Abstract
We aimed to estimate the prevalence of overweight in Moroccan patients with rheumatoid arthritis (RA) and its relationships with disease activity, functional disability, structural damage, and immunological status. Two hundred fifty patients with RA were consecutively included. Patients’ characteristics were specified. The following data were collected: age, disease duration, disease activity (evaluated with physical examination data, biological tests (erythrocyte sedimentation rate and C-reactive protein), and the disease activity score (DAS28)), radiographic changes (assessed by the Sharp’s method), functional disability (assessed by using the Health Assessment Questionnaire), extra-articular manifestations, immunological status, and treatment details. Overweight was defined according to the body mass index (BMI) values: underweight, <18.5; normal weight, 18.5–24.9; overweight, 25–29.9; and obesity, ≥30. The mean age of patients was 46.31 ± 12.64 years. The mean disease duration was 9.46 ± 8.43 years. Seventy-five patients (30%) were overweight, 42 (16.8%) were obese, and 133 (53.2%) were normal. Increased BMI was associated with the activity of disease (DAS28) (r = 0.426), structural damage (Sharp total score) (r = 0.297), the rate of rheumatoid factor (r = 0.311), and with the rate of anti-cyclic citrullinated protein antibodies (for all p ≤ 0.01). There were no statistically significant differences in BMI according to gender, dose and duration of corticosteroids, or functional impairment. In our sample, overweight seems to be prevalent in our RA patients. Overweight seems to occur independently of treatment and shown to be mainly associated to disease activity, structural damage, and immunological status. Large studies are needed to confirm those results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overweight and obesity is a state of chronic low-grade inflammation that predisposes people to several diseases and that is increasingly prevalent [1]. Recent data have found a relationship between the increase of body mass index (BMI) and high levels of tumor necrosis factor, interleukin 6, and C-reactive protein [2]. Increasing BMI associates with increased cardiovascular risk independently of many confounders [3]. Rheumatoid arthritis (RA) is the commonest chronic systemic inflammatory disease that leads to joint damage and bone destruction with functional incapacity in the long term and increased mortality [4, 5]. In patients with RA, reduced physical activity and treatment with corticosteroids may increase the risk of overweight [4]. Incoming studies have found that BMI is associated to disease activity, joint erosions, and poor disease outcome [4–6]. This factor may also be complicated by metabolic abnormalities and general organ dysfunction with increased mortality particularly related to cardiovascular diseases [7–9]. The influence of BMI and/or body fat on rheumatoid arthritis disease activity and severity is still unclear but the role of pro-inflammatory cytokines and adipokines has been recently highlighted [1, 3, 8]. Some studies have shown high BMI to be associated with RA and poor disease outcome [4, 8], whereas others have found low BMI to be associated with increased erosion in small joints and decreased survival, with high BMI being protective [1, 10]. The purpose of this study was to estimate the prevalence of overweight in Moroccan patients with RA and its relationships with disease activity, functional disability, structural damage, and immunological status.
Patients and methods
Patients
Patients with RA were included consecutively in this cross-sectional study at the Department of Rheumatology of the University Hospital of Rabat-Sale in Morocco between September 2009 and November 2010. Patients were recruited in consultation or during hospitalization. The local medical ethics committee of the Faculty of Medicine in Rabat approved the research and patients gave their consent for the study. Our research conformed to the Helsinki Declaration and to local legislation. For all patients the following data were collected: age, gender, cigarettes smoking (current smoker, ex-smoker, or never-smoker), the presence or absence of an exercise activity (assessed by self-report concerning regular physical exercise, leisure time, and activities of daily living), age at onset, diagnosis delay (months), disease duration (years), and pain intensity (visual analogue scale (VAS) 0–100 mm, 0 = no pain and 100 = severe pain imaginable). Disease activity was measured clinically using data from physical examination (duration of morning stiffness (minutes), night pain (number of awakenings), number of swollen and tender joints), biologically by using erythrocyte sedimentation rate and C-reactive protein tests, and by the disease activity score in 28 joints (DAS28). Radiographs of hands, wrists, and feet were evaluated by one observer and scored using Sharp’s method as modified by van der Heijde [11] were used to assess structural damage. The Moroccan version of Health Assessment Questionnaire translated and validated in Moroccan population was used to evaluate functional disability [12]. Also, identified were: extra-articular manifestations and immunological abnormalities (rheumatoid factor rate (RF) by Elisa method and anti-cyclic citrullinated protein antibody positivity by Elisa). Treatment (doses and duration) with corticosteroids, disease modifying antirheumatic drugs (DMARD’s), and biologic agents was specified. All parameters were collected at the same time of the day and by a single investigator.
Anthropometric measures
Weight (kilograms) and height (centimeters) were measured and the body mass index (BMI) (weight/height squared) has been calculated. In accordance with World Health Organization standards [8], overweight and obesity were defined by using the body mass index values: underweight, <18.5; normal weight, 18.5–24.9; overweight, 25–29.9; and obesity, ≥30 [13].
Statistics
The statistical package for the social sciences version 13.0 was used for statistical analysis. Data for patients were presented as mean and standard deviations for continuous variables and as frequencies and percentages for categorical variables. Comparisons between more than two groups were assessed using the analysis of variance. Correlations between BMI values and disease variables were performed with Pearson correlation coefficient completed with regression models for significant variables. Results were adjusted for the potential confounders (age, gender, and exercise activity). The significance level of p was set at 0.05.
Results
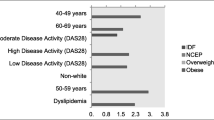
Two hundred fifty patients with RA were included in this cross-sectional study. The characteristics of patients are shown in Table 1. The mean age of our patients was = 46.31 ± 12.64 years (range, 21–72) and the mean disease duration was 9.46 ± 8.43 years. Two hundred twenty-two patients (88.8%) were treated with corticosteroids, 232 (92.8%) were treated with DMARD’s (81.9% treated with methotrexate), and 69 (27.6%) were treated with biologic agents. Seventy-five patients (30%) were overweight, 42 (16.8%) were obese, and 133 (53. 2%) were normal (Table 1). Current smokers had lower BMI values than other groups (p = 0.016). There were no statistically significant differences in BMI according to gender (p = 0.067), presence of extra-articular manifestations (p = 0.234), functional impairment (p = 0.381), or treatment with corticosteroids (dose and duration) (p = 0.343). Using BMI as a categorical variable, we have found that patients with overweight and obesity had significantly higher disease activity (DAS28) (p = 0.006; CI (95%), 0.337–0.777), severe structural damage (Sharp) (p < 0.001; CI (95%), 0.272–0.999), high levels of rheumatoid factor (p = 0.012; CI (95%), 0.163–0.364), and anti-cyclic citrullinated protein antibodies (0.004; CI (95%), 1.472–1.840).
In correlations, increased BMI has significant linear correlation with high disease activity (DAS28), high total Sharp score, the rate of rheumatoid factor, and with the rate of anti-cyclic citrullinated protein antibodies (r = 0.421; for all p ≤ 0.01) (Table 2). In multiple regression models, increased BMI was associated to disease activity (DAS28) (R 2 = 0.372), structural damage (R 2 = 0.488), and the rate of anti-cyclic citrullinated protein antibodies (R 2 = 0.187) (Table 3).
Discussion
In our data, overweight and obesity seem to be frequent in Moroccan patients with RA. Recently, attention has focused on relationship between overweight and rheumatic diseases especially after having shown the role of adipocytes in inflammation [14]. In our sample, increased BMI was significantly associated with higher disease activity (DAS28). Previous studies as the QUEST-RA database had shown similar results and a significant association between body fat and level of C-reactive protein (CRP) in RA patients has been demonstrated recently, although this did not extend to RA disease activity [7, 14–17]. The exact mechanism by which BMI may influence disease activity is not known but is possibly related to the levels of pro-inflammatory cytokines and adipokines (such as leptin and resistin) being produced by the white adipose tissue, contributing to an increased DAS28 score [7, 8, 17]. On the other hand, our data revealed that patients with high BMI had higher Sharp total score. Previous authors [4, 8] have found similar association between overweight and the risk of joint destruction in RA. However, prior studies have identified an association between increasing BMI and lower rates of radiographic progression in RA patients [1, 18]. In fact, there are methodological differences between studies, and a possible protective effect of obesity on radiographic damage was reported in early disease rather than in RA with prolonged duration [1, 16, 17]. This association is seemingly paradoxical, as adipose tissue is a potent source of cytokines and was associated with increased systemic inflammation in RA patients [17, 18]. Another adipokine, adiponectin, has potential anti-inflammatory activity in vascular endothelium and has been shown to be protective against atherosclerosis [17, 19]. A key feature of adiponectin physiology is that circulating levels diminish as adiposity increases. It has be shown that serum adiponectin levels are associated with radiographic damage in RA, suggesting that this adipokine may be a pathogenic mediator of the seemingly paradoxical relationship between increasing adiposity and protection from radiographic damage in RA [16, 17].
Also, our data had shown that increased BMI might be associated with rheumatoid factor and anti-cyclic citrullinated protein antibodies and add the observation that there could be different mechanisms in seropositive and seronegative RA [1, 15]. Indeed, few studies identified a protective effect of obesity only in patients seropositive for RF or anti-cyclic citrullinated protein antibodies [1, 14]. Such findings remain unclear and need further studies.
Finally, our study has found that cigarette smoking associates with reduced BMI. Similar results were reported in the study of Stavropoulos-Kalinoglou et al. [16]. These results should be confirmed in longitudinal studies.
In conclusion, overweight in our RA patients seems to occur frequently and independently of treatment and shown to be mainly associated to disease activity, structural damage, and immunological status. The underlying mechanisms of the association between BMI and disease features should be elucidated. Recognizing complicated relationships between overweight and RA could help to avoid their complications in particular cardiovascular diseases.
References
Van der Helm-van Mil AH, van der Kooij SM, Allaart CF, Toes RE, Huizinga TW (2008) A high body mass index has a protective effect on the amount of joint destruction in small joints in early rheumatoid arthritis. Ann Rheum Dis 67(6):769–774
Duarte GV, Follador I, Cavalheiro CM, Silva TS, Oliveira Mde F (2010) Psoriasis and obesity: literature review and recommendations for management. An Bras Dermatol 85(3):355–360
Stavropoulos-Kalinoglou A, Metsios GS, Koutedakis Y, Nevill AM, Douglas KM, Jamurtas A, van Zanten JJ, Labib M, Kitas GD (2007) Redefining overweight and obesity in rheumatoid arthritis patients. Ann Rheum Dis 66(10):1316–1321
Garcia-Poma A, Segami MI, Mora CS et al (2007) Obesity is independently associated with impaired quality of life in patients with rheumatoid arthritis. Clin Rheumatol 26:1831–1835
Symmons DP (2002) Epidemiology of rheumatoid arthritis: determinants of onset, persistence and outcome. Best Pract Res Clin Rheumatol 16(5):707–722
Sokka T, Toloza S, Cutolo M, Kautiainen H, Makinen H, Gogus F, Skakic V, Badsha H, Peets T, Baranauskaite A, Géher P, Ujfalussy I, Skopouli FN, Mavrommati M, Alten R, Pohl C, Sibilia J, Stancati A, Salaffi F, Romanowski W, Zarowny-Wierzbinska D, Henrohn D, Bresnihan B, Minnock P, Knudsen LS, Jacobs JW, Calvo-Alen J, Lazovskis J, Pinheiro Gda R, Karateev D, Andersone D, Rexhepi S, Yazici Y, Pincus T, QUEST-RA Group (2009) Women, men, and rheumatoid arthritis: analyses of disease activity, disease characteristics, and treatments in the QUEST-RA study. Arthritis Res Ther 11(1):R7
Giles JT, Bartlett SJ, Andersen R, Thompson R, Fontaine KR, Bathon JM (2008) Association of body fat with C-reactive protein in rheumatoid arthritis. Arthritis Rheum 58:2632–2641
Jawaheer D, Olsen J, Lahiff M, Forsberg S, Lähteenmäki J, da Silveira LG, Rocha FA, Magalhães Laurindo IM, da Mota LM Henrique, Drosos AA, Murphy E, Sheehy C, Quirke E, Cutolo M, Rexhepi S, Dadoniene J, Verstappen SM, Sokka T, QUEST-RA (2010) Gender, body mass index and rheumatoid arthritis disease activity: results from the QUEST-RA study. Clin Exp Rheumatol 28(4):454–461
Hippisley-Cox J, Coupland C, Robson J, Brindle P (2010) Derivation, validation, and evaluation of a new QRISK model to estimate lifetime risk of cardiovascular disease: cohort study using QResearch database. BMJ 341:c6624
Elkan AC, Håkansson N, Frostegård J, Cederholm T, Hafström I (2009) Rheumatoid cachexia is associated with dyslipidemia and low levels of atheroprotective natural antibodies against phosphorylcholine but not with dietary fat in patients with rheumatoid arthritis: a cross-sectional study. Arthritis Res Ther 11(2):R37
Van der Heijde DM, van Leeuwen MA, van Riel PL, van de Putte LB (1995) Radiographic progression on radiographs of hands and feet during the first 3 years of rheumatoid arthritis measured according to Sharp’s method (van der Heijde modification). J Rheumatol 22(9):1792–1796
Abourazzak FE, Benbouazza K, Amine B, Bahiri R, Lazrak N, Bzami F, Jroundi I, Abouqal R, Guillemin F, Hajjaj-Hassouni N (2008) Psychometric evaluation of a Moroccan version of health assessment questionnaire for use in Moroccan patients with rheumatoid arthritis. Rheumatol Int 28(12):1197–1203
WHO (1995) Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 854, WHO, Geneva p. 452
Kaufmann J, Kielstein V, Kilian S, Stein G, Hein G (2003) Relation between body mass index and radiological progression in patients with rheumatoid arthritis. J Rheumatol 30(11):2350–2355
Westhoff G, Rau R, Zink A (2007) Radiographic joint damage in early rheumatoid arthritis is highly dependent on body mass index. Arthritis Rheum 56(11):3575–3582
Stavropoulos-Kalinoglou A, Metsios GS, Panoulas VF, Douglas KM, Nevill AM, Jamurtas AZ, Kita M, Koutedakis Y, Kitas GD (2008) Cigarette smoking associates with body weight and muscle mass of patients with rheumatoid arthritis: a cross-sectional, observational study. Arthritis Res Ther 10(3):R59
Giles JT, Allison M, Bingham CO 3rd, Scott WM Jr, Bathon JM (2009) Adiponectin is a mediator of the inverse association of adiposity with radiographic damage in rheumatoid arthritis. Arthritis Rheum 61(9):1248–1256
Hashimoto J, Garnero P, van der Heijde D, Miyasaka N, Yamamoto K, Kawai S, Takeuchi T, Yoshikawa H, Nishimoto N (2009) A combination of biochemical markers of cartilage and bone turnover, radiographic damage and body mass index to predict the progression of joint destruction in patients with rheumatoid arthritis treated with disease-modifying anti-rheumatic drugs. Mod Rheumatol 19(3):273–282
Fairchild AJ, MacKinnon DP (2009) A general model for testing mediation and moderation effects. Prev Sci 10(2):87–99
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ibn Yacoub, Y., Amine, B., Laatiris, A. et al. Prevalence of overweight in Moroccan patients with rheumatoid arthritis and its relationships with disease features. Clin Rheumatol 31, 479–482 (2012). https://doi.org/10.1007/s10067-011-1874-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-011-1874-3