Abstract
Alzheimer disease (AD) is a progressive, irreversible entity associated with behavioral changes, memory loss and disturbance of daily life activities. Current diagnostic tools can detect neuronal degeneration in AD only after irreversible damage that already existed. Vestibular evoked myogenic potentials (VEMP) test utilizes the sacculocolic reflex arc and has been used in neuro-otology practice for many years. In this study, we aim to determine if VEMP can be used for diagnostic purposes at the earliest stages of AD. Twenty patients with AD and ten patients with mild cognitive impairment were enrolled in this study. Control group was 30 healthy volunteers with no neurological or otological diseases. Abnormal VEMP responses were found in most of the patients at different stages of AD. VEMP test may be used for early diagnosis of AD. Also, it may provide a novel advancement in understanding of pathophysiology of this disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dementia is a chronic, progressive and irreversible entity associated with behavioral changes, memory loss and disturbance of daily life activities. Alzheimer disease (AD) is known as the most common type of dementia [1]. There is no still definitive treatment for this unfortunate disease since described by Alois Alzheimer in 1901. Patients need long-term and meticulous care and it costs a significant economical burden on patient, caregivers and whole community health service [2]. Since then, early diagnosis and preventive medicine become more important than ever. Unfortunately, current diagnostic tool can detect neuronal degeneration only after irreversible damage that already existed. Immunohistochemistry using monoclonal antibodies, single-photon emission computed tomography (SPECT), detection of phosphorylated-tau proteins in cerebrospinal fluid and positron emission tomography (PET) are some of the techniques that are suggested for early diagnosis. However, they cannot be used in routine practice because of their high costs and limited availability in every medical center [3].
From where or how does AD starts have not been apparent yet. In postmortem histopathological studies, amyloid plaques and neurofibrillar tangles, which are believed to be pathognomonic for AD are detected in neocortex. Pathological changes can disseminate and invade the most part of the brain in advanced stages of the disease. However, a new study suggested that AD starts at sub-structures of brainstem and neocortex will be involved later [3].
Vestibular evoked myogenic potentials (VEMPs) are defined as action potentials from sternocleidomastoid muscle in response to acoustic stimuli. VEMP is a cheap and safe test and patients tolerate it very well most of the time. It utilizes the sacculocolic reflex arc and has been used in neuro-otology practice to detect vestibular system diseases for many years. Since neural pathway of sacculocolic reflex pass through the brainstem, it may provide information about the diseases, in which is brainstem involved [4–6].
The aim of this study was to show brainstem involvement by using VEMP test in Alzheimer patients at different stages and in patients with mild cognitive impairment. Also, we aim to determine whether this test can be used for diagnostic purposes at the early stages.
Material and method
This study was conducted by cooperation of two departments: Department of Otorhinolaryngology and Department of Neurology in Eskisehir Osmangazi University Faculty of Medicine in Turkey. Thirty patients with possible diagnosis of Alzheimer disease according to criteria of National Institute of Neurological and Communicative Disorders and Alzheimer’s Disease and related disorders associated with Alzheimer (NINCS-ARDRA) were enrolled in this study. After detailed neurological and otological examination, all patients underwent neuropsychiatric evaluation using Activity of Daily Living Scale, Geriatric Depression Scale, The Frontal Assessment Battery (FAB), neuropsychiatric inventory and Wechsler memory scale. Besides these test battery, Mini Mental State Exam (MMSE) was applied to all patients by experienced neurologist to evaluate the stage of the disease.
MMSE is widely used as a standardized screening test to evaluate the cognitive status in the patient with dementia. The test includes paper and pencil tasks, simple questions and problems. Every task has some points. At the end of the test any score ≥25 point is normal, between 19 and 25 point is mild–moderate and ≤19 point is moderate–severe dementia.
Control group was 30 healthy volunteers with no neurological or otological diseases. Study group consisted of 15 females and 15 males (mean age 67 ± 9.14 years) and control group of 12 females and 18 males (mean age 61 ± 7.66 years). Detailed otological, neurological and neuropsychiatric examinations were also performed on the control group. Cerebral magnetic resonance imaging, electroencephalography, bed-side vestibular tests, audiometric evaluations and VEMP were applied in the both group. Full biochemical and hematological work-up including thyroid function tests and Vitamin B12 level were obtained for both groups. Patients with limited neck movements and any type of hearing loss were excluded from the study because of false negativity of VEMP response.
The study was approved by Ethical Committee of Eskisehir Osmangazi University. Informed consent was obtained from their primary relatives or care-givers.
VEMP recordings were performed with Medelec Synergy machine (Oxford Instruments Medical Surrey, UK). After appropriate skin cleaning, an active electrode on middle 1/3 of sternocleidomastoid muscle (SCM), reference electrode on sternal notch and ground electrode on the forehead were placed. Test was performed on patients in supine position in a room isolated from noise. Sound stimuli presented through headphones as rarefaction clicks of 0.1 ms of duration and frequency of 5 Hz. In a total, 128 click stimuli were given to each ear with 110 decibels (dB). They were requested to turn their heads to the contralateral side of the acoustic stimuli whenever they heard the sound. Monaural-stimuli were given to right and left, respectively. Electromyographic (EMG) activity of sternocleidomastoid muscle was recorded ipsilaterally. For the reliability of the test, it was performed at least twice. In a total, 120 ears of 60 individuals were tested with VEMP. Prolongation of latency period according to average latency of control group or the absence/decrease of VEMP response was accepted as a pathological result.
SPSS 15.0 (Statistical Package for the Social Sciences, version 15.0, SSPS Inc., Chicago, IL, USA) was used for statistical analysis. Student’s t test was used to compare results of study and control groups. p < 0.05 was accepted as statistically significant.
Results
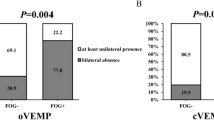
Demographical and clinical characteristics of the subjects are summarized in Table 1. Mean age of patient group is 67.46 ± 9.14 years (range 50–83) and 61 ± 7.66 years (range 50–78) for control group. After the detailed neuropsychiatric evaluation and MMSE, ten patients had diagnosed with mild cognitive impairment, ten patients had diagnosed with mild to moderate AD, and ten patients had moderate to severe AD. In the patient group, VEMP response of 18 (60.1%) patients was obtained bilaterally, but the amplitudes of them were decreased, latency was prolonged in either p13 or n23, or both. Of these 18 patients, eight of them had mild cognitive impairment, six of them had mild to moderate AD and four had moderate to severe AD. In eight patients (26.6%), response was obtained only unilaterally. Mild cognitive impairment diagnosed in two of them, whereas, mild to moderate AD in four patients and moderate to severe AD in two patients. Out of eight patients, VEMP results in the opposite ears were also abnormal in five patients. Delayed p13 or n23 was found. VEMP response was in the normal limit in the opposite ear of the other three patients who had initial stages of impairment. Bilaterally absent VEMP response was found in four patients (13.3%) who have moderate to severe AD (Table 2).
Normal biphasic VEMP responses (p13–n23) were obtained in 60 ears of 30 patients in control group. The results of 60 ears of control group are compared with 44 ears (8 unilateral, 18 bilateral) of patient group with biphasic VEMP response. In the patient group, left side p13, n23 latency were 15.01 ± 2.12 ms, 21.89 ± 2.71 ms, respectively. Mean amplitude value is 127.46 ± 33.0 μv. Right side p13, n23 latency were 15.03 ± 1.92 ms, 21.59 ± 2.44 ms, respectively. Mean amplitude value was 114.34 ± 40.23 μv. In control group, left side p13, n23 latency were 12.7 ± 1.30 ms, 21.33 ± 1.70 ms, respectively. Right side p13, n23 were 13.18 ± 1.25 ms and 21.66 ± 2.19 ms, respectively. Average amplitude was 196.80 ± 67.14 μv for left ear, 114.34 ± 40.23 μv for right ear (Table 3).
Mean latency of p13 in 44 ears of the patient group was longer than the control group (p < 0.05), which was statistically significant. Mean amplitude of response was lower than the control group, which was also statistically significant (p < 0.05). In the patient group, n23 latency was longer than the control group, but there was no statistical difference between them (p > 0.05).
Discussion
The prevalence of Alzheimer disease in Turkey is 5% in elderly population [1]. In every year, the number of case is increasing due to several reasons such as aging population, exposure to chemicals and so on. In 2050, 16 million AD patients are predicted to be present in USA [8]. Unfortunately, there is no curative management to this unfortunate disease, although a lot of studies were performed. Progression of the disease is different in every patient, but most of the time, they cannot perform daily routine activities at some stages and need special care. Due to high economic, social, psychological impacts on the society and caregiver, the preventive recommendations become more important, although there is no enough evidence about the benefit of them. Only serotonin re-uptake inhibitors are recommended for some patients at early stages in a study [9]. Therefore, early diagnosis is very important to use suggested preventive therapies.
Till date, pyramidal neurons of neocortex are accepted to be the most affected part of central nervous system in Alzheimer disease. When AD is diagnosed, neocortex has already been involved irreversibly. Neocortical and hippocampal involvement result in cognitive problems like impairment of memory, speech, judgement and abstract thinking and this status is already a very advanced stage. Most of the time, diagnosis of AD are focuses on these symptoms without considering cautionary signs consisting of depression, anxiety, disturbance of sleep and appetite. These are non-cognitive symptoms and they may be a part of the mild cognitive impairment. According to the latest literature, 12–15% of patients with mild cognitive impairment developed Alzheimer disease per year. Non-cognitive symptoms are accepted to result from degeneration of serotonergic nuclei and reduction of serotonin level from brainstem involvement [3]. In brainstem, 80% of serotonergic neurons are located in the dorsal part of raphe nucleus. In early stages of AD, pathological changes in serotonergic neurons in dorsal raphe nucleus were verified [9, 10]. According to Rüb’s study [9], pathology disseminates from dorsal raphe nucleus to entorhinal cortex, hippocampus, amygdale, orbitofrontal and prefrontal cortex, posterior association cortical regions and finally to primary sensory and motor cortical areas parallel to the progression to the disease. Because of the importance of early diagnosis, several evaluation methods which were expensive and not available in every center have been suggested in the literature. VEMP is suggested to use as a part of the evaluation in some neurological diseases such as MS and Parkinson disease; however, to the best of our knowledge, no study has been performed in the patients with AD at different stages. Sacculucolic reflex pathway starts from saccular macula, and then it consists of inferior vestibular nerve, lateral vestibular nucleus, medial and lateral vestibulospinal tractus, accessory nucleus, accessory nerve and sternocleidomastoid muscle [4, 5]. VEMP test is a clinical manifestation of sacculucolic reflex arc. Lateral vestibular nucleus, medial and lateral vestibulospinal tractus, as well as accessory nucleus are located in brainstem. Therefore, any pathology in the brainstem either in the nucleus or in the serotonin level may alter the VEMP results. Anatomically, sacculocolic reflex pathway does not pass through serotonergic nucleus, but decreased serotonin level in AD may affect the sacculocolic reflex arc and, clinically, abnormal VEMP response is obtained.
VEMP amplitudes can be affected by muscle tension, electrode conduction and location, impulse intensity. In our study, muscle activation was monitored throughout the recording with EMG and maintained at a constant level (50–200 μv). There was no limitation of neck movement in any patient. All the recordings were performed by the same clinician taking care of electrode location and conduction. In the literature, some authors indicated that age influences VEMP amplitudes, whereas age factor on VEMP response is controversial [4]. In the control group, VEMP amplitudes of the subjects in over 60 years of age were not lower than the others. Hence, we thought that age is not an influential factor on VEMP response.
Since serotonergic system in brainstem is expected to involve at early stage of AD, VEMP response supposed to be affected and give some clue for the early diagnosis.
In this study, VEMP was performed to the patients with AD at different stages. VEMP responses have changed in all patients even in the patients with mild cognitive impairment. Prolongation of p13 latency and decrease of amplitude may interestingly indicate beginning of brainstem involvement at the mild cognitive disorder stage; moreover, VEMP response was not obtained in patients with advanced stage of AD. The absence of VEMP response indicates that whole brainstem has been already involved and pathology disseminated to the cortex. Pollak et al. conducted a study of VEMP test on 54 Parkinson patients. They found that 7.4% of patients had bilateral and 37% of patients had unilateral absence of VEMP response. In addition, they concluded that the rate of abnormal VEMP response is higher in Parkinson patients with depression because of the influence of serotonin on the sacculocervical pathways [4]. The experimental study of Halberstadt [11] explored the effect of serotonergic projections from the dorsal raphe nucleus on vestibular nuclei neurons. According to our opinion, the same effect may be acceptable in AD.
In a study with multiple sclerosis (MS) patients, prolongation of p13 latency and decrease of amplitude were found to be associated with demyelinated plaques [5, 7]. Both Parkinson and multiple sclerosis are examples of neurodegenerative diseases like AD in which the brainstem pathways are affected. Several studies suggested that abnormal VEMP response was due to not only peripheral vestibular system, but also brainstem involvement [5, 6, 12, 13]. VEMP test was also performed in patients with brainstem infarct and no VEMP response could be recorded in several studies [6, 12], although, Pollak et al. [14] did not find any significant change on VEMP patterns in small group of patient with brainstem strokes.
In literature, there is no study of VEMP test on Alzheimer patients. According to our opinion, our study is a pioneering, small “pilot” study on Alzheimer patients using VEMP test. In this study, we found abnormal VEMP result in 18 ears of ten patients with mild cognitive impairment. Moreover, two patients demonstrated VEMP on only one side. According to this result, the absence or abnormality of VEMP may be an early sign of brainstem involvement in the beginning of Alzheimer disease. Therefore, we may suggest that VEMP test can be applied on every patient with non-cognitive symptoms or with mild cognitive impairment. Progression to Alzheimer disease may be stopped or delayed by using serotonin receptor mediators or new treatment modalities before neuronal degeneration occurs at neocortex. This study has been conducted with a small group and results need to be supported by wider series. If our idea will be proved, VEMP test could be a part of evaluation in dementia patients.
Conclusion
In conclusion, VEMP test is a clinical test which is cheap, safe, reliable, easy-to-use and tolerable by both physicians and patients. It may help for early diagnosis of AD. Also, it may provide a novel advancement in understanding of pathophysiology of this disease.
References
Arslantaş D, Ozbabalik D, Metintaş S, Ozkan S, Kalyoncu C, Ozdemir G, Arslantas A (2009) Prevalence of dementia and associated risk factors in Middle Anatolia, Turkey. J Clin Neurosci 16(11):1455–1459
Gurvit H (2004) Demans Sendromu, Alzhemier Hastalığı ve Alzhemier Dışı Demanslar. In: İstanbul Üniversitesi Tıp Fakültesi Temel ve Klinik Ders Kitapları, Nöroloji. Nobel, pp 367–417
Simic G, Stanic G, Mladinov M, Jovanov-Milosevic N, Kostovic I (2009) Does Alzheimer’s disease begin in the brainstem? Neuropathol Appl Neurobiol 35(6):532–554
Pollak L, Prohorov T, Kushnir M, Rabey M (2009) Vestibulocervical reflexes in idiopathic Parkinson disease. Neurophysiol Clin 39(4–5):235–240
Versino M, Colnaghi S, Callieco R, Bergamaschi R, Romani A, Cosi V (2002) Vestibular evoked myogenic potentials in multiple sclerosis patients. Clin Neurophysiol 113(9):1464–1469
Heide G, Luft B, Franke J, Schmidt P, Witte OW, Axer H (2010) Brainstem representation of vestibular evoked myogenic potentials. Clin Neurophysiol 121(7):1102–1108
Sartucci F, Logi F (2002) Vestibular-evoked myogenic potentials: a method to assess vestibule-spinal conduction in multiple sclerosis patients. Brain Res Bull 59(1):59–63
Alzheimer’s Association 2010 (2010) Alzheimer’s disease facts and figures. Alzheimers Dement 6(2):158–194
Rub U, Del Tredici K, Schultz C, Thal DR, Braak E, Braak H (2000) The evolution of Alzheimer’s disease-related cytoskeletal pathology in the human raphe nuclei. Neuropathol Appl Neurobiol 26(6):553–567
Kovacs GG, Klöppel S, Fischer I, Dorner S, Lindeck Pozza E, Birner P, Bötefur IC, Pilz P, Volk B, Budka H (2003) Nucleus-specific alteration of raphe neurons in human neurodegenerative disorders. Neuroreport 20(14):73–76
Halberstadt AL, Balaban CD (2007) Selective anterograde tracing of the individual serotonergic and nonserotonergic components of the dorsal raphe nucleus profection to the vestibular nuclei. Neuroscience 147(1):207–223
Chen CH, Young YH (2003) Vestibular evoked myogenic potentials in brainstem stroke. Laryngoscope 113(6):990–993
Murofushi T, Shimizu K, Takegoshi H, Cheng PW (2001) Diagnostic value of prolonged latencies in the vestibular evoked myogenic potential. Arch Otolaryngol Head Neck Surg 127(9):1069–1072
Pollak l, Kushnir M, Stryjer R (2006) Diagnostic value of vestibular evoked myogenic potentials in cerebellar and lower-brainstem strokes. Neurophysiol Clin 36(4):227–233
Author information
Authors and Affiliations
Corresponding author
Additional information
This study had been awarded with 1st rank in 1st Turkish National Otology and Neuro-Otology Congress in Cyprus.
Rights and permissions
About this article
Cite this article
Birdane, L., Incesulu, A., Gurbuz, M.K. et al. Sacculocolic reflex in patients with dementia: is it possible to use it for early diagnosis?. Neurol Sci 33, 17–21 (2012). https://doi.org/10.1007/s10072-011-0595-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-011-0595-3