Abstract
Purpose
Few studies have investigated the role of hybrid surgery (HS) that incorporates anterior cervical discectomy and fusion (ACDF) and artificial disc replacement (ADR) techniques. To our knowledge, this is the first study that provides a direct comparison of all three groups in terms of intra-operative parameters and outcomes with a minimum follow-up of 2 years.
Methods
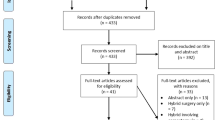
Seven consecutive patients who underwent HS were matched with another seven patients who underwent ACDF and ADR based on levels of surgery. Prospective data on demographics, pre-operative and post-operative assessments, complications and functional scores (VAS, NDI, EQ-5D health score and index) were analysed using Mann–Whitney U test. Type I error was set at 5 %.
Results
Duration of surgery was significantly shorter for ACDF at 135 min (p = 0.025) compared with HS and ADR. ACDF also had greater blood loss when compared with ADR (p < 0.036). ADR has the shortest duration of hospitalization followed by HS and ACDF (p < 0.031). The HS group returned to work fastest (54 days) when compared with both ACDF (107 days) and ADR (73 days) with statistical significance seen between HS and ACDF (p = 0.035). Cervical range of motion (ROM) and functional scores did not show any significant differences.
Conclusion
HS is comparable to ACDF and ADR in terms of safety and feasibility. Findings of shorter in-hospital stay and earlier return to work in HS group may be further explored in large, randomised controlled trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior approach to the cervical spine allows for decompression of the spinal cord and preserves neurological function when the primary compressive pathology lies anterior to the spinal cord [1]. To date, anterior cervical discectomy and fusion (ACDF) is the most accepted procedure with satisfactory clinical outcome and proven radiological fusion rates from 90 to 100 % [2, 3].
Lately, artificial disc replacement (ADR) of the cervical spine has gained popularity. Although the results of ADR are less established than that of ACDF, it has proven to be beneficial in terms of preserving motion of the cervical spine and possibly adjacent level degeneration [8, 9]. These benefits are more apparent in the context of multilevel surgeries [14, 15]. However, indications for ADR are more stringent and the procedure may be longer, leading to the possibility of increased blood loss and wound complications [10, 13, 22]. Given this trade-off, controversy still exists as to the ideal surgical technique(s) that could benefit patients with multilevel cervical disc diseases.
Hybrid surgery (HS) incorporates ACDF and ADR at different levels. The purpose is to combine the advantages in both techniques, thus showing preservation of cervical spine motion without prolonging operative duration and increasing complications. To our knowledge, the existing literature consists of a few studies looking independently at ACDF versus HS, or ADR versus HS. These studies do not allow direct comparison of the results between ACDF, HS and ADR. Therefore, the primary aim of this study was to explore the peri-operative parameters and outcome differences in all three types of surgery. The results of this study will provide grounds for a large, prospective randomised controlled trial.
Materials and methods
Seven consecutive patients who underwent HS by a single surgeon were prospectively enrolled into the study. Using the same hospital electronic database, we did a retrospective random selection of another 7 ACDF and 7 ADR patients matched to the same levels of operation as controls. Selection of appropriate controls was carried out by an independent party from a pool of computer-generated database without having prior knowledge of their outcomes. After this step, a check was performed to ensure that all patients had surgeries performed for prolapsed intervertebral discs, had no obvious degeneration at non-operated levels, and all matched patients had surgeries done within 1 year of each other. One control in the ACDF group and two in the ADR group had to be replaced with newly selected random subjects to meet the above criteria. In our study, spinal levels in which X-rays or MRI scans suggest facet joint arthropathy or hypermobility are treated with fusion. Patients with multi-level disease will receive HS if some levels require replacement and others fusion.
Following ethics board approval, prospective data including patient demographics (age, gender), presence of pre-operative myelopathy, intra-operative details (duration of operation, level of operation, types and sizes of implant, somatosensory evoked potentials (SSEP) and motor-evoked potentials (MEP), complications), post-operative details (drop in haemoglobin, length of hospitalization, and time to return to work), post-operative radiological findings (fusion, cervical spine mobility), functional scores (Visual analogue scale (VAS), Neck disability index (NDI), EQ-5D health score, and EQ-5D index) and surgery related-complications were collected.
In this study, the functional scores were obtained using self-administered questionnaires in the English language during routine follow-up visit at 2 years after the surgery. The evaluation of interbody fusion was according to Bridwell classification [4]. Cervical spine range of movement during flexion and extension was interpreted using lateral projections of the cervical spine obtained at the 2-year follow-up visit by two independent spine surgeons not directly involved in the management of the patient. Measurements were made directly on our radiographic software [Centricity Web V2.0, GE Medical Systems Information Technologies, Milwaukee, USA] using two methods. The first method employs lines placed on the superior endplate of C3 and the inferior endplate of C7 to measure global cervical spine flexion–extension, and lines placed on the superior endplate of the upper vertebra and the inferior endplate of the lower vertebra to measure flexion and extension of the ADR functional spinal unit. The second method uses lines projected from the posterior border of the dens and posterior vertebral line from C7 to measure global cervical spine flexion–extension (see Fig. 1 for method of measurement).
Statistical analysis was performed using StataCorp 2011. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP. Categorical variables were analysed using Fisher’s exact test. Continuous variables were summarized using median and standard deviations and analysed using Mann–Whitney U test. Type I error was set at 5 %.
Technique of ACDF and ADR
All three procedures were performed using a left horizontal incision 4–9 cm long, at the projected level of surgery. Blunt dissection was performed down to the anterior border of the spine taking care not to injure the trachea and oesophagus. A spinal needle was placed in the intervertebral disc to identify the correct level using image intensifier, followed by a complete discectomy and preparation of the endplates. For ACDF, an intervertebral cage packed with bone auto graft mixed with demineralised bone matrix was placed between the vertebras to act as a spacer. For ADR, an artificial disc was inserted under fluoroscopic guidance (see Fig. 2a, b). One drain was inserted and the platysma muscle was repaired. Closure was performed using continuous vicryl suturing for the subcutaneous and dermal layer and the skin using monocryl 3–0 sutures. Post-operatively, all patients with ACDF had 1 month of aspen collar. ADR and HS had 1 month of soft collar.
Results
The baseline patient characteristics were comparable in all three groups (Table 1). The median age was 51 years for HS, 48 years for ACDF and 46 years for ADR. There is no significant difference in gender ratio between the three groups of patient. Comparable number of patients displayed myelopathy features pre-operatively (4 in HS group, 3 in ACDF group, and 2 in ADR group). The levels of index surgery were matched in the three groups. In each arm of comparison, four patients underwent 2-level surgery, and three patients underwent 3-level surgery. The preoperative functional scores were similar in all groups. Minimum follow-up was for 24 months (range 24–45 months).
Disc arthroplasty implants used in the study were cobalt-chrome, UHMWPE, semi constrained disc, i.e. Prodisc-C (Synthes Spine, Paoli, PA, USA). Fusion constructs were performed using Cervios cages (Synthes spine, West Chester, PA). Iliac crest autograft was used for fusion.
The median duration of operation was shortest for ACDF (135 min) followed by HS (195 min) and ADR (197 min). This observation is statistically significant with p = 0.025 when ACDF is being compared with both HS and ADR (see Table 2). Intra-operative SSEP and MEP monitoring did not show any deterioration for all patients in the three groups. Although improvements were noticed for SSEP (3 in HS, 1 in ACDF, 2 in ADR group) and MEP (1 in ADR group), this was not statistically significant.
Post-operative haemoglobin drop, used as a surrogate marker of peri-operative blood loss showed significant difference between ACDF and ADR group (p = 0.036). The ACDF group experienced greater blood loss with a drop of post-operative haemoglobin of 1.2 g/L when compared with ADR group of 0 g/L. Drop in haemoglobin for the HS group (0.7 g/L) lies between both ACDF and ADR groups. No significant difference in blood loss was observed when the hybrid group was compared with both ACDF and ADR groups (p > 0.05).
The length of hospitalization showed statistically significant difference across the three groups. The ADR group had shortest stay of 3 days, followed by HS group of 5 days. The ACDF group required longest hospital stay of 7 days. This is likely to be directly related to donor site morbidity secondary to iliac crest bone graft harvesting.
Patients from HS group returned to work fastest (54 days) when compared with both ACDF (107 days) and ADR (73 days). Although statistical significance was not observed between HS and ADR, it was seen between HS and ACDF (p = 0.035).
At 2-year follow-up, fusion was successfully achieved in all ACDF and HS patients based on Bridwell classification [4] using plain X-rays. No patients undergoing HS or ADR have heterotopic ossification at the disc replacement levels. The three groups shared similar functional improvement at 2 years. Both global and ADR functional spinal units have similar range of movements. No patients needed revision surgery.
In our small series, only four patients demonstrated complications. Three patients (one in each group) had residual limb symptoms after the operation. This was transient in all patients and they improved 6 weeks post-operatively after several courses of outpatient physiotherapy and analgesics. No significant difference in the complication rates was noted across the three groups (see Table 3).
One patient had dysphagia after the operation which resolved during the first follow-up visit at 2 weeks after surgery. No other complications of dura/spinal cord injury, hoarseness of voice, wound infection or implant-related failures were observed at 2-year follow-up.
Discussion
The functional spinal unit (FSU) is mobile and mechanically stable in a normal person. Although ACDF can provide neurological decompression and stability to the FSU, it has the disadvantage of rendering it immobile, resulting in adjacent segment hypermobility and accelerated degeneration [5–7]. However, ACDF remains the gold standard in surgical management of cervical spondylotic myelopathy and has a high level of patient satisfaction [1]. Yet, it is known that the clinical outcomes and fusion rates of instrumented cervical fusion deteriorate as the number of vertebral levels of involvement increases. With the same capability at neurological decompression, ADR is able to preserve both motion and stability at the operated level [8, 9]. This also leads to reduction in adjacent level degeneration. The benefits of ADR in multilevel surgery are thus more obvious with preservation of spinal mobility, avoidance of pseudarthosis and reduction in adjacent segment disease (ASD).
Earlier result has found arthroplasty to be a safe alternative to ACDF for single-level disease with lower reoperation rates [2, 10–12]. With the newly released result of 4-year follow-up on patients with cervical arthroplasty [13], ADR is increasingly being recognized as a realistic surgical option in managing single-level disc disease between C3 and C7. Sasso et al. [13] concluded with level I evidence that the results of arthroplasty are superior to ACDF at 4 years’ follow-up. However, long-term study is needed to further determine its safety in other aspects, e.g. biology of wear debris, effects on the facet joints, ASD, device-fatigue and durability.
The evidence in multilevel ADR though promising is not as well established as its role in single level disease. There are positive level II/III evidence on the early results of multilevel arthroplasty [8, 14, 15]. In terms of reoperation rates and serious adverse events, similar results between the single-level and multilevel arthroplasty groups were found [11]. Moreover, several studies have shown the duration of operation for ADR to be much longer than ACDF [10, 13, 22]. At the same time, the study by Murrey et al. [10] showed no significant difference in the length of hospital stay between Prodisc-C and ACDF.
When selecting patients for HS, several factors may dissuade surgeons to perform ADR over fusion. These include degenerative diseases of the functional spinal unit that may render motion at that level unpredictable—facet joint arthropathy and spinal hypermobility. Since the spondylotic spine is often associated with multiple-level disease, and not all diseased levels may meet acceptable criteria for ADR [16], some surgeons turned to HS as an alternative to multi-level ACDF or ADR [17]. The need to show results of HS in carefully selected patients is important as it gives the surgeon the armamentarium in the treatment of degenerative cervical spinal conditions.
By simply combining ACDF and ADR in HS, the main objective lies at restoring or maintaining motion where appropriate, or favouring bony fusion when indicated by the extent of the degenerative changes and hypermobility [18, 19]. Theoretically, a HS should reach a balance between both ACDF and ADR in terms of both intra-operative and post-operative results. The existing literature either compares ACDF with HS or ADR with HS, thus causing difficulty when drawing conclusions as to where HS stands between ACDF and ADR. To our best knowledge, this is the first study that directly compared the three different techniques for multilevel cervical disc disease. By standardizing multiple factors including surgeon, technique and the protocol of treatment for our patients, we therefore provide a more direct and valid comparison of all three groups in a single-surgeon series performed by a surgeon skilled in both ADR and ACDF. The success of this pilot study will push off larger studies in the future that directly compare these three surgical procedures.
Our study has demonstrated that hybrid construct is a feasible alternative to ADR and ACDF in managing multilevel disc disease in carefully selected patients. In many aspects, the results of HS were between ACDF and ADR. In terms of duration of surgery, HS was similar to multilevel ADR. In terms of blood loss and duration of hospitalization, the results of HS were a fine balance between ACDF and ADR.
With regard to 2-year follow-up, our study showed no significant differences in functional outcome and cervical spine range of movement. Shin et al. [17] found HS to be superior to double-level ACDF by having a better functional outcome and less adjacent range of motion (ROM). Favourable results have also been shown in biomechanical analyses. Cho et al. [20] found that HS produced combined ROM at the operative levels comparable to the intact spine. Similar conclusions were also drawn by Lee et al.’s [21] cadaveric biomechanical study.
However, we noted earlier return to work in the HS group, as compared with both ADR and ACDF groups. This finding was not shown in earlier reported studies. The superiority of HS over ACDF and ADR could not be clearly explained, especially since HS would also involve iliac crest bone grafting similar in ACDF. There is a possibility that patients who received HS truly benefited from the advantages of both techniques. The inability of functional scores to demonstrate similar findings could be secondary to a small sample size. The current literature only compares ACDF with ADR. Mummaneni et al. [2] showed that patients with ADR returned to work in significantly fewer days (range 14–16 days) than patients treated with ACDF. Riew et al. [23] showed that at 6 weeks, significantly more patients (49.2 %) returned to work in the arthroplasty group than fusion group (39.4 %). No statistically significant differences in the percentage of patients who returned to work at 24 and 48 months were found in other studies [10, 13, 24].
With regard to complications, McAfee et al. [25] demonstrated a lower incidence of dysphagia with ADR in single level disease in their study of 251 patients. Our study showed only one patient in the HS group who developed dysphagia post-surgery. Although the literature showed heterotrophic ossification ranging from 50 to 70 % with Prodisc-C up to a minimum of 1-year follow-up, no patients in our study who underwent ADR or HS developed heterotopic ossification [26–28].
Finally, we recognize that this pilot study is limited by a relatively small study population and may not be powered to detect smaller differences. As the 95 % confidence interval estimate of median is not accurate, it should be interpreted carefully and be used to generate hypothesis only. Nevertheless, this study has some strengths being a single-surgeon series that uses a standardized treatment protocol for all patients. This allows valid comparison among all three groups. Given our findings that HS appears comparable to ACDF and ADR in terms of safety and feasibility, and superior in terms of earlier return to work, HS seems an attractive option in carefully selected patients. This should be further explored in large, randomised controlled trials.
References
Bohlman HH, Emery SE, Goodfellow DB, Jones PK (1993) Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 75(9):1298–1307
Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA (2007) Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine 6(3):198–209
Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr (2002) Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 50(2):229–236 (discussion 236–8)
Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K (1995) Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976) 20(12):1410–1418
DiAngelo DJ, Roberston JT, Metcalf NH, McVay BJ, Davis RC (2003) Biomechanical testing of an artificial cervical joint and an anterior cervical plate. J Spinal Disord Tech 16(4):314–323
Dmitriev AE, Cunningham BW, Hu N, Sell G, Vigna F, McAfee PC (2005) Adjacent level intradiscal pressure and segmental kinematics following a cervical total disc arthroplasty: an in vitro human cadaveric model. Spine (Phila Pa 1976) 30(10):1165–1172
Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K (1999) Strain on intervertebral discs after anterior cervical decompression and fusion. Spine (Phila Pa 1976) 24(7):670–675
Pimenta L, McAfee PC, Cappuccino A, Cunningham BW, Diaz R, Coutinho E (2007) Superiority of multilevel cervical arthroplasty outcomes versus single-level outcomes: 229 consecutive PCM prostheses. Spine (Phila Pa 1976). 32(12):1337–1344
Phillips FM, Tzermiadianos MN, Voronov LI, Havey RM, Carandang G, Dooris A, Patwardhan AG (2009) Effect of two-level total disc replacement on cervical spine kinematics. Spine (Phila Pa 1976) 34(22):E794–E799
Murrey D, Janssen M, Delamarter R et al (2009) Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J 9(4):275–286
Cheerag D. Upadhyaya MD, Jau-Ching Wu, Gopalakrishnan Balamurali MD, Regis WH, Vincent C, Traynelis MD, Bobby Tay MD, Domagoj Coric MD, Gregory RT, Praveen VM (2010) Combined results of the 3 US IDE randomized cervical arthroplasty trials with 2-years of follow-up. Neurosurgery 67(2):543
Anderson P, Sasso R, Newton M, Riew KD (2009) Reoperation rates for cervical arthroplasty vs. arthrodesis. Spine J 5(suppl):1S–189S
Sasso RC, Anderson PA, Riew KD, Heller JG (2011) Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. J Bone Joint Surg Am 93(18):1684–1692
Cardoso MJ, Rosner MK (2010) Multilevel cervical arthroplasty with artificial disc replacement. Neurosurg Focus 28(5):E19
Huppert J, Beaurain J, Steib JP, Bernard P, Dufour T, Hovorka I, Stecken J, Dam-Hieu P, Fuentes JM, Vital JM, Vila T, Aubourg L (2011) Comparison between single- and multi-level patients: clinical and radiological outcomes 2 years after cervical disc replacement. Eur Spine J 20(9):1417–1426 (Epub 2011 Feb 20)
Auerbach JD, Jones KJ, Fras CI, Balderston JR, Rushton SA, Chin KR (2008) The prevalence of indications and contraindications to cervical total disc replacement. Spine J 8(5):711–716 (Epub 2007 Nov 5)
Shin DA, Yi S, Yoon do H, Kim KN, Shin HC (2009) Artificial disc replacement combined with fusion versus two-level fusion in cervical two-level disc disease. Spine (Phila Pa 1976) 34(11):1153–1159 (discussion 1160–1161)
Giuseppe MV (2009) Barbagallo, Roberto Assietti, Leonardo Corbino, Giuseppe Olindo, Pietro V. Foti, Vittorio Russo, Vincenzo Albanese. Early results and review of the literature of a novel hybrid surgical technique combining cervical arthrodesis and disc arthroplasty for treating multilevel degenerative disc disease: opposite or complementary techniques? Eur Spine J 18(Suppl 1):S29–S39
Cardoso MJ, Mendelsohn A, Rosner MK (2011) Cervical hybrid arthroplasty with 2 unique fusion techniques. J Neurosurg Spine 15(1):48–54 Epub 2011 Apr 1
Cho BY, Lim J, Sim HB, Park J (2010) Biomechanical analysis of the range of motion after placement of a two-level cervical ProDisc-C versus hybrid construct. Spine (Phila Pa 1976) 35:1769–1776
Lee MJ, Dumonski M, Phillips FM, Voronov LI, Renner SM, Carandang G, Havey RM, Patwardhan AG. Disc Replacement Adjacent to Cervical Fusion: A Biomechanical Comparison of Hybrid Construct vs. Two-Level Fusion. Spine (Phila Pa 1976). 2011 Feb 1. [Epub ahead of print]
Sasso RC, Smucker JD, Hacker RJ, Heller JG (2007) Artificial disc versus fusion: a prospective, randomized study with 2-year follow-up on 99 patients. Spine (Phila Pa 1976) 32(26):2933–2940 (discussion 2941–2942)
Riew KD, Buchowski JM, Sasso R, Zdeblick T, Metcalf NH, Anderson PA (2008) Cervical disc arthroplasty compared with arthrodesis for the treatment of myelopathy. J Bone Joint Surg Am 90(11):2354–2364
Heller JG, Sasso RC, Papadopoulos SM et al (2009) Comparison of BRYAN cervical disc arthroplasty with anterior cervical decompression and fusion: clinical and radiographic results of a randomized, controlled, clinical trial. Spine 34(2):101–107
McAfee PC, Cappuccino A, Cunningham BW, Devine JG, Phillips FM, Regan JJ, Albert TJ, Ahrens JE (2010) Lower incidence of dysphagia with cervical arthroplasty compared with ACDF in a prospective randomized clinical trial. J Spinal Disord Tech 23(1):1–8
Ryu KS, Park CK, Jun SC, Huh HY (2010) Radiological changes of the operated and adjacent segments following cervical arthroplasty after a minimum 24-month follow-up: comparison between the Bryan and Prodisc-C devices. J Neurosurg Spine 13(3):299–307
Yi S, Kim KN, Yang MS, Yang JW, Kim H, Ha Y, Yoon do H, Shin HC (2010) Difference in occurrence of heterotopic ossification according to prosthesis type in the cervical artificial disc replacement. Spine (Phila Pa 1976) 35(16):1556–1561
Mehren C, Suchomel P, Grochulla F, Barsa P, Sourkova P, Hradil J, Korge A, Mayer HM (2006) Heterotopic ossification in total cervical artificial disc replacement. Spine (Phila Pa 1976) 31(24):2802–2806
Acknowledgments
We would like to thank Dr Chen Weiming Darren for his help in compiling the data required for the study.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hey, H.W.D., Hong, C.C., Long, A.S. et al. Is hybrid surgery of the cervical spine a good balance between fusion and arthroplasty? Pilot results from a single surgeon series. Eur Spine J 22, 116–122 (2013). https://doi.org/10.1007/s00586-012-2486-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2486-6