Abstract
Esophagojejunal anastomotic leakage (EJAL) is a serious complication of total or proximal gastrectomy for gastric cancer, with a reported incidence of 2.1–14.6% and mortality of up to 50%. EJAL is an independent prognostic factor for the poor survival of gastric cancer patients. Meticulous surgical techniques, experience with anastomotic devices, and a thorough understanding of various risk factors and preventive measures are essential and early diagnosis is critical for preventing EJAL-related death. Patients with suspected EJAL must be evaluated promptly, but contrast swallow is not recommended. There is no standard treatment strategy for EJAL, although conservative treatment with drainage and nutritional support is the most common approach. Effective endoscopic treatments have been reported but need further validation. Surgical treatment is associated with high mortality but should be considered to prevent death from suboptimal EJAL management, for patients with severe sepsis or when conservative treatment has failed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gastrectomy with lymphadenectomy is a standard treatment for gastric cancer, while total or proximal gastrectomy followed by esophagojejunal (EJ) anastomosis is a standard treatment for gastric cancer invading the upper third of the stomach and for adenocarcinoma of the esophagogastric junction [1]. Despite advances in surgical techniques and perioperative management, EJ anastomotic leakage (EJAL) remains a serious and potentially fatal complication of total or proximal gastrectomy, with incidences ranging from 2.1 to 14.6% [2,3,4,5,6,7,8,9,10,11,12,13,14,15]. EJAL has a negative impact on other postoperative outcomes, by increasing pulmonary complications, median length of hospital stay, delay before oral feeding, risk of anastomotic stricture, and the need for re-operation by up to 61% [15]. EJAL following gastrectomy has a reported mortality of up to 50% and is the leading cause of mortality-related death after this procedure [3,4,5,6,7,8,9,10,11,12, 15,16,17]. Furthermore, EJAL is an independent prognostic factor for poor survival after gastric cancer surgery [14, 15, 18].
Surgeons have tried various strategies to prevent EJAL. There is no doubt that advances in surgical techniques, better anatomical knowledge, and increased awareness of the risk factors and treatment options have contributed greatly to decreasing the incidence and mortality of EJAL. We reviewed the literature on EJAL following gastrectomy for gastric cancer to summarize the prevalence, risk factors, prevention strategies, and treatment of EJAL.
Prevalence
The prevalence of EJAL following open gastrectomy for gastric cancer has been reported to range from 2.1 to 14.6% [2,3,4,5,6,7,8,9,10,11,12,13,14,15], with mortality associated with EJAL ranging from 0 to 50% [3,4,5,6,7,8,9,10,11,12, 15,16,17]. The variations in the literature may be explained by differences in study cohort size, study design, country, and study periods (Table 1). The EJAL incidence and mortality tend to be lower in Asian countries (including Japan) than in Western countries. The incidence of EJAL following open total gastrectomy was 4.4% in a prospective cohort study including patients selected from a Japanese nationwide registry [13], whereas the incidence ranged from 4 to 26% in phase III studies conducted in Western countries [19, 20]. This difference may be attributed to the higher incidence of cardiopulmonary comorbidities and more intra-abdominal fat tissue in patients with gastric cancer from Western countries as well as the higher incidence of gastric cancer in Asian patients [8, 21]. Pulmonary insufficiency [5, 8], cardiovascular disease [9], and increased visceral fat area (VFA) [22,23,24] are all risk factors for EJAL. As gastric cancer is one of the most commonly diagnosed cancers in Japan [25], Japanese surgeons have considerable experience in performing gastric cancer surgery, which may account for the relatively lower incidence of EJAL in Japan.
The prevalence of EJAL varies with the year of each study because of changes in the anastomotic devices that were used at the time. An analysis of a large patient series at the National Cancer Center of Japan showed that the incidence of EJAL decreased from 20.0% in 1985 to 0.8% in 1997 [12]. Over the same period, the use of stapler anastomosis increased from 8 to 100%. Because the surgical outcomes of stapler anastomosis are clearly superior to those obtained with manually sutured anastomosis, it has become the standard method. After Kitano introduced laparoscopic gastrectomy in 1991, the technique became popular throughout the world, particularly in East Asia [26]. In 1999, Uyama et al. [27] reported the first case of laparoscopic total gastrectomy, which involved esophagojejunal anastomosis using a linear stapler with functional end-to-end anastomosis (FEEA). According to a recent large-scale cohort study and multi-center phase II studies, the prevalence of post-LTG EJAL ranges from 1.7 to 5.7% [28,29,30].
Risk factors
Identification of the risk factors of EJAL helps to decrease its incidence. The reported risk factors include patient and tumor characteristics and intraoperative factors. Sufficient blood supply [9, 31] and adequate tension on the anastomosis site [9, 32] are essential for proper healing. Long operation time [8], invasive surgery [2, 15, 24], anastomosis procedures [5], and surgeon inexperience (< 30 cases) [16] have all been reported as intraoperative risk factors. In a retrospective evaluation of a large patient cohort, Tu et al. [33] developed a nomogram to predict the individual risk of anastomotic leakage. Patient age ≥ 65 years, anemia (hemoglobin ≤ 8.0 g/dL), and malnutrition were independently associated with the risk of leakage. In a large, retrospective, cohort study using a Japanese web-based nationwide registry, age, sex, preoperative ADL, ascites, hypertension, previous percutaneous coronary intervention, steroid administration, weight loss, poor ASA score, splenectomy, Brinkman index, body mass index, elevated aspartate aminotransferase, and an elevated white blood cell count were identified as risk factors for anastomotic leakage following total gastrectomy [34]. Sarcopenia, characterized by muscle wasting, has also been reported to increase the risk of postoperative complications following surgery for several malignancies [35,36,37,38]. A recent meta-analysis demonstrated that preoperative sarcopenia was a risk factor for postoperative complications following gastrectomy, though it was not found to be a risk factor for anastomotic leakage [39]. Elderly patients tend to have more comorbidities, poor nutritional and performance status, and poor wound healing. Anemia and malnutrition may result in insufficient blood and energy supplies to the anastomosis, which might affect the healing of the anastomosis and reduce the levels of inflammatory cells, inflammatory factors, and administered antibiotics, thereby increasing the risks of infection and of anastomotic leakage [31, 40,41,42]. Obesity also increases the risk of postoperative complications. Body mass index (BMI) is a standard criterion of obesity, but the visceral fat area (VFA) may be more important to predict EJAL [22,23,24]. The presence of a thick mesentery in patients with a high VFA tends to produce excessive tension and pressure at the anastomosis site. In addition, the deep surgical field in these patients provides a less-than-optimal surgical view that could predispose to surgical errors during anastomosis surgery. Other reported patient factors include diabetes [6], pulmonary insufficiency [5, 8], cardiovascular disease [9], and chronic renal failure [6]. Pathological stage IV [2, 9] and esophageal invasion [6] have also been reported as tumor risk factors.
Several case controls have compared LTG and open total gastrectomy (OTG) mortality; however, a recent meta-analysis showed no difference in the incidence of EJAL between these procedures [43]. Two large-scale, prospective studies in Japan and Korea reported that LTG for clinical stage I gastric cancer patients is safe, with EJAL incidences of 1.6% and 1.9%, respectively [29, 30]. However, we cannot deny the possibility of publication or selection bias. A large-scale, retrospective cohort study using the NCD database and including ≥ 30,000 patients revealed that the rate of EJAL was higher for LTG than for OTG, for both clinical stage I (5.4% vs. 3.6%, p < 0.01) and stage II–IV patients (5.7% vs. 3.6%, p < 0.020) [28]. However, another prospective cohort study, using the NCD database, demonstrated no significant difference in the incidence of EJAL between LTG and OTG (5.3% vs. 6.1%, P = 0.59) [44]. This inconsistency could be due in part to selection bias, as the latter study included fewer institutions and the data were retrieved 2 years before the former study. Since there are no large-scale randomized controlled trials, whether laparoscopic surgery is a risk factor for EJAL remains unknown.
Various anastomosis techniques for the esophagojejunal anastomotic procedure following LTG have been described, including FEEA, overlap using a linear stapler [45], a single stapling technique [46], a double stapling technique [47], a hemi-double stapling technique using a circular stapler [48], and hand-sewn methods [49]. A meta-analysis showed that circular stapler methods were significantly associated with EJAL (4.7% vs. 1.1%, p < 0.001) [50]; however, there is no clear evidence based on randomized controlled trials. Therefore, the optimal procedure of EJA in LTG has not been established.
Prevention
The prevention of EJAL depends on the recognition and management of its risk factors. For example, addressing malnutrition with preoperative enteral feeding or immunonutrition therapy has been reported to reduce the incidence of anastomotic leakage [51, 52]. Precise surgical technique and good understanding of anastomotic devices are also essential. Circular staplers are the most commonly used devices to perform EJ anastomosis, but their use requires learning skills and avoiding some pitfalls. The incomplete placing of purse-string sutures, incorrect insertion of the anvil on the esophageal mucosal layer, and piercing the oral side of the jejunal limb when firing the stapler may result in serious complications, such as EJAL. The integrity of the ring of tissue retained in the circular stapler after completion of the anastomosis should be confirmed. If the mucosal or muscular layer of the ring is discontinuous, additional suturing is required to reinforce the anastomosis.
The usefulness of intraoperative air leak testing and endoscopic examination has been reported [16, 17, 53]. These methods have been shown to detect physical dehiscence and surgeons can add sutures that may prevent EJAL; however, neither method can prevent anastomotic leakage in every patient because the incidence of EJAL depends not only on intraoperative factors, but also on patient conditions. Nevertheless, intraoperative air-leak testing should be performed whenever surgeons suspect EJAL. The test can be performed easily, safely, and without additional cost, although the low sensitivity of intraoperative methods should be borne in mind.
In a prospective randomized trial of the benefit of supplemental oxygen, Schietroma et al [9] found that the risk of EJAL was 49% lower in patients who received 80% FiO2 than in those who received 30% FiO2 during and 6 h after open total gastrectomy surgery. Haverkamp et al [54] reported that the reinforcement of EJ and esophagogastric anastomoses with a fibrin patch (TachoSil; Baxter Healthcare, Deerfield, IL, USA) reduces the occurrence of EJAL. The patch, which contains human fibrinogen and thrombin, was folded into a harmonica shape and wrapped around the anastomosis. It improved the mechanical strength and may prove effective in clinical practice to prevent anastomotic leakage. Afaneh et al [55] used a degradable extracellular matrix scaffold derived from porcine urinary bladder (MatriStem; ACell Inc., Columbia, MD, USA) to reinforce the EJ anastomosis. A total of 37 patients who underwent total gastrectomy followed by EJ anastomosis were enrolled in their study. The scaffold was wrapped around the anastomosis and EJAL developed in only one patient (2.7%). Although both studies evaluated small-scale case series, the results warrant further investigation to clarify the efficacy of these methods.
Diagnosis
The successful management of EJAL depends on early detection and prompt treatment. The presence of digestive fluids in surgical drains is unequivocal evidence of EJAL, but initial clinical signs are often nonspecific, such as pyrexia, elevation of the white blood count or C-reactive protein, and abdominal pain [6, 33], and require further evaluation to detect EJAL. While several researchers have established classifications based on the degree of EJAL, there is currently no universally accepted classification [7, 56, 57]. However, Clavien et al. introduced an innovative system for grading complications based on the type of therapy required, called the Clavien–Dindo classification [58]. This classification uses objective criteria, providing the same results regardless of the subjectivity of the observers. The Clavien–Dindo classification is used worldwide and considered to be the most reliable classification system for complications, including EJAL [30, 59, 60].
Contrast swallow
Contrast swallow is performed routinely before resuming oral intake after upper gastrointestinal surgery because it is easy and inexpensive; however, its diagnostic sensitivity for anastomotic leakage is low [10, 61]. In a prospective study [11], of 76 patients who underwent total gastrectomy and a stapled EJ anastomosis, contrast swallow was done on postoperative days 5 and 9. Eight patients suffered EJAL, which developed before postoperative day 5 in 7, and contrast swallow gave false negative results in two of five patients. In another study, Tonouchi et al [3] reported that anastomotic leakage was diagnosed by contrast swallow in only 53% of the affected patients. The majority needed two or more contrast swallow tests before diagnosis, with only 12.5% successfully diagnosed at the first examination. Although routine contrast swallow is not recommended for diagnosis, the value of this test lies in the fact that it provides information on the location and extent of leakage. It can assist in selecting appropriate treatment and is useful for the follow-up of EJAL treatment.
Endoscopy
Endoscopy can be used to diagnose EJAL in patients with clinical evidence of leakage with nearly 100% sensitivity and specificity [62]. Moreover, Endoscopy can be used to treat EJAL by the placement of self-expanding metallic stents or the insertion of a nasojejunal feeding tube distal to the dehiscence of the anastomosis or by the insertion of drainage tube into the abscess cavity through the leak hole. Despite concerns that endoscopy may worsen a pre-existent EJAL, endoscopy is well tolerated and safe when performed by experienced endoscopists or surgeons [10, 62,63,64]. Hogan et al [62] compared routine follow-up with contrast swallow, CT, and endoscopy in a series of 38 patients with esophagogastric resection 1 week after surgery. In the eight patients with clinically apparent leaks, contrast swallow and CT each missed one leak that was subsequently confirmed by endoscopy. Endoscopy had a sensitivity and specificity of 100%, but there were incongruous radiological findings, and only two patients underwent endoscopy. As there are concerns about whether endoscopy can detect minor leaks, additional study of the reliability of endoscopy is needed.
Computed tomography
The presence of perianastomotic air and/or fluid on CT evaluation strongly suggests EJAL [62]. An elevated white blood count or C-reactive protein level is frequently associated with EJAL [6], but they are nonspecific signs. CT can detect not only EJAL but also other morbidities, such as intra-abdominal abscesses, ileus, or pneumonia, and should be performed as soon as any suspicious symptoms appear. CT also shows the extent of abscesses and their accessibility to a percutaneous drain, both of which are important for treatment.
In summary, considering that most patients with EJAL experience clinical signs such as pyrexia, and because the contrast swallow test has low diagnostic sensitivity for leakage, routine postoperative contrast swallow is not recommended for early leakage detection. Although endoscopy is highly sensitive and specific, it is not routinely recommended because of the costs and effort. If EJAL is suspected based on clinical signs, CT should be performed first, followed by a contrast swallow and/or endoscopy if needed.
Treatment
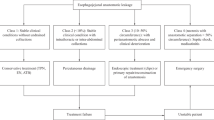
The treatment of EJAL following total gastrectomy includes the following: conservative treatment (with or without percutaneous drainage), endoscopic treatment, and surgery. A standard protocol for the treatment of EJAL has not been established because there is a lack of evidence from randomized controlled trials [7]. Proposed management algorithms [7, 65, 66] include surgical treatment if there is sepsis involving one organ or multi-organ failure, signs of diffuse peritonitis, or jejunal loop ischemia. Otherwise, conservative treatment, including fasting, antibiotics, nutritional support, and insertion of a nasojejunal tube, is recommended. If there is a perianastomotic collection, radiologically guided or endoscopic drainage with or without endoscopic management, such as glue, clips, or stents, should be considered. If conservative treatment has failed, surgery should be performed without delay. Figure 1 shows our recommended treatment algorithm.
Conservative treatment
Conservative treatment with or without percutaneous drainage is the most widely accepted treatment of EJAL, performed in 39–84.2% of patients [4,5,6, 15, 16, 33]. At the very least, fasting and antibiotics are necessary. Nutritional support is preferably administered via the enteral route, downstream of the leakage site, with a feeding jejunostomy or a nasojejunal feeding tube placed radiologically or endoscopically. If the enteral route is not an option, parenteral nutrition can be considered. A CT scan should be performed before initiating conservative treatment. If there is only a small volume of fluid surrounding the anastomosis, careful surveillance without percutaneous drainage is possible. If a moderate volume of fluid is detected, radiologically guided drainage should be considered. If the fluid has collected behind other organs, such as the colon or in the mediastinal space, the successful insertion of a drain is difficult, and its success depends on the radiological and surgical techniques used. It is important to position the drainage tube near the anastomosis when the gastrectomy is performed, if there is a concern of leakage, such as suspicion of incomplete formation of the circular anastomosis.
Endoscopic therapy
Several EJAL case series of patients treated with endoscopy and the placement of self-expanding metal stents originally developed for the palliative treatment of advanced gastrointestinal cancer have been reported [67,68,69,70,71]. Feith et al [71] reported that complete healing was achieved by stent implantation in 70% of 115 patients with anastomotic leakage following esophagogastrectomy or gastrectomy. The most frequent drawback was stent migration, which occurred in up to 61% of patients. If this occurs, a second procedure is needed to remove the stent, which may cause additional complications [72]. Repeated stent placement, stent-related pain, and symptomatic stricture after stent removal have all been reported [71, 73]. Non-stent endoscopic treatments, including endoscopic clipping, glue injection, and detachable snares, have been reported in some case series [74,75,76]. A comparison of non-stent treatment and self-expanding metallic stents by Shim et al [77] found no complications associated with the non-stent treatment, but successful sealing on the first attempt was significantly lower than that achieved with stent treatment (28.6% vs. 80.0%, P = 0.036).
The indications for endoscopic treatment are limited by the size of the dehiscence (< 2 cm or < 70% of the circumference) and the interval from perforation to intervention [68, 70, 77, 78]. The over-the-scope-clip system (OTSC), an innovative non-stent endoscopic therapy, can be used to close large gastric or colonic perforations following endoscopic mucosal resection or anastomotic leakage [79,80,81,82]. Openings up to 30 mm can be repaired with a closing force of 8–9 N, which is far stronger than that achieved with hemostatic clips [81]. A systematic review by Weiland et al. [80] reported successful procedures in 80–100% of patients, with durable clinical success in 57–100%; however, the success rate of OTSC is inversely associated with the time from the clinical diagnosis of the leakage to the application of the clip, ranging from 100% at 1 week to < 60% with time [81, 82]. Endoscopic vacuum therapy (EVT) was recently introduced in Europe as a treatment for upper gastrointestinal perforation and anastomotic leakage. In EVT, continuous negative pressure decreases bacterial contamination, secretion, and local edema, and promotes perfusion and the formation of granulation tissue. Briefly, following endoscopic rinsing, a sponge containing a drain is placed in the cavity of the leak, which removes the exudate and maintains negative pressure. The sponge is changed every 3 days until the leakage resolves. Small-case series of patients treated with EVT [83,84,85,86,87] include a comparison by Hwang et al. of EVT and endoscopic stenting in 18 patients with postsurgical gastroesophageal leakage [88]. They reported a better clinical success rate of 100% in the EVT group vs. 64% in the stent group, although the difference did not reach significance. Complications occurred in none of the EVT patients vs. 54.5% of the stent patients. Thus, EVT was more effective and safer than stenting for treating gastroesophageal leakage.
In summary, several endoscopic treatment methods have been reported. The self-expanding metal stent is the most common procedure, but it has several drawbacks, and can cause irreversible complications. Therefore, it should only be used when conservative treatment fails and the patient’s poor condition contraindicates surgery. Other new methods have been reported as safe and effective; however, as only small-scale case series are available, the optimal strategy for endoscopic treatment is still unclear.
Surgical treatment
Surgical treatment involves drainage and repair or refashioning of the anastomosis and has been reported as necessary following gastrectomy in 10–61% of patients [4,5,6,7,8, 15, 16, 33, 89]. In a recent systematic review, surgical treatment for EJAL was performed in 23.7% of patients [55]. Mortality following surgery for EJAL was much higher than that after other treatments: 62.96% after surgery, 28.6% after endoscopic treatment, and 18.2% with conservative treatment. It must be considered that surgery is generally performed on patients who are likely to be in a critical condition, as surgery is not recommended as the first choice, but rather for patients who are gravely ill, if radiologically guided insertion of a drainage tube is not possible, or when conservative treatment has failed.
Conclusions
EJAL is a serious and often life-threatening complication of total and proximal gastrectomy. Meticulous surgical techniques and experience with anastomotic devices are the key to its prevention. Surgeons must be familiar with the risk factors, and early diagnosis is essential to prevent EJAL-related death. Careful monitoring and appropriate evaluation of patients with suspicious symptoms are essential. Conservative treatment with appropriate drainage and nutritional support is currently the treatment of choice. Endoscopic treatment appears to be safe and effective but needs further investigation. Surgical treatment is associated with high mortality, but is appropriate for patients with severe sepsis and if conservative treatment fails to prevent death from suboptimal EJAL management.
References
Japanese Gastric Cancer A. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20(1):1–19.
Isozaki H, Okajima K, Ichinona T, Hara H, Fujii K, Nomura E. Risk factors of esophagojejunal anastomotic leakage after total gastrectomy for gastric cancer. Hepatogastroenterology. 1997;44(17):1509–12.
Tonouchi H, Mohri Y, Tanaka K, Ohi M, Kobayashi M, Yamakado K, et al. Diagnostic sensitivity of contrast swallow for leakage after gastric resection. World J Surg. 2007;31(1):128–31.
Lang H, Piso P, Stukenborg C, Raab R, Jahne J. Management and results of proximal anastomotic leaks in a series of 1114 total gastrectomies for gastric carcinoma. Eur J Surg Oncol. 2000;26(2):168–71.
Sauvanet A, Mariette C, Thomas P, Lozac’h P, Segol P, Tiret E, et al. Mortality and morbidity after resection for adenocarcinoma of the gastroesophageal junction: predictive factors. J Am Coll Surg. 2005;201(2):253–62.
Migita K, Takayama T, Matsumoto S, Wakatsuki K, Enomoto K, Tanaka T, et al. Risk factors for esophagojejunal anastomotic leakage after elective gastrectomy for gastric cancer. J Gastrointest Surg. 2012;16(9):1659–65.
Carboni F, Valle M, Federici O, Levi Sandri GB, Camperchioli I, Lapenta R, et al. Esophagojejunal anastomosis leakage after total gastrectomy for esophagogastric junction adenocarcinoma: options of treatment. J Gastrointest Oncol. 2016;7(4):515–22.
Deguchi Y, Fukagawa T, Morita S, Ohashi M, Saka M, Katai H. Identification of risk factors for esophagojejunal anastomotic leakage after gastric surgery. World J Surg. 2012;36(7):1617–22.
Schietroma M, Cecilia EM, Carlei F, Sista F, De Santis G, Piccione F, et al. Prevention of anastomotic leakage after total gastrectomy with perioperative supplemental oxygen administration: a prospective randomized, double-blind, controlled, single-center trial. Ann Surg Oncol. 2013;20(5):1584–90.
El-Sourani N, Bruns H, Troja A, Raab HR, Antolovic D. Routine use of contrast swallow after total gastrectomy and esophagectomy: is it justified? Pol J Radiol. 2017;82:170–3.
Lamb PJ, Griffin SM, Chandrashekar MV, Richardson DL, Karat D, Hayes N. Prospective study of routine contrast radiology after total gastrectomy. Br J Surg. 2004;91(8):1015–9.
Nomura S, Sasako M, Katai H, Sano T, Maruyama K. Decreasing complication rates with stapled esophagojejunostomy following a learning curve. Gastric Cancer. 2000;3(2):97–101.
Watanabe M, Miyata H, Gotoh M, Baba H, Kimura W, Tomita N, et al. Total gastrectomy risk model: data from 20,011 Japanese patients in a nationwide internet-based database. Ann Surg. 2014;260(6):1034–9.
Yoo HM, Lee HH, Shim JH, Jeon HM, Park CH, Song KY. Negative impact of leakage on survival of patients undergoing curative resection for advanced gastric cancer. J Surg Oncol. 2011;104(7):734–40.
Sierzega M, Kolodziejczyk P, Kulig J, Polish Gastric Cancer Study G. Impact of anastomotic leakage on long-term survival after total gastrectomy for carcinoma of the stomach. Br J Surg. 2010;97(7):1035–42.
Kanaji S, Ohyama M, Yasuda T, Sendo H, Suzuki S, Kawasaki K, et al. Can the intraoperative leak test prevent postoperative leakage of esophagojejunal anastomosis after total gastrectomy? Surg Today. 2016;46(7):815–20.
Nishikawa K, Yanaga K, Kashiwagi H, Hanyuu N, Iwabuchi S. Significance of intraoperative endoscopy in total gastrectomy for gastric cancer. Surg Endosc. 2010;24(10):2633–6.
Tokunaga M, Tanizawa Y, Bando E, Kawamura T, Terashima M. Poor survival rate in patients with postoperative intra-abdominal infectious complications following curative gastrectomy for gastric cancer. Ann Surg Oncol. 2013;20(5):1575–83.
Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, et al. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet. 1995;345(8952):745–8.
Cuschieri A, Fayers P, Fielding J, Craven J, Bancewicz J, Joypaul V, et al. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial. Surg Coop Group Lancet. 1996;347(9007):995–9.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108.
Takeuchi M, Ishii K, Seki H, Yasui N, Sakata M, Shimada A, et al. Excessive visceral fat area as a risk factor for early postoperative complications of total gastrectomy for gastric cancer: a retrospective cohort study. BMC Surg. 2016;16(1):54.
Tokunaga M, Hiki N, Fukunaga T, Ogura T, Miyata S, Yamaguchi T. Effect of individual fat areas on early surgical outcomes after open gastrectomy for gastric cancer. Br J Surg. 2009;96(5):496–500.
Sugisawa N, Tokunaga M, Tanizawa Y, Bando E, Kawamura T, Terashima M. Intra-abdominal infectious complications following gastrectomy in patients with excessive visceral fat. Gastric Cancer. 2012;15(2):206–12.
Cancer Registry and Statistics. Cancer Infromation Service, National Cancer Center, Japan. 2016.
Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994;4(2):146–8.
Uyama I, Sugioka A, Fujita J, Komori Y, Matsui H, Hasumi A. Laparoscopic total gastrectomy with distal pancreatosplenectomy and D2 lymphadenectomy for advanced gastric cancer. Gastric Cancer. 1999;2(4):230–4.
Kodera Y, Yoshida K, Kumamaru H, Kakeji Y, Hiki N, Etoh T, et al. Introducing laparoscopic total gastrectomy for gastric cancer in general practice: a retrospective cohort study based on a nationwide registry database in Japan. Gastric Cancer 2018.
Katai H, Mizusawa J, Katayama H, Kunisaki C, Sakuramoto S, Inaki N, et al. Single-arm confirmatory trial of laparoscopy assisted total or proximal gastrectomy with nodal dissection for clinical stage I gastric cancer: Japan Clinical Oncology Group study JCOG1401. J Clin Oncol 2018;36 (suppl; abstr 4028).
Hyung WJ, Yang HK, Han SU, Lee YJ, Park JM, Kim JJ, et al. A feasibility study of laparoscopic total gastrectomy for clinical stage I gastric cancer: a prospective multi-center phase II clinical trial, KLASS 03. Gastric Cancer 2018.
Esrig BC, Frazee L, Stephenson SF, Polk HC Jr, Fulton RL, Jones CE. The predisposition to infection following hemorrhagic shock. Surg Gynecol Obstet. 1977;144(6):915–7.
Marano L, Porfidia R, Pezzella M, Grassia M, Petrillo M, Esposito G, et al. Clinical and immunological impact of early postoperative enteral immunonutrition after total gastrectomy in gastric cancer patients: a prospective randomized study. Ann Surg Oncol. 2013;20(12):3912–8.
Tu RH, Lin JX, Zheng CH, Li P, Xie JW, Wang JB, et al. Development of a nomogram for predicting the risk of anastomotic leakage after a gastrectomy for gastric cancer. Eur J Surg Oncol. 2017;43(2):485–92.
Kikuchi H, Miyata H, Konno H, Kamiya K, Tomotaki A, Gotoh M, et al. Development and external validation of preoperative risk models for operative morbidities after total gastrectomy using a Japanese web-based nationwide registry. Gastric Cancer. 2017;20(6):987–97.
Sato T, Aoyama T, Hayashi T, Segami K, Kawabe T, Fujikawa H, et al. Impact of preoperative hand grip strength on morbidity following gastric cancer surgery. Gastric Cancer. 2016;19(3):1008–15.
Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE. Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer. 2012;107(6):931–6.
Peng PD, van Vledder MG, Tsai S, de Jong MC, Makary M, Ng J, et al. Sarcopenia negatively impacts short-term outcomes in patients undergoing hepatic resection for colorectal liver metastasis. HPB (Oxford). 2011;13(7):439–46.
Kawamura T, Makuuchi R, Tokunaga M, Tanizawa Y, Bando E, Yasui H, et al. Long-term outcomes of gastric cancer patients with preoperative sarcopenia. Ann Surg Oncol. 2018;25(6):1625–32.
Yang Z, Zhou X, Ma B, Xing Y, Jiang X, Wang Z. Predictive value of preoperative sarcopenia in patients with gastric cancer: a meta-analysis and systematic review. J Gastrointest Surg 2018.
Hunt TK, Zederfeldt BH, Goldstick TK, Conolly WB. Tissue oxygen tensions during controlled hemorrhage. Surg Forum. 1967;18:3–4.
Hooton TM, Haley RW, Culver DH, White JW, Morgan WM, Carroll RJ. The joint associations of multiple risk factors with the occurrence of nosocomial infection. Am J Med. 1981;70(4):960–70.
Hartmann M, Jonsson K, Zederfeldt B. Effect of tissue perfusion and oxygenation on accumulation of collagen in healing wounds. Randomized study in patients after major abdominal operations. Eur J Surg. 1992;158(10):521–6.
Inokuchi M, Otsuki S, Ogawa N, Tanioka T, Okuno K, Gokita K, et al. Postoperative complications of laparoscopic total gastrectomy versus open total gastrectomy for gastric cancer in a meta-analysis of high-quality case-controlled studies. Gastroenterol Res Pract. 2016;2016:2617903.
Etoh T, Honda M, Kumamaru H, Miyata H, Yoshida K, Kodera Y, et al. Morbidity and mortality from a propensity score-matched, prospective cohort study of laparoscopic versus open total gastrectomy for gastric cancer: data from a nationwide web-based database. Surg Endosc 2017.
Inaba K, Satoh S, Ishida Y, Taniguchi K, Isogaki J, Kanaya S, et al. Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg. 2010;211(6):e25-9.
Usui S, Nagai K, Hiranuma S, Takiguchi N, Matsumoto A, Sanada K. Laparoscopy-assisted esophagoenteral anastomosis using endoscopic purse-string suture instrument “Endo-PSI (II)” and circular stapler. Gastric Cancer. 2008;11(4):233–7.
Jeong O, Park YK. Intracorporeal circular stapling esophagojejunostomy using the transorally inserted anvil (OrVil) after laparoscopic total gastrectomy. Surg Endosc. 2009;23(11):2624–30.
Wang H, Hao Q, Wang M, Feng M, Wang F, Kang X, et al. Esophagojejunostomy after laparoscopic total gastrectomy by OrVil or hemi-double stapling technique. World J Gastroenterol. 2015;21(29):8943–51.
Moisan F, Norero E, Slako M, Varas J, Palominos G, Crovari F, et al. Completely laparoscopic versus open gastrectomy for early and advanced gastric cancer: a matched cohort study. Surg Endosc. 2012;26(3):661–72.
Umemura A, Koeda K, Sasaki A, Fujiwara H, Kimura Y, Iwaya T, et al. Totally laparoscopic total gastrectomy for gastric cancer: literature review and comparison of the procedure of esophagojejunostomy. Asian J Surg. 2015;38(2):102–12.
Mariette C, De Botton ML, Piessen G. Surgery in esophageal and gastric cancer patients: what is the role for nutrition support in your daily practice? Ann Surg Oncol. 2012;19(7):2128–34.
Waitzberg DL, Saito H, Plank LD, Jamieson GG, Jagannath P, Hwang TL, et al. Postsurgical infections are reduced with specialized nutrition support. World J Surg. 2006;30(8):1592–604.
Valenzuela-Salazar C, Rojano-Rodriguez ME, Romero-Loera S, Trejo-Avila ME, Banuelos-Mancilla J, Delano-Alonso R, et al. Intraoperative endoscopy prevents technical defect related leaks in laparoscopic Roux-en-Y gastric bypass: a randomized control trial. Int J Surg. 2018;50:17–21.
Haverkamp L, Ruurda JP, van Hillegersberg R. Technical feasibility of TachoSil application on esophageal anastomoses. Gastroenterol Res Pract. 2015;2015:534080.
Afaneh C, Abelson J, Schattner M, Janjigian YY, Ilson D, Yoon SS, et al. Esophageal reinforcement with an extracellular scaffold during total gastrectomy for gastric cancer. Ann Surg Oncol. 2015;22(4):1252–7.
Schuchert MJ, Abbas G, Nason KS, Pennathur A, Awais O, Santana M, et al. Impact of anastomotic leak on outcomes after transhiatal esophagectomy. Surgery. 2010;148(4):831–8 (discussion 8-40).
Bruce J, Krukowski ZH, Al-Khairy G, Russell EM, Park KG. Systematic review of the definition and measurement of anastomotic leak after gastrointestinal surgery. Br J Surg. 2001;88(9):1157–68.
Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111(5):518–26.
Tokunaga M, Kondo J, Tanizawa Y, Bando E, Kawamura T, Terashima M. Postoperative intra-abdominal complications assessed by the Clavien–Dindo classification following open and laparoscopy-assisted distal gastrectomy for early gastric cancer. J Gastrointest Surg. 2012;16(10):1854–9.
Katai H, Mizusawa J, Katayama H, Takagi M, Yoshikawa T, Fukagawa T, et al. Short-term surgical outcomes from a phase III study of laparoscopy-assisted versus open distal gastrectomy with nodal dissection for clinical stage IA/IB gastric cancer: Japan Clinical Oncology Group Study JCOG0912. Gastric Cancer. 2017;20(4):699–708.
Aday U, Gundes E, Ciyiltepe H, Cetin DA, Gulmez S, Senger AS, et al. Examination of anastomotic leak with aqueous contrast swallow after total gastrectomy: should it be carried out routinely? Contemp Oncol (Pozn). 2017;21(3):224–7.
Hogan BA, Winter DC, Broe D, Broe P, Lee MJ. Prospective trial comparing contrast swallow, computed tomography and endoscopy to identify anastomotic leak following oesophagogastric surgery. Surg Endosc. 2008;22(3):767–71.
Nederlof N, de Jonge J, de Vringer T, Tran TC, Spaander MC, Tilanus HW, et al. Does routine endoscopy or contrast swallow study after esophagectomy and gastric tube reconstruction change patient management? J Gastrointest Surg. 2017;21(2):251–8.
Page RD, Asmat A, McShane J, Russell GN, Pennefather SH. Routine endoscopy to detect anastomotic leakage after esophagectomy. Ann Thorac Surg. 2013;95(1):292–8.
Girard E, Messager M, Sauvanet A, Benoist S, Piessen G, Mabrut JY, et al. Anastomotic leakage after gastrointestinal surgery: diagnosis and management. J Visc Surg. 2014;151(6):441–50.
Messager M, Warlaumont M, Renaud F, Marin H, Branche J, Piessen G, et al. Recent improvements in the management of esophageal anastomotic leak after surgery for cancer. Eur J Surg Oncol. 2017;43(2):258–69.
Aryaie AH, Singer JL, Fayezizadeh M, Lash J, Marks JM. Efficacy of endoscopic management of leak after foregut surgery with endoscopic covered self-expanding metal stents (SEMS). Surg Endosc. 2017;31(2):612–7.
Hoeppner J, Kulemann B, Seifert G, Marjanovic G, Fischer A, Hopt UT, et al. Covered self-expanding stent treatment for anastomotic leakage: outcomes in esophagogastric and esophagojejunal anastomoses. Surg Endosc. 2014;28(5):1703–11.
Roy-Choudhury SH, Nicholson AA, Wedgwood KR, Mannion RA, Sedman PC, Royston CM, et al. Symptomatic malignant gastroesophageal anastomotic leak: management with covered metallic esophageal stents. AJR Am J Roentgenol. 2001;176(1):161–5.
Schubert D, Scheidbach H, Kuhn R, Wex C, Weiss G, Eder F, et al. Endoscopic treatment of thoracic esophageal anastomotic leaks by using silicone-covered, self-expanding polyester stents. Gastrointest Endosc. 2005;61(7):891–6.
Feith M, Gillen S, Schuster T, Theisen J, Friess H, Gertler R. Healing occurs in most patients that receive endoscopic stents for anastomotic leakage; dislocation remains a problem. Clin Gastroenterol Hepatol. 2011;9(3):202–10.
Aurello P, Magistri P, D’Angelo F, Valabrega S, Sirimarco D, Tierno SM, et al. Treatment of esophagojejunal anastomosis leakage: a systematic review from the last two decades. Am Surg. 2015;81(5):450–3.
Fernandez A, Vila JJ, Vazquez S, Gonzalez-Portela C, de la Iglesia M, Lozano M, et al. Self-expanding plastic stents for the treatment of post-operative esophago-jejuno anastomosis leak. A case series study. Rev Esp Enferm Dig. 2010;102(12):704–10.
Tekinbas C, Erol MM, Akdogan R, Turkyilmaz S, Aslan M. Treatment of anastomotic leaks after esophagectomy with endoscopic hemoclips. J Thorac Cardiovasc Surg. 2009;137(3):766–7.
Lee S, Ahn JY, Jung HY, Lee JH, Choi KS, Kim DH, et al. Clinical outcomes of postoperative upper gastrointestinal leakage according to treatment modality. Dig Dis Sci. 2016;61(2):523–32.
Lee S, Ahn JY, Jung HY, Lee JH, Choi KS, Kim DH, et al. Clinical outcomes of endoscopic and surgical management for postoperative upper gastrointestinal leakage. Surg Endosc. 2013;27(11):4232–40.
Shim CN, Kim HI, Hyung WJ, Noh SH, Song MK, Kang DR, et al. Self-expanding metal stents or nonstent endoscopic therapy: which is better for anastomotic leaks after total gastrectomy? Surg Endosc. 2014;28(3):833–40.
Kim YJ, Shin SK, Lee HJ, Chung HS, Lee YC, Park JC, et al. Endoscopic management of anastomotic leakage after gastrectomy for gastric cancer: how efficacious is it? Scand J Gastroenterol. 2013;48(1):111–8.
Galizia G, Napolitano V, Castellano P, Pinto M, Zamboli A, Schettino P, et al. The Over-The-Scope-Clip (OTSC) system is effective in the treatment of chronic esophagojejunal anastomotic leakage. J Gastrointest Surg. 2012;16(8):1585–9.
Weiland T, Fehlker M, Gottwald T, Schurr MO. Performance of the OTSC System in the endoscopic closure of iatrogenic gastrointestinal perforations: a systematic review. Surg Endosc. 2013;27(7):2258–74.
Albert JG, Friedrich-Rust M, Woeste G, Strey C, Bechstein WO, Zeuzem S, et al. Benefit of a clipping device in use in intestinal bleeding and intestinal leakage. Gastrointest Endosc. 2011;74(2):389–97.
Kirschniak A, Subotova N, Zieker D, Konigsrainer A, Kratt T. The Over-The-Scope Clip (OTSC) for the treatment of gastrointestinal bleeding, perforations, and fistulas. Surg Endosc. 2011;25(9):2901–5.
Laukoetter M, Mennigen R, Neumann P, Dhayat S, Horst G, Palmes D, et al. Successful closure of defects in the upper gastrointestinal tract by endoscopic vacuum therapy (EVT): a prospective cohort study. Surg Endosc. 2017;31(6):2687–96.
Wedemeyer J, Schneider A, Manns MP, Jackobs S. Endoscopic vacuum-assisted closure of upper intestinal anastomotic leaks. Gastrointest Endosc. 2008;67(4):708–11.
Loske G, Schorsch T, Muller C. Endoscopic vacuum sponge therapy for esophageal defects. Surg Endosc. 2010;24(10):2531–5.
Wedemeyer J, Brangewitz M, Kubicka S, Jackobs S, Winkler M, Neipp M, et al. Management of major postsurgical gastroesophageal intrathoracic leaks with an endoscopic vacuum-assisted closure system. Gastrointest Endosc. 2010;71(2):382–6.
Kuehn F, Loske G, Schiffmann L, Gock M, Klar E. Endoscopic vacuum therapy for various defects of the upper gastrointestinal tract. Surg Endosc. 2017;31(9):3449–58.
Hwang J, Jeong Y, Park Y, Yoon H, Shin C, Kim N, et al. Comparison of endoscopic vacuum therapy and endoscopic stent implantation with self-expandable metal stent in treating postsurgical gastroesophageal leakage. Medicine. 2016;95(16):e3416-e.
Schardey HM, Joosten U, Finke U, Staubach KH, Schauer R, Heiss A, et al. The prevention of anastomotic leakage after total gastrectomy with local decontamination. A prospective, randomized, double-blind, placebo-controlled multicenter trial. Ann Surg. 1997;225(2):172–80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Rie Makuuchi and the co-authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Makuuchi, R., Irino, T., Tanizawa, Y. et al. Esophagojejunal anastomotic leakage following gastrectomy for gastric cancer. Surg Today 49, 187–196 (2019). https://doi.org/10.1007/s00595-018-1726-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-018-1726-8