Abstract
The aim of this study was to evaluate the predictive value of biological, radiological and clinical parameters for the progression of radiographic joint damage in rheumatoid arthritis (RA) patients treated with conventional disease-modifying anti-rheumatic drugs (DMARDs). We analyzed the 145 patients with active RA for less than 5 years who were participating in the prospective 1-year randomized controlled trial of tocilizumab (SAMURAI trial) as a control arm treated with conventional DMARDs. Progression of joint damage was assessed by sequential radiographs read by two independent blinded X-ray readers and scored for bone erosion and joint space narrowing (JSN) using the van der Heijde-modified Sharp method. Multivariate analysis revealed that increased urinary levels of C-terminal crosslinked telopeptide of type II collagen (U-CTX-II), an increased urinary total pyridinoline/total deoxypyridinoline (U-PYD/DPD) ratio and low body mass index (BMI) at baseline were independently associated with a higher risk for progression of bone erosion. In addition to these three variables, the JSN score at baseline was also significantly associated with an increased risk of progression of the JSN score and total Sharp score. High baseline U-CTX-II levels, U-PYD/DPD ratio and JSN score and a low BMI are independent predictive markers for the radiographically evident joint damage in patients with RA treated with conventional DMARDs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although rheumatoid arthritis (RA) has features of a systemic disease and capable of exhibiting a variety of extra-articular manifestations, it is predominantly characterized by structural destruction of the joints, leading to functional disability [1–4]. Joint destruction often progresses early in the disease process [5–8], but the process is highly variable from patient to patient [9–12]. The identification of patients with rapid joint destruction very early in the disease process is of critical importance to clinicians wanting to optimize treatment strategies. Indeed, although new biological therapies are highly effective in preserving joint structure, they are expensive and may have side effects. Thus, targeting these treatments to RA patients manifesting rapid progression of the disease may be beneficial.
Several prospective studies have been performed to identify predictive factors indicative of a worse radiological progression of RA [13–31]. The earlier investigations revealed the importance of the rheumatoid factor (RF), inflammation markers or radiographic damage at baseline [13, 14, 16–18, 20, 21], while more recent ones have identified biochemical markers of bone, cartilage and synovial tissue metabolism and catabolic enzymes as being associated with progression in RA [15, 19, 22, 24, 27–29]. Alternatively, RA is also associated with accelerated atherosclerosis and increased cardiovascular mortality and, recently, it has been shown that macrophage inhibitory cytokine 1 (MIC-1), which is linked to clinical events in atherosclerosis, may be involved in the pathological process of erosive joint destruction [32]. The body mass index (BMI) has also been reported to be associated with the radiographic progression of RA, independent of inflammation markers [23, 30, 31], and recent new information suggests the potential involvement of adipokines as regulators of inflammation in RA [33]. These new findings have lead to the recognition of RA as a disease involving a variety of pathological conditions related with joint destruction and made clinicians aware of the fact that RA is a systemic disease in terms of the pathology of the bone and destruction of cartilage. However, to date, there has been no study that has analyzed concomitantly in the same population the independent contribution of these various anthropometric, clinical, laboratory and radiological features to the prediction of disease progression in RA.
The aims of the study reported here were to determine which combination of a few risk factors identified among a panel of clinical, biological and radiological parameters would be powerful in predicting the radiological progression of bone erosion and joint space narrowing (JSN) in RA patients treated with conventional disease-modifying anti-rheumatic drugs (DMARDs).
Methods
Patients and protocol
The patient cohort consists of 148 patients with RA receiving conventional DMARDs who participated in the control arm of the SAMURAI trial described in a recent publication [34]. The aim of the SAMURAI, which was a 52-week-long multi-center clinical trial, was to evaluate the effect of tocilizumab on radiological joint damage. Three hundred and six patients with RA diagnosed according to the American College of Rheumatology criteria [35] were randomly assigned to tocilizumab monotherapy (8 mg/kg intravenously every 4 weeks) or conventional DMARDs. For the DMARDs group, the dose, type and combination of DMARDs and/or immunosuppressants could vary according to disease activity at the discretion of the treating physician. The study protocol was approved by the Ministry of Health, Labor and Welfare of Japan, and by the ethical committee at each participating site, and patients gave their written informed consent.
Radiographic assessment
Posteroanterior radiographs of hands and anteroposterior radiographs of feet were performed at baseline and at weeks 28 and 52 or at the last visit for patients who withdrew from the study prior to week 52. Radiographs were scored using the van der Heijde-modified Sharp method [36, 37] for bone erosion, joint space narrowing (JSN) and total sharp score (TSS) independently by two readers who were well trained and competent to score radiographs in accordance with the method. The readers were blinded to the treatment group and chronological order of the films.
Clinical assessment
The Disease Activity Score on 28 joints (DAS28), clinical improvement in signs and symptoms of RA, tender joint count, swollen joint count, and modified health assessment questionnaire (MHAQ) [38] were assessed at baseline.
Laboratory examinations
Fasting blood samples and the second morning urine samples were obtained from all subjects at clinical visits. C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were measured in the local clinical test laboratory of each investigation site.
To assess bone formation, we measured serum intact-osteocalcin (OC) using a two-site immunoradiometric assay (Mitsubishi Kagaku Iatron, Japan) and serum bone alkaline phosphatase (bone ALP) by an enzyme-linked immunosorbent analysis (ELISA; Quidel, San Diego, CA). Markers of bone resorption included urinary N-terminal crosslinked telopeptide of type I collagen (U-NTX-I), which was measured by an ELISA (Ostex Int, Seattle, WA), and urinary total deoxypyridinoline (U-DPD) and total pyridinoline (U-PYD), measured by a high-performance liquid chromatography (HPLC) assay. Markers of cartilage synthesis included the N-terminal propeptide of type IIA collagen (PIIANP; Linco, St. Louis, MO) and the C-terminal propeptide of type II collagen (PIICP; IBEX Diagnostics, Montreal, Canada). Cartilage degradation was assessed by the urinary excretion of the C-terminal crosslinked telopeptide of type II collagen (CTX-II CartiLaps ELISA; NORDIC Biosciences, Herlev, Denmark). Synovial tissue metabolism was assessed by measuring the urinary excretion of glucosyl–galactosyl–pyridinoline (Glc–Gal–PYD) by HPLC, serum matrix metalloproteinase-3 (MMP-3) by ELISA (Daiichi Pure Chemical, Japan) and serum amyloid protein A (SAA) by a latex immunoassay (LIA; Eiken Chemical, Japan). Other measures included serum interleukin-6 (IL-6) using a chemiluminescent enzyme immunoassay (CLEIA) (Fujirebio Japan), RF by LIA (Mitsubishi Kagaku Iatron, Japan), and immunoglobulin G (IgG) by LIA (Eiken Chemical, Japan).
Statistical analysis
For analyzing the correlation between markers at baseline and at the 52-week radiological progression of joint damage, we normalized the markers by logarithmic transformation when needed. First, the markers were selected by Pearson correlation coefficient with TSS, erosion score, and JSN score (|r| > 0.15). Then, the predictive factors were selected based on the multivariate regression analysis using the backward elimination method, the forward selection method, and the best-subset selection procedure using Mallows’ Cp- adjusted R 2.
The odds ratio of progression in TSS, bone erosion and JSN score according to the levels of these baseline factors were estimated by logistic regression analysis with a 95% confidence interval (95% CI). The progression of joint damage was defined as an increase of TSS of 0.5 or more at 52 weeks.
All statistical analyses were two-sided, and p values <0.05 were considered to be significant. All statistical analyses were carried out using SAS ver. 8.2, TS2MO (SAS Institute, Cary, NC).
Results
One hundred and forty-five patients were included in the intent to treatment (ITT) analyses. Demographics and baseline disease characteristics are shown in Tables 1 and 3. At baseline, the mean age and the disease duration were 53.1 and 2.4 years, respectively. Patients had very active disease, as indicated by a DAS28 score of 6.4 and CRP of 4.9 mg/dl at baseline. The kinds of DMARDs and immunosuppressants used for RA treatment during the study and the number of patients are shown in Table 2.
Bivariate linear correlation analyses showed that baseline values of U-PYD, the ratio U-PYD/DPD, U-CTX-II, U–Glc–Gal–PYD, TSS, erosion score, JSN score, age and BMI were associated significantly with the 1-year increase in all three radiological indices of joint damage, i.e. bone erosion score, JSN score and TSS (Table 3). The baseline levels of U-DPD, S-PIIANP, triglyceride, ferritin also had a significant association with one or two variables among these three radiographic progression parameters (Table 3). None of the clinical indices of disease activity nor the biological parameters of inflammation were associated significantly with radiological progression. In the multivariate analyses, increased levels of U-CTX-II, an increased U-PYD/DPD ratio and decreased BMI were the only independent predictors of the progression of bone erosion (Table 4). Together, these three variables explained 17% of the interindividual variance in the progression of bone erosion. For the progression of JSN and TTS, baseline JSN was also an independent predictor in addition to U-CTX-II, the U-PYD/DPD ratio and BMI (Table 4).
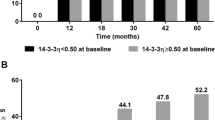
Logistic regression analysis after the categorization of the four predictive variables with the cut-off value of 500 ng/mmol/creatinine in U-CTX-II, median level for the U-PYD/DPD ratio, two cut-off values of 18.5 and 25 kg/m2, respectively, in BMI and a 0 or >0 score in JSN score at baseline showed that the odds ratio for a yearly increase of TSS >0.5 was 2.6- to 9.9-fold higher risk in the high-risk group than in patients with low risk levels (Fig. 1a); the respective figures for progression in erosion score and for progression in JSN were 2.8–4.8 and 1.8–20.0, respectively (Fig. 1b, c). Baseline levels in the categorized groups are shown in Table 5.
Odds ratio (95% confidence interval) of radiological progression associated with high baseline joint space narrowing (JSN), high urinary C-terminal telopeptide of type II collagen (U-CTXII), high urinary total pyridinoline/total deoxypyridinoline (U-PYD/DPD), or low body mass index (BMI). Progression of joint damage over 1 year was defined as an increase >0.5 U of the total Sharp score (a), bone erosion (b) or JSN (c)
Discussion
Based on our analysis of a panel of several demographical, clinical and laboratory parameters of disease activity, we found that increased urinary CTX-II, a high PYD/DPD ratio and low BMI were independent predictors of radiological progression in bone erosion and TTS in patients with RA receiving conventional DMARDs and that baseline JSN was also an independent predictor of radiological progression in JSN and TTS. These results suggest that these factors should be useful in identifying patients at high risk.
The bivariate analyses revealed that the baseline levels of U-PYD, the U-PYD/DPD ratio, U-CTX-II, TSS, erosion score, JSN score, U-Glc–Gal–PYD, age and BMI were significantly associated with the 1-year increase in all three indices of TSS, erosion score and JSN score and that the baseline levels of U-DPD, S-PIIANP, triglycerides and ferritin were significantly associated with one or two variables among these three radiographic progression parameters. However, there was no significant association with radiographic progression in the baseline levels of inflammation markers, MMP-3, hematological parameters, patients-reported functional assessments, such as MHAQ, and objective symptomatic scores. Although several previous studies showed that MMP-3 was predictive of radiological progression [22, 29, 39, 40] in RA, our data and those of Cunnane et al. [41] failed to reveal a significant association. Circulating MMP-3 levels have been reported to be significantly decreased after treatment with methotrexate or sulfasalazine or both together [29, 41–44]. These findings suggest that levels of MMP-3 are dependent on the type, duration and intensity of the pharmacotherapy. It is thus possible that differences in the therapeutic regimen between studies may explain some of the inconsistencies in the relation of MMP-3 to progression. Additional factors may include differences in disease duration and activity and variation in assay characteristics, which are not standardized between studies. Consistent with the results of a recent study [29], we confirmed that patient-reported functional assessments and clinical symptomatic indices were not useful in predicting radiological progression.
Inflammation markers, such as CRP and ESR, have been regarded as useful predictors of joint damage in RA. However, our study confirmed the recent findings of Young-Min [29], showing that when novel and more specific markers of joint tissue metabolism were included in the model, these unspecific laboratory tests were no longer predictive. Among these novel tissue turnover markers, the strongest and most consistent association with progression was observed for urinary CTX-II, a biochemical marker of cartilage degradation, a finding consistent with several previous studies involving patients with early RA receiving MTX or etanercept [19], very early RA receiving the COBRA combination therapy or sulfasalazine alone [45] or late RA treated with conventional DMARDs [29]. Taken together, the results from these previous studies and the current one suggest that urinary CTX-II is predictive of radiological progression across patient populations and independent of the type of therapy. We also found that urinary-Glc–Gal–PYD, a specific biochemical marker of synovial tissue metabolism, was associated significantly with radiographical progression in bivariate analysis. This result was consistent with that of a previous study [19] of early RA patients receiving methotrexate or etanercept. However, urinary-Glc–Gal–PYD did not remain in the final panel of predictors after multivariate analysis, confirming the recent study of Young-Min [29] who showed that Glc–Gal–PYD was predictive in bivariate, but not in multivariate analyses when CTX-II was included in the model. This lack of independent predictive value is likely to be due to the high correlation of Glc–Gal–PYD with CTX-II (r = 0.61, p < 0.001) and suggests that in early active RA, degradation of cartilage is closely linked to synovitis. Whether urinary Glc–Gal–PYD could be an independent predictor of progression in late RA or in patients receiving biological therapies remains to be determined.
Previously published cross-sectional studies found an increased urinary PYD/DPD ratio in patients with RA [46–49]. Our study, however, is the first showing that U-PYD/DPD ratio is an independent predictor of radiological progression. Both PYD and DPD are non-reducible crosslinks of mature collagen molecules, and they are believed to be important factors for maintaining the structure of the collagen fibril network in the matrix of the various tissues, including bone and cartilage. In healthy tissues, the PYD/DPD ratio is highest in cartilage (ratio: 50), intermediate in synovial tissue and tendons (ratio: 15–16) and lowest in bone (ratio: 3.5) [50–52]. The tissue PYD/DPD ratio can be altered in RA tissue, with the latter showing a higher ratio than healthy synovium [23, 51]. In addition, a high tissue PYD/DPD ratio in bone caused by the overhydroxylation of Lys at the helical cross-linking sites in type I collagen has been observed in the hip fracture cases [53] and osteoporosis [54]. Thus, the PYD/DPD ratio may theoretically provide some indication of the type of articular tissue that is predominantly degraded in RA. In our study, this ratio, but not PYD and DPD separately, was associated with radiological progression of bone erosion and JSN independently of CTX-II, which is a specific marker of cartilage degradation and of Glc–Gal–PYD (a specific marker of synovial metabolism), suggesting indeed the added value of this parameter. One possibility is that this ratio partially reflects structural alterations of bone tissue matrix associated with increased bone fragility, as suggested by some ex vivo biochemical studies [53, 54].
We found that high BMI was correlated negatively with the progression of joint erosion and JSN and that patients with lower values (<18.5), defined as underweight, had a 4.8-fold (95% CI 1.1–20) higher risk than the patients with higher BMI (>25) who were defined as overweight. Previously published reports showed a body weight loss due to disease activity [55–58] in RA, although no significant correlation between BMI and inflammation markers was observed at baseline in our study (data not shown). Our results agree with studies published previously by Kaufmann [23], Westhoff [31] and van der Helm-van Mil [30] which showed that high BMI was protective against the radiological progression in early RA. It has been suggested that the relationships between BMI and joint damage are mediated in part by the adipocytokines secreted by fat tissues. Interestingly, we recently reported that increased serum levels of adiponectin—which is negatively associated with BMI—are associated with a greater overall joint destruction in patients with RA [59]. Using a bivariate analysis, we found that triglycerides, but not total cholesterol and its subfractions were negatively correlated with radiological progression. However, in the multiple variable model, triglycerides were not an independent predictors, possibly because of its positive association with BMI (r = 0.29, p < 0.001).
Previously published data showed that high initial radiographical damage evaluated with TSS or the Larsen score was associated with subsequent radiological progression [16, 17] and that the initial erosion score in particular has a predicting value for radiological prognosis [14, 18, 23]. These data were analyzed without biochemical markers of joint tissue turnover as the initial factors; however, we found that baseline radiological joint damage of the extent of JSN was strongly and independently predictive of biochemical markers of joint tissue turnover associated with progression.
We believe that the four independent predictors of radiological progression we identified in this study may reflect different and complementary information of the various pathophysiological processes involved in joint destruction. The baseline Sharp score provides an estimation of the amount of joint destruction that has occurred, on average, during 2.3 years of disease duration before the start of the follow-up. Urinary CTX-II is a dynamic indicator of the rate at which cartilage tissue will deteriorate during the course of the disease. The PYD/DPD ratio may be related to increased bone fragility, and the BMI may provide integrated information on contribution of adipose tissue metabolism to maintain joint tissues health. These four independent predictors were statistically selected using those patients with high disease activity who were participating in the control arm of the SAMURAI study and who had >6 tender joints (of 49 evaluated), >6 swollen joints (of 46 evaluated joints), ESR of >30 mm/h and CRP of >2 mg/dl. These predictors may therefore be beneficial for targeting new biological therapies to patients with rapid progression of joint destruction.
Although our study covered one of the largest ranges of predictive variables for the progression of joint damage ever investigated concomitantly in the same population, due to sample volume limitation we could not analyze a number of the biochemical markers that have been reported to be associated with joint damage in RA, including anti-CCP antibody, cartilage oligomeric matrix protein (COMP) [25, 26, 60], osteoprotegerin (OPG) and Receptor Activator of Nuclear Factor-kappa B Ligand (RANKL) [61]. Our study included patients with RA within 5 years of disease duration, so it remains to be determined whether the same set of predictive factors will also perform similarly in patients with earlier RA. Furthermore, our study could not clarify the prognostic factors in the each type of DMARDs treatment nor whether CTX-II, the PYD/DPD ratio, the JSN score and BMI predict progression independent of the type of DMARDs treatment, since the dose, type and combination of DMARDs and/or immunosuppressants was varied and changed according to disease activity at the discretion of the treating physician in our study. However, our data could provide the prognostic values of CTX-II, PYD/DPD ratio, JSN score and BMI in the actual clinical practice of RA treatment.
In summary, among of a panel of 40 different variables, we identified baseline joint damage, urinary CTX-II, the PYD/DPD ratio and BMI as strong and independent factors of radiological progression in patients with RA receiving conventional DMARDs. If confirmed in other studies, this set of few variables may be useful to identify patients with RA who are at high risk for disease progression.
References
Kuper HH, van Leeuwen MA, van Riel PL, Prevoo ML, Houtman PM, Lolkema WF, et al. Radiographic damage in large joints in early rheumatoid arthritis: relationship with radiographic damage in hands and feet, disease activity, and physical disability. Br J Rheumatol. 1997;36:855–60.
Corbett M, Dalton S, Young A, Silman A, Shipley M. Factors predicting death, survival and functional outcome in a prospective study of early rheumatoid disease over fifteen years. Br J Rheumatol. 1993;32:717–23.
Drossaers-Bakker KW, de Buck M, van Zeben D, Zwinderman AH, Breedveld FC, Hazes JM. Long-term course and outcome of functional capacity in rheumatoid arthritis: the effect of disease activity and radiologic damage over time. Arthritis Rheum. 1999;42:1854–60.
Welsing PM, van Gestel AM, Swinkels HL, Kiemeney LA, van Riel PL. The relationship between disease activity, joint destruction, and functional capacity over the course of rheumatoid arthritis. Arthritis Rheum. 2001;44:2009–17.
Plant MJ, Jones PW, Saklatvala J, Ollier WE, Dawes PT. Patterns of radiological progression in early rheumatoid arthritis: results of an 8 year prospective study. J Rheumatol. 1998;25:417–26.
Fex E, Jonsson K, Johnson U, Eberhardt K. Development of radiographic damage during the first 5–6 yr of rheumatoid arthritis. A prospective follow-up study of a Swedish cohort. Br J Rheumatol. 1996;35:1106–15.
Fuchs HA, Kaye JJ, Callahan LF, Nance EP, Pincus T. Evidence of significant radiographic damage in rheumatoid arthritis within the first 2 years of disease. J Rheumatol. 1989;16:585–91.
van der Heijde DM. Joint erosions and patients with early rheumatoid arthritis. Br J Rheumatol. 1995;34:74–8.
Scott DL, Grindulis KA, Struthers GR, Coulton BL, Popert AJ, Bacon PA. Progression of radiological changes in rheumatoid arthritis. Ann Rheum Dis. 1984;43:8–17.
Gay S, Gay RE, Koopman WJ. Molecular and cellular mechanisms of joint destruction in rheumatoid arthritis: two cellular mechanisms explain joint destruction? Ann Rheum Dis. 1993;52:S39–47.
Ochi T, Iwase R, Yonemasu K, Matsukawa M, Yoneda M, Yukioka M, et al. Natural course of joint destruction and fluctuation of serum C1q levels in patients with rheumatoid arthritis. Arthritis Rheum. 1988;31:37–43.
Hulsmans HM, Jacobs JW, van der Heijde DM, van Albada-Kuipers GA, Schenk Y, Bijlsma JW. The course of radiologic damage during the first six years of rheumatoid arthritis. Arthritis Rheum. 2000;43:1927–40.
van der Heijde DM, van Riel PL, van Leeuwen MA, van ‘t Hof MA, van Rijswijk MH, van de Putte LB. Prognostic factors for radiographic damage and physical disability in early rheumatoid arthritis. A prospective follow-up study of 147 patients. Br J Rheumatol. 1992;31:519–25.
van Zeben D, Hazes JM, Zwinderman AH, Vandenbroucke JP, Breedveld FC. Factors predicting outcome of rheumatoid arthritis: results of a followup study. J Rheumatol. 1993;20:1288–96.
Mansson B, Carey D, Alini M, Ionescu M, Rosenberg LC, Poole AR, et al. Cartilage and bone metabolism in rheumatoid arthritis. Differences between rapid and slow progression of disease identified by serum markers of cartilage metabolism. J Clin Invest. 1995;95:1071–7.
van der Heide A, Remme CA, Hofman DM, Jacobs JW, Bijlsma JW. Prediction of progression of radiologic damage in newly diagnosed rheumatoid arthritis. Arthritis Rheum. 1995;38:1466–74.
Jansen LM, van der Horst-Bruinsma IE, van Schaardenburg D, Bezemer PD, Dijkmans BA. Predictors of radiographic joint damage in patients with early rheumatoid arthritis. Ann Rheum Dis. 2001;60:924–7.
Kaltenhauser S, Wagner U, Schuster E, Wassmuth R, Arnold S, Seidel W, et al. Immunogenetic markers and seropositivity predict radiological progression in early rheumatoid arthritis independent of disease activity. J Rheumatol. 2001;28:735–44.
Garnero P, Gineyts E, Christgau S, Finck B, Delmas PD. Association of baseline levels of urinary glucosyl-galactosyl-pyridinoline and type II collagen C-telopeptide with progression of joint destruction in patients with early rheumatoid arthritis. Arthritis Rheum. 2002;46:21–30.
Boers M, Kostense PJ, Verhoeven AC, van der Linden S. Inflammation and damage in an individual joint predict further damage in that joint in patients with early rheumatoid arthritis. Arthritis Rheum. 2001;44:2242–6.
Vittecoq O, Pouplin S, Krzanowska K, Jouen-Beades F, Menard JF, Gayet A, et al. Rheumatoid factor is the strongest predictor of radiological progression of rheumatoid arthritis in a three-year prospective study in community-recruited patients. Rheumatology (Oxford). 2003;42:939–46.
Green MJ, Gough AK, Devlin J, Smith J, Astin P, Taylor D, et al. Serum MMP-3 and MMP-1 and progression of joint damage in early rheumatoid arthritis. Rheumatology (Oxford). 2003;42:83–8.
Kaufmann J, Kielstein V, Kilian S, Stein G, Hein G. Relation between body mass index and radiological progression in patients with rheumatoid arthritis. J Rheumatol. 2003;30:2350–5.
Verstappen SM, Poole AR, Ionescu M, King LE, Abrahamowicz M, Hofman DM, et al. Radiographic joint damage in rheumatoid arthritis is associated with differences in cartilage turnover and can be predicted by serum biomarkers: an evaluation from 1 to 4 years after diagnosis. Arthritis Res Ther. 2006;8:R31.
Meyer O, Nicaise-Roland P, Santos MD, Labarre C, Dougados M, Goupille P, et al. Serial determination of cyclic citrullinated peptide autoantibodies predicted five-year radiological outcomes in a prospective cohort of patients with early rheumatoid arthritis. Arthritis Res Ther. 2006;8:R40.
Berglin E, Johansson T, Sundin U, Jidell E, Wadell G, Hallmans G, et al. Radiological outcome in rheumatoid arthritis is predicted by presence of antibodies against cyclic citrullinated peptide before and at disease onset, and by IgA-RF at disease onset. Ann Rheum Dis. 2006;65:453–8.
Charni N, Juillet F, Garnero P. Urinary type II collagen helical peptide (HELIX-II) as a new biochemical marker of cartilage degradation in patients with osteoarthritis and rheumatoid arthritis. Arthritis Rheum. 2005;52:1081–90.
Garnero P, Jouvenne P, Buchs N, Delmas PD, Miossec P. Uncoupling of bone metabolism in rheumatoid arthritis patients with or without joint destruction: assessment with serum type I collagen breakdown products. Bone. 1999;24:381–5.
Young-Min S, Cawston T, Marshall N, Coady D, Christgau S, Saxne T, et al. Biomarkers predict radiographic progression in early rheumatoid arthritis and perform well compared with traditional markers. Arthritis Rheum. 2007;56:3236–47.
van der Helm-van Mil AH, van der Kooij SM, Allaart CF, Toes RE, Huizinga TW. A high body mass index is protective on the amount of joint destruction in small joints in early rheumatoid arthritis. Ann Rheum Dis. 2008;67:769–74.
Westhoff G, Rau R, Zink A. Radiographic joint damage in early rheumatoid arthritis is highly dependent on body mass index. Arthritis Rheum. 2007;56:3575–82.
Brown DA, Moore J, Johnen H, Smeets TJ, Bauskin AR, Kuffner T, et al. Serum macrophage inhibitory cytokine 1 in rheumatoid arthritis: a potential marker of erosive joint destruction. Arthritis Rheum. 2007;56:753–64.
Otero M, Lago R, Gomez R, Lago F, Dieguez C, Gomez-Reino JJ, et al. Changes in plasma levels of fat-derived hormones adiponectin, leptin, resistin and visfatin in patients with rheumatoid arthritis. Ann Rheum Dis. 2006;65:1198–201.
Nishimoto N, Hashimoto J, Miyasaka N, Yamamoto K, Kawai S, Takeuchi T, et al. Study of active controlled monotherapy used for rheumatoid arthritis, an IL-6 inhibitor (SAMURAI): evidence of clinical and radiographic benefit from an x ray reader-blinded randomised controlled trial of tocilizumab. Ann Rheum Dis. 2007;66:1162–7.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24.
van der Heijde D. How to read radiographs according to the Sharp/van der Heijde method. J Rheumatol. 2000;27:261–3.
van der Heijde D, Simon L, Smolen J, Strand V, Sharp J, Boers M, et al. How to report radiographic data in randomized clinical trials in rheumatoid arthritis: guidelines from a roundtable discussion. Arthritis Rheum. 2002;47:215–8.
Pincus T, Summey JA, Soraci SA Jr, Wallston KA, Hummon NP. Assessment of patient satisfaction in activities of daily living using a modified Stanford Health Assessment Questionnaire. Arthritis Rheum. 1983;26:1346–53.
Yamanaka H, Matsuda Y, Tanaka M, Sendo W, Nakajima H, Taniguchi A, et al. Serum matrix metalloproteinase 3 as a predictor of the degree of joint destruction during the six months after measurement, in patients with early rheumatoid arthritis. Arthritis Rheum. 2000;43:852–8.
Posthumus MD, Limburg PC, Westra J, van Leeuwen MA, van Rijswijk MH. Serum matrix metalloproteinase 3 in early rheumatoid arthritis is correlated with disease activity and radiological progression. J Rheumatol. 2000;27:2761–8.
Cunnane G, Fitzgerald O, Beeton C, Cawston TE, Bresnihan B. Early joint erosions and serum levels of matrix metalloproteinase 1, matrix metalloproteinase 3, and tissue inhibitor of metalloproteinases 1 in rheumatoid arthritis. Arthritis Rheum. 2001;44:2263–74.
Posthumus MD, Limburg PC, Westra J, van Leeuwen MA, van Rijswijk MH. Serum matrix metalloproteinase 3 levels during treatment with sulfasalazine or combination of methotrexate and sulfasalazine in patients with early rheumatoid arthritis. J Rheumatol. 2002;29:883–9.
Roux-Lombard P, Eberhardt K, Saxne T, Dayer JM, Wollheim FA. Cytokines, metalloproteinases, their inhibitors and cartilage oligomeric matrix protein: relationship to radiological progression and inflammation in early rheumatoid arthritis. A prospective 5-year study. Rheumatology (Oxford). 2001;40:544–51.
Posthumus MD, Limburg PC, Westra J, van Leeuwen MA, van Rijswijk MH. Serum matrix metalloproteinase 3 levels in comparison to C-reactive protein in periods with and without progression of radiological damage in patients with early rheumatoid arthritis. Clin Exp Rheumatol. 2003;21:465–72.
Garnero P, Landewe R, Boers M, Verhoeven A, Van Der Linden S, Christgau S, et al. Association of baseline levels of markers of bone and cartilage degradation with long-term progression of joint damage in patients with early rheumatoid arthritis: the COBRA study. Arthritis Rheum. 2002;46:2847–56.
Muller A, Jakob K, Hein GE. Evaluation of free and peptide bound collagen crosslink excretion in different skeletal diseases. Ann Rheum Dis. 2003;62:65–7.
Astbury C, Bird HA, McLaren AM, Robins SP. Urinary excretion of pyridinium crosslinks of collagen correlated with joint damage in arthritis. Br J Rheumatol. 1994;33:11–5.
Black D, Marabani M, Sturrock RD, Robins SP. Urinary excretion of the hydroxypyridinium cross links of collagen in patients with rheumatoid arthritis. Ann Rheum Dis. 1989;48:641–4.
Seibel MJ, Duncan A, Robins SP. Urinary hydroxy-pyridinium crosslinks provide indices of cartilage and bone involvement in arthritic diseases. J Rheumatol. 1989;16:964–70.
Kaufmann J, Mueller A, Voigt A, Carl HD, Gursche A, Zacher J, et al. Hydroxypyridinium collagen crosslinks in serum, urine, synovial fluid and synovial tissue in patients with rheumatoid arthritis compared with osteoarthritis. Rheumatology (Oxford). 2003;42:314–20.
Takahashi M, Kushida K, Hoshino H, Suzuki M, Sano M, Miyamoto S, et al. Concentrations of pyridinoline and deoxypyridinoline in joint tissues from patients with osteoarthritis or rheumatoid arthritis. Ann Rheum Dis. 1996;55:324–7.
Eyre DR, Koob TJ, Van Ness KP. Quantitation of hydroxypyridinium crosslinks in collagen by high-performance liquid chromatography. Anal Biochem. 1984;137:380–8.
Saito M, Fujii K, Soshi S, Tanaka T. Reductions in degree of mineralization and enzymatic collagen cross-links and increases in glycation-induced pentosidine in the femoral neck cortex in cases of femoral neck fracture. Osteoporos Int. 2006;17:986–95.
Bailey AJ, Wotton SF, Sims TJ, Thompson PW. Post-translational modifications in the collagen of human osteoporotic femoral head. Biochem Biophys Res Commun. 1992;185:801–5.
Helliwell M, Coombes EJ, Moody BJ, Batstone GF, Robertson JC. Nutritional status in patients with rheumatoid arthritis. Ann Rheum Dis. 1984;43:386–90.
Roubenoff R, Roubenoff RA, Ward LM, Holland SM, Hellmann DB. Rheumatoid cachexia: depletion of lean body mass in rheumatoid arthritis. Possible association with tumor necrosis factor. J Rheumatol. 1992;19:1505–10.
Munro R, Capell H. Prevalence of low body mass in rheumatoid arthritis: association with the acute phase response. Ann Rheum Dis. 1997;56:326–9.
Morgan SL, Anderson AM, Hood SM, Matthews PA, Lee JY, Alarcon GS. Nutrient intake patterns, body mass index, and vitamin levels in patients with rheumatoid arthritis. Arthritis Care Res. 1997;10:9–17.
Ebina K, Fukuhara A, Ando W, Hirao M, Koga T, Oshima K, et al. Serum adiponectin concentrations correlate with severity of rheumatoid arthritis evaluated by extent of joint destruction. Clin Rheumatol. 2009;28:445–51.
Lindqvist E, Eberhardt K, Bendtzen K, Heinegard D, Saxne T. Prognostic laboratory markers of joint damage in rheumatoid arthritis. Ann Rheum Dis. 2005;64:196–201.
Geusens PP, Landewé RB, Garnero P, Chen D, Dunstan CR, Lems WF, et al. The ratio of circulating osteoprotegerin to RANKL in early rheumatoid arthritis predicts later joint destruction. Arthritis Rheum. 2006;54:1772–7.
Acknowledgments
The authors wish to thank Takahiro Kakehi, B.Sc., Tamiko Kuraishi, B.Sc., Yukiyasu Mariko, M.Sc. and Yuichi Kawata, B.Sc., for their valuable assistance with the design and analysis of the study and preparation of this manuscript. This work was supported by Chugai Pharmaceutical Co., Ltd., Tokyo, Japan.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Hashimoto, J., Garnero, P., van der Heijde, D. et al. A combination of biochemical markers of cartilage and bone turnover, radiographic damage and body mass index to predict the progression of joint destruction in patients with rheumatoid arthritis treated with disease-modifying anti-rheumatic drugs. Mod Rheumatol 19, 273–282 (2009). https://doi.org/10.1007/s10165-009-0170-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10165-009-0170-4