Abstract
Acute and chronic anxiety represents the core symptoms in anxiety disorders. Anxiolytic pharmacological treatment mainly consists in administration of benzodiazepines and antidepressants. Whereas benzodiazepines show little, antidepressants show a relative large interindividual variability in terms of drug response where about one-third of patients do not respond at all. With no meaningful predictors available, there is increasing hope that genetics can help in adding important pieces of information in order to avoid lengthy drug trials and/or to avoid side effects. However, only few studies have been conducted with antidepressants and benzodiazepines in anxiety disorders. Similar to studies in major depression, some significant findings indicate that presence of the long allele of the serotonin transporter (5-HTT) gene is associated with favorable response. Other significant findings pointed to the serotonin 2A (5-HT2A) receptor and to the tryptophan hydroxylase (TPH1) genes. To date, the most promising strategy in clinical practice appears to incorporate testing of functional CYP450 gene variants (CYP1A2, CYP3A4, CYPD26 and CYP2C19) to avoid over- or under-dosing in poor or rapid metabolizers, respectively. As research progresses, it is likely that further gene variants will be detected that in conjunction with clinical variables will lead to algorithms allowing for individualized anxiolytic drug treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute (e.g., panic attacks) and chronic anxiety represents the core symptoms within the heterogeneous group of anxiety disorders. Clinically most relevant forms include panic disorder (PD), general anxiety disorder (GAD), posttraumatic stress disorder (PTSD) and obsessive compulsive disorder (OCD). Despite this variety of disorders, the main pharmacological treatment of the core symptom anxiety typically includes benzodiazepines (as prototype of anxiolytic drugs) and antidepressants, in particular the newer selective serotonin reuptake inhibitors (SSRIs). Other drugs with anxiolytic effects include the serotonin (5-HT)-1A agonist buspirone and atypical antipsychotics. However, these latter drugs are not considered medications of first-choice, whereas SSRIs have become the pharmacological first-line treatment in anxiety disorders (Denys and De Geus 2005). Benzodiazepines are effective and mostly well tolerated for acute symptom relief but become problematic in long-term treatment due to the well known potential of abuse, tolerance, dependence and withdrawal symptoms. Antidepressants, on the other hand, may have 1–3 weeks elapse before the anxiolytic activity becomes evident but, if tolerated and efficacious, represent the cornerstone of long-term treatment in anxiety disorders. Benzodiazepines are composed by a variety of different compounds which all act as GABA agonists (Stein and Stein 2008). Benzodiazepines show relatively little variability in response (with typically significant anxiolytic effects in most individuals), but benzodiazepines vary substantially in their metabolic pathways and in their half-lives. In contrast, antidepressants can vary substantially in their mechanism of action and generally do show a higher variability in drug response with approximately one-third of patients who do not respond at all on a given antidepressant (Holsboer 2008).
In general terms, the variability in drug response and side effects is likely to depend to a large extent on genetic factors (Roses 2000). One formal genetic study analyzing benzodiazepines effects on a small numbers of healthy twins (6 monozygotic and 4 dizygotic twin pairs) reported that genetic factors seem to contribute to effects of diazepam on affectivity (Alda et al. 1987). There is only limited data available on formal genetic studies focusing on drug response in anxiety disorders. However, anxiety disorders overlap with major depression and increased anxiety is an often reported symptom in depressed patients (i.e., anxious depression). Since in major depression, the variability of response to antidepressants has repeatedly been reported to depend on genetic factors (Serretti et al. 2005), it is plausible that drug response in anxiety disorders will be modulated by genetic factors as well. Furthermore, as will be explained in more details below, the metabolism of both benzodiazepines and antidepressants is modulated by CYP450 enzymes who are showing significant activity differences based on genetic polymorphisms. Altogether, there is reasonable evidence to assume that genetic factors are involved in anxiolytic drug response.
Genetic approaches to the drug response can either be classified as hypothesis-free (generally using genome-wide approaches and termed pharmacogenomics) or involve hypothesis-driven approaches (generally termed pharmacogenetic approaches). Pharmacogenetics is based on scrutinizing single genes, or genes belonging to a known functional system or pathway. The pharmacokinetics of the drug influence biotransformation/metabolism of the drug, transportation of the active substances or metabolites to the target sites, where all have the potential to significantly modulate response and side effects. It has been noted that the effect of modulation in pharmacokinetically relevant genes on the levels of drug in blood plasma is larger and easier to detect than psychopathologically defined outcomes of modulation in genes involved in the pharmacodynamics, as these are of minor magnitude (Maier and Zobel 2008). Further along this line, pharmacodynamics describe genes that code for particular target organs involved in drug action and may modulate response to treatment and also to some side effects. Due to the importance of pharmacokinetics and the well-known liver enzyme pathways (i.e., cytochrome P450 or CYP450 genes) involved in the degradation of anxiolytic drugs, this review will particularly emphasize on the potential of genetic analyses in these genes to predict response and side effects. Furthermore, this review will also highlight most important findings in pharmacodynamics.
Pharmacokinetics of benzodiazepines and antidepressants
The plasma level achieved by a drug is influenced at several levels, starting from absorption, distribution up to the elimination of a drug. The bioavailability of the drug is determined by the first-pass or pre-systemic metabolism at either the gut wall or in the liver. The plasma level of drug may further be influenced by several sociodemographic factors (e.g., age, sex and ethnicity) and environmental factors including inhibition or induction by other compounds (e.g., smoking, co-medication or dietary habits). Besides these, genetic factors also play an important role in determining the therapeutic level achieved by a drug in other oxidative or conjugating systems. Drug metabolism can be divided into Phase I (drug oxidation) and Phase II metabolism (drug conjugation allowing for subsequent excretion). Phase I metabolizers include cytochrome P450s (CYP450), flavin containing monooxigenases, reductases, esterases and alcohol dehydrogenases. The Phase II drug metabolizing enzymes include N-acetyltransferase (NAT), thiopurine methyltransferase (TPMT), glutathione transferase and UDP-glucurunosyltransferase (UGT). Despite these various factors and enzymes influencing plasma levels, the CYP450 enzymes play a key role, as about 80% of all Phase I drug metabolism (including virtually all anxiolytic and antidepressants drugs) are catalyzed by CYP450 enzymes (Eichelbaum et al. 2006; Ingelman-Sundberg et al. 2007).
The CYP450 are a highly diverse group of heme-containing monooxygenases catalyzing a variety of reactions including epoxidation, N-dealkylation, O-dealkylation, S-oxidation and hydroxylation. Genetic polymorphisms determining the functional activity of the CYP450s are well documented. The presence of specific polymorphisms can lead to (1) poor metabolizer (PM) phenotype, characterized by complete absence of activity due to both alleles being non-functional; (2) intermediate metabolizer (IM), one allele is non-functional or both the alleles are partially defective; (3) extensive metabolizer (EM) with both the alleles functional; and (4) ultrarapid metabolizer (UM) exhibiting the highest activity due to more than two functional genes (Ingelman-Sundberg et al. 2007). PM status, if undetected, may cause severe side effects in individuals treated with standard doses (Phillips et al. 2001). On the other hand, rapid metabolizers may not respond to normal doses and thus may falsely be classified as not complying with drug treatment. The human CYP450 family of genes consists of around 57 members of which CYP family 1, family 2 and family 3 (CYP1, CYP2 and CYP3, respectively) are expressed mainly in the smooth endoplasmic reticulum of hepatocytes, and catalyze majority of the biotransformations of drugs and xenobiotics (Ingelman-Sundberg et al. 2007). Of these, CYP3A4, CYP2D6, CYP1A2, CYP2C9 and CYP2C19 metabolize the majority of the benzodiazepines and antidepressants.
CYP1, subfamily A, polypeptide 2 (CYP1A2)
CYP1A2 is involved in the metabolism of antidepressants such as amitriptyline, clomipramine, duloxetine (Table 1). Considerable interindividual variability in the expression (15-fold) and activity (30- to 60-fold) of CYP1A2 has been observed. The gene is located on chr15q24.1 and more than 35 different allelic variants have been reported in this gene of ~7.75 kb (http://www.cypalleles.ki.se). However, only two SNPs, namely, CYP1A2*1C (−3,860 G>A) and CYP1A2*1F (intron 1, C>A) have been reported to be of functional relevance (Nakajima et al. 1999); the former leading to decreased and the latter increased inducibility among smokers. Recently, decreased serum levels of duloxetine have been reported in smokers (Fric et al. 2008); however, associations between genotypes and serum levels have not been investigated.
CYP3, subfamily A, polypeptide 4 (CYP3A4)
CYP3A4 is a 27.2 kb gene located on chr7q21-q22.1 along with the other members of the CYP3A sub-family (CYP3A4, CYP3A5, CYP3A7 and CYP3A43). CYP3A4 is involved in the metabolism of most benzodiazepines and some antidepressants such as buspirone, mirtazapine and venlafaxine (Table 1). Of note, CYP3A4 can be inhibited and/or induced by a variety of substances and females may have a higher CYP3A4 activity (Wolbold et al. 2003). The CYP3A4 gene harbors more than 40 rare allelic variations. The CYP3A4*1B (−392 A>G; rs2740574) promoter polymorphism is the most commonly investigated polymorphism. It varies in frequency from 2 to 4% in Europeans, 60 to 75% in the African population but is absent in Chinese and Japanese populations. The functional relevance of this variant remains controversial (Yamazaki and Shimada 1996; Rodriguez-Antona et al. 2005), but so far, genetic variations in the CYP3A4 gene have not been analyzed with respect to anxiolytic drug response.
CYP3, subfamily A, polypeptide 5 (CYP3A5)
CYP3A5, like CYP3A4 is inducible and accounts for 30–50% of the total CYP3A protein content. The gene is 31.8 kb and has ~23 polymorphisms, of these CYP3A5*3, a 6,986 A>G substitution in intron 3 (rs776746) causes a splicing defect leading to primarily non-functional protein. This polymorphism is more common in Europeans than the wild type, functional CYP3A5*1. The frequency of CYP3A*3 varies from 85–98% in Europeans to 55–64% in African American individuals, thus the frequency of functional allele is considerably lower in Europeans than African Americans. The other defective alleles CYP3A5*6, a splicing defect and CYP3A5*7, a frame-shift mutation, occur at a frequency of 17% and 8% respectively in African American individuals. These alleles are absent in European and Asian individuals (Hustert et al. 2001; Lee et al. 2003). The in vitro metabolism of midazolam, a substrate of CYP3A5, is affected by the presence of these polymorphisms; however, no in vivo effect has been observed. On the other hand, metabolism of alprazolam may be impaired, as higher plasma levels are observed in subjects homozygous for the CYP3A5*3 polymorphism, whereas heterozygous subjects (CYP3A5*1/*3) showed intermediate plasma levels. The pharmacodynamic response (measured by the change in Digit Symbol Substitution Test score) was higher in CYP3A5*3 homozygotes but was statistically insignificant. Thus, an effect of genotype on plasma levels of alprazolam has been reported but no association with clinical measures has been observed (Park et al. 2006; Kharasch et al. 2007).
CYP2, subfamily D, polypeptide 6 (CYP2D6)
CYP2D6 is one of the most polymorphic CYP450 gene located on chr22q13.1 with a size of ~4.4 kb, with more than 110 genetic known variations (Zanger et al. 2008) and most of the interindividual variations has been attributed to a genetic component (De Leon 2007). CYP2D6 is involved in the metabolism of 25% of all the prescribed drugs and 80% of antidepressants and antipsychotics (Table 1). Depending upon the activity status of the enzyme, an individual can be classified as ultra rapid (UM), extensive (EM), intermediate (IM) and poor (PM) metabolizers. The EM is the wild type CYP2D6*1, the IM phenotype is primarily due to the presence of either of CYP2D6*9 (lysine deletion), *10 (mis-sense), *17 (mis-sense) and *41 (splicing defect) alleles. The CYP2D6*41 variant is more common in Europeans (10–15%), CYP2D6*17 in Africans (30%) and CYP2D6*10 among Asians (50%) (Zanger et al. 2008). Major determinants of the PM phenotype are CYP2D6*4 (splicing defect) and *5 (gene deletion). The CYP2D6*4 is one of the most frequent inactivating polymorphism among Europeans occurring at a frequency varying from 10 to 25% and accounting for 70–90% of PM status. Finally, the UM phenotype is due to CYP2D6 gene duplication where interethnic variation has also been observed with up to 13 duplicated copies in some populations. The frequency of duplication varies from 1 to 5% in Europeans, 21% in Saudi Arabia; and 29% in Ethiopia and Algeria (Mclellan et al. 1997; Akillu et al. 1996). Besides the duplication of the wildtype gene CYP2D6*1, duplication of the various defective and partially active alleles has also been observed.
The usefulness of predictive testing for the UM, IM and PM phenotype has consistently been demonstrated (Gaedigk et al. 2008; Kirchheiner 2008). For example, the UM phenotype has been associated with increased clearance of paroxetine and therefore UM patients would require higher doses of the drug (Kirchheiner et al. 2004). Similarly, Kawanishi et al. (2004) observed association between the occurrence of CYP2D6 duplications and lack of response to antidepressants evidenced by higher scores of the Hamilton Depression Rating Scale. Furthermore, Rau et al. (2004) reported increased occurrence of the UM’s among non-responders and PMs in patients with adverse events receiving antidepressants. It has been shown that variation in plasma levels of these drugs (e.g. fluvoxamine and paroxetine) may lead to different treatment response in patients with PD (Sandmann et al. 1998, Watanabe et al. 2007). However, no correlation has been shown between CYP2D6 genotypes and clinical response in anxious patients using antidepressants. In summary, testing of CYP2D6 polymorphisms may potentially become a valid method to predict dosing and/or outcome in anxiolytic drugs.
CYP2, subfamily C, polypeptide 19 (CYP2C19)
CYP2C19 is another important gene on chromosome 10q24.1-q24.3 involved in the metabolism of antidepressants. The gene is ~90.2 kb in size and about 30 allelic variants are known for CYP2C19, including CYP2C19*2 (splicing defect, exon5), CYP2C19*3 (Trp212Ter, exon4) and CYP2C*17 (−806 C > T, promoter region). CYP2C19*2 and 3 are associated with the PM phenotype whereas CYP2C19*17 leads to increased activity due to an increased transcription. The frequency of CYP2C19*2 allele varies from 15% in Europeans up to ~28% in the Japanese population and accounts for ~70–80% PM individuals in both populations. CYP2C19*3 is only present in the oriental population with a frequency from 3 to 4% and accounts for 25% PMs in this population. The frequency of CYP2C19*17 varies from 20 to 25% in Europeans and Africans, but is only present in ~2% in the Chinese population. The usefulness of CYP2C19 genotyping to predict antidepressant side effects (e.g. amitriptyline) and response (e.g. escitalopram) has consistently been reported (Steimer et al. 2005; Ingelman-Sundberg et al. 2007; Rudberg et al. 2008).
CYP2C19 also metabolizes several benzodiazepines for e.g. clobazam, diazepam and others (Table 1). The presence of CYP2C19*2 polymorphism has been shown to lead to a higher concentration of desmethylclobazam/clobazam concentration ratio in epileptic patients (Giraud et al. 2004; Kosaki et al. 2004, Parmeggiani et al. 2004). Similarly, Seo et al. (2008) observed greater response in individuals who were poor metablizers (PM). Although the incidence of adverse events was higher in PM individuals, no association either with adverse events or with tolerance was observed. Thus genetic polymorphism in CYP2C19 may be related to interindividual variation of plasma levels of clobazam and possibly to the occurrence of side effects. Similar increased plasma levels of diazepam etizolam and quazepam have also been reported in the CYP2C19 PM individuals (Bertilsson et al.1989; Qin et al. 1999; Fukasawa et al. 2005; Fukasawa et al. 2004).
In summary, variants of the CYP2D6 and CYP2C19 genes have been reported to be associated with dosage, side effects and response of some of the drugs effective in anxiety disorders suggesting its potential use for personalized medicine (Fukasawa et al. 2007). There is a plausible potential for the CYP1A2 and CYP3A4 genes to be included in further studies.
Pharmacogenetics of pharmacodynamic aspects
Serotonin transporter (5-HTT) gene
The neurotransmitter serotonin (5-HT) has been implicated in a wide range of psychiatric conditions including depression, anxiety disorders, obsessive–compulsive disorder, psychosis, eating disorders, and substance abuse/dependence (Veenstra-VanderWeele et al. 2000). The serotonin transporter (5-HTT) enzyme is a key modulator of serotonergic neurotransmission in the synaptic cleft and the main target of all SSRIs. Thus, any genetic variant affecting 5-HTT expression levels may intuitively be associated with response to antidepressants. A cornerstone in the field of psychiatric genetics has been the detection of a functional insertion/deletion promoter polymorphism (5-HTTLPR) where the short allele has been associated with lower transcriptional activity (Lesch et al. 1993, 1996). Numerous studies and meta-analyses have since consistently reported a poorer response in s-allele carriers treated with SSRIs for major depression (Serretti et al. 2005).
Stein et al. (2006) had initially demonstrated the presence of a genetic component in treatment response in social anxiety disorder patients and showed that the short variant of the 5-HTTLPR has been associated with poorer response. This was reflected by persistent higher scores in social anxiety and social phobia scales (Table 2). Perna et al. (2005) provided the first experimental evidence that allelic variation of 5-HTTLPR influences the response to SSRIs at equal bioavailability in PD, supporting the hypothesis that the availability of 5-HT transporter is important for a clinically useful effect. In their study, patients carrying one or two long alleles showed better response. In further sub-analyses, they observed that the effect of the 5-HTTLPR was driven specifically by female patients. The authors further pointed out, that their findings were neither explained by differences in clinical and/or demographical features of the sample, nor to paroxetine plasma levels (Perna et al. 2005). Kim et al. (2006) have examined PD patients and, however, detected no significant association with the 5-HTTLPR polymorphism and clinical response.
Several studies have investigated the role of the 5-HTTLPR in the treatment response of OCD patients: Billett et al. (1997) retrospectively analyzed patients after a 10-week trial and found no association with the 5-HTTLPR and OCD. In another study, McDougle et al. (1998) found a non-significant trend for an association of the L-allele with poorer response to several antidepressants including clomipramine, fluvoxamine, fluoxetine, sertraline and paroxetine. Di Bella et al. (2002) and Zhang et al. (2004) failed to find a relation among response and the 5-HTTLPR. In contrast, Denys et al. (2007) reported that the heterozygous form of the 5-HTTLPR genotype (short/long) has been associated with favorable response to venlafaxine. Despite some inconsistent findings, the highest or most consistent level of evidence for an association between genotype and clinical effects in anxiolytic drugs has thus far perhaps been given for this serotonin transporter gene polymorphism.
Serotonin receptor 1A (5-HT1A) gene
The 5-HT1A receptor is a G protein-linked receptor that acts primarily via inhibition of adenylyl cyclase and is located both pre- and post-synaptically. Most of the interest in this receptor centers on its possible involvement in the pathogenesis and treatment of anxiety and depression. 5-HT1A receptor partial agonists such as buspirone have anxiolytic and antidepressant properties (De Vry 1995). The 5-HT1A receptor gene knockout mice exhibit increased anxiety as indicated by decreased exploratory activity in multiple paradigms (Heisler et al. 1998; Parks et al. 1998; Ramboz et al. 1998). Interestingly, these mice respond poorly to benzodiazepines, and these mice have decreased GABAA receptor binding within the limbic system (Sibille et al. 2000). This ties together the serotonergic and GABAergic pathways, the two systems most frequently addressed by current anxiolytic therapies. The efficacy of buspirone and other partial agonists in the treatment of anxiety suggests that investigations of HTR1A polymorphisms are warranted. The resistance of the 5-HT1A receptor gene knockout mouse to the effects of benzodiazepines should serve to further stimulate research on HTR1A variants in anxiety, such as the functional -1019C/G promoter polymorphism. However, up to date, no pharmacogenetic study has been reported with buspirone. Such studies need to be addressed in the future and 5-HT1A receptor gene should be considered a prime candidate gene in pharmacogenetics studies of anxiolytic drugs.
Serotonin receptors 1B (5-HT1B) and 2A (5-HT2A) genes
Genetic variants in receptors that might be involved in the therapeutic efficacy of SSRIs, such as the terminal 5-HT1B autoreceptor and the postsynaptic 5-HT2A receptor, have also been evaluated. Tot et al. (2003) firstly evaluated the 5-HT2A A1438G and T102C variants and treatment response in OCD patients but failed to detect significant associations among 5-HT2A polymorphisms and treatment response. Zhang et al. (2004) found a significant association between the A1438G polymorphism of the5-HT2A gene and response in OCD patients treated with serotonin reuptake inhibitors. Consistent with that finding, Denys et al. (2007) have shown that patients carrying the 1438 G allele and G/G genotype in the 5-HT2A gene have been associated with paroxetine response in OCD patients.
Tryptophan hydroxylase (TPH), catecol-O-methyltransferase (COMT) and monoamino oxidase (MAO) genes
TPH is a rate-limiting enzyme in serotonin synthesis. Two isoforms have been detected, TPH1 and TPH2 (Walther and Bader 2003). Kim et al. (2006) reported no significant association of CGI-I scores and the A218C variant of the TPH1gene in patients affected with PD. No studies with the TPH2 gene with response to anxiolytic drugs have been performed.
COMT is an enzyme inactivating catecholamines, including norepinephrine and dopamine that have been examined in genetic association studies conducted with OCD and PD (Karayiorgou et al. 1999; Domschke et al. 2004; Rothe et al. 2006). MAOA and MAOB are enzymes that degrade a variety of biogenic amines such as 5-HT, dopamine and norepinephrine. MAOA gene has been reported in genetic studies of OCD and PD (Deckert et al. 1999; Karayiorgou et al. 1999; Sand et al. 2000; Hamilton et al. 2002). Regarding antidepressants response in OCD patients, Zhang et al. (2004) reported no association neither with COMT nor with MAOA gene variants.
Dopamine receptor 2 (DRD2) and 4 (DRD4)
Although none of the current drug treatments for anxiety disorders appears to target dopamine receptors, the dopaminergic system represents another important neurotransmitter system. However, the mechanism of action for anxiolytic drugs such as antidepressants have not yet been understood completely, and study findings related to MAOA, MAOB and COMT which modulate dopamine concentrations may serve as indirect evidence that the dopaminergic system may be involved in anxiolysis. Moreover, antidepressants such as buproprion exert their therapeutic effect by increasing dopaminergic neurotransmission. Lawford et al. (2003) have examined male Vietnam combat veterans patients with a diagnosis of PTSD and found no significant association among TaqI A DRD2 genotypes and treatment response (Lawford et al. 2003). Zhang et al. (2004) have reported no significant association among DRD2 and DRD4 gene variants in OCD patients and response to antidepressants.
Other genes
Domschke et al. (2008a, b) have presented that the cannabinoid receptor CNR1 rs1049353 G allele conferred an increased risk for poor response to antidepressant treatment particularly in the subgroup of patients with high anxiety which was particularly present in the female subgroup of patients. In another study, Domschke et al. (2009) have shown that the TT variant of the brain-derived neurotrophic factor (BDNF) rs7124442 polymorphism was associated with poorer treatment outcome over 6 weeks in 81 German anxious depression patients.
Discussion
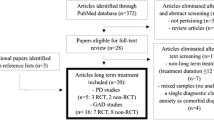
Benzodiazepines and SSRIs play a major role in the acute and chronic pharmacologic management in anxiety disorders. Benzodiazepines are effective in most individuals (i.e. with little interindividual variability in response) but are only recommended for acute symptom relief. However, the success of long-term antidepressant treatment is limited due to the fact that a large portion of patients do not respond sufficiently (De Mooij-van Malsen et al. 2008). Genetic factors affecting the metabolism and mechanism of action of both classes of drugs are hypothesized to be involved in drug response and side effects (Denys and De Geus 2005, De Leon 2006). However, only few studies (and mostly with relative small sample sizes) have thus far investigated the role of variants in genes that modulate plasma levels and outcome to anxiolytic drugs. Moreover, no genome wide association studies have been performed in drug response for anxiety disorders. Finally, virtually no pharmacogenetic studies have been performed with benzodiazepines and no single study has investigated gene variants of the GABA genes. In other words, with respect to anxiety disorders, pharmacogenetics is still in an early stage of development and more studies need to be performed. Moreover, a notable heterogeneity among studies including sample sizes, response assessment, and statistical methods hampers the comparison across studies. Despite inconsistent findings across different anxiety-related phenotypes, studies focusing on the serotonin transporter yielded the most consistent findings. Similar—and intuitively plausible-based on findings in depressive disorders—subjects carrying at least one long allele showed in general favorable outcomes (McDougle et al. 1998; Denys et al. 2007). Some positive results were also obtained with polymorphisms of the 5-HT2A gene (Zhang et al. 2004; Denys et al. 2007), although these findings need to be replicated in further and larger samples before meaningful conclusions can be drawn. One significant finding has been reported for the TPH1 gene (Kim et al. 2006). No significant findings have been reported for the MAO-A, COMT, DRD2 and DRD4 genes (Lawford et al. 2003; Zhang et al. 2004). No studies have yet been conducted involving the 5-HT1A, 5-HT1B or TPH2 genes, although they represent good candidates for future studies.
At the present time, the CYP450 gene variants appear to harbor the most promising potential in terms of their usefulness in predicting dosage (plasma levels), response and side effects. Both the CYP2D6 and CYP2C19 genes are of particular relevance in this context as both are involved in the metabolism of most anxiolytic drugs with many known functional gene variants (Black et al. 2007). The classification into poor, intermediate, extensive and rapid metabolizer status would allow to predict or adjust dosages in some drugs to avoid toxic serum levels in poor responders and to avoid non-response in rapid metabolizers (De Leon 2007). Such tests for the CYP2D6 and CYP2C19 genes are commercially available as for example the FDA approved Roche AmpliChip and are easily interpretable. However, the costs associated to such commercially available tests have hampered its widespread use in clinical practice until today (De Leon 2006). The CYP1A2 and CYP3A4 are further important genes in anxiolytic drug metabolism that have not been investigated yet, however. In Table 1, we have listed the most important benzodiazepines and antidepressants and by which CYP450 enzymes these drugs are mainly metabolized (for further details and current updates including CYP450 inhibitors and inducers, we recommend further reading such as the website http://www.medicine.iupui.edu/flockhart/clinlist.htm.)
Obviously, even if dosing based on CYP450 genes has appropriately been taken care of, there is neither a guarantee for a sufficient response nor for the absence of side effects. However, information obtained from CYP450 gene testing may provide important pieces of information which is likely to be beneficial in some individuals. As research progresses, further gene variants involved in metabolism need to be included to optimize doing strategies. One very promising example of the clinical use of genetic testing in dosing strategies is the combination of CYP2C9 and vitamin-K epoxide reductase (VKORC1) gene variants in the dosing of warfarin. In 2007, the FDA has approved the Nanosphere Verigene Warfarin Metabolism Nucleic Acid Test that detects variants in both genes that account for 30–50% of the variability in dosing of warfarin (Flockhart et al. 2008).
As for anxiety disorders, the combination of genetic variants and relevant clinical factors (e.g. age, sex, symptomatology) as well as thorough assessment of co-medication, smoking and diet habits, will ultimately allow designing useful treatment algorithms. These algorithms will allow for a meaningful and clinical significant prediction of dose, as well as for useful prediction of response and side effects likelihood. Despite a scarcity of studies available today, the first steps toward this vision of personalized medicine have been made. The collection of large samples which may include anxious depression as important phenotype, such as the STAR*D sample (e.g. Fava et al. 2008) or from other groups (e.g. Domschke et al. (2008a, b)), combined with high-throughput technology (allowing for genome-wide analysis) needed in this area of research are on their way. Thus, optimism is timely and, importantly, these findings will also enhance our biological understanding of the underlying pathological mechanisms and allow researchers to design novel drug targets.
References
Akillu E, Persson I, Bertilsson L et al (1996) Frequent distribution of ultrapid metabolizers in an Ethiopian population carrying duplicated and multiduplicated functional CYP2D6 alleles. J Pharmacol Exp Ther 278:441–446
Alda M, Dvoráková M, Posmurová M et al (1987) Pharmacogenetic study with diazepam in twins. Neuropsychobiology 17:4–8
Andersson T, Miners JO, Veronese ME et al (1994) Diazepam metabolism by human liver microsomes is mediated by both S-mephenytoin hydroxylase and CYP3A isoforms. Br J Clin Pharmacol 38:131–137
Araki K, Yasui-Furukori N, Fukasawa T et al (2004) Inhibition of the metabolism of etizolam by itraconazole in humans: evidence for the involvement of CYP3A4 in etizolam metabolism. Eur J Clin Pharmacol 60:427–430
Ball SE, Ahern D, Scatina J et al (1997) Venlafaxine: in vitro inhibition of CYP2D6 dependent imipramine and desipramine metabolism; comparative studies with selected SSRIs, and effects on human hepatic CYP3A4, CYP2C9 and CYP1A2. Br J Clin Pharmacol 43:619–626
Bertilsson L, Henthorn TK, Sanz E et al (1989) Importance of genetic factors in the regulation of diazepam metabolism: relationship to S-mephenytoin, but not debrisoquin, hydroxylation phenotype. Clin Pharmacol Ther 45:348–355
Billett EA, Richter MA, King N et al (1997) Obsessive compulsive disorder, response to serotonin reuptake inhibitors and the serotonin transporter gene. Mol Psychiatry 2:403–406
Black JL 3rd, O’Kane DJ, Mrazek DA (2007) The impact of CYP allelic variation on antidepressant metabolism: a review. Expert Opin Drug Metab Toxicol 3:21–31
Bloomer JC, Woods FR, Haddock RE et al (1992) The role of cytochrome P4502D6 in the metabolism of paroxetine by human liver microsomes. Br J Clin Pharmacol 33:521–523
Brachtendorf L, Jetter A, Beckurts KT, Hölscher AH, Fuhr U (2002) Cytochrome P450 enzymes contributing to demethylation of maprotiline in man. Pharmacol Toxicol 90(3):144–149
Brøsen K, Skjelbo E, Rasmussen BB et al (1993) Fluvoxamine is a potent inhibitor of cytochrome P4501A2. Biochem Pharmacol 45:1211–1214
Coller JK, Somogyi AA, Bochner F (1999) Flunitrazepam oxidative metabolism in human liver microsomes: involvement of CYP2C19 and CYP3A4. Xenobiotica 29:973–986
Contin M, Riva R, Albani F et al (1999) Effect of felbamate on clobazam and its metabolite kinetics in patients with epilepsy. Ther Drug Monit 21:604–608
De Leon J (2006) AmpliChip CYP450 test: personalized medicine has arrived in psychiatry. Expert Rev Mol Diagn 6:277–286
De Leon J (2007) The crucial role of the therapeutic window in understanding the clinical relevance of the poor versus the ultrarapid metabolizer phenotypes in subjects taking drugs metabolized by CYP2D6 or CYP2C19. J Clin Psychopharmacol 27:241–245
De Mooij-van Malsen A, Olivier B, Kas MJ (2008) Behavioural genetics in mood and anxiety: a next step in finding novel pharmacological targets. Eur J Pharmacol 585:436–440
De Vry J (1995) 5-HT1A receptor agonists: recent developments and controversial issues. Psychopharmacology (Berl.) 121:1–26
Deckert J, Catalano M, Syagailo YV et al (1999) Excess of high activity monoamine oxidase A gene promoter alleles in female patients with panic disorder. Hum Mol Genet 8(4):621–624
Denys D, de Geus F (2005) Predictors of pharmacotherapy response in anxiety disorders. Curr Psychiat Rep 7:252–257
Denys D, Van Nieuwerburgh F, Deforce D et al (2007) Prediction of response to paroxetine and venlafaxine by serotonin-related genes in obsessive-compulsive disorder in a randomized, double-blind trial. J Clin Psychiat 68:747–753
Di Bella D, Erzegovesi S, Cavallini MC et al (2002) Obsessive-compulsive disorder, 5-HTTLPR polymorphism and treatment response. Pharmacogenom J 2:176–181
Domschke K, Freitag CM, Kuhlenbäumer G et al (2004) Association of the functional V158 M catechol-O-methyl-transferase polymorphism with panic disorder in women. Int J Neuropsychopharmacol 7:183–188
Domschke K, Dannlowski U, Ohrmann P (2008a) Cannabinoid receptor 1 (CNR1) gene: impact on antidepressant treatment response and emotion processing in major depression. Eur Neuropsychopharmacol 18:751–759
Domschke K, Deckert J, Arolt V, Baune B (2008b) Anxious versus non-anxious depression: difference in treatment outcome. Psychopharmacol. Oct 6 [Epub ahead of print]
Domschke K, Lawford B, Laje G et al (2009) Brain-derived neurotrophic factor (BDNF) gene: no major impact on antidepressant treatment response. Int J Neuropsychopharmacol
Eichelbaum M, Ingelman-Sundberg M, Evans WE (2006) Pharmacogenomics and individualized drug therapy. Annu Rev Med 57:119–137
Fava M, Rush AJ, Alpert JE et al (2008) Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiat 165(3):342–351
Firkusny L, Gleiter CH (1994) Maprotiline metabolism appears to co-segregate with the genetically-determined CYP2D6 polymorphic hydroxylation of debrisoquine. Br J Clin Pharmacol 37:383–388
Flockhart DA, O’Kane D, Williams MS et al (2008) Pharmacogenetic testing of CYP2C9 and VKORC1 alleles for warfarin. Genet Med 10:139–150
Fric M, Pfuhlmann B, Laux G et al (2008) The influence of smoking on the serum level of duloxetine. Pharmacopsychiatry 41:151–155
Fujisaki H, Hirotsu K, Ogawa T et al (2001) Metabolism of quazepam and its metabolites in humans: identification of metabolic enzymes and evaluation of drug interaction in vitro. Xenobiot Metab Dispos 16:558–568
Fukasawa T, Yasui-Furukori N, Aoshima T et al (2004) Single oral dose pharmacokinetics of quazepam is influenced by CYP2C19 activity. Therapeut Drug Monitor 26:529–533
Fukasawa T, Yasui-Furukori N, Suzuki A (2005) Pharmacokinetics and pharmacodynamics of etizolam are influenced by polymorphic CYP2C19 activity. Eur J Clin Pharmacol; 61(11):791–795
Fukasawa T, Suzuki A, Otani K (2007) Effects of genetic polymorphism of cytochrome P450 enzymes on the pharmacokinetics of benzodiazepines. J Clin Pharm Ther 32(4):333–341
Gaedigk A, Simon SD, Pearce RE et al (2008) The CYP2D6 activity score: translating genotype information into a qualitative measure of phenotype. Clin Pharmacol Ther 83:234–242
Gardiner SJ, Begg EJ (2006) Pharmacogenetics, drug-metabolizing enzymes, and clinical practice. Pharmacol Rev 58(3):521–590
Ghahramani P, Ellis SW, Lennard MS et al (1997) Cytochromes P450 mediating the N-demethylation of amitriptyline. Br J Clin Pharmacol 43:137–144
Giraud C, Tran A, Rey E et al (2004) In vitro characterization of clobazam metabolism by recombinant cytochrome P450 enzymes: importance of CYP2C19. Drug Metab Dispos 32:1279–1286
Hamilton SP, Slager SL, Heiman GA et al (2002) Evidence for a susceptibility locus for panic disorder near the catechol-O-methyltransferase gene on chromosome 22. Biol Psychiat 51(7):591–601
Heisler LK, Chu HM, Brennan TJ et al (1998) Elevated anxiety and antidepressant-like responses in serotonin 5-HT1A receptor mutant mice. Proc Natl Acad Sci USA 95:15049–15054
Hirota N, Ito K, Iwatsubo T et al (2001) In vitro/in vivo scaling of alprazolam metabolism by CYP3A4 and CYP3A5 in humans. Biopharm Drug Dispos 22:53–71
Holsboer F (2008) How can we realize the promise of personalized antidepressant medicines? Nat Rev Neurosci 9:638–646
Hustert E, Haberl M, Burk O et al (2001) The genetic determinants of the CYP3A5 polymorphism. Pharmacogenetics 11(9):773–779
Ingelman-Sundberg M, Sim SC, Gomez A et al (2007) Influence of cytochrome P450 polymorphisms on drug therapies: pharmacogenetic, pharmacoepigenetic and clinical aspects. Pharmacol Ther 116:496–526
Jeppesen U, Gram LF, Vistisen K et al (1996) Dose-dependent inhibition of CYP1A2, CYP2C19 and CYP2D6 by citalopram, fluoxetine, fluvoxamine and paroxetine. Eur J Clin Pharmacol 51:73–78
Karayiorgou M, Sobin C, Blundell ML et al (1999) Family-based association studies support a sexually dimorphic effect of COMT and MAOA on genetic susceptibility to obsessive-compulsive disorder. Biol Psychiat 45:1178–1189
Kawanishi C, Lundgren S, Agren H et al (2004) Increased incidence of CYP2D6 gene duplication in patients with persistent mood disorders: ultrarapid metabolism of antidepressants as a cause of nonresponse. A pilot study. Eur J Clin Pharmacol 59:803–807
Kharasch ED, Walker A, Isoherranen N et al (2007) Influence of CYP3A5 genotype on the pharmacokinetics and pharmacodynamics of the cytochrome P4503A probes alfentanil and midazolam. Clin Pharmacol Ther 82(4):410–426
Kim W, Choi YH, Yoon KS et al (2006) Tryptophan hydroxylase and serotonin transporter gene polymorphism does not affect the diagnosis, clinical features and treatment outcome of panic disorder in the Korean population. Prog Neuropsychopharmacol Biol Psychiat 30:1413–1418
Kirchheiner J (2008) CYP2D6 phenotype prediction from genotype: which system is the best? Clin Pharmacol Ther 83:225–227
Kirchheiner J, Henckel HB, Meineke I et al (2004) Impact of the CYP2D6 ultrarapid metabolizer genotype on mirtazapine pharmacokinetics and adverse events in healthy volunteers. J Clin Psychopharmacol 24:647–652
Kivistö KT, Lamberg TS, Kantola T, Neuvonen PJ (1997) Plasma buspirone concentrations are greatly increased by erythromycin and itraconazole. Clin Pharmacol Ther 62:348–354
Kosaki K, Tamura K, Sato R et al (2004) A major influence of CYP2C19 genotype on the steady-state concentration of N-desmethylclobazam. Brain Development 26:530–534
Koyama E, Chiba K, Tani M et al (1996) Identification of human cytochrome P450 isoforms involved in the stereoselective metabolism of mianserin enantiomers. J Pharmacol Exp Ther 278:21–30
Kronbach T, Mathys D, Umeno M et al (1989) Oxidation of midazolam and triazolam by human liver cytochrome P450IIIA4. Mol Pharmacol 36:89–96
Lawford BR, McD Young R, Noble EP et al (2003) D2 dopamine receptor gene polymorphism: paroxetine and social functioning in posttraumatic stress disorder. Eur Neuropsychopharmacol 13:313–320
Lee SJ, Usmani KA, Chanas B et al (2003) Genetic findings and functional studies of human CYP3A5 single nucleotide polymorphisms in different ethnic groups. Pharmacogenetics 13(8):461–472
Lesch KP, Aulakh CS, Wolozin BL et al (1993) Regional brain expression of serotonin transporter mRNA and its regulation by reuptake inhibiting antidepressants. Brain Res Mol Brain Res 17:31–36
Lesch KP, Bengel D, Heils A et al (1996) Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science 274:1527–1531
Maier W, Zobel A (2008) Contribution of allelic variations to the phenotype of response to antidepressants and antipsychotics. Eur Arch Psychiatry Clin Neurosci 258:12–20
McDougle CJ, Epperson CN, Price LH et al (1998) Evidence for linkage disequilibrium between serotonin transporter protein gene (SLC6A4) and obsessive compulsive disorder. Mol Psychiatry 3:270–273
Mclellan RA, Oscarson M, Seidegard J et al (1997) Frequent occurrence of CYP2D6 gene duplication in Saudi Arabians. Pharmacogenetics 7:187–191
Miura M, Ohkubo T (2004) In vitro metabolism of quazepam in human liver and intestine and assessment of drug interactions. Xenobiotica 34(11–12):1001–1011
Nakajima M, Yokoi T, Mizutani M et al (1999) Genetic polymorphism in the 5’-flanking region of human CYP1A2 gene: effect on the CYP1A2 inducibility in humans. J Biochem 125:803–808
Nielsen KK, Flinois JP, Beaune P et al (1996) The biotransformation of clomipramine in vitro, identification of the cytochrome P450s responsible for the separate metabolic pathways. J Pharmacol Exp Ther 277:1659–1664
Obach RS, Cox LM, Tremaine LM (2005) Sertraline is metabolized by multiple cytochrome P450 enzymes, monoamine oxidases, and glucuronyl transferases in human: an in vitro study. Drug Metab Dispos 33(2):262–270
Otton SV, Wu D, Joffe RT et al (1993) Inhibition by fluoxetine of cytochrome P450 2D6 activity. Clin Pharmacol Ther 53:401–409
Park JY, Kim KA, Park PW et al (2006) Effect of CYP3A5*3 genotype on the pharmacokinetics and pharmacodynamics of alprazolam in healthy subjects. Clin Pharmacol Ther 79:590–599
Parks CL, Robinson PS, Sibille E et al (1998) Increased anxiety of mice lacking the serotonin1A receptor. Proc Natl Acad Sci USA 95:10734–10739
Parmeggiani A, Posar A, Sangiorgi S, Giovanardi-Rossi P (2004) Unusual side-effects due to clobazam: a case report with genetic study of CYP2C19. Brain Development 26:63–66
Perna G, Favaron E, Di Bella D et al (2005) Antipanic efficacy of paroxetine and polymorphism within the promoter of the serotonin transporter gene. Neuropsychopharmacology 12:2230–2235
Phillips KA, Veenstra DL, Oren E et al (2001) Potential role of pharmacogenomics in reducing adverse drug reactions, a systematic review. JAMA 286:2270–2279
Preskorn SH, Alderman J, Greenblatt DJ et al (1997) Sertraline does not inhibit cytochrome P450 3A-mediated drug metabolism in vivo. Psychopharmacol Bull 33:659–665
Qin XP, Xie HG, Wang W et al (1999) Effect of the gene dosage of CgammaP2C19 on diazepam metabolism in Chinese subjects. Clin Pharmacol Therapeut 66:642–646
Ramboz S, Oosting R, Amara DA et al (1998) Serotonin receptor 1A knockout: an animal model of anxiety-related disorder. Proc Natl Acad Sci USA 95:14476–14481
Rao N (2007) The clinical pharmacokinetics of escitalopram. Clin Pharmacokinet 46(4):281–290
Rau T, Wohlleben G, Wuttke H et al (2004) CYP2D6 genotype: impact on adverse effects and nonresponse during treatment with antidepressants—a pilot study. Clin Pharmacol Ther 75:386–393
Rodriguez-Antona C, Sayi JG, Gustafsson LL et al (2005) Phenotype-genotype variability in the human CYP3A locus as assessed by the probe drug quinine and analyses of variant CYP3A4 alleles. Biochem Biophys Res Commun 338:299–305
Roses AD (2000) Pharmacogenetics and the practice of medicine. Nature 405:857–865
Rothe C, Koszycki D, Bradwejn J et al (2006) Association of the Val158Met catechol O-methyltransferase genetic polymorphism with panic disorder. Neuropsychopharmacology 31:2237–2242
Rudberg I, Mohebi B, Hermann M et al (2008) Impact of the ultrarapid CYP2C19*17 allele on serum concentration of escitalopram in psychiatric patients. Clin Pharmacol Ther 83:322–327
Sand P, Lesch KP, Catalano M et al (2000) Polymorphic MAO-A and 5-HT-transporter genes: analysis of interactions in panic disorder. World J Biol Psychiatry 1:147–150
Sandmann J, Lörch B, Bandelow B et al (1998) Fluvoxamine or placebo in the treatment of panic disorder and relationship to blood concentrations of fluvoxamine. Pharmacopsychiatry 31:117–121
Senda C, Kishimoto W, Sakai K et al (1997) Identification of human cytochrome P450 isoforms involved in the metabolism of brotizolam. Xenobiotica 27:913–922
Seo T, Nagata R, Ishitsu T et al (2008) Impact of CYP2C19 polymorphisms on the efficacy of clobazam therapy. Pharmacogenomics 9(5):527–537
Serretti A, Artioli P, Quartesan R (2005) Pharmacogenetics in the treatment of depression: pharmacodynamic studies. Pharmacogenet Genomics 15:61–67
Sibille E, Pavlides C, Benke D et al (2000) Genetic inactivation of the Serotonin(1A) receptor in mice results in down regulation of major GABA(A) receptor alpha subunits, reduction of GABA(A) receptor binding, and benzodiazepine-resistant anxiety. J Neurosci 20:2758–2765
Skinner MH, Kuan HY, Pan A et al (2003) Duloxetine is both an inhibitor and a substrate of cytochrome P4502D6 in healthy volunteers. Clin Pharmacol Ther 73:170–177
Spina E, Pollicino AM, Avenoso A et al (1993) Effect of fluvoxamine on the pharmacokinetics of imipramine and desipramine in healthy subjects. Ther Drug Monit 1993(15):243–246
Steimer W, Zöpf K, von Amelunxen S et al (2005) Amitriptyline or not, that is the question: pharmacogenetic testing of CYP2D6 and CYP2C19 identifies patients with low or high risk for side effects in amitriptyline therapy. Clin Chem 51:376–385
Stein MB, Stein DJ (2008) Social anxiety disorder. Lancet 371:1115–1125
Stein MB, Seedat S, Gelernter J (2006) Serotonin transporter gene promoter polymorphism predicts SSRI response in generalized social anxiety disorder. Psychopharmacology (Berl) 187:68–72
Timmer CJ, Sitsen JM, Delbressine LP (2000) Clinical pharmacokinetics of mirtazapine. Clin Pharmacokinet 38:461–474
Tot S, Erdal ME, Yazici K et al (2003) T102C and -1438 G/A polymorphisms of the 5-HT2A receptor gene in Turkish patients with obsessive-compulsive disorder. Eur Psychiatry 18:249–254
Veenstra-VanderWeele J, Anderson GM, Cook EH (2000) Pharmacogenetics and the serotonin system: initial studies and future directions. Eur J Pharmacol 410:165–181
Venkatakrishnan K, Greenblatt DJ, von Moltke LL et al (1998) Five distinct human cytochromes mediate amitriptyline N-demethylation in vitro: dominance of CYP 2C19 and 3A4. J Clin Pharmacol 38:112–121
Walther DJ, Bader M (2003) A unique central tryptophan hydroxylase isoform. Biochem Pharmacol 66:1673–1680
Wandel C, Bocker R, Bohrer H et al (1994) Midazolam is metabolized by at least three different cytochrome P450 enzymes. Br J Anaesth 73:658–661
Watanabe T, Ueda M, Saeki Y et al (2007) High plasma concentrations of paroxetine impede clinical response in patients with panic disorder. Ther Drug Monit 29:40–44
Wolbold R, Klein K, Burk O et al (2003) Sex is a major determinant of CYP3A4 expression in human liver. Hepatology 38:978–988
Yamazaki H, Shimada T (1996) Progesterone and testosterone hydroxylation by cytochrome P450 2C19, 2C9, and 3A4 in human liver microsomes. Arch Biochem Biophys 346:161–169
Zanger UM, Turpeinen M, Klein K et al (2008) Functional pharmacogenetics/genomics of human cytochromes P450 involved in drug biotransformation. Anal Bioanal Chem 392:1093–1108
Zhang L, Liu X, Li T et al (2004) Molecular pharmacogenetic studies of drug responses to obsessive-compulsive disorder and six functional genes. Zhonghua Yi Xue Yi Chuan Xue Za Zhi 21:479–481
Zhu M, Zhao W, Jimenez H et al (2005) Cytochrome P450 3A-mediated metabolism of buspirone in human liver microsomes. Drug Metab Dispos 33(4):500–507
Author information
Authors and Affiliations
Corresponding author
Additional information
A. K. Tiwari and R. P. Souza contributed equally.
Rights and permissions
About this article
Cite this article
Tiwari, A.K., Souza, R.P. & Müller, D.J. Pharmacogenetics of anxiolytic drugs. J Neural Transm 116, 667–677 (2009). https://doi.org/10.1007/s00702-009-0229-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-009-0229-6