Abstract
Gastric cancer surgery has evolved considerably over the past years, with substantial improvement on outcomes. Meanwhile, esophagojejunal anastomotic fistula (EJF) continues to impair postoperative results. This study aimed to assess EJF regarding its incidence, risk factors, management and the impact on overall survival. We retrospectively analyzed 258 consecutive patients who underwent total or completion gastrectomy for GC from 2009 and 2017. Clinicopathological characteristics analysis was performed comparing patients who developed EJF with patients with other clinical or surgical complications, as well as patients without any postoperative complications. Fifteen (5.8%) patients had EJF and 81 (31.4%) had other complications (including other surgical fistulas). The median time of EJF diagnosis was on the eighth postoperative day (range 3–76). Completion gastrectomy (p = 0.048) and longer hospital stay (p < 0.001) were associated with the occurrence of EJF. The surgical mortality of patients with EJF was higher than in non-EJF patients (26.7% vs. 4.5%; p < 0.001). Nine patients were treated conservatively and six required surgery. The mortality rate of EJF was 11.1% and 50% in patients who underwent conservative and surgical treatment, respectively. Patients with other complications and patients with EJF had worse survival compared to patients without any complication (p = 0.004 and p = 0.013, respectively). Completion gastrectomy is the main risk factor for EJF occurrence. Still, EJF is associated with high postoperative mortality, longer hospital stay and has a negative impact on long-term survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgery remains the cornerstone regarding gastric cancer (GC) treatment, mostly in advanced cases. The improvement in surgical techniques and the development of new technologies over the past years have afforded better outcomes in gastric cancer surgery [1]. In spite of these advances, some postoperative (PO) complications such as esophagojejunal anastomotic fistula (EJF) after total, proximal or completion gastrectomy continue to occur, leading to a longer hospital stay, increased morbidity and higher costs. Yet, it delays or nullifies the possibility of adjuvant therapy, worsening quality of life and survival [2].
Several factors have been associated with its occurrence. For instance, patient conditions such as age, malnutrition and multiple clinical conditions as well as intraoperative technical errors during the esophagojejunostomy are reported to be possible risk factors for EJF [3].
The knowledge regarding the predictive factors may be important to decrease its incidence, to provide early diagnosis and to improve surgical outcomes. Therefore, the aim of this study was to assess the incidence and characteristics of the patients who developed EJF after gastrectomy for GC, as well as their long-term outcomes.
Patients and methods
We retrospectively reviewed all consecutive patients submitted to gastrectomy due to gastric adenocarcinoma from 2009 to 2017 at the Cancer Institute, Medical School, University of São Paulo. All clinical data were extracted from our prospective database. The inclusion criteria were patients who underwent total gastrectomy or completion gastrectomy for gastric stump neoplasia. Patients with a histological type different from adenocarcinoma and emergency surgeries were excluded from the analysis.
Patients were staged preoperatively through abdominal and pelvis computed tomography, endoscopy and serum tumor markers. TNM staging was performed according to the TNM 7th edition [4].
Clinical characteristics evaluated included the American Society of Anesthesiologists (ASA) classification [5], Charlson Comorbidity Index (CCI) [6], Neutrophil-to-lymphocyte ratio (NLR) and laboratory tests. CCI was considered without the inclusion of GC neoplasm as comorbidity. Patients who lost more than 10% of body weight in the past 6 months received nutritional support through enteral or parenteral diet for at least 10 days prior to surgery.
Surgical complications were graded according to Clavien–Dindo’s classification. Major complications were considered Clavien III–V [7]. The hospitalization period and the number of retrieved lymph nodes were also evaluated. Surgical mortality was considered when it occurred within 30 days after surgery or during hospital stay after the procedure.
The PO follow-up was performed on a quarterly basis in the first year and every 6 months in the following years. Follow-up tests for relapse detection were performed based on the presence of symptoms. The absence in consultations for more than 12 months was considered as loss of follow-up.
All cases were operated in a high-volume center by surgeons with extensive experience in the surgical management of GC. The surgical technique, extension of resection and dissected lymph node chains followed the recommendations of the Japanese Gastric Cancer Association guidelines and the Brazilian Gastric Cancer Association guidelines [8, 9]. In all cases of open surgery, the esophagojejunal anastomosis (EJA) was performed with an end-to-side circular stapler (either Autosuture™DST, US Surgical, Norwalk, CT or Ethicon endo surgery, Inc., Somerville, NJ). The size of the stapling device was chosen according to patients’ characteristics. The 25 mm device was used in the majority of patients. Nevertheless, larger (28–29 mm) and smaller (21 mm) staplers were used whenever necessary. The esophageal and jejunal resected margins (doughnut rings) were evaluated for possible anastomotic failure and checked for tumor-free margins. In every case of laparoscopic surgery, the EJA was performed with a side-to-side anastomosis with endolinear stapler (either Autosuture™DST, US Surgical, Norwalk, CT or Ethicon endo surgery, Inc., Somerville, NJ) [10]. The EJA was routinely tested intraoperatively for leakage with air or through the blue-dimethylene test. Whenever positive for leak, additional stitches or re-anastomosis were done. Roux-en-Y alimentary tract reconstruction was performed in all cases. All patients received a Dobbhoff feeding tube.
Enteral feeding started at first flatus (between first and third PO day) and was maintained until the patients accepted well the oral diet. The integrity of EJA was routinely tested in all patients before oral diet was initiated. In asymptomatic patients, an oral blue-dimethylene test was routinely performed between the seventh and tenth PO day. In suspected patients with leakage (fever, abdominal pain, abnormal drain output, sustained tachycardia, leukocytosis or elevated reactive C protein) a radiologic study with water-soluble contrast-medium was added to the oral blue dye test. The abdominal drain was removed only in asymptomatic patients and after the patients had good acceptance of oral diet.
EJF was defined as the presence of contrast leakage during the radiologic examination; through an upper endoscopy with direct visualization of the fistula’s orifice or the abdominal drain (Fig. 1); abnormal drain output (saliva, gastrointestinal content or blue dye); through re-laparotomy. Additional tests such as computer tomography were carried out to assess leakage-related complications. The “other surgical fistulas” are represented in Supplementary file 1 and are defined as fistulas other than EJF.
The study was approved by the hospital ethics committee (NP993/16) and registered in the international research registry database (http://www.researchregistry.com).
Statistical analysis
Descriptive statistics included frequencies with percentages for nominal variables and mean with standard deviation for continuous variables. The Chi square tests were used for categorical variables and ANOVA or t test for continuous variables. The factors associated with fistula occurrence were determined by binary logistic regression analysis by the backward elimination with a stay level of 0.20.
The overall survival (OS) was estimated using the Kaplan–Meier method and the differences in survival were examined using the Log rank test. To determine factors associated with better OS, univariate and multivariate Cox proportional hazard regression models were used. Covariates with p values less than 0.05 were selected for the multivariate model. The survival time in months was calculated from the date of surgery until the date of death/recurrence. Patients alive were censored at the date of the last contact. All tests were two-sided and p < 0.05 was considered statistically significant. The analysis was performed using SPSS software, version 18.0 (SPSS Inc, Chicago, IL).
Results
Nine hundred and sixty-four patients underwent surgical treatment for GC during the period of study. A total of 258 patients underwent total or completion gastrectomy and were enrolled in the study. Of these, 15 (5.8%) patients had EJF, 81 (31.4%) had other complications (including other surgical fistulas) and 162 (62.8%) patients did not have any PO complications. They were labeled as “no complication” group and were used as the control group (NC). Supplementary file 1 represents all other complications.
The mean age of the total population was 62.3 years (range 25–94) with a male preponderance (69.7% vs. 30.3%). Most tumors were located at the distal or middle part of the stomach (65.9%). Total gastrectomy was performed in 208 (80.6%) and completion gastrectomy in 50 (19.4%). Surgery with curative intent was performed in 230 (89.1%) patients and 168 (65.1%) patients underwent D2 lymphadenectomy. The median of lymph nodes retrieved was 39 (range 21–114). Forty-four (17%) patients received neoadjuvant therapy.
Surgical and clinicopathological characteristics of patients with EJF, other complications (OC) and NC are summarized in Table 1. Gender, Charlson index, ASA class and type of surgery were similar between the groups. Patients with EJF were older compared with the NC group (p = 0.042).
Completion gastrectomy was more frequent in the EJF group, reaching statistical significance when compared to all non-EJF patients (which corresponded to OC + NC cases, data not shown) (p = 0.048). The extension of lymphadenectomy, type of approach, histological type, pT status, pN status and tumor final stage were not related to EJF occurrence.
Surgical outcomes
The median time for EJF diagnosis was on the eighth PO day (range 3–76). Major complications occurred in 28 (34.6%) patients in the OC group and 12 (80%) patients in the EJF group (p = 0.001). Table 1 represents the 30- and 90-day mortality. Surgical mortality was higher in EJF patients than in all non-EJF patients (26.7% vs. 4.5%, p < 0.001).
Patients with EJF had a longer hospital stay (36.7 days, ± 14.7, p < 0.001) when compared to other groups (NC = 11.6 days, ± 2.8; OC = 20.6 days, ± 9.4). Adjuvant therapy was more common in the NC and OC group when compared with EJF patients (54.9, 38.3 and 20%, respectively) (p < 0.004).
Table 2 shows the independent risk factors associated with the EJF onset. The multivariate analysis identified type of gastric resection (completion gastrectomy) as an independent risk factor for EJF [OR 3.34 (IC95% 1.06–10.57); p = 0.040].
Management details and pathologic data of EJF cases are presented in Table 3. Nine patients were treated conservatively and six required surgery. Thoracoscopy was performed in two patients and laparotomy was needed in four cases. Extensive lavage of the abdominal cavity followed by drainage, large spectrum intravenous antibiotics and antifungal treatment were performed. Stitches at the fistula site were attempted in all laparotomy cases. The mortality rate of EJF was 11.1% and 50% in patients who underwent conservative and surgical treatment, respectively.
Survival analysis
The median follow-up of the study population was 25.5 months (range 1–102). Ninety-nine patients relapsed and 101 died. The disease-free survival (DFS) and OS rate for the entire cohort was 61.6% and 60.9%, respectively. Survival of patients with NC, OC and EJF is represented in Fig. 2. Patients with OC and EJF had worse survival than patients without any complication (p = 0.004 and p = 0.013, respectively).
In the Cox proportional hazard model, EJF and OC were independent predictors associated to poor survival [HR 2.40 (IC95% 1.16–4.94); p = 0.018 and HR 2.30 (IC95% 1.48–3.59); p < 0.001], respectively. Other independent predictors of survival were ASA classification, histological type, pathological stage and adjuvant chemotherapy (Table 4).
Discussion
Esophagojejunal anastomotic leakage has been considered a major issue in GC surgery. The incidence reported ranges from 0 to 15%. According to recent studies, PO mortality may reach up to 60% [2, 11, 12]. Aurello et al. published a systematic review of 3893 patients who underwent total gastrectomy for GC. EJF occurred in 114 (2.9%) patients. The mortality rate was 26.3% and was more frequent in patients who needed reoperations [13]. In our analysis, the leakage rate was 5.8%, which is comparable to western specialized centers [14,15,16]. Eastern high-volume specialized centers in GC surgery have reported even lower rates, ranging from 0 to 2.1% [11, 12, 17]. Such complication may be ascribed to local and systemic factors. For instance, inadequate surgical technique, limited blood supply, excessive inflammatory reaction to suture material and tumor stage are local reasons for anastomotic failure [3, 18, 19]. Systemic conditions such as cardiovascular disease, age, smoking and malnutrition are likely reported to foment the onset of anastomotic leakage [20].
According to our results, completion gastrectomy was correlated with EJF when compared to total gastrectomy (p = 0.048). Still, removing the gastric remnant was an independent risk factor for such complication. This might be explained due to the complexity of the procedure caused by organs’ adhesions around the gastric remnant. In our study, patients who developed gastric stump neoplasm had been submitted to partial gastric resection due to benign diseases, with a minimum interval between the operations of 18 years. In fact, Takahashi et al. compared total gastrectomy for gastric stump carcinoma to usual total gastrectomy. The completion gastrectomy was related with longer operative time, more blood loss and, therefore, more severe PO complications [21].
The extension of lymphadenectomy (D1 vs. D2) and tumor stage have been reported as an independent risk factor for complications in GC surgery [22, 23]. In our institution, more than 70% of treated patients are diagnosed in very advanced stage disease and D2 lymphadenectomy is the standard procedure [24]. However, according to our analysis, tumor stage and the extension of lymphadenectomy were neither related to EJF development nor OC. It is important to emphasize that low rate of complications in GC surgery is related to centralization and surgeon’s experience [25,26,27]. On the other hand, age was associated with EJF when compared with NC patients (68 vs. 61.2 years; p = 0.042). Tu et al. identified age ≥ 65 years as an independent risk factor for anastomotic leakage in 1893 patients who underwent total gastrectomy for GC [OR 1.867 (IC95% 1.058–3.294); p = 0.031] [28]. Besides, it has been reported that patients’ clinical conditions such as heart disease, cirrhosis, diabetes mellitus and malnutrition are correlated with EJF. [29,30,31] In the present analysis, ASA classification and Charlson index were used to assess the impact of comorbidities on the occurrence of EJF and no association was found.
The time of EJF onset may vary. Migita et al. reported a median time for diagnosis of 7 days (range 3–16) [32]. Our data suggest that this period could be even longer. The median time of EJF diagnosis was on the eighth PO day. However, 4 patients were diagnosed after the 13th day after surgery. One of them had been discharged from the hospital for quite a while and returned to the hospital on the 76th in which the EJF was diagnosed. Low output fistulas with local block may delay the diagnosis and, in these cases, it is impossible to predict the exact day of fistula onset. Therefore, the possibility of late manifestation should be considered.
Further, our results have shown that EJF is related to a longer hospital stay. Even longer than in OC patients. This demonstrates the severity of this complication, leading to the necessity of intensive care, multidisciplinary approaches, diagnostic and therapeutic invasive procedures, reoperations and, ultimately, a significant increase in costs. Selby et al. reported that major complications were linked with tripled normalized costs following curative-intent total gastrectomy [33].
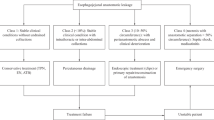
Regarding its management, early detection of EJF is the key to achieve the best end-result. Treatment measures are divided into three categories: conservative, endoscopic and surgery. Conservative treatment includes clinical support, infection control with large spectrum antibiotics and antifungal treatment, proper drainage and early nutritional support [34]. Conjointly, endoscopic treatment with stent placement has been reported as an option to treat EJF with low morbidity and mortality [35, 36]. The extension of dehiscence must be considered before the stent placement. Smaller fistulas (≤ 50% of the anastomosis) have better results than in larger dehiscence (≥ 50% area). Larger defects may reflect a major surgical technical error, such as tension or ischemia, and the possibility of fistula healing is low. The time onset of its appearance is another important factor. Early fistula lacks adequate inflammatory blocking, bringing the risk of a complete anastomosis rupture after stent deployment. To place a stent after the seventh PO, when inflammatory blocking around the anastomosis is more consolidated is considered safer. Severe stent-related complications are rare. Nevertheless, stent migration is the most common complication with about 20% incidence. Other complications are esophageal perforation, reflux, bleeding, ulcers and pneumonia [37]. In addition, a Dobbhoff feeding tube may be placed during endoscopy to offer proper nutritional support. During the last decade, endoluminal vacuum therapy has been a promising and effective technique for gastrointestinal perforation and leak management. It was described for the first time in 2008 by Weidenhagen et al. for rectal anastomotic fistula. From there on, the endoluminal vacuum therapy was adapted for the upper GI tract with good results [38, 39].
Surgery is strongly recommended when conservative management fails to adequately drain the fistula/abscess and/or due to the necessity of anastomosis repair. Other indications are diffuse peritonitis, bleeding, sepsis, bowel obstruction and other fistulas [40.] It is related to higher mortality rates when compared with conservative and endoscopic approach [41, 42]. In our data, EJF was more lethal when compared to non-EJF patients (26.7% vs. 4.5%; p < 0.001). Moreover, the mortality rate of patients who required reoperation reached 50%. Similar results were published by Lang et al., in which EJF occurred in 7.5% (83/1114) patients and the mortality rate was 64% (16/25) after reoperation [14]. These findings highlight the magnitude of such complication. It is important to emphasize that the high mortality in reoperations is influenced by the fact that surgery is offered to more severe and critical patients. Despite this important selection bias, it is clear that surgery plays an important role to handle these dramatic cases.
Another interesting aspect found in our study is the negative impact of EJF and OC on long-term survival (p = 0.013 and p = 0.004, respectively). Sierzega et al. identified anastomotic leakage as an independent predictor of survival in 41/690 (5.9%) total gastrectomy patients [HR 3.47 (IC95% 1.82–6.64); p = 0.001] [43]. Major complications such as infection may lead to sustained suppression of patients’ immune system, rendering them to be more susceptible to cancer relapse. Beyond that, surgical complications may restrain patients to return to intended oncologic treatment and, therefore, increase the risk of relapse due to the lack of the benefits of adjuvant therapy [44, 45]. Genuinely, our results showed that adjuvant chemotherapy could not be offered to patients with EJF (p = 0.010).
Although, this was a large population-based study, it still had some potential limitations. Due to its retrospective nature, the study lacks some important information. For example, the operative time and the blood loss were not analyzed. Such factors may contribute to the occurrence of complications. Furthermore, the vast majority of patients (96%) were operated by open approach and, in such cases, the anastomosis was performed with end-to-side circular stapler. Therefore, no comparison could be made regarding the best method to perform the esophagojejunostomy. Indeed, this ought to be determined in prospective randomized trials with large sample size, as the incidence of EJF is quite low.
Conclusions
Esophagojejunal anastomotic fistula after radical total gastrectomy has a low incidence and it is associated with high postoperative mortality. The completion gastrectomy is the main risk factor for its occurrence. Furthermore, EJF is related to longer hospital stay and has a negative impact on long-term survival.
References
Barchi LC, Jacob CE, Bresciani CJ, Yagi OK, Mucerino DR, Lopasso FP et al (2016) Minimally invasive surgery for gastric cancer: time to change the paradigm. Arq Bras Cir Dig. 29(2):117–120
Yoo HM, Lee HH, Shim JH, Jeon HM, Park CH, Song KY (2011) Negative impact of leakage on survival of patients undergoing curative resection for advanced gastric cancer. J Surg Oncol 104(7):734–740
Gong W, Li J (2017) Combat with esophagojejunal anastomotic leakage after total gastrectomy for gastric cancer: a critical review of the literature. Int J Surg. 47:18–24
Washington K (2010) 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol 17(12):3077–3079
Irlbeck T, Zwißler B, Bauer A (2017) ASA classification: transition in the course of time and depiction in the literature. Anaesthesist 66(1):5–10
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Zilberstein B, Malheiros C, Lourenço LG, Kassab P, Jacob CE, Weston AC et al (2013) Brazilian consensus in gastric cancer: guidelines for gastric cancer in Brazil. Arq Bras Cir Dig 26(1):2–6
Association JGC (2017) Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 20(1):1–19
Zilberstein B, Jacob CE, Barchi LC, Yagi OK, Ribeiro U, Coimbra BG et al (2014) Simplified technique for reconstruction of the digestive tract after total and subtotal gastrectomy for gastric cancer. Arq Bras Cir Dig 27(2):133–137
Hyodo M, Hosoya Y, Hirashima Y, Haruta H, Kurashina K, Saito S et al (2007) Minimum leakage rate (0.5%) of stapled esophagojejunostomy with sacrifice of a small part of the jejunum after total gastrectomy in 390 consecutive patients. Dig Surg 24(3):169–172
Deguchi Y, Fukagawa T, Morita S, Ohashi M, Saka M, Katai H (2012) Identification of risk factors for esophagojejunal anastomotic leakage after gastric surgery. World J Surg 36(7):1617–1622
Aurello P, Magistri P, D’Angelo F, Valabrega S, Sirimarco D, Tierno SM et al (2015) Treatment of esophagojejunal anastomosis leakage: a systematic review from the last two decades. Am Surg 81(5):450–453
Lang H, Piso P, Stukenborg C, Raab R, Jähne J (2000) Management and results of proximal anastomotic leaks in a series of 1114 total gastrectomies for gastric carcinoma. Eur J Surg Oncol 26(2):168–171
Meyer L, Meyer F, Dralle H, Ernst M, Lippert H, Gastinger I et al (2005) Insufficiency risk of esophagojejunal anastomosis after total abdominal gastrectomy for gastric carcinoma. Langenbecks Arch Surg. 390(6):510–516
Selby LV, Vertosick EA, Sjoberg DD, Schattner MA, Janjigian YY, Brennan MF et al (2015) Morbidity after total gastrectomy: analysis of 238 patients. J Am Coll Surg 220(5):863–871
Nomura S, Sasako M, Katai H, Sano T, Maruyama K (2000) Decreasing complication rates with stapled esophagojejunostomy following a learning curve. Gastric Cancer 3(2):97–101
Masoomi H, Kim H, Reavis KM, Mills S, Stamos MJ, Nguyen NT (2011) Analysis of factors predictive of gastrointestinal tract leak in laparoscopic and open gastric bypass. Arch Surg 146(9):1048–1051
Takeuchi M, Ishii K, Seki H, Yasui N, Sakata M, Shimada A et al (2016) Excessive visceral fat area as a risk factor for early postoperative complications of total gastrectomy for gastric cancer: a retrospective cohort study. BMC Surg 16(1):54
Budisin N, Budisin E, Golubovic A (2001) Early complications following total gastrectomy for gastric cancer. J Surg Oncol 77(1):35–41
Takahashi H (2006) Total gastrectomy of gastric stump carcinomas is more invasive than usual total gastrectomy for gastric carcinomas. Masui 55(1):79–81
Barchi LC, Charruf AZ, de Oliveira RJ, Jacob CE, Cecconello I, Zilberstein B (2016) Management of postoperative complications of lymphadenectomy. Transl Gastroenterol Hepatol 1:92
Barchi LC, Ramos MFKP, Dias AR, Yagi OK, Ribeiro-Júnior U, Zilberstein B et al (2019) Total omentectomy in gastric cancer surgery: Is it always necessary? Arq Bras Cir Dig 32(1):e1425
Ramos MFKP, Pereira MA, Charruf AZ, Dias AR, Castria TB, Barchi LC et al (2019) Conversion therapy for gastric cancer: expanding the treatment possibilities. Arq Bras Cir Dig 32(2):e1435
Busweiler LAD, Dikken JL, Henneman D, van Berge Henegouwen MI, Ho VKY, Tollenaar RAEM et al (2017) The influence of a composite hospital volume on outcomes for gastric cancer surgery: a Dutch population-based study. J Surg Oncol 115(6):738–745
Pasquer A, Renaud F, Hec F, Gandon A, Vanderbeken M, Drubay V et al (2016) Is centralization needed for esophageal and gastric cancer patients with low operative risk?: A nationwide study. Ann Surg 264(5):823–830
Sano T, Katai H, Sasako M, Maruyama K (2002) One thousand consecutive gastrectomies without operative mortality. Br J Surg 89(1):123
Tu RH, Lin JX, Zheng CH, Li P, Xie JW, Wang JB et al (2017) Development of a nomogram for predicting the risk of anastomotic leakage after a gastrectomy for gastric cancer. Eur J Surg Oncol 43(2):485–492
Onodera H, Ikeuchi D, Nagayama S, Imamura M (2004) Weakness of anastomotic site in diabetic rats is caused by changes in the integrity of newly formed collagen. Dig Surg 21(2):146–151
Kim SH, Son SY, Park YS, Ahn SH, Park DJ, Kim HH (2015) Risk factors for anastomotic leakage: a retrospective cohort study in a single gastric surgical unit. J Gastric Cancer 15(3):167–175
Girard E, Messager M, Sauvanet A, Benoist S, Piessen G, Mabrut JY et al (2014) Anastomotic leakage after gastrointestinal surgery: diagnosis and management. J Visc Surg 151(6):441–450
Migita K, Takayama T, Matsumoto S, Wakatsuki K, Enomoto K, Tanaka T et al (2012) Risk factors for esophagojejunal anastomotic leakage after elective gastrectomy for gastric cancer. J Gastrointest Surg 16(9):1659–1665
Selby LV, Gennarelli RL, Schnorr GC, Solomon SB, Schattner MA, Elkin EB et al (2017) Association of hospital costs with complications following total gastrectomy for gastric adenocarcinoma. JAMA Surg 152(10):953–958
Carboni F, Valle M, Federici O, Levi Sandri GB, Camperchioli I, Lapenta R et al (2016) Esophagojejunal anastomosis leakage after total gastrectomy for esophagogastric junction adenocarcinoma: options of treatment. J Gastrointest Oncol. 7(4):515–522
Dasari BV, Neely D, Kennedy A, Spence G, Rice P, Mackle E et al (2014) The role of esophageal stents in the management of esophageal anastomotic leaks and benign esophageal perforations. Ann Surg 259(5):852–860
Ramos MF, Martins BAC, Alves AM, Maluf-Filho F, Ribeiro-Júnior U, Zilberstein B et al (2015) Endoscopic stent for treatment of esophagojejunostomy fistula. Arq Bras Cir Dig 28(3):216–217
Turkyilmaz A, Eroglu A, Aydin Y, Kurt A, Bilen Y, Karaoglanoglu N (2010) Complications of metallic stent placement in malignant esophageal stricture and their management. Surg Laparosc Endosc Percutan Tech 20(1):10–15
Weidenhagen R, Gruetzner KU, Wiecken T, Spelsberg F, Jauch KW (2008) Endoscopic vacuum-assisted closure of anastomotic leakage following anterior resection of the rectum: a new method. Surg Endosc 22(8):1818–1825
Pournaras DJ, Hardwick RH, Safranek PM, Sujendran V, Bennett J, Macaulay GD et al (2018) Endoluminal vacuum therapy (E-Vac): a treatment option in oesophagogastric surgery. World J Surg 42(8):2507–2511
Messager M, Warlaumont M, Renaud F, Marin H, Branche J, Piessen G et al (2017) Recent improvements in the management of esophageal anastomotic leak after surgery for cancer. Eur J Surg Oncol 43(2):258–269
Oh SJ, Choi WB, Song J, Hyung WJ, Choi SH, Noh SH et al (2009) Complications requiring reoperation after gastrectomy for gastric cancer: 17 years experience in a single institute. J Gastrointest Surg 13(2):239–245
Li QG, Li P, Tang D, Chen J, Wang DR (2013) Impact of postoperative complications on long-term survival after radical resection for gastric cancer. World J Gastroenterol 19(25):4060–4065
Sierzega M, Kolodziejczyk P, Kulig J, Group PGCS (2010) Impact of anastomotic leakage on long-term survival after total gastrectomy for carcinoma of the stomach. Br J Surg 97(7):1035–1042
Aloia TA, Zimmitti G, Conrad C, Gottumukalla V, Kopetz S, Vauthey JN (2014) Return to intended oncologic treatment (RIOT): a novel metric for evaluating the quality of oncosurgical therapy for malignancy. J Surg Oncol 110(2):107–114
Ramos MFKP, Pereira MA, Barchi LC, Yagi OK, Dias AR, Szor DJ et al (2018) Duodenal fistula: the most lethal surgical complication in a case series of radical gastrectomy. Int J Surg. 53:366–370
Acknowledgements
The authors thank other members of the service involved in gastric cancer treatment: Donato R. Mucerino, Carlos E. Jacob (im memoriam), Osmar K. Yagi, Claudio J.C. Bresciani, Marcelo Mester, Amir Charruf, Cynthia Chiaradia, Rodrigo Jose de Oliveira and Fabio P. Lopasso.
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
LCB and MFKPR: study design, data retrieval, critical analysis, and draft of the manuscript. MAP: data retrieval and statistical analysis. ARD: data retrieval and review of the manuscript. URJ, BZ, and IC: critical analysis and review of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All the authors are committed to the Committee on Publication Ethics guidelines and declare that this article has not been submitted to another journal.
Research involving human participants and/or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent is not required for this type of study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Barchi, L.C., Ramos, M.F.K.P., Pereira, M.A. et al. Esophagojejunal anastomotic fistula: a major issue after radical total gastrectomy. Updates Surg 71, 429–438 (2019). https://doi.org/10.1007/s13304-019-00659-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-019-00659-8