Abstract
The purpose of this study is to summarize our experience in managing patients with an atypical or malignant meningioma at our institution, with a specific focus on determining the prognostic factors for treatment outcome. We reviewed the records of 126 patients with atypical or malignant meningiomas from January 2001 to August 2011. Data collected included gender, age, Karnofsky Performance Scale (KPS) score, pathology results, cleavability, and bone invasion. The symptoms and signs were recorded for further outcome analysis. There were 37 malignant meningiomas and 89 atypical meningiomas. Total resection (Simpson grade I–II) was achieved in 80.9 % of atypical patients (n = 72) and 67.6 % of malignant patients (n = 25). Forty patients (44.9 %) in the atypical group underwent radiotherapy after surgery, while 26 (70.2 %) patients underwent radiotherapy in the malignant group. The median follow-up duration was 25 months. Patients with a secondary tumor had a much shorter progression-free survival (PFS) than those with a primary tumor in the malignant group. The malignant meningioma group had lower overall survival. Progression-free survival for patients in the malignant group who received postoperative radiotherapy was longer than that for those who did not receive radiotherapy. In conclusion, total resection of the tumor was important because patients with a secondary tumor were much more likely to have recurrence than patients with a primary tumor in the atypical and malignant meningioma groups. Also, radiotherapy should be performed after surgery for a malignant meningioma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meningiomas are among the most common primary brain tumors in adults, accounting for 33 % of all brain tumors with an incidence of 6 per 100,000 [12]. The majority of meningiomas are benign tumors (90 %) with a good prognosis after total resection. However, about 4.7–7.2 % of meningiomas are atypical and malignant meningiomas [4], which have a high risk of recurrence of 35–75 % despite total resection and/or radiation therapy (Simpson grade I–II). Radiotherapy is an important adjuvant therapy for atypical and malignant meningiomas. Some studies have shown that patients with these tumors benefit from radiotherapy, but there is no agreement on what kind of patients should receive postoperative radiotherapy [17]. Thus, the aim of this retrospective study was to determine the characteristics of patients and factors that influence outcome in the treatment of atypical or malignant meningiomas.
Materials and methods
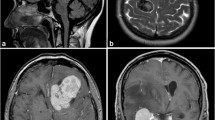
This study was approved by our Institutional Review Board. We reviewed retrospectively the medical records of 126 patients with atypical (n = 89) and malignant (n = 37) meningiomas who underwent surgical treatment from January 2001 to August 2011 in Beijing Tiantan Hospital. Data were collected from the patient data management system and included gender, age, Karnofsky Performance Scale (KPS) score, pathology results, cleavability, and bone invasion. The extent of resection was confirmed by reviewing the postoperative imaging studies and the operative records (Simpson grade I–II was defined as total resection (TR) and grade III–IV was defined as subtotal resection (STR). We used the term “atypical” as synonymous with WHO 2000 grade II and the term “malignant” as synonymous with WHO 2000 grade III. Data on cleavability were obtained from original operative records with special emphasis on bone invasion.
The follow-up was performed from 2 to 8 years after discharge with radiology. All patients underwent CT and/or MRI scans at 3 and 6 months and 1–2 years for the radiographic evaluation after surgery. Neurological outcomes were assessed using overall survival (OS) and progression-free survival (PFS) rates. Recurrence was diagnosed if a new lesion was detected on a follow-up MRI scan. We excluded 30 patients because of inadequate data in their records on their disease history. The median follow-up was 25 months (15 patients after 2010, 111 patients before 2010). Further, the follow-up time was about 6 months to 8 years for the atypical group and 3 months to 5 years for the malignant meningiomas. Symptoms and signs were recorded for outcome analysis.
The criteria for postoperative radiotherapy were carried out by the pathology of the patients with operation excision degree. For malignant meningiomas, the number of patients with Simpson grade I–II who received TR was 25 and 26 cases underwent radiotherapy. Among the patients with atypical meningiomas, the number of patients with Simpson grade I–II who received TR was 72 and 40 cases received radiotherapy.
Statistical analysis
The statistical analysis was performed with SPSS 17.0 software for Windows (SPSS Inc, Chicago, IL, USA). The differences in clinical parameters between groups were analyzed by Kruskal–Wallis and chi-square tests. The univariate Cox survival analysis was used to compare different survival functions according to clinical factors (gender, age, tumor location, symptom, KPS, primary or secondary lesion, pathology grade, tumor size, cleavability, skull invasion, etc.) and therapeutic factors (Simpson grade, with or without radiotherapy). OS and PFS rates were calculated after the operations. Multivariate Cox survival analysis was achieved by the forward log–rank test. Differences were considered significant at p < 0.05.
Results
Patient and tumor characteristics
Our study included 126 patients, 37 with malignant meningiomas and 89 with atypical meningiomas. The clinical and therapeutic characteristics are shown in Table 1. There were significant differences between the two groups in patient age, KPS score, presence of primary tumor, tumor size, and radiotherapy (p < 0.05). The mean age of patients with atypical meningiomas was 53.3 years which was older than the patients (50.8 years) in the malignant group (p < 0.01). The atypical group had a higher KPS score with a median of 90 (range, 50–100) than the malignant group which had a median of 80 (range, 30–70) (p < 0.01). In the atypical group, 78 (87.6 %) patients presented with primary lesions, which was significantly different from the malignant group in which 14 (37.8 %) of the patients had primary tumors (p < 0.01). Tumor size was described by the maximum diameter. The malignant group had a mean maximum diameter of 6.37 cm which was significantly larger than the mean maximum diameter of 5.95 cm in the atypical group (p = 0.026). Twenty-six patients in the malignant group underwent postoperative radiotherapy compared with 40 patients in the atypical group (p = 0.01). The patients underwent postoperative radiotherapy as aforementioned criteria. There were no significant differences in sex, tumor location, symptoms, cleavability, skull invasion, or multi-occupation between the two groups (p > 0.100). Seventy-two (80.9 %) patients in the atypical group had total resection compared with 25 (67.5 %) patients in the malignant group (p > 0.01).
Analysis of the malignant group
The malignant group included 37 patients (19 males and 18 females) with a mean age of 50.8 years (range, 16–71 years) (Table 2). The mean PFS was 27.2 months (range, 1–94 months; 95 % confidence interval (CI), 14.8–39.5). The 1-, 2-, and 5-year PFS rates were 54.4, 38.6, and 12.1 %, respectively. Twenty-six patients received the adjunctive radiotherapy after surgery, and 15 (57.7 %) of them relapsed. Eleven patients did not receive the adjunctive radiotherapy, and nine (81.8 %) of these patients relapsed. The PFS of the patients who received postoperative radiotherapy was longer than that of those who did not receive radiotherapy (hazard ratio (HR), 0.410; p = 0.039). Patients with bone invasion had a threefold risk of recurrence (HR, 3.108; p < 0.01). A secondary tumor was much more likely to relapse than a primary tumor; the increased risk was threefold (HR, 3.289; p = 0.015). However, patients with noncleavable tumors had a 61.7 % lower risk of progression compared with patients who had cleavable tumors (HR, 0.383; p = 0.038). Fourteen out of 17 patients with noncleavable tumors (82.4 %) received the adjunctive radiotherapy after surgery, and 12 out of 20 patients with cleavable tumors (60 %) also received the adjunctive radiotherapy after surgery. The results showed that five patients relapsed in the noncleavable group and ten patients relapsed in the cleavable group. The mean OS was 40.9 months (range, 2–94 months; 95 % CI, 27.5–54.4). The 1-, 2-, and 5-year survival rates were 81.7, 59.7, and 19.9 %, respectively. The OS rates of patients on radiotherapy, bone invasion, or secondary tumor had much significance with PFS rates (p < 0.05). Nine of the 12 patients with STR relapsed, whereas 15 of the 25 patients with TR relapsed (p > 0.05). However, the patients who had STR showed a decline in PFS (HR, 1.630; p = 0.654). Other factors such as gender, age, tumor location, symptoms, KPS score, and tumor size demonstrated no significant difference between the PFS and OS rates (p > 0.05). On multivariate analysis (Table 4), adjunctive radiotherapy was a beneficial factor for the OS rate (HR, 0.151; p < 0.01). Patients with multi-occupation had a lower OS rate than the patients without multi-occupation (HR, 3.775; p = 0.026). The only parameter that influenced PFS was the presence of a primary or secondary tumor. Patients with secondary tumors had a much shorter PFS than those with primary tumors (HR, 3.289; p = 0.015).
Analysis of the atypical group
The atypical group included 89 patients with a mean age of 53.3 years (range, 7–73 years) (Table 3). The mean PFS was 72.6 months (range, 2–102 months; 95 % CI, 61.8–83.4). The 1-, 2-, 5-, and 8-year PFS rates in this group were 82.9, 74.5, 67.5, and 47.6 %, respectively. Female patients had a twofold increased risk of recurrence (HR, 2.361; p = 0.044). Patients with paresis were much more likely to relapse than the patients with other symptoms (HR, 2.524; p = 0.028). Patients with secondary atypical meningiomas showed a threefold increased risk of recurrence (HR, 2.948; p = 0.012). A KPS score of more than 80 presented longer PFS compared with that less than 80 (HR, 0.458; p = 0.074). There was no significant difference in the median PFS between the patients with TR and those with STR (HR, 1.551; p = 0.356). The 1-, 2-, 5-, and 8-year OS rates in the atypical group were 97.1, 93.6, 89.1, and 89.1 %, respectively. The mean OS in this group was 96.6 months (range, 10–107 months; 95 % CI, 89.4–103.9). A KPS score of more than 80 was related to OS (HR, 0.094; p < 0.01). The TR group had longer OS than the STR group (HR, 6.055; p = 0.021). For other factors such as age, tumor location, size, noncleavable tumor, bone invasion, multi-occupation, and radiotherapy, there was no significant difference between PFS and OS (p > 0.05). On multivariate analysis (Table 4), patients with paresis had a lower PFS rate than patients with other symptoms (HR, 3.098; p = 0.010). The factor of secondary tumor was related to poor PFS (HR, 3.526; p < 0.01). Only KPS score might influence OS and that of more than 80 was a beneficial factor for OS (HR, 0.096; p < 0.01).
Discussion
The existence of malignant and atypical meningiomas has been recognized since 1938, when Cushing and Eisenhardt reported a variant of meningioma in patients with a mean survival time of 2.5 years [17]. Since that time, the treatment of malignant and atypical meningiomas has been associated with high recurrence. In this retrospective study, we were able to identify clinical features that predict the progression and clinical outcome of atypical or malignant meningiomas. We found that patients with atypical meningiomas have longer PFS and OS than the patients with malignant meningiomas (p < 0.01) (Fig. 1). Patients with the symptom of paresis in the atypical group had a lower PFS rate than the patients in that group with other symptoms (p = 0.010). Patients with secondary tumors in the malignant group had a much lower PFS rate than patients in that group with primary tumors. In the atypical group, a KPS score of more than 80 was related to good prognosis (p < 0.05), but that was poor in the malignant group (p > 0.05). Statistics from our results showed that the female relapse rate was two times the male relapse rate, and it was not clear whether gender and estrogen in the occurrence of meningiomas had an important role. This needed a lot of data to prove. Other factors such as tumor location, symptoms, cleavability, bone invasion, and multi-occupation had no significant difference between the two groups (p > 0.100). Among these, the location of the tumor showed no difference between the two groups (p = 0.98). It does not mean that the resection rate has some relationship between them (80.9 % in the atypical group vs 67.5 % in the malignant group). One reason is that an atypical tumor in the brain is more excisable than a malignant tumor in the same location. And, for the malignant tumor, it invades the brain more than the atypical one, so the surgical resection becomes more difficult. Palma et al. reported a group of recurrent meningioma patients (42 with grade II and 29 with grade III) who received adjuvant radiotherapy. The overall survival rate at 10 years was 79 and 34 % for patients with atypical and malignant meningiomas, respectively (p < 0.01); median recurrence-free survival was 11.9 and 2 years, respectively (p < 0.01) [12]. However, patients with atypical meningiomas had a poor prognosis, with a median survival time of less than 2 years [9]. In our study, we found that patients with malignant meningiomas had worse overall survival rate than patients with atypical meningiomas.
Operation should be the first choice for the treatment of atypical or malignant meningiomas. Many studies have shown that total resection might lead to a higher local control rate than subtotal resection for benign and malignant meningiomas [6]. Jaaskelainen et al. reported that the recurrence rate of meningiomas for Simpson grade II was double that for grade I [7]. So, they suggested that gross total resection could be a good prognosis for the Simpson grade I resection. In our study, complete resection had some relationship with patients’ outcome. In the malignant group, the STR patients showed a tendency for lower PFS rate. The median PFS of the TR group had no significant difference with that of the STR group for atypical meningiomas. But, the TR group had a longer OS than the STR group. Palma and his colleague reported that radical excision was significantly related to prolonged survival on multivariate analysis (p < 0.01) [12]. Goyal et al. also concluded that patients with TR had a longer OS and PFS than patients with STR (p = 0.02). Therefore, they recommended a total resection to prolong the survival period [5].
For STR, adjuvant radiotherapy is required after surgery [2]. It is well known that postoperative radiotherapy is the common treatment for patients with atypical meningiomas to improve the survival rate [6]. Some authors have suggested that radiotherapy is also a necessary supplementary treatment for malignant meningiomas regardless of the extent of resection [4, 11]. In our analysis, the malignant group showed good prognosis with radiotherapy after surgery (p < 0.05). But, for the atypical group, radiotherapy produced no significant difference between PFS and OS (p > 0.05) (Fig. 2). Subtotal resection of atypical meningiomas should follow with adjuvant radiotherapy [11]. However, it does not apply to the TR group of atypical meningioma [10]. Modha and Gutin reported that patients with TR for atypical meningiomas should receive radiotherapy whether there was bone invasion or not. In our study, there was no significant difference between PFS and OS after radiotherapy for the atypical group (p > 0.05).
The PFS rate of prognosis with radiotherapy for the malignant meningioma group and the atypical meningioma group. a There was a significant difference between the radiotherapy group and non-radiotherapy group with regard to prognosis of the PFS rate in the malignant group (p = 0.039); b there was no significant difference between the non-radiotherapy group and radiotherapy group for the prognosis of PFS rate in the atypical group (p = 0.422). PFS progression-free survival, RT radiotherapy, NRT none radiotherapy
There is controversy over whether bone or brain invasion should be considered in the classification of meningiomas [16]. Sindou et al. reported that meningiomas were classified as noncleavable when pial invasion was observed by the surgeon and cleavable when dissection in the extrapial plane was performed [15]. They studied 150 consecutive patients with intracranial meningiomas. Dissection between tumor and underlying cortex was achieved in the extrapial plane predominantly in only 54.6 % of patients. The other nearly half of the patients with pial and bone invasion had noncleavable meningiomas. However, from our analysis, the noncleavable cases showed a lower risk of progression than the cleavable cases in the malignant group. Perhaps radiotherapy plays a positive role on the PFS of patients with malignant meningiomas, whether it is cleavable or noncleavable (HR = 0.410; p = 0.039). Although bone or pial invasion has not become a classification criterion, the recurrence rate should be considered for atypical or malignant meningiomas [14, 17]. Ho et al. reported that bone invasion was an adverse prognostic factor for atypical meningiomas (p < 0.01) [3]. Though we did not find significant difference, it also seemed that cleavable and skull invasion were adverse prognostic factors in the atypical group. If the tumor is cleavable with local invasion, we would advise patients to undertake radiotherapy after operation for the atypical lesion. It would improve the prognosis by our statistics.
According to WHO Classification 2000, atypical meningiomas (grade II) present at least four mitotic figures per 10 high-power fields, and malignant meningiomas (grade III) present frank histological malignancy or 20 mitotic figures per 10 high-power fields [13]. So, when the mitosis is closer to 20 per 10 high-power fields, it may reflect more aggressive tumor biology compared to low mitosis in atypical meningiomas [1]. Perry et al. summarized different studies of mean MIB-1 LI (label index) and reported a range of 2.1 to 9.3 % for atypical meningiomas and 11.0 to 16.3 % for malignant meningiomas [14]. They suggested 10 % of MIB-1 LI as the cutoff point for atypical and malignant meningiomas. And, they suggested an MIB-1 LI of 4 % as the appropriate threshold for atypical meningiomas [8]. In our study, we did not obtain the same results as reported in the literature. This should be further explored.
In conclusion, atypical and malignant meningiomas are difficult to treat as demonstrated by high recurrence and mortality rates. It is important to resect the tumor totally because a secondary tumor is much more likely to relapse than a primary tumor for atypical and malignant meningiomas. Patients with malignant meningiomas should receive radiotherapy immediately after surgery regardless of the extent of resection. But, for atypical meningiomas, the symptoms, KPS score, and primary or secondary lesion should be evaluated before radiotherapy. Moreover, further prospective studies should be carried out to analyze the influence of postoperative radiotherapy for atypical and malignant meningiomas.
References
Bruna J, Brell M, Ferrer I, Gimenez-Bonafe P, Tortosa A (2007) Ki-67 proliferative index predicts clinical outcome in patients with atypical or anaplastic meningioma. Neuropathology 27:114–120
Campbell BA, Jhamb A, Maguire JA, Toyota B, Ma R (2009) Meningiomas in 2009: controversies and future challenges. Am J Clin Oncol 32:73–85
Ho DM-T, Hsu C-Y, Ting L-T, Chiang H (2002) Histopathology and MIB-1 labeling index predicted recurrence of meningiomas—a proposal of diagnostic criteria for patients with atypical meningioma. Cancer 94:1538–1547
Dziuk T, Woo S, Butler EB, Thornby J, Grossman R, Dennis WS, Lu H, Carpenter LS, Chiu JK (1998) Malignant meningioma: an indication for initial aggressive surgery and adjuvant radiotherapy. J Neurooncol 37:177–188
Goyal LK, Suh JH, Mohan DS, Prayson RA, Lee J, Barnett GH (2000) Local control and overall survival in atypical meningioma: a retrospective study. Int J Radiat Oncol Biol Phys 46:57–61
Hug EB, Devries A, Thornton AF, Munzenride JE, Pardo FS, Hedley-Whyte ET, Bussiere MR, Ojemann R (2000) Management of atypical and malignant meningiomas: role of high-dose, 3D-conformal radiation therapy. J Neurooncol 48:151–160
Jaaskelainen J, Haltia M, Servo A (1986) Atypical and anaplastic meningiomas: radiology, surgery, radiotherapy, and outcome. Surg Neurol 25:233–242
Kasuya H, Kubo O, Tanaka M, Amano K, Kato K, Hori T (2006) Clinical and radiological features related to the growth potential of meningioma. Neurosurg Rev 29:293–296
Louis DN, Ohgaki H, Wiestler OD (2007) WHO classification of tumors of the central nervous system. IARC, Lyon
Milosevic MF, Frost PJ, Laperriere NJ, Wong CS, Simpson WJ (1996) Radiotherapy for atypical or malignant intracranial meningioma. Int J Radiat Oncol Biol Phys 34:817–822
Modha A, Gutin P (2005) Diagnosis and treatment of atypical and anaplastic meningiomas: a review. Neurosurgery 57:538–550
Palma L, Celli P, Franco C, Cervoni L, Cantore G (1997) Long-term prognosis for atypical and malignant meningiomas: a study of 71 surgical cases. J Neurosurg 86:793–800
Pearson BE, Markert JM, Fisher WS, Guthrie BL, Fiveash JB, Palmer CA, Riley K (2008) Hitting a moving target: evolution of a treatment paradigm for atypical meningiomas amid changing diagnostic criteria. Neurosurg Focus 24:E3
Perry A, Stafford SL, Scheithauer BW, Suman VJ, Lohse CM (1997) Meningioma grading: an analysis of histologic parameters. Am J Surg Pathol 21:1455–1465
Sindou M, Alaywan M (1998) Most intracranial meningiomas are not cleavable tumours: anatomic-surgical evidence and angiographic predictability. Neurosurgery 42:476–480
Vranic A, Popovic M, Cör A, Prestor B, Pizem J (2010) Mitotic count, brain invasion, and location are independent predictors of recurrence-free survival in primary atypical and malignant meningiomas: a study of 86 patients. Neurosurgery 67:1124–1132
Whittle IR, Smith C, Navoo P, Collie D (2004) Meningiomas. Lancet 363:1535–1543
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Hoi Sang, San Diego, USA
In this manuscript, the authors describe their experience with 89 atypical and 37 malignant meningioma treatments with surgical excision (total excision in 97 patients) with some followed by postoperative irradiation (66 patients). These patients were followed clinically for 2 to 8 years. The conclusions of the study are the following: (1) patients with secondary tumors have a much shorter progression-free survival (PFS) than those with primary tumors in the malignant group, (2) the malignant meningioma patients had a reduced overall survival, and (3) PFS in patients with malignant meningiomas who received postoperative radiotherapy is longer than those who did not receive radiotherapy.
This study is based on the experience of one of the most busy neurosurgical departments in China and is therefore worthy of note. With the detailed analysis of this extensive experience, this manuscript adds further to our knowledge of the natural history of atypical and malignant meningiomas especially in their need for and response to radiotherapy.
Peng Zhao and Mengqing Hu contribute equally to this study.
Rights and permissions
About this article
Cite this article
Zhao, P., Hu, M., Zhao, M. et al. Prognostic factors for patients with atypical or malignant meningiomas treated at a single center. Neurosurg Rev 38, 101–107 (2015). https://doi.org/10.1007/s10143-014-0558-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-014-0558-2