Abstract
Brainstem degeneration in Parkinson’s disease (PD) may explain the occurrence of many non-motor symptoms in this condition. Purposes of the present work were to investigate brainstem function in PD through a battery of vestibular-evoked myogenic potentials (VEMP) allowing a comprehensive brainstem exploration and to correlate VEMP findings with symptoms related to brainstem involvement. Cervical (cVEMP), masseter (mVEMP) and ocular (oVEMP) VEMPs were investigated in 24 PD patients and compared with those recorded in 24 age-matched controls. Presence of symptoms ascribable to brainstem dysfunction, such as daytime sleepiness, REM sleep behavior disorder and depression, was investigated through Epworth Sleepiness Scale, Parkinson’s Disease Sleep Scale, REM Sleep Disorder Screening Questionnaire (RBD-SQ) and Geriatric Depression Scale. Postural instability was additionally assessed through mini-BESTest. The frequency of alteration of VEMPs in patients was 83.3 % when considering the whole set and 41.7 % for cVEMP, 66.7 % for mVEMP and 45.8 % for oVEMP. This was significantly different from controls, with absence being the prevalent alteration in PD. A significant inverse correlation between the number of altered VEMPs and mini-BESTest and a direct correlation with RBD-SQ were found. The VEMP battery under study allowed the identification of brainstem dysfunctions in PD patients, which correlated with clinical tests suggestive of postural and REM sleep disorders. VEMPs might represent a valuable tool of brainstem assessment in PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brainstem involvement represents a key passage in the pathological spreading of Parkinson’s disease [1]: it occurs early, often precedes degeneration of substantia nigra neurons and is associated with the presence of non-motor symptoms such as sleep disorders and depression [2]. These features are likely the result of both direct brainstem lesions and of its misconnections with higher structures. A mismodulation of physiological stimuli processing, which may involve brainstem–subcortical connections, has been suggested by neurophysiological studies and, in turn, may reflect specific symptoms of the disease [3]. Among neurophysiological methods, vestibular-evoked myogenic potentials (VEMPs) are an expression of central oligosynaptic volleys which pathways lay at different levels of the brainstem. So far, three typologies of VEMPs have been characterized: the cervical VEMP (cVEMP) corresponds to the vestibulo-collic reflex and is mediated by an ipsilateral disynaptic pathway involving the medial vestibulospinal tract and the XI cranial nerve nucleus [4]. The masseter VEMP (mVEMP) corresponds to the vestibulo-masseteric reflex [5–7] and is mediated by a disynaptic crossed and bilateral connection between the vestibular complex and the trigeminal nerve nuclei [8–10]. The ocular VEMP (oVEMP) represents the vestibulo-ocular reflex and is mediated by a disynaptic crossed pathway linking the Vestibular Nuclei (VN) to the III cranial nerve nucleus, via the medial longitudinal fasciculus [11]. These VEMPs have been successfully used already, singularly or in combination, in neurological disorders involving the brainstem [12]. In PD, cVEMPs only have been investigated with the main focus on relationships of central vestibular excitability with clinical signs of postural instability [13] or therapeutic intervention [14].
We hypothesized that the application of a battery of VEMPs (cVEMP, mVEMP and oVEMP) may be able to indirectly assess brainstem function along its whole extension. Accordingly, here we (a) assessed cVEMPs, mVEMPs and oVEMPs in a cohort of patients with established PD; (b) compared frequency of VEMP alterations between PD and matched controls; (c) correlated VEMP findings with clinical features of PD and symptoms ascribable to brainstem involvement. We conclude that this VEMP battery is a quick and easy way of investigation of brainstem in PD and correlates with simple tests of balance and sleep.
Materials and methods
Participants
Twenty-four patients with established idiopathic PD (14 males and 10 females; aged 66.2 ± 6.8 years; disease duration 6.1 ± 3.4 years) and 24 healthy controls (15 males and 9 females aged 61.9 ± 10.3 years) were enrolled. All patients had no past or present history of vestibular disorders, hearing loss, muscular and osteoarticular cervical conditions. Participants were evaluated in the morning, patients in ON phase, to minimize potential EMG artifacts due to the lack of dopaminergic control, on motor symptoms. The study protocol was approved by the local ethical committee (ID prot. N. 987, 19/09/2011) and all subjects gave their written informed consent prior to inclusion in the study.
Clinical evaluation
Patients underwent thorough clinical examination with the administration of the Unified Parkinson Disease Rating Scale (UPDRS) and Hoehn and Yahr scale (H&Y). Symptoms ascribable to brainstem dysfunction were assessed through a battery of the following self-administered tests: Epworth Sleepiness Scale (ESS), for detection of excessive daily somnolence in PD [15]; Parkinson’s Disease Sleep Scale (PDSS) that evaluates a wide range of nocturnal symptoms affecting the general quality of sleep in PD [16]; REM Sleep Behavior Disorder Screening Questionnaire (RBD-SQ), which has high sensitivity and specificity in PD [17]; Geriatric Depression Scale (GDS), and finally, the Mini Balance Evaluation Systems Test (Mini-BESTest), for detection of balance disorders and postural instability [18].
VEMP assessment
All subjects underwent bilateral recording of cVEMP, mVEMP and oVEMP from the active sternocleidomastoid (SCM), masseter (MM) and inferior oblique (IOM) muscles, respectively. EMG responses were recorded through surface electrodes positioned on the target muscles in a belly-to-tendon montage, as detailed elsewhere [4, 6, 11]. Recordings were performed in a quiet room, with participants comfortably sitting on a chair with supports for neck, head and arms. Subjects were instructed to contract target muscles steadily at 30–50 % of their maximal voluntary contraction, with the aid of a visual feedback. Rectified and unrectified EMG activity was recorded (CED 1902 quadsystem amplifier), amplified (×5000), filtered (5–5,000 Hz) and sampled (10 kHz) within a temporal window of 200 ms (50 ms pre-stimulus), using an analog/digital converter (CED 1401power) with Signal 5.0 software on a PC. Vestibular stimulation was induced via click stimuli (300–500, 0.1 ms, 5 Hz, 140 dB SPL) produced by an attenuator (CED 3505 HP) driven by software (CED Signal 5.0 script for VEMP) and released either to the right or left ear through calibrated stereophonic earphones (TDH-49P earphones, Telephonics). For each VEMP the following parameters were measured: (a) onset and peak latency of the first wave (i.e., p13 for the cVEMP, p11 for the mVEMP and n10 for the oVEMP) and peak latency of the second wave (i.e., n23 for the cVEMP and p15 for the oVEMP), on averaged unrectified EMG; the n15 wave of the mVEMP was not assessed as it is undetectable in normal hearing people [7]; (b) interside peak latency difference between the first waves; (c) absolute amplitudes either for a single peak (p11) or peak-to-peak (p13/n23 and n10/p15); (d) corrected amplitude (background muscle activation/absolute amplitude), which was normalized, for comparisons with controls [19]; (e) amplitude asymmetry ratio [20].
Criteria for abnormality were set as follows: (a) peak latencies above 2.5 SD of control values; (b) corrected amplitudes below 2.5 SD of controls; (c) absence of the response. Severity of abnormalities was scored increasingly according to detection of no alteration, delay, amplitude reduction, or absence of the response. A mean score ± SD was then calculated for each single VEMP as well as for the whole VEMP battery (total VEMP score).
Statistical analysis
Statistical analysis was performed using SPSS 16.0 for Windows (Chicago, IL, USA). Results were expressed as mean ± SD or frequencies. Pearson’s χ 2 test and Mann–Whitney U test were used for comparisons between groups and Bonferroni’s correction for multiple comparisons applied, where appropriate. Correlations between clinical and VEMP findings were performed calculating the Spearman’s correlation coefficient. Statistical significance was set at p < 0.05.
Results
Clinical findings
Twelve out of 24 patients (50 %) had tremor-dominant disease, 10 (41.6 %), rigid-dominant form and 2 (8.4 %) exhibited a postural-instability gait-difficulty phenotype. Patients had consistent response to dopaminergic treatment and no signs of fluctuations, dyskinesias, wearing-off or other symptoms attributable to prolonged use of L-DOPA. As summarized in Table 1, mean H&Y was 2.4 ± 0.7, with 9 patients above H&Y = 2.5. None of the patients had cognitive impairment or dementia assessed through MMSE. Nineteen out of 24 patients (79.2 %) had at least one score susceptible of a sleep disturbance. Among these, 12 (50 %) marked scores above the cut-off for ESS, 7 (29.2 %) above the cut-off for RBD and 4 (16.7 %) had low mean PDSS scores. Moreover, 9 patients (37.5 %) had high scores on the GDS, ascribable to some degree of depression and 9 patients (37.5 %) had low scores on Mini-BESTest, indicating the presence of postural instability. Patients and controls did not differ significantly by age and gender.
VEMP alterations
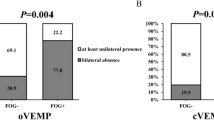
Figure 1 shows the VEMP battery recorded in a representative control subject and in a PD patient. Averaged raw parameters are shown in Table 2. After Bonferroni correction for multiple comparisons, no difference in latencies was detected for all VEMPs between patients and controls. In patients, amplitudes were significantly smaller for mVEMPs (p = 0.0001), borderline for oVEMPs (p = 0.01) and normal for cVEMPs. When the whole battery was considered, VEMPs were significantly more altered in patients than controls (p = 0.0003). In particular, in the PD group, 4/24 (16.6 %) subjects had a normal VEMP battery, 10/24 (41.7 %) had one altered VEMP, 3/24 (12.5 %) had two altered VEMPs and 7/24 (29.2 %) had all three VEMPs abnormal. By comparison, frequencies in the control group were 18/24 (75 %), 5/24 (20.8 %), 1/24 (4.2 %) and 0, respectively. Considering each VEMP separately (Fig. 2), the rate of abnormality in patients was 41.7, 66.7 and 45.8 % for cVEMP, mVEMP and oVEMP, respectively, compared with 4.2, 16.7 and 12.5 % in controls (all p < 0.01). No significant differences were seen in patients, between unilateral and bilateral alteration for each VEMP: in particular, the cVEMP was altered unilaterally in six patients (25 %) and bilaterally in 4 patients (16.7 %); the oVEMP showed unilateral and bilateral alterations in 5 (20.8 %) and six patients (25 %), respectively. The mVEMP was altered unilaterally in 6 patients (25 %) and bilaterally in 9 (37.5 %), following right stimulation, and unilaterally in 9 patients (37.5 %) and bilaterally in 5 patients (20.8 %) following left stimulation. Taking the whole VEMP set, patterns of alterations were the following: delay 6.9 %, low amplitude 2.8 %, absence 41.7 % with significantly higher proportion of absent responses (p < 0.01); in controls, alterations were equally distributed (delay 4.2 %, low amplitude 2.8 % and absence 4.2 %). Patterns of alterations recorded in each single VEMP are shown in Table 3. Patients significantly differed from controls also in the extent of alterations: the total VEMP score in patients was 8.13 ± 6.28 versus 1.79 ± 3.99 in controls (p = 0.0001). Mean scores for each single VEMP are reported in Table 3.
Cervical (cVEMP), masseter (mVEMP) and ocular (oVEMP) VEMPs recorded from sternocleidomastoid (SCM), masseter (MM) and inferior oblique (IOM) muscles in control and PD subjects. In the control subject, cVEMP appears as an ipsilateral p13/n23 wave, mVEMP appears as a bilateral and symmetric p11 wave followed by an n21 wave and oVEMP as a contralateral n10/p15 wave. In the patient, oVEMPs and mVEMPs are absent and amplitude of cVEMP is reduced. Arrows indicate the time of stimulus delivery
Clinical–neurophysiological correlations
The number of altered VEMPs correlated inversely with Mini-BESTest scores (rho = −0.458; p = 0.024) and directly with RBD-SQ scores (rho = 0.633; p = 0.001) (Fig. 3). Total VEMP scores also significantly correlated with RBD-SQ (rho = 0.665; p = 0.0004). This was still significant for cVEMP (rho = 0.694; p = 0.0001) and oVEMP (rho = 0.427 and p = 0.04) but not for mVEMP. No significant correlations were found with age, disease duration, LEDD, H&Y stage, UPDRS, GDS and PDSS scores.
Discussion
This study demonstrated that a VEMP battery, composed of cVEMP, mVEMP and oVEMP, allowed distinguishing significantly between patients with established PD and healthy controls. The frequency of cVEMP abnormalities in PD is in line with that found elsewhere [13]. By contrast, as far as we know, no studies exploring mVEMP and oVEMP in PD exist; therefore, no comparison is possible. Considering that in PD, cVEMP amplitude is ameliorated by l-DOPA administration [14] and that our patients were examined in ON phase, a potential higher rate of VEMP alterations would have missed in our study. Few of our controls also exhibited VEMP alterations, which can be explained by the well-known age-related effects on VEMPs, attributed to a progressive reduction of peripheral receptors as well as of excitability of nuclear vestibular neurons with age [21]. In agreement with previous studies on cVEMPs in PD, absent responses and low amplitudes were the prevalent patterns of alteration detected in our patients. These findings are consistent with cVEMP abnormalities described in Alzheimer’s disease [22]. In neurodegenerative disorders, loss of neurons within the brainstem as well as impairment of interneuron connections may account for the higher rate of decrease or loss of the reflex response. A paradigm of the possible underlying mechanism may come from studies on multiple sclerosis patients in which delay is replaced by absence of signal, when the damage leads to a block of synaptic transmission [12].
Although vestibular nuclei are not reported as being directly affected by the pathological process in PD [1], a hypothesis is that their function can be altered in PD. On one hand, the presence of D2 receptors on vestibular neurons [23] as well as the influence of L-DOPA on cVEMP amplitude [14] suggests a modulatory role for the dopaminergic system on vestibular function. On the other hand, disruption of vestibular interconnections with brainstem structures [24, 25], which are affected by the PD process [1], may have a role in VEMP impairment in PD. Finally, a possible role for an abnormal vestibular function at peripheral level should also be considered. In this regard, peripheral vestibular alterations in PD have been excluded [26] although their presence can be associated with postural abnormalities, such as lateral trunk flexion [27]. In our cohort, a role for peripheral vestibular alteration is not likely as it was excluded before enrolment.
VEMPs are thought to play a role in postural stabilization of the head during gait. In this respect, the significant correlation found between VEMP alterations and Mini-BESTest scores suggests that brainstem may represent a site in which a neural misprocessing, responsible for postural instability in PD, may occur. The finding that abnormalities of the trigemino-cervical reflex are linked to postural alteration in PD [28] is in line with this assumption. In PD, balance impairment has been linked to a failure in non-dopaminergic high-order processing of incoming sensory inputs for adequate motor responses and to impairment in attention, which is another important feature in PD [29]. However, postural instability may also reflect a dysfunction in low-level postural sensory integration, in which reciprocal connections between the pedunculopontine nucleus (PPN), the mesencephalic reticular formation and VN seem to play a central role [30].
A significant correlation was also found between VEMP alterations and RBD-SQ, which is a screening test for REM sleep behavior disorder (RBD). Cholinergic and monoaminergic dysregulations in PPN, locus subcoeruleus/subcoeruleus complex, periacqueductal gray matter and pontine tegmentum have been accounted for RBD in PD [31]. In particular, impairment of PPN cholinergic neurons linked to brainstem areas, including the VN, is considered responsible for muscle tone dysregulation in RBD [31]. With regard to the monoaminergic system, its association with RBD in humans has been proved by a lesser radiologically detectable locus coeruleus/subcoeruleus complex in PD patients with RBD [25]. We speculate that misconnections in networks involving the vestibular complex, all the aforementioned areas and, possibly, other brainstem nuclei, may underlie the association between VEMP alterations and high scores on the RBD-SQ.
In conclusion, our study demonstrated that VEMP battery is impaired in patients with PD and this correlates with postural instability and RBD. This adds insights to the relationship between disruption of brainstem connections and presence of non-motor symptoms which occur especially at earliest stages of the disease. The emerged results prompt further studies to test the usefulness of VEMPs also at earlier stages of the disease, when recognition of mechanisms leading to the disease is poorer but some non-motor symptoms have already occurred.
References
Braak H, Del Tredici K, Rűb U, de Vos RAI, Jansen Steur ENH, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Grinberg LT, Rueb U, di Lorenzo Alho AT, Heinsen H (2010) Brainstem pathology and non-motor symptoms in PD. J Neurol Sci 289:81–88
Nonnekes J, Geurts ACH, Oude Nijhuis AB (2014) Reduced StartReact effect and freezing of gait in Parkinson’s disease: two of a kind? J Neurol 261:943–950
Colebatch JG, Halmagyi GM, Skuse NF (1994) Myogenic potentials generated by a click-evoked vestibulocollic reflex. JNNP 57:190–197
Deriu F, Tolu E, Rothwell JC (2003) A short latency vestibulomasseteric reflex evoked by electrical stimulation over the mastoid in healthy humans. J Physiol 553:267–279
Deriu F, Tolu E, Rothwell JC (2005) A sound-evoked vestibulomasseteric reflex in healthy humans. J Neurophysiol 93:2739–2751
Deriu F, Ortu E, Capobianco S et al (2007) Origin of sound-evoked EMG responses in human masseter muscles. J Physiol 580:195–209
Giaconi E, Deriu F, Tolu E, Cuccurazzu B, Yates BJ, Billig J (2006) Transneuronal tracing of vestibulo-trigeminal pathways innervating the masseter muscle in the rat. Exp Brain Res 171:330–339
Cuccurazzu B, Deriu F, Tolu E, Yates BJ, Billig I (2007) A monosynaptic pathway links the vestibular nuclei and masseter muscle motoneurons in rats. Exp Brain Res 176:665–671
Deriu F, Giaconi E, Rothwell JC, Tolu E (2010) Reflex responses of masseter muscles to sound. Clin Neurophysiol 10:1690–1699
Rosengren SM, McAngus Todd NP, Colebatch JG (2005) Vestibular-evoked extraocular potentials produced by stimulation with bone-conducted sound. Clin Neurophysiol 116:1938–1948
Magnano I, Pes GM, Pilurzi G et al (2014) Exploring brainstem function in multiple sclerosis by combining brainstem reflexes, evoked potentials, clinical and MRI investigations. Clin Neurophysiol 125:2286–2296
Pollak L, Prohorov T, Kushnir M, Rabey M (2009) Vestibulocervical reflexes in idiopathic Parkinson disease. Clin Neurophysiol 39:235–240
Potter-Nerger M, Reich M, Colebatch JC, Deuschl G, Volkmann J (2012) Differential effect of Dopa and subthalamic stimulation on vestibular activity in Parkinson’s disease. Mov Disord 10:1268–1275
Kumar S, Bhatia M, Behari M (2003) Excessive daytime sleepiness in Parkinson’s disease as assessed by Epworth Sleepiness Scale (ESS). Sleep Med 4:339–342
Chaudhuri KR, Pal S, DiMarco A et al (2002) The Parkinson’s disease sleep scale: a new instrument for assessing sleep and nocturnal disability in Parkinson’s disease. JNNP 73:629–635
Nomura T, Inoue Y, Kagimura T, Uemura Y, Nakashima K (2011) Utility of the REM sleep behavior disorder screening questionaire (RBD-SQ) in Parkinson’s disease patients. Sleep Med 12:711–713
Franchignoni F, Horak F, Godi M, Nardone A, Giordano A (2010) Using psychometric techniques to improve the balance evaluation system’s test: the mini-BESTest. J Rehabil Med 4:323–331
Papathanasiou ES, Murofushi T, Akin FW, Colebatch JG (2014) International guidelines for the clinical application n of cervical vestibular evoked myogenic potentials: an expert consensus report. Clin Neurophysiol 125:658–666
Welgampola MS, Colebatch JG (2001) Vestibulocollic reflexes: normal values and the effect of age. Clin Neurophysiol 113:1971–1979
Lopez I, Honrubia V, Baloh RW (1997) Aging and the human vestibular nucleus. J Vestib Res 7:77–85
Birdane L, Incensulu A, Gurbuz MK, Ozbabalik D (2012) Sacculocollic reflex in patients with dementia: is it possible to use it for early diagnosis? Neurol Sci 33:17–21
Vibert N, Serafin M, Crambes O, Vidal PP, Műhlethaler M (1995) Dopaminergic agonists have both presynaptic and postsynaptic effects on the guinea pig’s vestibular nucleus neurons. Eur J Neurosci 7:555–562
Schuerger RJ, Balaban CD (1999) Organization of the coeruleo-vestibular pathway in rats, rabbits and monkeys. Brain Res Rev 30:189–217
Halberstadt AL, Balaban CD (2007) Selective anterograde tracing of the individual serotonergic and nonserotonergic components of the dorsal raphe nucleus projection to the vestibular nuclei. Neuroscience 147:207–223
Pastor MA, Day BL, Marsden CD (1993) Vestibular induced postural responses in Parkinson’s disease. Brain 116:1177–1190
Vitale C, Marcelli V, Furia T et al (2011) Vestibular impairment and adaptive postural imbalance in parkinsonian patients with lateral trunk flexion. Mov Disord 2:1458–1463
Perrotta A, Serrao M, Bartolo M et al (2005) Abnormal head nociceptive withdrawal reaction to facial nociceptive stimuli in Parkinson’s disease. Clin Neurophysiol 116:2091–2098
Yarnall A, Rochester L, Burn DJ (2011) The interplay of cholinergic function, attention, and falls in Parkinson’s disease. Mov Disord 26:2496–2503
Aravamuthan BR, Angelaki DE (2012) Vestibular responses in the macaque pedunculopontine nucleus and central mesencephalic reticular formation. Neuroscience 223:183–199
Boeve BF, Silber MH, Saper CB et al (2007) Pathophysiology of REM sleep behavior disorder and relevance to neurodegenerative disease. Brain 130:2770–2788
Acknowledgments
The authors are thankful to Prof. J.C. Rothwell for his helpful suggestions and Mr. Paul Gottlieb for language revision. Dr Francesca Ginatempo was supported by Fondazione Banco di Sardegna Sassari (Italy).
Conflict of interest
The authors report no conflicts.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Natale, E.R., Ginatempo, F., Paulus, K.S. et al. Abnormalities of vestibular-evoked myogenic potentials in idiopathic Parkinson’s disease are associated with clinical evidence of brainstem involvement. Neurol Sci 36, 995–1001 (2015). https://doi.org/10.1007/s10072-014-2054-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-014-2054-4