Abstract
Purpose
Although several studies have established the safety and efficacy of cervical disc arthroplasty (CDA) as compared to anterior cervical discectomy and fusion (ACDF), few studies have investigated the role of hybrid surgery (HS) that incorporates ACDF and CDA techniques in multilevel cervical degenerative disc disease (MLCDDD).
Methods
This prospective study enrolled patients with MLCDDD who underwent HS. Twenty consecutive patients who underwent HS were compared with patients who underwent ACDF and CDA at the same level of surgery. Patients were followed up for more than 2 years. Intraoperative parameters, clinical features and outcome scores were recorded. Radiological assessments included overall range of motion (ROM), disc height (DHI), and changes in adjacent disc spaces.
Results
Duration of surgery was significantly shorter for ACDF compared with HS and CDA (P < 0.05). The VAS, SF-36, JOA, and NDI scores improved significantly after surgery in all the patients without significant differences among the groups. Cervical ROM increased significantly in CDA and HS groups as compared with ACDF-treated patients (P < 0.05). The mean DHI at the treated level was significantly restored after surgery in all the groups. The HS group returned to work faster (30 days) when compared with both ACDF (62 days) and CDA (65 days) (P < 0.05).
Conclusion
HS is an effective, reliable, and safe procedure for the treatment MLCDDD. Such a surgical construct is comparable to ACDF and CDA in terms of safety and feasibility. However, large, randomized controlled trials are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical radiculopathy and myelopathy are common diagnoses in adult patients and have been shown to cause significant disability and loss of productivity [1]. Surgical options exist for the treatment of cervical radiculopathy and myelopathy. These include posterior decompression and fusion, anterior cervical discectomy and fusion (ACDF) and cervical disc arthroplasty (CDA).
To date, ACDF is the most accepted treatment with a satisfactory clinical outcome. Such a procedure is highly effective in terms of resolving symptoms, improving nerve function, and restoring the physiological curvature of the cervical spine. However, it has been pointed out that fusion may alter the normal biomechanics of the spine, which may result in acceleration of adjacent segment degeneration (ASD) and a need for subsequent reoperation. These concerns have stimulated the search for motion-preserving procedures such as artificial cervical disc arthroplasty [2, 3]. Although the results of CDA are less established than those of ACDF, it has been proven to be beneficial in terms of preserving motion of the cervical spine and possibly adjacent level degeneration [4, 5]. These benefits are unknown in the context of multilevel surgeries where the role of CDA needs further investigations. Furthermore, controversy exists as to the ideal surgical techniques that could benefit patients with multilevel cervical disc diseases (MLDDD). In this regard, hybrid surgery (HS) that incorporates ACDF and CDA at different levels can be considered a possible option. The purpose is to combine the advantages of both techniques in terms of vertebral stability and spine motion preservation. The primary aim of the present study was to explore the outcome differences in all three types of surgery.
Materials and methods
Patient populations and indications
Between January 2009 and January 2013, twenty consecutive patients who underwent HS by a single surgeon were prospectively enrolled in the study. The surgical database at this institution was queried to identify 20 ACDF and 20 CDA patients corresponding to the same levels of operation as controls. Patients were diagnosed based on preoperative radiograph, CT scan and MRI findings. All patients enrolled in the study were suitable candidates for both CDA and ACDF. Enrollment required a diagnosis of degenerative disc disease with symptomatic radiculopathy or myeloradiculopathy at 2 contiguous levels from C-3 to C-7. The exclusion criteria were one or more than 2 vertebral levels requiring treatment, prior spine surgery at the operative levels, ossification of the posterior longitudinal ligament, severe facet arthritis, lack of motion or instability at the level of surgery, narrowing of the spinal canal, fracture, infection, tumor, and osteoporosis. Preoperative features were considered to define the precise selection criteria for choosing each kind of implant. In this regard, the presence of motion on preoperative dynamic X-rays was an element if favor for CDA. If no motion at the target level was observed, ACDF was preferred. In case of radiographic signs of instability (i.e., translational instability of more than 2 mm), ACDF was achieved. When advanced vertebral body spondylosis or facet degeneration was observed, ACDF was chosen. Overall, patients received CDA or HS if both or at least one-level met the criteria for arthroplasty, respectively. In HS cases, CDA was performed at a mobile and non-spondylotic segment.
Surgical procedure
A standard right-sided approach was undertaken to access the anterior cervical spine. Blunt dissection was performed down to the anterior border of the spine taking care not to injure the trachea and esophagus. A complete anterior discectomy was performed. When indicated, the posterior longitudinal ligament was released to allow for excision of extruded disc material. For ACDF, intervertebral ROI-C cages (LDR Médical, France) packed with demineralized bone matrix were placed between the vertebras to act as a spacer. Correct level distraction and ideal cage choice were performed according to the lateral fluoroscopically assisted trialing. The trial was then removed and the appropriate-sized final cage endplates were inserted. Thereafter, the dedicated double anchoring system was implanted in the up and down vertebral body to obtain an intervertebral strength positioning (Fig. 1a) [6]. For CDA, the ProDisc-C (Depuy Synthes, Raynham, MA, USA) or Mobi-C (LDR Médical, France) was inserted under fluoroscopic guidance (Fig. 1b). When hybrid surgery was performed, both procedures were applied (Fig. 1c). Post-operatively, all patients with ACDF had no more than 2 weeks of collar prescription while CDA and HS had 1 week, or less, of soft collar.
Data collection and outcome evaluation
Data including patient demographics (age, gender), intra-operative details (duration of operation, level of operation, types and sizes of implant, complications), post-operative details (length of hospitalization, and time to return to work), post-operative functional scores, radiological findings, and surgery-related complications were collected.
During follow-up, clinical and radiographic data were collected on the last day of hospital stay, at 1 and 6 months, and every year. All the patients were included in the clinical and radiographic evaluations at each follow-up time point. Outcome measures used were the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36) [7], Neck Disability Index (NDI) [8], and Visual Analog Scale (VAS) scores for neck and arm pain [9]. All patients were asked to complete questionnaires, even in the form of interview, before surgery and at each follow-up examination. The NDI and VAS scores ranged from 0 to 100. Odom’s grading system (poor, fair, good, or excellent) was used to evaluate patient satisfaction with the surgery [10]. Myelopathy was graded using the Japanese Orthopedic Association (JOA) score [11].
Anteroposterior, lateral, and flexion–extension radiographs were taken before surgery, within 1 week after surgery, and at 1 and 6 months after surgery. Subsequent follow-up examinations were performed every 12 months. MRI was routinely performed to evaluate preoperative spinal cord compression. The range of motion (ROM) was measured on the dynamic full flexion and extension radiographs, and the angle of the implant was measured on the immediate postoperative lateral radiograph [12]. A kyphotic angle was considered to be a positive value. The disc height (DHI) was measured on the lateral radiograph as the distance from the highest portion of the lower end-plate of the cephalad vertebra to the closest portion of the upper end-plate of the caudal vertebra. Degenerative changes in the adjacent segments were evaluated on MRI at 12 or 24 months postoperatively. Disc degeneration was graded on T2-weighted sagittal and axial images as described by Miyazaki [13]. The evaluation of interbody fusion was according to Bridwell classification [14].
Statistical analysis
Continuous data were computed by means and SDs. Differences in functional outcome measures between pre-operative and post-operative time points and during further follow-up were determined using the t test for paired samples if a normality test was passed or a Wilcoxon signed-rank test if a normality test was failed. Categorical variables were analyzed using Fisher’s exact test.
Results
Patient population
Sixty patients (33 men and 27 women; mean age 46.40 years, range 30–75 years) underwent surgery for MLDDD. All patients were older than 18 years and had MLDDD between C3 and C7 with intractable radiculopathy or myelopathy. Thirty-five patients (58.3 %) had radicular pain, 15 (25 %) had myelopathy, and 10 (16.6 %) had both radiculopathy and myelopathy. Most patients had a history of incapacitating neck and arm pain lasting longer than 6 weeks, which was unresponsive to physical therapy and anti-inflammatory medication, or had new neurological deficits resulting from myelopathy. Table 1 summarizes patients’ characteristics.
All the patients had a minimum of 24 months follow-up (24–40 months). The median age was 44.2 years for HS, 47.3 years for ACDF and 40.5 years for CDA. There was no significant difference in gender ratio between the three groups of patients. A comparable number of patients presented with myelopathy features pre-operatively (10 in HS group, 9 in ACDF group, and 9 in CDA group). In each group, all the patients had 2-level surgery. The preoperative functional scores were similar in all groups. ROI-C (LDR Médical, France) cage was used for pure ACDF and hybrid surgery. For CDA and HS, the ProDisc-C (Depuy Synthes, Raynham, MA, USA) cervical arthroplasty was used in 87.5 % of the cases and MOBI-C (LDR Médical, France) in the remaining 12.5 % of cases.
The median duration of operation was significantly shorter for ACDF (95 ± 2.3 min) when compared with HS (140 ± 1.7 min) and CDA (160 ± 2.1 min) (P < 0.05). The length of hospitalization did not show statistically significant difference across the three groups. The average hospitalization time, following the surgical treatment, was 2 days. The HS group returned to work faster (30 days) when compared with both ACDF (62 days) and CDA (65 days) (P < 0.05) (see Table 2).
Outcomes
The VAS, SF-36, JOA, and NDI scores improved significantly after surgery in all the patients (P < 0.05 compared to pre-op) without significant differences among the groups. Using Odom’s criteria, 90 % of patients rated their level of satisfaction with the surgery as excellent or good, without significant difference among the groups (P > 0.05). Clinical outcomes are summarized in Table 3.
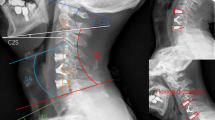
Cervical ROM increased significantly in CDA (from 41.6 ± 7.5 to 47.2 ± 6.6) and HS (from 40.2 ± 6.7 to 47.1 ± 7.1) groups as compared with ACDF-treated patients (from 40.5 ± 9.4 to 36.5 ± 7.3) (P < 0.05). The mean DHI at the treated level was significantly restored after surgery in all the groups. Briefly, the height of intervertebral space was significantly improved from 6 ± 0.9 mm measured before surgery to 7.4 ± 0.2 mm at 1 week and 7.1 ± 0.4 mm at 24 months following the surgical treatment (P < 0.05). At 2-year follow-up, fusion was successfully achieved in all ACDF and HS patients according to the criteria suggested by Pitzen and collaborators [15]. No patients undergoing HS or CDA presented with heterotopic ossification at the disc replacement levels. The three groups shared similar functional improvement at 2 years without significant differences (see Table 4). No patients needed revision surgery. Only one patient complained of minor dysphagia at 12 months follow-up with a complete resolution at 24 months follow-up. Overall, no device-related complications were observed including device mobilization, subsidence or segmental collapse by 24 months. An illustrative case is shown in Fig. 2.
Discussion
Here, we investigated the safety and efficacy HS using cervical artificial discs and cages comparing the results to the standard surgical treatments, ACDF and pure CDA, for the treatment of multilevel cervical disc diseases (MLDDD). Results were presented through 24 months mean follow-up as part of a prospective study compared to retrospectively investigated patients for ACDF and CDA matching, as control, for the same levels of operation. Duration of surgery was significantly shorter for ACDF compared with HS and CDA (P < 0.05). The VAS, SF-36, JOA, and NDI scores improved significantly after surgery in all the patients without significant differences among the groups. Cervical ROM increased significantly in CDA and HS groups compared with ACDF-treated patients (P < 0.05). The mean DHI at the treated level was significantly restored after surgery in all the groups. The HS group returned to work faster (30 days) when compared with both ACDF (62 days) and CDA (65 days) (P < 0.05).
This 45-year-old man presented with a 2-year history of progressive numbness and weakness in both hands with left prevalence. T2-weighted MRI showed C5–C6 and C6–C7 disc herniation with left foraminal stenosis prominent in the C6–C7 (a–c). The preoperative disc height at C5–C6 was 5.3 and 6 mm at C6–C7. The preoperative range of motion (ROM) was 41.2. Postoperative lateral and anterior–posterior radiographs showed the cervical implants (MOBI-C at C5–C6 and ROI-C at C6–C7) in a proper position (d, e). The postoperative disc height was 8.4 and 7.4 mm at C5–C6 and C6–C7, respectively. Postoperative ROM was 48.2 as assessed on flexion–extension lateral radiographs at 24 months following surgery (f, g). The patient was discharged at the post-operative day 2 and returned to work free of symptoms following 30 days
When dealing with a patient affected by cervical spine disc disease, ACDF and cervical arthroplasty are two possible operative techniques [16]. According to the literature, only 43 % of patients meet the indications for cervical disc arthroplasty [17]. For the remaining 57 % of suffering patients, ACDF is still the gold standard to achieve the reduction of the neurological deficits. One of the major concerns regarding ACDF is that it could not preserve the normal kinematics of the spine and might, therefore, result in adjacent segment degeneration (ASD). Such an occurrence could eventually lead to the need for additional treatment. In this regard, increased motion and increased intradiscal pressure have been reported in the untreated levels adjacent to fused levels [18]. It has been pointed out that these changes may lead to ASD as seen in 25 % of patients who underwent single-level ACDF within 10 years [19]. By preserving treated segment natural motion as well as overall cervical spine biomechanics, CDA may avoid ASD and related symptoms while providing mechanical stability following neural decompression [20]. With the newly released result of 4-year follow-up on patients with cervical arthroplasty [21], where CDA was found to be superior to ACDF, arthroplasty is increasingly being recognized as a realistic surgical option in managing single-level disc disease. However, as the number of treated segments increases from one level to two contiguous levels, the available clinical data comparing CDA to ACDF diminish greatly. In this regard, it is well known that the clinical outcomes and fusion rates of instrumented cervical fusion change as the number of the treated vertebral levels increases. While promising evidence in multilevel ACDF and CDA exist [4] little is known about HS. When selecting patients for HS some factors should be considered. These include degenerative diseases of the functional spinal unit that may render motion at that level unpredictable. Since the spondylotic spine is often associated with multiple-level disease, and not all the affected levels may meet acceptable criteria for CDA [17], some surgeons turned to HS as an alternative to multi-level ACDF or CDA [22]. The main role for HS would lie in restoring or maintaining motion where appropriate, or promoting bony fusion when indicated by the extent of the degenerative changes and hypermobility. Accordingly, HS should provide a balance between both ACDF and CDA in terms of both intra-operative and post-operative results. The existing literature does not provide firm arguments since available data come from comparison between ACDF with HS or CDA with HS.
In this study, it was directly compared the three different techniques for MCDD providing a direct comparison of all three groups in a single-surgeon series. The results suggest that hybrid construct is a feasible alternative to CDA and ACDF in managing multilevel disc disease in selected patients. In many aspects, the results from HS were almost superposed on these of ACDF and CDA. Duration of surgery was significantly shorter for ACDF. The outcome scores improved significantly after surgery in all the patients without significant differences. Radiographic features were positively observed in all the groups without differences except for ROM, which was significantly increased in both CDA and HS groups. No patients in CDA or HS group developed heterotopic ossification. Of mention, the HS group returned to work faster when compared with both ACDF and CDA. Although this issue deserves further investigations, it seems to be in agreement with previous studies showing a more rapid return to work in patients with CDA compared with ACDF [23].
In a previous study, blood loss and duration of hospitalization were found similar in patients with HS and ACDF and CDA [23]. In a different study, HS was found to be superior to double-level ACDF, since better functional outcome and less adjacent range of motion (ROM) were observed [22]. Biomechanical studies indicate that HS could maintain the combined motion of operative levels [24, 25], without difference from the normal spine. In this regard, emerging evidence has shown that HS does not affect the cervical spinal kinematics, the intradiscal pressure in adjacent segments and facet joint force [26]. On the contrary, 2-level fusion constrains ROM of operative levels and induced compensatory increase of motion at adjacent levels that may adversely increase the intradiscal pressure [26]. Concerning the complications, in the present study, only one patient presented with postoperative dysphagia with a complete resolution at 24 months follow-up.
The study suffers from some limitations. First, the follow-up was short to assume firm observations. Second, the study compared patients prospectively treated with two groups retrospectively reviewed. Nevertheless, this allowed valid comparison among all the three groups with sound results expanding data of a previous study [23].
Overall, the findings provided suggest that hybrid construct is a safe and effective surgical strategy for decompression in patients with multilevel cervical disc diseases.
Long-term follow-up in large, randomized controlled trials will be helpful for determining this conclusion.
References
Schoenfeld AJ, George AA, Bader JO, Caram PM Jr (2012) Incidence and epidemiology of cervical radiculopathy in the United States military: 2000 to 2009. J Spinal Disord Tech 25:17–22. doi:10.1097/BSD.0b013e31820d77ea
Lawrence BD, Hilibrand AS, Brodt ED, Dettori JR, Brodke DS (2012) Predicting the risk of adjacent segment pathology in the cervical spine: a systematic review. Spine 37:S52–S64. doi:10.1097/BRS.0b013e31826d60fb
Wang L, Song YM, Liu LM, Liu H, Li T (2014) Clinical and radiographic outcomes of dynamic cervical implant replacement for treatment of single-level degenerative cervical disc disease: a 24-month follow-up. Eur Spine J 23:1680–1687. doi:10.1007/s00586-014-3180-7
Pimenta L, McAfee PC, Cappuccino A, Cunningham BW, Diaz R, Coutinho E (2007) Superiority of multilevel cervical arthroplasty outcomes versus single-level outcomes: 229 consecutive PCM prostheses. Spine 32:1337–1344. doi:10.1097/BRS.0b013e318059af12
Phillips FM, Tzermiadianos MN, Voronov LI, Havey RM, Carandang G, Dooris A, Patwardhan AG (2009) Effect of two-level total disc replacement on cervical spine kinematics. Spine 34:E794–E799. doi:10.1097/BRS.0b013e3181afe4bb
Grasso G, Giambartino F, Tomasello G, Iacopino G (2014) Anterior cervical discectomy and fusion with ROI-C peek cage: cervical alignment and patient outcomes. Eur Spine J 23(Suppl 6):650–657. doi:10.1007/s00586-014-3553-y
King JT Jr, Roberts MS (2002) Validity and reliability of the Short Form-36 in cervical spondylotic myelopathy. J Neurosurg 97:180–185
Vernon H, Mior S (1991) The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther 14:409–415
Bijur PE, Silver W, Gallagher EJ (2001) Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med 8:1153–1157
Odom GL, Finney W, Woodhall B (1958) Cervical disk lesions. J Am Med Assoc 166:23–28
Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K (2001) Interobserver and intraobserver reliability of the japanese orthopaedic association scoring system for evaluation of cervical compression myelopathy. Spine 26:1890–1894 (discussion 1895)
Lim MR, Girardi FP, Zhang K, Huang RC, Peterson MG, Cammisa FP Jr (2005) Measurement of total disc replacement radiographic range of motion: a comparison of two techniques. J Spinal Disord Tech 18:252–256
Miyazaki M, Hong SW, Yoon SH, Morishita Y, Wang JC (2008) Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J Spinal Disord Tech 21:288–292. doi:10.1097/BSD.0b013e31813c0e59
Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K (1995) Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine 20:1410–1418
Pitzen TR, Chrobok J, Stulik J, Ruffing S, Drumm J, Sova L, Kucera R, Vyskocil T, Steudel WI (2009) Implant complications, fusion, loss of lordosis, and outcome after anterior cervical plating with dynamic or rigid plates: two-year results of a multi-centric, randomized, controlled study. Spine 34:641–646. doi:10.1097/BRS.0b013e318198ce10
Sasso RC, Smucker JD, Hacker RJ, Heller JG (2007) Clinical outcomes of BRYAN cervical disc arthroplasty: a prospective, randomized, controlled, multicenter trial with 24-month follow-up. J Spinal Disord Tech 20:481–491. doi:10.1097/BSD.0b013e3180310534
Auerbach JD, Jones KJ, Fras CI, Balderston JR, Rushton SA, Chin KR (2008) The prevalence of indications and contraindications to cervical total disc replacement. Spine J 8:711–716. doi:10.1016/j.spinee.2007.06.018
Gallucci M, Limbucci N, Paonessa A, Splendiani A (2007) Degenerative disease of the spine. Neuroimaging Clin N Am 17:87–103. doi:10.1016/j.nic.2007.01.002
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81:519–528
Pracyk JB, Traynelis VC (2005) Treatment of the painful motion segment: cervical arthroplasty. Spine 30:S23–S32
Sasso RC, Anderson PA, Riew KD, Heller JG (2011) Results of cervical arthroplasty compared with anterior discectomy and fusion: four-year clinical outcomes in a prospective, randomized controlled trial. Orthopedics 34:889. doi:10.3928/01477447-20110922-24
Shin DA, Yi S, Yoon DH, Kim KN, Shin HC (2009) Artificial disc replacement combined with fusion versus two-level fusion in cervical two-level disc disease. Spine 34:1153–1159. doi:10.1097/BRS.0b013e31819c9d39 (discussion 1160–1151)
Hey HW, Hong CC, Long AS, Hee HT (2013) Is hybrid surgery of the cervical spine a good balance between fusion and arthroplasty? Pilot results from a single surgeon series. Eur Spine J 22:116–122. doi:10.1007/s00586-012-2486-6
Lee MJ, Dumonski M, Phillips FM, Voronov LI, Renner SM, Carandang G, Havey RM, Patwardhan AG (2011) Disc replacement adjacent to cervical fusion: a biomechanical comparison of hybrid construct versus two-level fusion. Spine 36:1932–1939. doi:10.1097/BRS.0b013e3181fc1aff
Jia Z, Mo Z, Ding F, He Q, Fan Y, Ruan D (2014) Hybrid surgery for multilevel cervical degenerative disc diseases: a systematic review of biomechanical and clinical evidence. Eur Spine J 23:1619–1632. doi:10.1007/s00586-014-3389-5
Zhao Y, Li Q, Mo Z, Sun Y, Fan Y (2013) Finite element analysis of cervical arthroplasty combined with fusion against 2-level fusion. J Spinal Disord Tech 26:347–350. doi:10.1097/BSD.0b013e318246b163
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Grasso, G. Clinical and radiological features of hybrid surgery in multilevel cervical degenerative disc disease. Eur Spine J 24 (Suppl 7), 842–848 (2015). https://doi.org/10.1007/s00586-015-4281-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4281-7