Abstract
Background
Multilevel cervical degenerative disc disease (CDDD) can be treated surgically with anterior cervical discectomy and fusion (ACDF), cervical disc arthroplasty (CDA), or a hybrid surgery (HS) of the two in which both procedures are used at different vertebral levels. A systematic review and meta-analysis was performed to compare the clinical and radiographical outcomes of HS against ACDF or CDA alone.
Methods
Three electronic databases were searched for articles published before December 2018. The literature was searched and assessed by independent reviewers according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement.
Results
Eight papers were identified as eligible with a total of 424 patients. Post-operative C2–C7 range of motion (ROM) was significantly greater after HS than ACDF (p = 0.004; mean difference (MD) 6.14°). The ROM of the superior adjacent segment was significantly lower after HS than ACDF (p < 0.0001; MD − 2.87°) as was the ROM of the inferior adjacent segment (p = 0.0005; MD − 3.11°). HS patients’ return to work was shorter than those who underwent ACDF (p < 0.00001; MD − 32.01 days) and CDA (p < 0.00001; MD − 32.92 days). There were no statistically significant differences in functional outcomes following CDA compared with HS. There was no significant difference in operation time, intra-operative blood loss, or post-operative complications between any of the procedures.
Conclusion
The number of included studies was small, the heterogeneity between them was substantial, and the quality of evidence was very low. Large randomised controlled trials are required to provide strong evidence that would enable recommendation of one intervention over another.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cervical degenerative disc disease (CDDD) and associated changes to surrounding structures can impinge on the spinal cord and spinal nerves presenting as myelopathy, radiculopathy, or both. For decades, anterior cervical discectomy and fusion (ACDF) has been considered the optimal surgical management of CDDD [3]. However, ACDF is associated with adjacent segment disease (ASD) [4, 6, 14, 26] due to a reduced range of motion (ROM) at the fused segments and a compensatory increase in mobility in adjacent vertebral levels [24]. Symptomatic ASD may require revision surgery [3, 4, 14, 29]; an additional burden on patients and healthcare providers. Treating multilevel CDDD with ACDF is associated with greater morbidity and poorer outcomes with each additional vertebral level involved [7, 33].
Cervical disc arthroplasty (CDA) is as an alternative procedure. Clinical and biomechanical studies report superior preservation of the kinematics of the cervical spine [9, 18], a reduction of abnormal motion at adjacent levels [9], and a lower incidence of ASD after CDA than ACDF [8], although ASD may still occur long-term [19]. Complications of CDA include implant subsidence and heterotopic ossification (HO) of surrounding soft tissue [19, 22, 25]. Multilevel CDA is a safe and effective alternative to ACDF [11], with preservation of cervical ROM and lower incidence of ASD [31, 39] and fewer revision surgeries [38]. Functional and clinical outcomes are equivalent to single-level CDA [37]; however, extensive use of CDA for multilevel CDDD is restricted by numerous contraindications [1, 19, 22].
Hybrid surgery (HS) involving a combination of ACDF and CDA at adjacent vertebral levels is being utilised in the treatment of multilevel CDDD. HS is appropriate in a select group of patients with different types of disease and different degrees of degeneration at contiguous levels, with the most appropriate intervention used at each. [35] The definition of HS varies throughout the literature, frequently including anterior cervical corpectomy and fusion (ACCF) as well as ACDF or CDA. Previous systematic reviews and meta-analyses have examined the outcomes of HS versus ACDF [10, 20, 28, 34,35,36], and included HS involving ACCF [10, 20, 36]. The objective of this review is to assess the safety and efficacy of HS comprising ACDF and CDA only, compared with both ACDF and CDA alone in the management of multilevel CDDD.
Materials and methods
Study selection
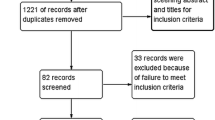
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [23]. Review protocol: PROSPERO ID CRD42017065980. A systematic literature review was performed using PubMed/Medline, Embase (via OVID), and Web of Science. Databases were searched from their date of inception to August 2017. A later search filtered for papers published between August 2017 and December 2018. Searches were generated using MeSH terms and keywords (Appendix 1). Two reviewers (M.A.H. and E.C.G.) screened studies by title and abstract. The full text of potentially eligible studies was assessed. Reference lists of included studies and previous systematic reviews were searched. References were managed using Mendeley and Microsoft Excel.
Inclusion and exclusion criteria
Studies meeting the following criteria were eligible for inclusion: (1) adult patient population with multilevel CDDD; (2) randomised controlled trials (RCTs) and non-randomised studies comparing HS with either ACDF or CDA or both; (3) appropriate clinical and/or radiographical outcomes reported. For studies with overlapping populations, the most recent study was included. Study types excluded were the following: non-comparative, biomechanical/in vitro/cadaveric, systematic reviews and meta-analyses, letters, or abstracts. Other exclusions were the following: full text not in English, HS involving corpectomy, revision surgeries, non-contiguous operative levels, serious comorbidities, or a non-hospital setting.
Risk of bias assessment
We used the Methodological Index for Non-Randomised Studies (MINORS) to perform the risk of bias assessment of non-randomised studies [27], and the Cochrane collaboration’s tool for assessing the risk of bias in the RCT using Review Manager (RevMan) software (version 5.3). This was performed independently by two reviewers (M.A.H and E.C.G) and disagreement resolved by discussion. A third reviewer (A.K.D) was available for mediation, throughout the review process.
Data extraction
Data was extracted into an Excel spreadsheet by two reviewers (M.A.H. and E.C.G.). General characteristics of the included studies were extracted as well as the following outcomes: Neck Disability Index (NDI), Visual Analogue Scale (VAS), C2–C7 range of motion (ROM), superior adjacent segment (SAS) ROM, inferior adjacent segment (IAS) ROM, operation time, intra-operative blood loss, return to work, and complications.
Quality of evidence assessment
The quality of the evidence was assessed according to the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) working group which categorises evidence as being of high, moderate, low, or very low quality (Appendix 2) [2].
Statistical analysis
Data analysis and forest plots were produced using RevMan v5.3. Heterogeneity between studies was estimated using chi2 (p > 0.05) and the value of I2. A random effects model was applied to data due to substantial heterogeneity. For continuous data, the mean difference (MD) and 95% confidence intervals (CI) were calculated (inverse variance), and for dichotomous data, the odds ratio (OR) and 95% CI (Mantel-Haenszel). p value < 0.05 was considered statistically significant.
Results
Search results
A flow diagram of the selection process is shown in Fig. 1. Searching three electronic databases identified eight eligible studies (seven observational studies and one RCT) with a total of 424 patients [12, 13, 15,16,17, 21, 30, 32]: Grasso [12] n = 60 (14.2%); Hey [13] n = 21 (4.95%); Jang [15] n = 49 (11.6%); Ji [16] n = 40 (9.43%); Kang [17] n = 24 (5.66%); Mende [21] n = 111 (26.2%); Wang [30] n = 77 (18.2%); Xiong [32] n = 42 (9.91%). Of 424 patients, 175 underwent HS, 208 ACDF, and 41 CDA. Characteristics of included studies are in Table 1, reported outcomes in Table 2, and complications in Table 3.
Risk of bias
MINORS scores for the seven non-randomised studies are shown in Table 4 (range 11–18, mean 16.4). Six studies were considered to have a moderate risk of bias and one study a high risk. The risk of bias assessment of the RCT is seen in Fig. 2: participants were randomised using the odd or even hospital number, giving a high risk of selection bias.
NDI
Measurements of post-operative NDI were extracted from seven studies [12, 13, 15,16,17, 30, 32]. All seven compared HS and ACDF and three HS with CDA [12, 13, 30]. There was no significant difference in NDI after HS versus ACDF (MD = − 1.69; 95% CI − 4.07 to 0.69; p = 0.16; I2 = 83%). Values from Ji et al. [16] and Kang et al. [17] were higher following ACDF than following HS but no standard deviations were provided so they were not included in pooled analysis. NDI scores were not significantly different following CDA compared with HS (MD = 0.57; 95% CI − 3.01 to 4.16; p = 0.75; I2 = 71%).
VAS
Post-operative VAS scores for HS versus ACDF were obtained from all eight studies [12, 13, 15,16,17, 21, 30, 32] and for HS versus CDA from three [12, 13, 30] (Fig. 3). Mende et al. did not provide standard deviations so their data was not included [21]. The pooled estimate did not show favour to any of the procedures: ACDF (MD = − 0.08; 95% CI − 0.43 to 0.26; p = 0.64; I2 = 40%), CDA (MD = − 0.41; 95% CI − 1.17 to 0.34; p = 0.28; I2 = 76%). Values from the last follow-up appointment were used. Four studies reported a combined VAS score for neck and arm pain [12, 13, 17, 30], three provided separate VAS scores for neck and arm pain [16, 21, 32], and one reported VAS arm pain alone [15]. Where two scores were provided, the VAS for arm pain was used as it was common to all.
C2–C7 ROM
The post-operative C2–C7 ROM was reported in seven studies for HS versus ACDF [12, 13, 15,16,17, 30, 32] and three for CDA [12, 13, 30] (Fig. 4). ROM was significantly greater after HS compared with ACDF (MD = 6.14; 95% CI 1.94 to 10.35; p = 0.004; I2 = 74%). There was no significant difference in C2–C7 ROM between HS and CDA (MD = 6.42; 95% CI = − 12.97 to 25.80; p = 0.52; I2 = 98%).
SAS ROM
The post-operative SAS ROM for HS and ACDF was reported by four studies [16, 17, 30, 32] (Fig. 5). One study measured SAS ROM after CDA [30]. Ji et al. reported the relative difference in ROM to the pre-operative ROM; therefore, the data is too heterogeneous for inclusion in the pooled analysis [16]. SAS ROM was significantly lower after HS than after ACDF (MD = − 2.87; 95% CI = − 4.06 to − 1.68; p < 0.00001; I2 = 0%). SAS ROM was significantly greater after HS than after CDA (11.3 ± 2.7 and 10.7 ± 1.5, respectively; p < 0.05) [30].
IAS ROM
The post-operative IAS ROM for HS and ACDF was reported by four studies [16, 17, 30, 32] (Fig. 6). One study measured IAS after CDA [30]. Ji et al. reported the relative difference in ROM compared with the pre-operative ROM; therefore, the data is too heterogeneous for inclusion in the pooled analysis [16]. IAS ROM was significantly lower after HS than after ACDF (MD = − 3.11; 95% CI = − 4.87 to − 1.35; p = 0.0005; I2 = 35%), and after HS compared with CDA (10.0 ± 5.0 and 11.1 ± 1.8, respectively; p < 0.05) [30].
Intra-operative blood loss
Four studies reported intra-operative blood loss during HS and ACDF [16, 17, 30, 32] and one during CDA [30]. There was no significant blood loss for HS versus ACDF (MD = − 14.58; 95% CI − 36.18 to 7.02; p = 0.19; I2 = 93%). Blood loss during CDA was 38.9 ± 9.6 mL compared with 38.8 ± 15.2 mL during HS (p > 0.005) [30]. Hey et al. used the post-operative drop in haemoglobin as a surrogate for blood loss (not included in analysis), which showed no significant difference following HS compared with ACDF or CDA (p > 0.05) [13].
Operation time
Operation time (minutes) was reported by seven studies for HS and ACDF [12, 13, 15,16,17, 30, 32]: there was no significant difference (MD = 9.96; 95% CI − 16.99 to 36.92; p = 0.47; I2 = 99%). Three studies reported the operation time for HS and CDA and there was no significant difference (MD = − 10.67; 95% CI − 26.85 to 5.52; p = 0.20; I2 = 93%) [12, 13, 30].
Return to work
Patients’ return to work following HS and ACDF was reported in three studies [12, 13, 21], and following HS and CDA in two [12, 13]; Mende et al. did not provide standard deviations so data could not be used in the pooled analysis, but reported a shorter return to work for HS than for ACDF by approximately 63 days [21]. Patients who underwent HS returned to work significantly sooner than those after ACDF (MD − 32.01; 95% CI − 33.13 to − 30.90; p < 0.00001; I2 = 0%) and after CDA (MD = − 32.92; 95% CI − 43.58 to − 22.06; p < 0.00001; I2 = 27%).
Complications
All eight studies reported post-operative complications (Table 3; Fig. 7) [12, 13, 15,16,17, 21, 30, 32]. A total of 37 events were reported after HS and 36 after ACDF (OR = 1.45; 95% CI = 0.57 to 3.66; p = 0.44; I2 = 53%). Three studies also reported a total of 13 complications after HS and 6 after CDA [12, 13, 30] (OR = 1.24; 95% CI 0.40 to 3.79; p = 0.71; I2 = 0%). Neither was statistically significant.
Discussion
Hybrid surgery comprised of ACDF and CDA for multilevel CDDD aims to overcome the poor outcomes and contraindications associated with its two component procedures used in isolation [1, 3, 4, 6, 7, 14, 19, 22, 26, 29, 33]. The main findings of this systematic review and meta-analysis are that HS may be associated with greater post-operative C2–C7 ROM, reduced ROM in the adjacent segments, and a quicker return to work than ACDF. CDA patients also returned to work quicker than HS patients. High-quality evidence is lacking, and large robust comparative studies are not available.
HS versus ACDF
Hybrid surgery was associated with a significantly greater post-operative C2–C7 ROM (p = 0.004), which echoes similar reviews [20, 28, 34, 35]. However, some of these included corpectomy procedures in some hybrid constructs [20, 35], which limits the usefulness of comparing their results with our own. Only three included studies reported adjacent segment ROM [17, 30, 32], with one case of ASD reported after HS and three following ACDF (Table 3). HS aims to reduce the incidence of ASD seen after ACDF while preserving cervical spine kinematics [4, 6, 14, 26], and we found significantly lower SAS ROM (p < 0.00001) and IAS ROM (p = 0.0005) after HS than after ACDF, as reported elsewhere in the literature [20, 34, 35].
Patients who had HS returned to work 32 days sooner than ACDF patients (p < 0.00001). There was no significant difference in patients’ functional and pain scores (NDI, VAS) at final follow-up but information in the months immediately following surgery is lacking. Return to work may be also be affected by post-operative care, with different types of collar worn for varying times between groups and between studies [12, 13]. Sociodemographic factors may influence this variable such as the type of work or the government support available. Unfortunately, patient professions are not reported by any paper, but the studies were conducted in different countries (Table 1), making differences in available support likely.
Unlike similar reviews, we found there was no significant difference in blood loss between included studies [20, 28, 34]. Although the ACDF element of HS has been associated with less blood loss than that of CDA [10], the results from meta-analyses of multilevel CDA versus ACDF have been equivocal [31, 39]. The greatest amount of blood loss was recorded by Kang et al. [17] perhaps because their 24 patients required 3-level intervention, whereas the majority in the other studies were 2-level. Jang et al. compared 3-level HS with 3-level ACDF but they did not measure intra-operative blood loss [15].
HS versus CDA
HS patients returned to work approximately 33 days sooner than the CDA group, with no significant difference in functional outcomes. As discussed in relation to HS versus ACDF, post-operative care and sociodemographic factors may influence this, although it is not clear why this strong effect is seen between HS and both its component procedures.
Heterogeneity between the studies may influence the ROM. The majority were 2-level procedures except 3/7 of the HS and 3/7 of the CDA procedures performed by Hey et al. were 3-level operations [13]; however, this represents a small percentage of the total number of HS and CDA operations. All three studies that compared HS with CDA used the ProDisc-C or MOBI-C discs (Table 1) but do not clearly state which were used for each procedure or the reasons behind choosing one over another [12, 13, 30]. A meta-analysis comparing the durability of CDA using different prosthetic devices found that MOBI-C and ProDisc-C were the best and second best, respectively [5]. Durability of the device has implications for long-term complications, although we identified no significant difference in complications. It is difficult to say how a different prosthesis may affect the ROM particularly within a hybrid construct.
Strengths and limitations
We excluded studies in which HS involved vertebral corpectomy, thus reducing potential confounding which such heterogeneity in the procedure may introduce. This is also the only review we could find which attempted to compare HS with both of its constituent procedures. Despite there being less evidence than multilevel ACDF or CDA, some surgeons choose to provide hybrid surgery to a select group of suitable patients who they feel would benefit. This review provides evidence in support of hybrid surgery, which may encourage more surgeons to use it which in turn would provide a greater pool of HS patients that are eligible for inclusion in future research.
A small number of studies met the inclusion criteria which, combined with the low n value, limited the statistical power. The studies also come to different conclusions as to which intervention is favoured. The quality of evidence from the included studies is very low (Appendix 1): most studies are observational with only one RCT, all of which were affected by bias to some degree. The small number of relevant studies means it was not possible to perform subgroup analyses for 3-level or 2-level surgery.
Future systematic reviews on the topic could utilise a network meta-analysis, to robustly ascertain the comparative effectiveness of the three interventions.
Conclusion
Hybrid surgery appears to be an effective treatment with improved post-operative C2–C7 ROM and less ROM in the adjacent segments compared with ACDF alone in the treatment of multilevel CDDD. The paucity of studies, high heterogeneity between studies, and low quality of evidence preclude strong recommendations in favour of HS over other interventions. Large randomised controlled trials under standardised settings and standardised surgical procedures are required to provide high-quality evidence that is currently lacking.
References
Auerbach JD, Jones KJ, Fras CI, Balderston JR, Rushton SA, Chin KR (2008) The prevalence of indications and contraindications to cervical total disc replacement. Spine J 8(5):711–716
Balshem H, Helfand M, Schünemann HJ et al (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64(4):401–406
Bohlman HH, Emery SE, Goodfellow DB, Jones PK (1993) Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 75(9):1298–1307
Bydon M, Xu R, De la Garza-Ramos R, Macki M, Sciubba DM, Wolinsky J-P, Witham TF, Gokaslan ZL, Bydon A (2014) Adjacent segment disease after anterior cervical discectomy and fusion: incidence and clinical outcomes of patients requiring anterior versus posterior repeat cervical fusion. Surg Neurol Int 5(Suppl 3):S74–S78
Chen C, Zhang X, Ma X (2017) Durability of cervical disc arthroplasties and its influence factors: a systematic review and a network meta-analysis. Medicine (Baltimore) 96(6):e5947
Cho SK, Riew KD (2013) Adjacent segment disease following cervical spine surgery. J Am Acad Orthop Surg 21(1):3–11
De La Garza-Ramos R, Xu R, Ramhmdani S, Kosztowski T, Bydon M, Sciubba DM, Wolinsky J-P, Witham TF, Gokaslan ZL, Bydon A (2016) Long-term clinical outcomes following 3- and 4-level anterior cervical discectomy and fusion. J Neurosurg Spine 24:885–891
Findlay C, Ayis S, Demetriades AK (2018) Total disc replacement versus anterior cervical discectomy and fusion. Bone Joint J 100–B(8):991–1001
Gandhi AA, Kode S, DeVries NA, Grosland NM, Smucker JD, Fredericks DC (2015) Biomechanical Analysis of Cervical Disc Replacement and fusion using single level, two level, and hybrid constructs. Spine (Phila Pa 1976) 40(20):1578–1585
Gao WS, Tang XH, Li CJ, Ren B (2018) Comparison of three operative techniques in multilevel cervical spondylotic myelopathy: a meta-analysis. Int JClin Exp Med 11(5):4352–4370
Gornet MF, Lanman TH, Burkus JK, Hodges SD, McConnell JR, Dryer RF, Copay AG, Nian H, Harrell FE (2017) Cervical disc arthroplasty with the Prestige LP disc versus anterior cervical discectomy and fusion, at 2 levels: results of a prospective, multicenter randomized controlled clinical trial at 24 months. J Neurosurg Spine 26(6):653–667
Grasso G (2015) Clinical and radiological features of hybrid surgery in multilevel cervical degenerative disc disease. Eur Spine J 24(S7):842–848
Hey HWD, Hong CC, Long AS, Hee HT (2013) Is hybrid surgery of the cervical spine a good balance between fusion and arthroplasty? Pilot results from a single surgeon series. Eur Spine J 22(1):116–122
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81(4):519–528
Jang S-R, Lee S-B, Cho K-S (2017) A comparison of anterior cervical discectomy and fusion versus fusion combined with artificial disc replacement for treating 3-level cervical spondylotic disease. J Korean Neurosurg Soc 60(6):676–683
Ji GY, Oh CH, Shin DA, Ha Y, Kim KN, Shin HC, Yoon DH (2015) Artificial disk replacement combined with fusion versus 2-level fusion in cervical 2-level disk disease with a 5-year follow-up. J Spinal Disord Tech
Kang L, Lin D, Ding Z, Liang B, Lian K (2013) Artificial disk replacement combined with midlevel ACDF versus multilevel fusion for cervical disk disease involving 3 levels. Orthopedics 36(1):e88–e94
Lee JH, Kim JS, Lee JH, Chung ER, Shim CS, Lee S-H (2014) Comparison of cervical kinematics between patients with cervical artificial disc replacement and anterior cervical discectomy and fusion for cervical disc herniation. Spine J 14(7):1199–1204
Leven D, Meaike J, Radcliff K, Qureshi S (2017) Cervical disc replacement surgery: indications, technique, and technical pearls. Curr Rev Musculoskelet Med 10(2):160–169
Lu VM, Zhang L, Scherman DB, Rao PJ, Mobbs RJ, Phan K (2017) Treating multi-level cervical disc disease with hybrid surgery compared to anterior cervical discectomy and fusion: a systematic review and meta-analysis. Eur Spine J 26(2):546–557
Mende KC, Kahl N, Detzner M, Lefering R, Franke J, Weber F (2015) Comparison of dual level fusion and hybrid treatment in the cervical spine based on patient outcome. J Spine. https://doi.org/10.4172/21657939.1000218
Moatz B, Tortolani PJ (2012) Cervical disc arthroplasty: pros and cons. Surg Neurol Int 3(Suppl 3):S216–S224
Moher D, Liberati A, Tetzlaff J, Altman DG (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–341
Park D-H, Ramakrishnan P, Cho T-H, Lorenz E, Eck JC, Humphreys SC, Lim T-H (2007) Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine 7(3):336–340
Park C-K, Ryu K-S (2018) Are controversial issues in cervical total disc replacement resolved or unresolved?: A review of literature and recent updates. Asian Spine J 12(1):178
Saavedra-Pozo FM, Deusdara RAM, Benzel EC (2014) Adjacent segment disease perspective and review of the literature. Ochsner J 14(1):78–83
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 73(9):712–716
Tian P, Fu X, Li Z-J, Sun X-L, Ma X-L (2015) Hybrid surgery versus anterior cervical discectomy and fusion for multilevel cervical degenerative disc diseases: a meta-analysis. Sci Rep 5(1):13454
Van Eck CF, Regan C, Donaldson WF, Kang JD, Lee JY (2014) The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion: a study of 672 consecutive patients. Spine (Phila Pa 1976) 39(26):2143–2147
Wang K-F, Duan S, Zhu Z-Q, Liu H-Y, Liu C-J, Xu S (2018) Clinical and radiologic features of 3 reconstructive procedures for the surgical management of patients with bilevel cervical degenerative disc disease at a minimum follow-up period of 5 years: a comparative study. World Neurosurg 113:e70–e76
Wu T-K, Wang B-Y, Meng Y, Ding C, Yang Y, Lou J-G, Liu H (2017) Multilevel cervical disc replacement versus multilevel anterior discectomy and fusion: a meta-analysis. Medicine (Baltimore) 96(16):e6503
Xiong Y, Xu L, Yu X et al (2018) Comparison of 6-year follow-up result of hybrid surgery and anterior cervical discectomy and fusion for the treatment of contiguous two-segment cervical degenerative disc diseases. Spine (Phila Pa 1976) 43(20):1418–1425
Yu S, Li F, Yan N, Yuan C, He S, Hou T (2014) Anterior fusion technique for multilevel cervical spondylotic myelopathy: a retrospective analysis of surgical outcome of patients with different number of levels fused. PLoS One 9(3):e91329
Zang L, Ma M, Hu J, Qiu H, Huang B, Chu T (2015) Comparison of hybrid surgery incorporating anterior cervical discectomy and fusion and artificial arthroplasty versus multilevel fusion for multilevel cervical spondylosis: a meta-analysis. Med Sci Monit 21:4057–4067
Zhang J, Meng F, Ding Y, Li J, Han J, Zhang X, Dong W (2016) Hybrid surgery versus anterior cervical discectomy and fusion in multilevel cervical disc diseases. Medicine (Baltimore) 95(21):e3621
Zhao C-M, Chen Q, Zhang Y, Huang A-B, Ding W-Y, Zhang W (2018) Anterior cervical discectomy and fusion versus hybrid surgery in multilevel cervical spondylotic myelopathy: a meta-analysis. Medicine (Baltimore) 97(34):e11973
Zhao H, Cheng L, Hou Y, Liu Y, Liu B, Mundra JJ, Nie L (2015) Multi-level cervical disc arthroplasty (CDA) versus single-level CDA for the treatment of cervical disc diseases: a meta-analysis. Eur Spine J 24(1):101–112
Zhong Z-M, Zhu S-Y, Zhuang J-S, Wu Q, Chen J-T (2016) Reoperation after cervical disc arthroplasty versus anterior cervical discectomy and fusion: a meta-analysis. Clin Orthop Relat Res 474(5):1307–1316
Zou S, Gao J, Xu B, Lu X, Han Y, Meng H (2017) Anterior cervical discectomy and fusion (ACDF) versus cervical disc arthroplasty (CDA) for two contiguous levels cervical disc degenerative disease: a meta-analysis of randomized controlled trials. Eur Spine J 26(4):985–997
Acknowledgements
Mrs Sheila Fisken, Medical Librarian, University of Edinburgh for advice and assistance with an optimal search strategy.
Funding
This study did not receive funding to carry out this research. Dr Salma Ayis was funded by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Due to the nature of the study, informed consent from participants was not required.
Disclaimer
The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, or the Department of Health.
Additional information
Comments
The group from Edinburgh performed a systematic literature review and meta-analysis with the aim to compare clinical and radiological outcomes after hybrid surgery for multilevel cervical degenerative disc disease. Those outcomes were compared against both anterior cervical fusion and motion preserving disc arthroplasty. With a poor quality of underlying included studies that predominantly report on Asian populations, also the results of this pooled analysis have to be interpreted with caution and are unlikely to provide us with clear guidance as to whether this option should be offered to our patients more often. The data, however, point towards at least noninferiority of hybrid surgery. Offering it to selected patients therefore appears reasonable and safe. With more experience gained over time—or should high-quality RCT data provide better evidence—the role of hybrid surgery will be better defined. The authors provide us with a good starting point from where this treatment option can progressively be explored.
Martin N. Stienen
Zurich (CH)/Stanford (USA)
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine degenerative
This study was performed while the corresponding author was located at the University of Edinburgh.
Appendices
Appendix 1
((ACDF OR fusion OR discectomy) OR (disc replacement OR arthroplasty OR CDA OR ADR)) AND hybrid AND cervical
Appendix 2
Grade: HS vs ACDF
Question: HS compared with ACDF for cervical degenerative disc disease
Bibliography: Hybrid surgery versus ACDF or CDA for cervical degenerative disc disease. Cochrane Database of Systematic Reviews [Year], Issue [Issue].

CI: Confidence interval; MD: Mean difference; OR: Odds ratio
Explanation
a. Study Design: Only one of the studies that report this outcome is a RCT.
b. Bias downgraded 1 level: Inherent detection bias when measuring C2-C7 ROM as it is not possible to be blinded to patient's intervention as it is clear on the radiograph if they have a hybrid or ACDF.
c. Inconsistency downgraded 1 level: Statistical heterogeneity was high across all studies, but methodology similar using Cobb angles measured from lateral radiographs.
d. Imprecision downgraded 1 level: Number of participants is low.
e. Bias downgraded 1 level: Detection bias from self-reported outcomes via patient questionnaire, no mention of blinding of the staff assisting with clinical evaluation as to patients' treatment (with the exception of Kang et al).
f. Inconsistency downgraded 1 level: Statistical heterogeneity was high across all studies, but methodology in recording pain scores similar.
g. Inconsistency downgraded 2 levels: Statistical heterogeneity very high, and difference in type of prosthesis and 3-level/2-level surgery between studies may affect this outcome.
h. Moderate statistical heterogeneity
Grade: HS vs CDA
Question: HS compared with CDA for cervical degenerative disc disease
Bibliography: Hybrid surgery versus ACDF or CDA for cervical degenerative disc disease. Cochrane Database of Systematic Reviews [Year], Issue [Issue].

CI: Confidence interval; MD: Mean difference; OR: Odds ratio
Explanation
a. Bias downgraded 1 level: Inherent detection bias as it is not possible to be blinded to patient's intervention as it is clear on the radiograph if they have a disc replacement or a cage fusion.
b. Inconsistency downgraded 1 level: Statistical heterogeneity is high and data from Hey et al are median not mean values.
c. Imprecision downgraded 1 level. Number of patients analysed is very low, 95% CI of average effect size is very wide.
d. Bias downgraded 1 level: Detection bias from self-reported outcomes via patient questionnaire, no mention of blinding of the staff assisting with clinical evaluation as to patients' treatment.
e. Inconsistency downgraded 2 levels: Statistical heterogeneity is high and clinical heterogeneity that could effect this outcome relating to time in collar post op.
f. Imprecision downgraded 1 level: Number of patients analysed is very low.
g. Performance bias and detection bias inherent in surgical procedure and risk of bias from study design, however these are unlikely to affect this outcome.
h. Imprecision downgraded 1 level. Number of patients analysed is very low, but pooled effect estimate does not cross the line of null effect.
Rights and permissions
About this article
Cite this article
Hollyer, M.A., Gill, E.C., Ayis, S. et al. The safety and efficacy of hybrid surgery for multilevel cervical degenerative disc disease versus anterior cervical discectomy and fusion or cervical disc arthroplasty: a systematic review and meta-analysis. Acta Neurochir 162, 289–303 (2020). https://doi.org/10.1007/s00701-019-04129-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04129-3