to greater anatomical and functional damage, as compared to keratitis and orbital and lacrimal apparatus infections, irrespective of the antibiotic susceptibility of the organisms.
The incidence of MDR (acquired resistance to at least one agent in 3 or more antimicrobial categories) [29] in our study, though high (nearly two-thirds), was largely similar between CLR and CLS groups. Overall, significantly higher resistance was seen for Amikacin, Gentamicin and Ceftazidime among the CLR isolates compared to the CLS ones. No such difference in susceptibility between CLR and CLS groups was found for any other antibiotics in the panel, in case of microbial keratitis and orbital infections. But in infectious endophthalmitis, the CLR isolates were also marginally more resistant to fluoroquinolones (Ciprofloxacin, Ofloxacin, Gatifloxacin, Moxifloxacin) than the CLS isolates. Although the resistance rates for fluoroquinolones as well as Imipenem and Piperacillin–Tazobactum were higher than a previous report on GNB endophthalmitis in south India, no significant difference was seen between CLR and CLS isolates for these antibiotics [30]. Notably, 83.3% (n = 20/24) of the CLR isolates in our study were susceptible to Imipenem, 62.5% (overall n = 15/24) to all the 4 fluoroquinolones, while 58.3% (n = 14/24) were susceptible to Amikacin, respectively. Conversely, 16.7% (n = 4/24) of Imipenem resistant and 37.5% (n = 9/24) and 41.7% (n = 10/24) of fluoroquinolones and Amikacin resistant isolates, respectively, were also resistant to colistin. This co-resistance of 16.7% (n = 4/24) ocular isolates to colistin and Carbapenem was much lower than the 52% (n = 14/27) of co-resistant isolates to colistin and Meropenem in systemic infections in our country [27]. Thus, it appears that a reappraisal of antibiotic hierarchy is necessary for future decision making in antimicrobial therapy.
The presence of plasmids carrying drug resistant genes signifies the possibility of rapid horizontal transfer of plasmid specific drug resistance to other susceptible members of the same species or a different species of bacteria [31]. We found mcr-1 and mcr-2 in only 1 and 4 isolates, respectively, among the 16 tested isolates. The clinical outcome was good in all except one of these five isolates. We suspect that the plasmids may have been lost while the isolates were stocked in culture media. Besides, we tested only for mcr-1 and mcr-2 genes, while many others (mcr-3, 4 and 5) have been described to mediate CLR [32]. Hence, it appears that plasmid mcr-1- and mcr-2-mediated colistin resistance is not widely prevalent among ocular isolates in our region, though some other Asian countries have reported a high prevalence of mcr-1-mediated plasmid resistance in the environment [28].
Interestingly, CLR isolates of organisms considered to be intrinsically resistant appeared to have higher overall resistance to non-colistin antibiotics (except Ceftazidime and Piperacillin–Tazobactum) in the panel compared to the acquired resistant ones. Intrinsic resistance is mediated by chromosomal mutations in two regulatory systems PhoPQ and PmrAB, which are responsible for modifying GNB lipopolysaccharide (LPS) formation and other cellular activities [33]. Thus, these mutations confer resistance to both colistin and other cationic antimicrobials. On the other hand, mcr-1 encodes phosphoethanolamine transferase enzyme which attaches a phosphoethanolamine to lipid A of GNB LPS which reduces the electrostatic attraction between colistin and anionic outer membrane of GNB. This, however, does not interfere with colistin-mediated disruption of outer membrane and hence action by other cationic antimicrobials [33]. This might explain the increased antimicrobial resistance among intrinsically resistant CLR isolates compared to the acquired resistant ones, in our study. We followed the CLSI (Clinical and Laboratory Standard Institute) guidelines for different antibiotic susceptibility tests. Accordingly, we used the Kirby–Bauer disc diffusion method for the other antibiotics in the panel and not broth microdilution as done for colistin. In a small subgroup, we tested samples by both Kirby–Bauer and broth microdilution and it did not affect the final results of our study (data not shown).
We did not find any data on concentration of colistin in vitreous following intravitreal or intravenous administration or into deeper corneal tissues following topical application. Since colistin is prepared as fortified antibiotic from parenteral colistimethate sodium powder for topical and intravitreal use in ocular infections, we speculate that tissue concentration of colistin on corneal surface or intravitreally would be much higher compared to that after intravenous injection. Our study was also limited by the use of isolates from a limited geographical area, and by the use of only two of the five genes implicated in plasmid-mediated resistance [32]. Nevertheless, we have demonstrated for the first time the high prevalence of CLR in different types of ocular infections. CLR resulted in poorer clinical outcomes, at least in microbial keratitis and orbital infections. However, CLR isolates may remain susceptible to ‘lower-order’ antibiotics, and these should be considered in the management of CLR infections. Finally, plasmid mcr-1- and mcr-2-mediated transfer of resistance in ocular infections appears to be limited in CLR, though it needs further study.
References
Asbell PA, Sanfilippo CM, Pillar CM et al (2015) Antibiotic resistance among ocular pathogens in the United States five-year results from the Antibiotic Resistance Monitoring in Ocular Microorganisms (ARMOR) surveillance study. JAMA Ophthalmol 133(12):1445–1455
Kunimoto DY, Das TP, Sharma S et al (1999) Microbiologic spectrum and susceptibility of isolates: part I. Postoperative endophthalmitis. Am J Ophthalmol 128(2):240–242
Sheng Y, Sun W, Gu Y et al (2011) Endophthalmitis after cataract surgery in China, 1995–2009. J Cataract Refract Surg 37:1715–1722
Irvine WD, Flynn HW Jr, Miller D et al (1992) Endophthalmitis caused by Gram negative organisms. Arch Ophthalmol 110:1450–1454
Lauren ML, Ly N, Anderson D et al (2010) Resurgence of colistin: a review of resistance, toxicity, pharmacodynamics and dosing. Pharmacotherapy 30(12):1279–1291
European Medicines Agency (2016) Updated advice on the use of colistin products in animals within the European Union: development of resistance and possible impact on human and animal health, pp 1–56
Jain R, Murthy SI, Motukupally SR, Jain M (2014) Use of topical colistin in multiple drug-resistant Pseudomonas aeruginosa bacterial keratitis. Cornea 33(9):923–927
Samant P, Ramugade S (2014) Successful use of intravitreal and systemic colistin in treating multidrug resistant Pseudomonas aeruginosa postoperative endophthalmitis. Indian J Ophthalmol 62(12):1167–1170
Dogra M, Sharma M, Katoch D, Dogra M (2018) Management of multi drug resistant endogenous Klebsiella pneumoniae endophthalmitis with intravitreal and systemic colistin. Indian J Ophthalmol 66(4):596–597
Taneja M, Senthil S, Paulose R et al (2016) Intravitreal colistin for multidrug resistant acute endophthalmitis following Descemet-stripping endothelial keratoplasty due to Klebsiella pneumoniae. JCRS Case Rep 4(3):52–56
Bialvaei A, Kafil HS (2015) Colistin, mechanisms and prevalence of resistance. Curr Med Res Opin 31(4):707–721
Karaiskos I, Giamarellou H (2014) Multidrug resistant and extensively drug resistant Gram-negative pathogens: current and emerging therapeutic approaches. Expert Opin Pharmacother 15(10):1351–1370
Loutet SA, Valvano MA (2011) Extreme antimicrobial peptide and polymyxin B resistance in the genus Burkholderia. Front Microbiol 2:159
Olaitan AO, Morand S, Rolain JM (2014) Mechanisms of polymyxin resistance: acquired and intrinsic resistance in bacteria. Front Microbiol 5(643):1–18
Falagas ME, Rafailidis PI, Matthaiou DK (2010) Resistance to polymyxins: mechanisms, frequency and treatment options. Drug Resist Updates 13:132–138
Jayol A, Poirel L, Dortet L, Nordmann P (2016) National survey of colistin resistance among carbapenemase-producing Enterobacteriaceae and outbreak caused by colistin-resistant OXA-48-producing Klebsiella pneumoniae, France, 2014. Euro Surveill 21(37):30339
Terveer EM, Nijhuis R, Crobach M et al (2017) Prevalence of colistin resistance gene (mcr-1) containing Enterobacteriaceae in faeces of patients attending a tertiary care hospital and detection of a mcr-1 containing, colistin susceptible E. coli. PLoS One 12(6):e0178598
Arjun R, Gopalakrishnan R, Nambi PS et al (2017) A study of 24 patients with colistin-resistant Gram-negative isolates in a tertiary care hospital in South India. Indian J Crit Care Med 21(5):317–321
Fernandes M, Vira D, Medikonda R, Kumar N (2015) Extensively and pandrug resistant Pseudomonas aeruginosa keratitis: clinical features, risk factors and outcome. Graefes Arch Clin Exp Ophthalmol 254(2):315–322
Sanghi S, Pathengay A, Jindal A et al (2014) Acute-onset post-operative endophthalmitis caused by multidrug-resistant Klebsiella pneumoniae. Clin Ophthalmol 8:1783–1785
Jones DB, Liesegang TJ, Robinson NM (1994) Laboratory diagnosis of ocular infections. Cumitech 13A. Am Soc Microbio 31
Recommendations for MIC determination of colistin (polymyxin E) as recommended by the joint CLSI-EUCAST Polymyxin Breakpoints Working Group (2016). Published on www.eucast.org. Accessed July 2017
Cavaco L, Mordhorst H, Hendriksen R (2016) PCR for plasmid-mediated colistin resistance genes, mcr-1 and mcr-2 (multiplex). Laboratory protocol. European Union Reference Laboratory. Antimicrobial Resistance. Version 2
Prim N, Turbau M, Rivera A et al (2017) Prevalence of colistin resistance in clinical isolates of Enterobacteriaceae: a four-year cross-sectional study. J Infect. https://doi.org/10.1016/j.jinf.2017.09.008
Poirel L, Jayol A, Nordmann P (2017) Polymyxins: antibacterial activity, susceptibility, testing and resistance mechanisms encoded by plasmids or chromosomes. Clin Microbiol Rev 30(2):557–597
Veeraraghavan B, Jesudason MR, Prakasah JA et al (2018) Antimicrobial susceptibility profiles of Gram-negative bacteria causing infections collected across India during 2014–2016: study for monitoring antimicrobial resistance trend report. Indian J Med Microbiol 36:32–36
Ramesh N, Prasanth M, Ramkumar S et al (2016) Colistin susceptibility of Gram negative clinical isolates from Tamil Nadu, India. Asian Biomed 10(1):35–39
Liu YY, Wang W, Walsh TR et al (2016) Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis 16:161–168
Magiorakos AP, Srinivasan A, Carey RB et al (2012) Multidrug resistant, extensively drug resistant and pandrug resistant bacteria: an international expert proposal for interim standard definition for acquired resistance. Clin Microbiol Infect 18(3):268–281
Jindal A, Pathengay A, Khera M et al (2013) Combined ceftazidime and amikacin resistance among Gram-negative isolates in acute-onset post-operative endophthalmitis: prevalence, antimicrobial susceptibilities and visual outcome. J Ophthalmic Inflamm Infect 3:62. https://doi.org/10.1186/1869-5760-3-62
Norberg P, Bergstrom M, Jethava V et al (2011) The IncP-1 plasmid backbone adapts to different host bacterial species and evolves through homologous recombination. Nat Commun 2:268. https://doi.org/10.1038/ncomms1267
Rebelo AR, Bortolaia V, Kjeldgaard JS et al (2018) Multiplex PCR for detection of plasmid-mediated colistin resistance determinants, mcr-1, mcr-2, mcr-3, mcr-4 and mcr-5 for surveillance purposes. Euro Surveill. https://doi.org/10.2807/1560-7917.ES.2018.23.6.17-00672
Exner M, Bhattacharya S, Christiansen B et al (2017) Antibiotic resistance: what is so special about multi-drug resistant Gram-negative bacteria? GMS Hyg Infect Control 12. ISSN2196-5226
Acknowledgements
We thank to Aparajita Mullick, Silpa Priyadarshini, Manas Ranjan Barik, Savitri Sharma, Shivaji Sisinthy, Prity Sahay, Swati Shradhhanjali—Ocular Microbiology and Molecular Biology, L. V. Prasad Eye Institute, Bhubaneswar and Hyderabad.
Funding
This study was funded by HERF (Hyderabad Eye Research Foundation).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors report any conflict of interest.
Ethical approval
Institutional ethics committee approval (2017-91-IM-17) was taken and tenets of Declaration of Helsinki were adhered to. This study does not contain any studies with animals, performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants, whose clinical information had been included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mitra, S., Basu, S., Rath, S. et al. Colistin resistance in Gram-negative ocular infections: prevalence, clinical outcome and antibiotic susceptibility patterns. Int Ophthalmol 40, 1307–1317 (2020). https://doi.org/10.1007/s10792-020-01298-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-020-01298-4