Abstract
Reduced phospholipase A2 (PLA2) activity has been reported in the brain and in blood cells of patients with Alzheimer’s disease (AD). Individuals with mild cognitive impairment (MCI) are at increased risk of developing AD. In the present study, we determined the activity of distinct PLA2 subgroups (iPLA2, sPLA2 and cPLA2) in older adults with MCI as compared to patients with mild dementia due to AD and to cognitively healthy controls. We investigated whether decreased PLA2 activity at baseline is associated with the progression of MCI to AD upon follow-up during a period of 4 years. The activity of PLA2 subgroups was determined in platelets from 169 elderly adults. Progression of MCI to AD was ascertained by standard clinical criteria for AD upon follow-up. At baseline, iPLA2 activity was significantly decreased (p = 0.001) in patients with AD and MCI as compared to controls. Patients with MCI who progressed to AD during follow-up showed significantly lower iPLA2 activity at baseline as compared to patients with MCI who did not progress to AD (p = 0.009). Moreover, subjects from the control group at baseline who progressed to MCI during follow-up had lower sPLA2 and cPLA2 (p = 0.014 and p = 0.009, respectively). Our findings suggest that low platelet iPLA2 activity may be a risk marker for AD in subjects with MCI. Moreover, low sPLA2 and cPLA2 were related to cognitive decline in healthy controls, suggesting a relationship with the very early stages of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Phospholipase A2 (PLA2) comprises a super-family of enzymes that have a major role in membrane phospholipid homeostasis. The activity of PLA2 generates important intracellular signaling molecules and downstream products such as arachidonic acid and choline (Schaloske and Dennis 2006; Burke and Dennis 2009). PLA2 enzymes are classified into three major groups based on their structure, cellular localization, requirement for Ca2+ and substrate specificity. The most studied subtypes are the secreted calcium-dependent PLA2 (sPLA2), the cytosolic calcium-dependent PLA2 (cPLA2) and the intracellular calcium-independent PLA2 (iPLA2) (Dennis 1994). PLA2 subtypes are involved in distinct biological functions and processes. The subtypes iPLA2 and cPLA2 are related to neuronal degeneration and death, whereas, cPLA2 and sPLA2 are related to inflammatory processes (Lambeau and Gelb 2008; Schaeffer et al. 2011a). Thus, changes in each of these subtypes may contribute to distinct aspects of several neuropsychiatric disorders including Alzheimer’s disease (AD).
Membrane composition is under a dynamic homeostatic control. In animal models and post-mortem brain, the inhibition of PLA2 was associated with reduction in membrane fluidity, therefore, affecting its function (Schaeffer et al. 2011b, 2012). Reduced cPLA2 and iPLA2 activity has been associated with mechanisms of neuronal degeneration and memory impairment that may be relevant to the pathogenesis of AD (Sun et al. 2004; Schaeffer et al. 2009a, 2010). In primary cultures of cortical and hippocampal neurons, we found that the inhibition of iPLA2 activity reduced neurite outgrowth and neuronal viability (Forlenza et al. 2007a), and increased the phosphorylation state of Tau (De-Paula et al. 2010). Moreover, we reported that in rodents, iPLA2 inhibition in the brain disrupted short and long-term memory acquisition and retrieval (Schaeffer and Gattaz 2005, 2007). Conversely, conditioned training in adult rats led to PLA2 activation in parallel to enhancement of memory performance (Schaeffer et al. 2009b).
In post-mortem studies, PLA2 activity was significantly reduced in the AD brain, and this reduction correlated with the number of neuritic plaques and neurofibrillary tangles (Gattaz et al. 1995, 1996; Talbot et al. 2000). Accordingly, in patients with mild and moderate AD, we found in an in vivo 31P-spectroscopy study that intracerebral phospholipid breakdown (a surrogate marker of PLA2 activity) was reduced and correlated with worse cognitive performance (Forlenza et al. 2005). In addition, patients with AD and mild cognitive impairment (MCI) showed significantly lower PLA2 activity in platelets as compared to controls (Forlenza et al. 2005; Gattaz et al. 2004). Taken together, these findings suggest that reduced PLA2 activity may contribute to neuropathological and cognitive abnormalities observed in AD. Therefore, in the present study we evaluated, in a longitudinal study with 4 years of follow-up, whether reduced PLA2 activity at baseline is associated with cognitive decline and with an increased risk of AD in patients with MCI. We confirmed previous findings of reduced platelet PLA2 activity in patients with AD and found that reduced enzyme activity at baseline increased the risk for cognitive decline during follow-up.
Methods
Sample
One hundred and sixty-nine elderly adults were included in this study, including 44 with mild or moderate AD (mean age ± standard deviation 74.8 ± 6.5 years), 59 with MCI (71.9 ± 5.8 years) and 66 physically and cognitively healthy controls (67.4 ± 5.4 years). All subjects had a baseline assessment between April 2004 and December 2006. At baseline, both MCI individuals and controls were free of psychoactive drugs. Conversely, AD patients received treatment with cholinesterase inhibitors (rivastigmine, donepezil or galantamine) at therapeutic doses. Current use of any prescription drugs with potential effect on PLA2 (such as corticosteroids and anti-platelet agents) was regarded as exclusion criteria. Therefore, the presence of medical comorbidities requiring such treatments or with relevant platelet involvement (e.g., atherosclerosis-related, metabolic syndrome, hypercortisolism, chronic inflammatory diseases, etc.) and neuroimaging-confirmed relevant subcortical cerebrovascular disease were also ruled out. All participants are subjects of an on-going prospective study on aging and cognition carried out at the memory clinic of the Institute of Psychiatry, University of São Paulo, Brazil (Diniz et al. 2008; Forlenza et al. 2010). Local Ethical Committee approved this study and all subjects signed a written informed consent prior to inclusion in the study.
Clinical assessment
All participants underwent standardized clinical and neuropsychological evaluations at baseline and follow-up evaluations. A detailed description of the cognitive assessment and diagnostic procedures can be found elsewhere (Diniz et al. 2008; Forlenza et al. 2010). For the sake of conciseness, we only show the scores in the Cambridge Cognitive Test (CAMCOG) (Roth et al. 1986; Nunes et al. 2008) and the Mini-Mental State Examination (MMSE) (Folstein et al. 1975).
The diagnosis of AD and MCI as well as the characterization of normal cognitive function in the healthy controls was established by consensus at expert multidisciplinary meetings taking into account all available information about current medical history and neuropsychological test scores. The diagnosis of dementia due to AD was made according to the NINCDS-ADRDA diagnostic criteria (McKhann et al. 1984). Diagnosis of MCI was established according to the Mayo Clinic criteria (Petersen et al. 1999): (1) subjective cognitive complaint, preferably corroborated by an informant; (2) objective cognitive impairment in the neuropsychological assessment; (3) preserved global intellectual function; (4) preserved or minimal impairments in activities of daily living; and (5) not demented.
Changes in cognitive status of MCI and control subjects were determined on annual follow-up reassessments over 4 years for MCI subjects and for controls, taking into account all evidence of objective and clinically relevant cognitive decline over time, endorsed by a comprehensive neuropsychological and functional assessment. The characterization of the conversion of MCI to AD considered that former MCI patients, upon reassessment, met the NINCDS-ADRDA diagnostic criteria; otherwise, the diagnoses of MCI or normal cognition were reinforced. Therefore, we reclassified all participants upon follow-up as: (1) MCI-AD, subjects with MCI who progressed to AD; (2) MCI-MCI, subjects with MCI who retained this diagnosis on follow-up; (3) Con-MCI, control subjects who progressed to MCI on follow-up; (4) Con-Con, control subjects who retained this diagnosis on follow-up. All clinical and diagnostic procedures were done blind to the values of PLA2 activity (see below).
Determination of PLA2 Activity
Platelets were isolated from samples of peripheral blood at the baseline visit and at follow-up. Blood samples were centrifuged at 515×g for 15 min at 20 °C in acid citrate dextrose solution. Aliquots of platelet-rich plasma (PRP) were re-suspended in a wash solution (sodium citrate 30 mM, pH 6.5, potassium chloride 5 mM, calcium chloride 2 mM, magnesium chloride 1 mM, glucose 5 mM, albumin 500 μg/mL, apyrase 50 μg/mL), centrifuged at 1159×g for 8 min at 20 °C, and the pellet was re-suspended in tris-sucrose solution. Platelet aliquots were immediately stored at −70 °C and protein levels were determined by a modified Lowry method prior to experimentation (Bio-Rad, Hercules, California).
PLA2 activity was determined in platelets by a radio-enzymatic assay in triplicate (Talib et al. 2008, 2012). Accordingly, 14C-labeled fatty acid is preferentially cleaved by PLA2 at the sn-2 position of the phosphatidylcholine molecule. To access cPLA2 and sPLA2 activity, the substrate was l-a-1-palmitoyl-2-arachidonyl-phosphatidylcholine labeled with [l-14C] at the sn-2 position (New England Nuclear, Boston Massachusetts). For the determination of iPLA2 activity, the substrate was l-3-phosphatidylcholine, 1-palmitoyl-2- [1-14C]-palmitoyl. Total PLA2 activity was estimated by the sum of the activities of PLA2 subgroups. After a 30 min incubation at 37 °C, the reaction was stopped by adding a solution of HCl–isopropanol (1:11.7, v/v), and the [1-14C]-fatty acid released by the enzymatic reaction was extracted with n-heptane. The radioactivity of [1-14C]-fatty acid was then measured in a liquid scintillation counter (Tri-Carb 2100TR; Packard, Meriden, CT). PLA2 activity was calculated in picomoles per milligram of protein per minute (pmol/mg–protein/min). All determinations were done in the same radio-enzymatic procedure. The inter- and intra-assay variability were 6.0 and 3.3 % (cPLA2), 5.2 and 1.8 % (iPLA2), 6.8 and 3.8 % (sPLA2), respectively.
Statistical analysis
Chi-square tests were carried out to assess the distribution of categorical variables across the diagnostic groups at baseline. Multivariate analysis of variance (MANOVA), with type III sum of squares, was done to assess for mean differences in socio-demographic, cognitive variables and PLA2 activity between diagnostic groups in the baseline assessment. Post-hoc analysis with Tukey test was done to assess for pairwise differences among diagnostic groups.
Time-dependent Cox regression analysis was done to determine the predictors of progression of cognitive decline in the control group and of progression to AD in subjects with MCI.
MANOVAs were performed to assess whether baseline PLA2 activity differed according to the cognitive outcome in the MCI (MCI-AD vs. MCI-MCI) and the control group (Con-MCI vs. Con-Con) in the follow-up analysis.
Statistical tests were performed with the Statistical Package for Social Sciences v. 14 for Windows (SPSS Inc., Chicago, IL) and significance was established as p < 0.05. When indicated, data are given as mean ± standard deviation.
Results
Baseline assessment
As expected, patients with AD were significantly older, less educated and attained lower scores on cognitive screening tests (CAMCOG and MMSE) as compared to subjects with MCI and controls. There was no significant difference in the gender distribution among groups (Table 1).
After controlling for age, educational level and cognitive performance, we found that AD patients had lower platelet iPLA2 activity (F = 7.459, df. = 2, p = 0.001), higher cPLA2 (F = 16.57, df. = 2, p ≤ 0.001) and higher total PLA2 activity (F = 3.584, df. = 2, p = 0.039) as compared to MCI and controls. There was no significant difference in sPLA2 among the three groups (F = 1.194, df. = 2, p = 0.3).
Longitudinal assessment
Follow-up data were available for 50 out of 59 MCI patients (mean follow-up of 51.1 ± 8.2 months) and 58 out of 66 control subjects (mean follow-up of 56.9 ± 19.3 months). The main reasons for discontinuation of follow-up were loss of contact (55 %), unwillingness to perform additional cognitive assessments (35 %), severe and unstable medical condition that precluded cognitive assessment (5 %) and death (5 %).
In the MCI group, during 4 years of follow-up, 18 subjects (36 %) progressed to AD (MCI-AD) and 32 subjects (64 %) remained with the MCI diagnosis (MCI-MCI). In the same period of time, 23 controls (40 %) progressed to MCI (Con-MCI) and 35 controls (60 %) retained normal cognitive function (Con-Con). Patients with MCI who were lost through follow-up had less years of education as compared to those with complete longitudinal data (p = 0.001). No other significant differences were found between these groups regarding age, baseline values of cognitive performance and the activity of distinct PLA2 subtypes (data not shown). Among controls, there were no significant differences between subjects who were lost upon follow-up and those who completed the longitudinal assessment (data not shown).
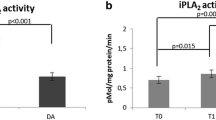
In the MCI group, we found no significant difference in age, years of education and cognitive performance between converter (MCI-AD) and non-converter (MCI-MCI) subjects (Table 2). MCI-AD subjects were more frequently men (p = 0.04) as compared to MCI-MCI subjects (Table 2). After controlling for gender, MCI-AD subjects had a significantly lower iPLA2 activity than MCI-MCI (F = 7.4, df. = 1, p = 0.009). In the Cox regression analysis, decreased iPLA2 activity (p < 0.001) and male gender (p = 0.002) were the best predictors of progression from MCI to AD. There were no significant differences in cPLA2 activity (F = 3.95, df. = 1, p = 0.06) and sPLA2 activity (F = 1.8, df. = 1, p = 0.19) when comparing the MCI-MCI and MCI-AD groups (Fig. 1).
Activities in platelets of a iPLA2, b sPLA2 and c cPLA2 at baseline in four outcome groups after 4-year follow-up: 35 controls that retained normal cognitive function (Con-Con), 23 controls that progressed to MCI (Con-MCI), 32 MCI that remained with the MCI diagnosis (MCI-MCI) and 18 MCI individuals at baseline that progressed to AD (MCI-AD). PLA2 activities in pMol/mg protein/min, mean ± standard error
At baseline, individuals from the control group who converted to MCI (Con-MCI) had significantly lower cPLA2 activity (F = 7.3, df. = 1, p = 0.009), sPLA2 activity (F = 6.37, df. = 1, p = 0.014) and total PLA2 (F = 9.05, df. = 1, p = 0.004) as compared to controls that remained cognitively normal through follow-up (Con-Con). No significant differences in iPLA2 activity were observed between these groups (F = 0.9, df. = 1, p = 0.98) (Fig. 1). There were no significant differences in age, cognitive performance and gender distribution between Con-MCI and Con-Con subjects (Table 2).
Discussion
iPLA2
In the present study, we found in a cross-sectional analysis that patients with AD and MCI showed significantly lower platelet iPLA2 activity than healthy controls. In the longitudinal analysis, lower iPLA2 activity at baseline was associated with higher risk of progression from MCI to AD during 4 years of follow-up. The reduction in iPLA2 activity preceded global cognitive deterioration in subjects with MCI who converted to AD, as at baseline CAMCOG or MMSE scores were not reduced in these subjects as compared to those who did not progress to AD.
Platelets are frequently used as peripheral models for neurons, as they share several membrane receptors and intracellular signal transduction machinery (Bakken et al. 2006; Bianchi et al. 2002). Among the PLA2 enzymes, iPLA2 is the most abundant in neurons (Forlenza et al. 2007b). Accordingly, in a recent study we found a high correlation between total PLA2 activity in platelets and brain tissue from epileptic patients who underwent a lobectomy to treat therapy resistant epilepsy (Talib et al. 2013). Thus, our finding in platelets may reflect a relationship between low iPLA2 activity in the brain and the risk for AD.
Low iPLA2 activity has been associated to many features related to AD physiopathology. In cellular and animal models, inhibition of iPLA2 activity leads to decreased LTP formation and memory impairment, reduced neurite outgrowth in hippocampal neurons, increased β-amyloid production and Tau phosphorylation, and may contribute to the cholinergic and glutamatergic dysfunctions observed in early stages of AD (Schaeffer et al. 2011a, b; Schaeffer and Gattaz 2005, 2007, 2008; Forlenza et al. 2002, 2007a). On the other hand, we found in rodents and in humans that memory training and cognitive stimulation via environmental enrichment increase iPLA2 activity in the brain and in platelets, respectively (Schaeffer et al. 2009b, 2011b).
cPLA2, sPLA2, and total PLA2
Contrasting to the finding of decreased iPLA2 activity, cPLA2 activity was increased in our patients with AD at baseline. It should be noticed that all our AD patients were on treatment with cholinesterase inhibitors (ChE-I), which are reported to increase protein kinase C (PKC) (Nordberg 2006). PKC stimulates the production of arachidonic acid through stimulation of cPLA2 activity (Sun et al. 2004; Farooqui and Horrocks 2004). Thus, in our sample ChE-I treatment may account for increased cPLA2 activity in AD patients. We also found a significant increase in total PLA2 activity in the AD group as compared to MCI, probably due to increased cPLA2 activity. Krzystanek et al. (2007) and Fonteh et al. (2013) also found an increased total PLA2 activity in platelets and in the CSF of AD patients as compared to controls, interpreting that these findings may be associated with the up regulation of inflammatory mechanisms in AD; yet, in this case, all AD patients were not receiving treatment with cholinesterase inhibitors.
The activity of sPLA2 is also related to the stimulation of inflammatory activity via the production and release of arachidonic acid (Heneka et al. 2010). Higher pro-inflammatory activity has been reported in AD and in its prodromal stages (Sun et al. 2010; Diniz et al. 2010; Forlenza et al. 2009). An increase in sPLA2 has been reported in the cerebrospinal fluid (CSF) of AD patients (Chalbot et al. 2009). However, in the present study in platelets, we did not find changes in sPLA2 activity in AD patients or a relationship with the progression from MCI to AD.
In our sample we found lower sPLA2, cPLA2 and total PLA2 in controls at baseline who converted to MCI during the follow-up. sPLA2 and cPLA2 subtypes are related to inflammatory response, neuronal differentiation and growth, and prevention of apoptosis (Smalheiser et al. 1996; Arioka et al. 2005; Ikeno et al. 2005; Masuda et al. 2005; Forlenza et al. 2007b; Buchhave et al. 2010). Therefore, it is conceivable that reduced activity of both sPLA2 and cPLA2 at the pre-clinical stages of AD may render neurons more susceptible to apoptosis and maybe contribute to Aβ formation through changes in the properties of neuronal membranes (Emmerling et al. 1993, 1996; Nitsch et al. 1997; Cho et al. 2006; Masuda et al. 2008; Schaeffer et al. 2011b). This assumption is in line with the early 31P-spectroscopy study of Pettegrew et al. (1988), who hypothesized that the lowering of phospholipid metabolism in the brain may precede the onset of senile plaques at early stages of AD. In our sample, sPLA2 and cPLA2 activities in the MCI-AD group did not differ from controls (Fig. 1), suggesting that with the progression of the disease the enzymes’ activities increase to the level of controls. This has also been observed in the brains of subjects with AD and discussed as an inflammatory response of reactive astrocytes around to Aβ-plaques (Stephenson et al. 1996, 1999; Colangelo et al. 2002; Moses et al. 2006). It is worth noticing that both plaques and soluble oligomers of Aβ may induce the glial cells to produce inflammatory cytokines which, in turn, activate sPLA2 and cPLA2 (but not iPLA2) (Schaeffer et al. 2010).
In summary, our findings suggest that low platelet iPLA2 activity may be a risk marker for AD in subjects with MCI, whereas, low sPLA2 and cPLA2 may be related to the very early stages of the disease. These results stress the importance to study the different subgroups of PLA2, which may present distinct roles in the pathology of AD. It is conceivable that the inclusion of PLA2 activities may enhance the predictive power of other biomarkers, such as CSF Aβ42 and Tau protein, in the early diagnosis of AD.
References
Arioka M, Cheon SH, Ikeno Y, Nakashima S, Kitamoto K (2005) A novel neurotrophic role of secretory phospholipases A2 for cerebellar granule neurons. FEBS Lett 579:2693–2701
Bakken AM, Staeffler A, Jørgensen HA, Holmsen H (2006) Glycerophospholipid molecular species in platelets and brain tissues––are platelets a good model for neurons? Platelets 17(7):484–492
Bianchi M, Moser C, Lazzarini C, Vecchiato E, Crespi F (2002) Forced swimming test and fluoxetine treatment: in vivo evidence that peripheral 5-HT in rat platelet-rich plasma mirrors cerebral extracellular 5-HT levels, whilst 5-HT in isolated platelets mirrors neuronal 5-HT changes. Exp Brain Res 143(2):191–197
Buchhave P, Zetterberg H, Blennow K, Minthon L, Janciauskiene S, Hansson O (2010) Soluble TNF receptors are associated with Aβ metabolism and conversion to dementia in subjects with mild cognitive impairment. Neurobiol Aging 31(11):1877–1884
Burke JE, Dennis EA (2009) Phospholipase A2 structure/function, mechanism, and signaling. J Lipid Res 50 (Suppl S2):37-42
Chalbot S, Zetterberg H, Blennow K, Fladby T, Grundke-Iqbal I, Iqbal K (2009) Cerebrospinal fluid secretory Ca2+-dependent phospholipase A2 activity is increased in Alzheimer disease. Clin Chem 55(12):2171–2179
Cho HW, Kim JH, Choi S, Kim HJ (2006) Phospholipase A2 is involved in muscarinic receptor-mediated sAPPα release independently of cyclooxygenase or lypoxygenase activity in SHSY5Y cells. Neurosci Lett 397:214–218
Colangelo V, Schurr J, Ball MJ, Pelaez RP, Bazan NG, Lukiw WJ (2002) Gene expression profiling of 12633 genes in Alzheimer hippocampal CA1: transcription and neurotrophic factor down regulation and up-regulation of apoptotic and pro-inflammatory signaling. J Neurosci Res 70:462–473
Dennis EA (1994) Diversity of group types, regulation, and function of phospholipase A2. J Biol Chem 269(18):13057–13060
De-Paula VJ, Schaeffer EL, Talib LL, Gattaz WF, Forlenza OV (2010) Inhibition of phospholipase A2 increases tau phosphorylation at Ser214 in embryonic rat hippocampal neurons. Prostaglandins Leukot Essent Fatty Acids 82:57–60
Diniz BS, Nunes PV, Yassuda MS, Pereira FS, Flaks MK, Viola LF, Radanovic M, Abreu ID, Borelli DT, Gattaz WF, Forlenza OV (2008) Mild cognitive impairment: cognitive screening or neuropsychological assessment? Rev Bras Psiquiatr 30:316–321
Diniz BS, Teixeira AL, Ojopi EB, Talib LL, Mendonça VA, Gattaz WF, Forlenza OV (2010) Higher serum sTNFR1 level predicts conversion from mild cognitive impairment to Alzheimer’s disease. J Alzheimers Dis 22(4):1305–1311
Emmerling MR, Moore CJ, Doyle PD, Carroll RT, Davis RE (1993) Phospholipase A2 activation influences the processing and secretion of the amyloid precursor protein. Biochem Biophys Res Commun 197:292–297
Emmerling MR, Dudley DT, Dyer RD, Carroll RT, Doyle PD, Davis RE (1996) The role of arachidonic acid in the secretion of the amyloid precursor protein (APP). Ann N Y Acad Sci 777:310–315
Farooqui AA, Horrocks LA (2004) Brain phospholipases A2: a perspective on the history. Prostaglandins, Leucotrienes and Essential Fatty acids 71:161–169
Folstein MF, Folstein SE, Mchugh PR (1975) Mini-Mental State: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Fonteh AN, Chiang J, Cipolla M, Hale J, Diallo F, Chirino A, Arakaki X, Harrington MG (2013) Alterations in cerebrospinal fluid glycerophospholipids and phospholipase A2 activity in Alzheimer’s disease. J Lipid Res. Jul 18 [Epub ahead of print]
Forlenza OV, Schaeffer EL, Gattaz WF (2002) Phospholipase A2 activity in rat embryonic brain and in primary cultures of cortical neurons. J Neural Transm 109(5–6):623–631
Forlenza OV, Wacker P, Nunes PV, Yacubian J, Castro CC, Otaduy MC, Gattaz WF (2005) Reduced phospholipid breakdown in Alzheimer’s brains: a 31P spectroscopy study. Psychopharmacology 180(2):359–365
Forlenza OV, Mendes CT, Marie SK, Gattaz WF (2007a) Inhibition of phospholipase A2 reduces neurite outgrowth and neuronal viability. Prostaglandins Leukot Essent Fatty Acids 76:47–55
Forlenza OV, Schaeffer EL, Gattaz WF (2007b) The role of phospholipase A2 in neuronal homeostasis and memory formation: implications for the pathogenesis of Alzheimer’s disease. J Neural Transm 114(2):231–238
Forlenza OV, Diniz BS, Talib LL, Mendonça VA, Ojopi EB, Gattaz WF, Teixeira AL (2009) Increased serum IL-1beta level in Alzheimer’s disease and mild cognitive impairment. Dement Geriatr Cogn Disord 28(6):507–512
Forlenza OV, Diniz BS, Talib LL, Radanovic M, Yassuda MS, Ojopi EB, Gattaz WF (2010) Clinical and biological predictors of Alzheimer’s disease in patients with amnestic mild cognitive impairment. Rev Bras Psiquiatr 32(3):216–222
Gattaz WF, Maras A, Cairns NJ, Levy R, Förstl H (1995) Decreased phospholipase A2 activity in Alzheimer brains. Biol Psychiatry 37:13–17
Gattaz WF, Cairns NJ, Levy R, Förstl H, Braus DF, Maras A (1996) Decreased phospholipase A2 activity in the brain and in platelets of patients with Alzheimer’s disease. Eur Arch Psychiatry Clin Neurosci 246(3):129–131
Gattaz WF, Forlenza OV, Talib LL, Barbosa NR, Bottino CM (2004) Platelet phospholipase A2 activity in Alzheimer’s disease and mild cognitive impairment. Journal of Neural Transmission 111:591–601
Heneka MT, O’Banion MK, Terwel D, Kummer MP (2010) Neuroinflammatory processes in Alzheimer’s disease. J. Neural Transm 117(8):919–947
Ikeno Y, Konno N, Cheon SH, Bolchi A, Ottonello S, Kitamoto K et al (2005) Secretory phospholipases A2 induce neurite outgrowth in PC12 cells through lysophosphatidylcholine generation and activation of G2A receptor. J Biol Chem 280:28044–28052
Krzystanek E, Krzystanek M, Opala G, Trzeciak HI, Siuda J, Małecki A (2007) Platelet phospholipase A2 activity in patients with Alzheimer’s disease, vascular dementia and ischemic stroke. J Neural Transm 114(8):1033–1039
Lambeau G, Gelb MH (2008) Biochemistry and physiology of mammalian secreted phospholipases A2. Annu Rev Biochem 77:495–520
Masuda S, Murakami M, Takanezawa Y, Aoki J, Arai H, Ishikawa Y et al (2005) Neuronal expression and neuritogenic action of group X secreted phospholipase A2. J Biol Chem 80:23203–23214
Masuda S, Yamamoto K, Hirabayashi T, Ishikawa Y, Ishii T, Kudo I et al (2008) Human group III secreted phospholipase A2 promotes neuronal outgrowth and survival. Biochem J 409:429–438
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of department of health and human Services task force on Alzheimer’s disease. Neurology 34(7):939–944
Moses GS, Jensen MD, Lue LF, Walker DG, Sun AY, Simonyi A et al (2006) Secretory PLA2-IIA: a new inflammatory factor for Alzheimer’s disease. J Neuroinflammation 3:28
Nitsch RM, Deng A, Wurtman RJ, Growdon JH (1997) Metabotropic glutamate receptor subtype mGluR1α stimulates the secretion of the amyloid β-protein precursor ectodomain. J Neurochem 69:704–712
Nordberg A (2006) Mechanisms behind the neuroprotective actions of cholinesterase inhibitors in Alzheimer disease. Alzheimer Dis Assoc Disord 20(2Suppl 1):S12–8. Review
Nunes PV, Diniz BS, Radanovic M, Abreu ID, Borelli DT, Yassuda MS, Forlenza OV (2008) CAMCOG as a screening tool for diagnosis of mild cognitive impairment and dementia in a Brazilian clinical sample of moderate to high education. Int J Geriatr Psychiatry 23:1127–1133
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E (1999) Mild Cognitive Impairment: clinical characterization and outcome. Arch Neurol 56:303–308
Pettegrew JW, Moossy J, Withers G, McKeag D, Panchalingam K (1988) 31P nuclear magnetic resonance study of the brain in Alzheimer’s disease. J Neuropathol Exp Neurol 47:235–248
Roth M, Tym E, Mountjoy CQ, Huppert FA, Hendrie H, Verma S, Goddard R (1986) CAMDEX: a standardized Instrument for the diagnosis of mental disorders in the elderly with special reference to early detection of dementia. Br J Psychiatry 149:698–709
Schaeffer EL, Gattaz WF (2005) Inhibition of calcium-independent phospholipase A2 activity in rat hippocampus impairs acquisition of short- and long-term memory. Psychopharmacology 181:392–400
Schaeffer EL, Gattaz WF (2007) Requirement of hippocampal phospholipase A2 activity for long-term memory retrieval in rats. J Neural Transm 114:379–385
Schaeffer EL, Gattaz WF (2008) Cholinergic and glutamatergic alterations beginning at the early stages of Alzheimer disease: participation of the phospholipase A2 enzyme. Psychopharmacology 198(1):1–27
Schaeffer EL, Forlenza OV, Gattaz WF (2009a) Phospholipase A2 activation as a therapeutic approach for cognitive enhancement in early-stage Alzheimer disease. Psychopharmacology 202(1–3):37–51
Schaeffer EL, Zorron PuL, Gagliotti DA, Gattaz WF (2009b) Conditioning training and retrieval increase phospholipase A(2) activity in the cerebral cortex of rats. J Neural Transm 116:41–50
Schaeffer EL, da Silva ER, Novaes Bde A, Skaf HD, Gattaz WF (2010) Differential roles of phospholipases A2 in neuronal death and neurogenesis: implications for Alzheimer disease. Prog Neuropsychopharmacol Biol Psychiatry 34(8):1381–1389
Schaeffer EL, De-Paula VJ, da Silva ER, de A Novaes B, Skaf HD, Forlenza OV, Gattaz WF (2011a) Inhibition of phospholipase A(2) in rat brain decreases the levels of total Tau protein. J Neural Transm 118(9):1273–1279
Schaeffer EL, Skaf HD, Novaes Bde A, da Silva ER, Martins BA, Joaquim HD, Gattaz WF (2011b) Inhibition of phospholipase A2 in rat brain modifies different membrane fluidity parameters in opposite ways. Prog Neuropsychopharmacol Biol Psychiatry 35(7):1612–1617
Schaeffer EL, Gattaz WF, Eckert GP (2012) Alterations of brain membranes in schizophrenia: impact of phospholipase A(2). Curr Top Med Chem 12(21):2314–2323
Schaloske RH, Dennis EA (2006) The phospholipase A2 superfamily and its group numbering system. Biochim Biophys Acta 1761(11):1246–1259
Smalheiser NR, Dissanayake S, Kapil A (1996) Rapid regulation of neurite outgrowth and retraction by phospholipase A2-derived arachidonic acid and its metabolites. Brain Res 721:39–48
Stephenson DT, Lemere CA, Selkoe DJ, Clemens JA (1996) Cytosolic phospholipase A2 (cPLA2) immunoreactivity is elevated in Alzheimer’s disease brain. Neurobiol Dis 3:51–63
Stephenson D, Rash K, Smalstig B, Roberts E, Johnstone E, Sharp J et al (1999) Cytosolic phospholipase A2 is induced in reactive glia following different forms of neurodegeneration. Glia. 27:110–128
Sun GY, Xu J, Jensen MD, Simonyi A (2004) Phospholipase A2 in the central nervous system: implications for neurodegenerative diseases. J Lipid Res 45(2):205–213
Sun GY, Shelat PB, Jensen MB, He Y, Sun AY, Simonyi A (2010) Phospholipases A2 and inflammatory responses in the central nervous system. Neuromolecular Med 12(2):133–148
Talbot K, Young RA, Jolly-Tornetta C, Lee VM, Trojanowski JQ, Wolf BA (2000) A frontal variant of Alzheimer’s disease exhibits decreased calcium-independent phospholipase A2 activity in the prefrontal cortex. Neurochem Int 37(1):17–31
Talib LL, Yassuda MS, Diniz BS, Forlenza OV, Gattaz WF (2008) Cognitive training increases platelet PLA2 activity in healthy elderly subjects. Prostaglandins Leukot Essent Fatty Acids 78:265–269
Talib LL, Diniz BS, Zainaghi IA, Forlenza OV, Gattaz WF (2012) A radioenzymatic assay to identify three groups of phospholipase A(2) in platelets. Prostaglandins Leukot Essent Fatty Acids 86(4–5):149–153
Talib LL, Valente KD, Vincentiis S, Gattaz WF. (2013) Correlation between platelet and brain PLA(2) activity. Prostaglandins Leukot Essent Fatty Acids. doi:10.1016/j.plefa.2013.07.002. [Epub ahead of print]
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gattaz, W.F., Talib, L.L., Schaeffer, E.L. et al. Low platelet iPLA2 activity predicts conversion from mild cognitive impairment to Alzheimer’s disease: a 4-year follow-up study. J Neural Transm 121, 193–200 (2014). https://doi.org/10.1007/s00702-013-1088-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-013-1088-8