Abstract
Purpose
The traditional surgical approach to treat multi-level cervical disc disease (mCDD) has been anterior cervical discectomy and fusion (ACDF). There has been recent development of other surgical approaches to further improve clinical outcomes. Collectively, when elements of these different approaches are combined in surgery, it is known as hybrid surgery (HS) which remains a novel treatment option. A systematic review and meta-analysis was conducted to compare the outcomes of HS versus ACDF for the treatment of mCDD.
Methods
Relevant articles were identified from six electronic databases from their inception to January 2016.
Results
From 8 relevant studies identified, 169 patients undergoing HS were compared with 193 ACDF procedures. Operative time was greater after HS by 42 min (p < 0.00001), with less intraoperative blood loss by 26 mL (p < 0.00001) and shorter return to work by 32 days (p < 0.00001). In terms of clinical outcomes, HS was associated with greater C2–C7 range of motion (ROM) preservation (p < 0.00001) and less functional impairment (p = 0.008) after surgery compared to ACDF. There was no significant difference between HS and ACDF with respect to postoperative pain (p = 0.12). The postoperative course following HS was not significantly different to ACDF in terms of length of stay (p = 0.24) and postoperative complication rates (p = 0.18).
Conclusions
HS is a novel surgical approach to treat mCDD, associated with a greater operative time, less intraoperative blood loss and comparable if not superior clinical outcomes compared to ACDF. While it remains a viable consideration, there is a lack of robust clinical evidence in the literature. Future large prospective registries and randomised trials are warranted to validate the findings of this study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The frequency of cervical disc disease (CDD) increases with age, with over 85 % of the population aged over 60 expected to have severe degeneration of at least one cervical level [1]. Additionally, one study observed symptomatic CDD in 25 % of young adults [2]. Multi-level cervical disc disease (mCDD) is a condition most commonly seen in the elderly that can present with neurologic deficit and impact on quality of life [3].
Anterior cervical discectomy and fusion (ACDF) has been the gold standard for treating mCDD for many years [4]. Although ACDF preserves neurological function of the spinal cord effectively, this approach has been associated with significant decrease in range of motion (ROM) and increase in long-term complications such as adjacent segment disease [5]. As a result, a variety of alternative motion-sparing surgical procedures have been developed [6–9]. These include artificial disc replacement (ADR) by arthroplasty and anterior cervical corpectomy and fusion (ACCF). In the context of multi-level surgery, ADR [10, 11] has been proven to be beneficial in terms of cervical spine motion preservation after surgery and ACCF [12] is associated with high fusion rates.
When a surgical approach consists of elements of ACDF, ADR and ACCF in varying proportions, it can be considered as a hybrid of these approaches, termed hybrid surgery (HS). HS is seen as a novel option in treating mCDD where not all disease levels may meet acceptable criteria for one particular approach [13]. The use of HS in the treatment of mCCD is relatively novel and thus its multi-level effectiveness is not thoroughly established. This is because the different approaches that constitute HS for mCDD may each possess unique indication criteria, exclusive to the other HS components. Rather than to challenge the indications for the different elements that constituted the HS, the aim of this study was to compare the outcomes of mCCD surgery treated by novel HS, a collection of elements from multiple approaches, to that of traditional ACDF, a single, controlled approach.
Methods
Literature search strategy
The present review was conducted according to PRISMA guidelines and recommendations [14, 15]. Electronic searches were performed using Ovid Medline, PubMed, Cochrane Central Register of Controlled Trials (CCTR), Cochrane Database of Systematic Reviews (CDSR), ACP Journal Club and Database of Abstracts of Review of Effectiveness (DARE) from their dates of inception to January 20 [1] 6. To achieve maximum sensitivity of the search strategy and identify all studies, we combined the terms: “hybrid”, “replacement or arthroplasty”, “fusion” and “cervical” as either keywords or MeSH terms. The reference lists of all retrieved articles were reviewed for further identification of potentially relevant studies. All identified articles were systematically assessed using the inclusion and exclusion criteria.
Selection criteria
Eligible comparative studies for the present systematic review and meta-analysis included those in which: (1) study designs were comparative studies, either RCTs or non-RCTs, (2) population including patients with multi-level cervical degenerative disc disease, (3) intervention group hybrid surgery (ADR with another approach), (4) control group being ACDF, (5) outcomes reporting at least one of the following measurements: surgical outcomes, intraoperative blood loss; operative time; length of stay; complications; and/or preoperaitve and postoperative functional outcomes, C2–C7 range of motion (ROM); subjective pain perception Visual Analogue Scale (VAS); neck disability index (NDI); superior and/or inferior adjacent segment ROM; and functional Japanese Orthopaedic Association (JOA) scale. Measurements were standardised across studies after analysing for heterogeneity and reported methodology. Excluded studies included those where patients had a neoplastic indication (metastasis or myeloma), infection, trauma, spondylolisthesis, or serious osteoporosis. When institutions published duplicate studies with accumulating numbers of patients or increased lengths of follow-up, only the most complete reports were included for quantitative assessment at each time interval. All publications were limited to those involving human subjects and in the English language. Abstracts, case reports, conference presentations, editorials and expert opinions were excluded. Review articles were omitted because of potential publication bias and duplication of results.
Data extraction and critical appraisal
All data were extracted from article texts, tables and figures. Two investigators independently reviewed each retrieved article (K.P., L.Z.) Discrepancies between the two reviewers were resolved by discussion and consensus with a third reviewer (V.M.L.).
Because quality scoring is controversial in meta-analyses of observational studies, two reviewers independently appraised each article included in our analysis according to a critical review checklist of the Dutch Cochrane Centre proposed by MOOSE [16]. The key points of this checklist include: (1) clear definition of study population; (2) clear definition of outcomes and outcome assessment; (3) independent assessment of outcome parameters; (4) sufficient duration of follow-up; (5) no selective loss during follow-up; and (6) important confounders and prognostic factors identified. Discrepancies between the two reviewers were resolved by discussion and consensus.
Statistical analysis
The odds ratio (OR) or weighted mean difference (WMD) was used as a summary statistic. In the present study, both fixed- and random-effect models were tested. In the fixed-effects model, it was assumed that treatment effect in each study was the same, whereas in a random-effects model, it was assumed that there were variations between studies. χ2 tests were used to study heterogeneity between trials. I 2 statistic was used to estimate the percentage of total variation across studies, owing to heterogeneity rather than chance, with values greater than 50 % considered as substantial heterogeneity. I 2 can be calculated as: I 2 = 100 % × (Q − df)/Q, with Q defined as Cochrane’s heterogeneity statistics and df defined as degree of freedom. If there was substantial heterogeneity, the possible clinical and methodological reasons for this were explored qualitatively. In the present meta-analysis, the results using the random-effects model were presented to take into account the possible clinical diversity and methodological variation between studies. Specific analyses considering confounding factors were not possible because raw data were not available. All P values were two-sided. All statistical analyses were conducted with Review Manager Version 5.3.3 (Cochrane Collaboration, Software Update, Oxford, United Kingdom).
Results
Literature search
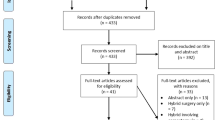
A total of 521 references were identified through six electronic database searches (Fig. 1). After exclusion of duplicate or irrelevant references, 505 potentially relevant articles were retrieved. After detailed evaluation of these articles, 27 studies remained for assessment. Manual search of reference lists yielded one new study. After applying the selection criteria, eight comparative studies were selected for analysis. The study characteristics of these trials are summarised in Table 1. Baseline patient characteristics and risk factors are summarised in Table 2. The quality assessment of each included study is presented in Table 3.
Demographics
The included studies describe a total of 360 patients treated for mCDD, with 169 (46.9 %) and 193 (53.1 %) treated by HS and ACDF, respectively. Their demographic features are reported in Table 1. Mean age ranged from 44.2 to 53.6 years in the HS group and from 47.3 to 55.3 years in the ACDF group. Proportion of males ranged from 42.8 to 66.7 % in the HS group and 45.0 to 67.2 % in the ACDF group. Average number of levels treated was 2.46 and 2.44 in the HS and ACDF groups, respectively. There was no statistically significant difference in these features between the HS and ACDF groups.
Operative time
Data were extracted from six studies, three 2-level and three 3-level studies (Fig. 2a). Overall operative time was significantly longer in HS than ACDF (MD 41.82 min; 95 % CI 40.60–43.03; p < 0.00001) with pooled means of 135 vs 122 min, respectively. The difference was significant in 2-level studies (MD 44.30 min; 95 % CI 4306–45.55; p < 0.00001), however, not 3-level studies (p = 0.09). Subgroup difference was significant (p < 0.00001).
Intraoperative blood loss
Data were extracted from four studies, one 2-level and three 3-level studies (Fig. 2b). Overall intraoperative blood loss was significantly lower after HS than ACDF (MD 25.53 mL; 95 % CI −36.13 to −14.93; p < 0.00001) with pooled means of 167 vs 202 millilitres, respectively. The difference was significant in the 2-level study (MD −46.00 mL; 95 % CI −62.57 to −29.43; p < 0.00001), however, not 3-level studies (p = 0.11). Subgroup difference was significant (p = 0.002).
Length of stay
Data were extracted from two studies, one 2-level and one 3-level studies (Fig. 2c). Overall length of stay was not significantly different after HS or ACDF (p = 0.24). The difference was not significant in the 2-level study (p = 0.14) or 3-level study (p = 0.59). Subgroup difference was not significant (p = 0.30).
Complications
Data were extracted from eight studies, where three 2-level and four 3-level studies observed complications (Table 2; Fig. 3). Overall complication rates were not significantly associated with either HS or ACDF (p = 0.18). Complications were more associated with HS than ACDF in 2-level (OR 2.08; 95 % CI 1.13–6.96; p = 0.03), however, this was not observed in 3-level studies (p = 0.63). Subgroup difference was not significant (p = 0.06).
Return to Work Time
Data were extracted from two 2-level studies (Fig. 4). Overall return to work time was significantly earlier after HS than ACDF (MD −32.01 d; 95 % CI −33.13 to −30.90; p < 0.00001) with pooled means of 27 vs 74 days, respectively.
C2–C7 range of motion (ROM)
Pre- and postoperative C2–C7 ROM measurements were extracted from seven studies, three 2-level and four 3-level studies. Overall postoperative C2–C7 measurements were significantly greater after HS than ACDF (MD, 9.22; 95 % CI 6.97–11.46; p < 0.00001) with pooled means of 41.9 vs 32.5, respectively (Fig. 5a). Further comparisons are reported in Table 4.
Visual analogue scale (VAS)
Pre- and postoperative VAS measurements were extracted from six studies, three 2-level and three 3-level studies. Overall postoperative VAS measurements were not significantly different after HS than ACDF (p = 0.12, Fig. 5b). Further comparisons are reported in Table 4.
Neck disability index (NDI)
Pre- and postoperative NDI measurements were extracted from four studies, two 2-level and two 3-level studies. Overall postoperative NDI measurements were significantly lower after HS than ACDF (MD −1.33; 95 % CI −2.32 to −0.34; p = 0.008) with pooled means of 8.67 vs 10.22, respectively (Fig. 5c). Further comparisons are reported in Table 4.
Superior adjacent segment range of motion (ROM)
Pre- and postoperative superior adjacent segment ROM measurements were extracted from three studies, one 2-level and two 3-level studies. Overall postoperative superior adjacent ROM measurements were significantly lower after HS than ACDF (MD −3.75; 95 % CI −5.97 to −1.52; p = 0.0009) with pooled means of 14.77 vs 19.17, respectively (Supplementary Fig. 1a). Further comparisons are reported in Supplementary Table 1.
Inferior adjacent segment range of motion (ROM)
Pre- and postoperative inferior adjacent segment ROM measurements were extracted from three studies, one 2-level and two 3-level studies. Overall postoperative inferior adjacent ROM measurements were significantly lower after HS than ACDF (MD −3.05; 95 % CI −4.75 to −1.34; p = 0.0005) with pooled means of 13.31 vs 16.47, respectively (Supplementary Fig. 1b). Further comparisons are reported in Supplementary Table 1.
Japanese orthopaedic association (JOA) scale
Pre- and postoperative JOA measurements were extracted from four studies, one 2-level and three 3-level studies. Overall postoperative JOA measurements were significantly greater after HS than ACDF (MD 0.56; 95 % CI 0.26–0.86; p = 0.0002) with pooled means of 14.20 vs 13.80, respectively (Supplementary Fig. 1c). Further comparisons are reported in Supplementary Table 1.
Discussion
The surgical rationale behind HS in treating mCDD is to achieve the benefits of ACDF as well as those of the other approaches. Overall, HS showed greater operative time, less intraoperative blood loss and earlier return to work compared to ACDF. Length of stay and postoperative complications between HS and ACDF were not significantly different. After HS, postoperative C2–C7 ROM and functional NDI outcomes were improved, while pain VAS outcomes were comparable to ACDF. Lower postoperative superior and inferior segment ROM measurements were observed after HS.
Given the novelty of HS, it is not necessarily surprising a longer operative time than ACDF has been demonstrated. During the advent of cervical ADR, a large Food and Drugs Administration (FDA) trial [17] showed operative time compared to ACDF was significantly longer. This was attributed to the time required to learn the new technique. The current case for HS is remarkably similar given its early stage of use. Given that the operative time would include any significant amounts of teaching and clarification, as well as operating, it may explain the observation that HS involves significantly less intraoperative blood loss despite a longer operative time.
From a postoperative standpoint, it has been posited that both complication rates and length of stay would be comparable between HS and ACDF due to the use of similar surgical approaches and nerve decompression procedures [18, 19]. What is interesting is that HS patients seem to return to work earlier than ACDF patients. This may be due to greater fusion rates and reduced postoperative immobilisation with cervical instrumentation insertion during ACDF which can only be observed after discharge [5, 20].
In terms of HS and its components, it would seem that the relationship between number of levels treated with HS and clinical outcomes is not clearly linear. As a reference, Bohlman et al. reported fusion rates after ACDF at one-, two-, three- and four-level operations were 89, 73, 73 and 0 %, respectively [4]. Other studies comparing treatment for single-level cervical disc disease and mCDD showed no major clinical differences in outcomes between them in with either ACDF [21] or ADR [11] individually.
There is currently a lack within the literature of comparative outcomes between 2- and 3-level HS operations and they are mostly only inferable from analyses of individual HS components. A comparison of 2-level ACCF and 3-level ACDF showed no significant difference in outcomes [22]. Studies of ACDF only have established that a direct correlation exists between the number of construct fusion levels and the occurrence of pseudarthrosis [4, 23, 24]. Should such a tendency for complicated recovery extend beyond pseudarthrosis, it could then be associated with the subgroup differences seen in the follow-up parameters of this review. Technically ADR inclusion within HS should circumvent the concern for non-union and theoretical decrease overall pseudarthrosis rates when implemented in multi-levels [10]. Future comparative studies are needed to investigate the differences between 2- and 3-level HS outcomes more fully.
It is worth noting the difference between clinical outcomes of NDI and VAS between 2- and 3-level studies, with the former subgroup not detecting significance for either outcome while the latter subgroup detecting significance in both outcomes. It is difficult to determine the exact reason for this observation as there are many potential confounding factors. These include the nature of 3-level surgery which involves a vertebral body at both ends and any bias in operation based on the same geographical location.
Limitations
This study was able to extensively search the current literature for all examples of HS–this includes ACDF, ADR, and ACCF. However, a consequence of this inherent variation of HS components may weaken the implications derived which may be dependent on each component to different degrees. This would be overcome with larger studies. Furthermore, this study remains severely limited by the small size and number of studies that compare the clinical outcomes of HS to the more traditional ACDF. While this currently renders analysis difficult to ascertain significance in more outcomes, it does illustrate the need to continue to evaluate novel approaches such as HS to fully evaluate their applicability.
Another constraint on this study was the low quality of evidence afforded by the currently available literature. Although the challenges of designing higher quality comparative studies involving novel neurosurgical techniques must be recognised, the accuracy and precision of these studies are compromised by many factors. First, the entire cohort of 362 cases was studied over an accumulative 35-year study period, indicating a very low accrual rate per study which is reflective of the small cohort sizes as well. Second, the retrospective or ambispective nature of most studies poorly controls for selection and observation biases. And third, most studies were observational in nature which limits the validity of reported outcomes. The credibility of the evidence in the future would be strengthened by larger, perhaps multi-institutional, more prospective and randomised controlled trials.
In addition, the validity of the comparative postoperative courses following ACDF vs HS needs to be clarified with long-term studies. This is due to the long-term nature of complications such as adjacent segment disease which only manifest many years after surgery [5]. There is a paucity of comparative data in the literature for long-term follow-up studies investigating ACDF vs HS, as well as studies reporting adjacent segment disease. Only Kan et al. [25] and Kang et al. [26] reported adjacent segment disease with the former being the only paper to report nonzero outcomes for both ACDF and HS. Given it is also the reduction in these long-term complications associated with ACDF which provide impetus to explore alternative treatment strategies for mCDD, the true effectiveness of such strategies including HS can only be warranted once their effects on these long-term complications are elucidated as well.
Finally, the novel and variable nature of HS currently limits the significance of these early findings. It is the unstandardized mixture of different approaches in the HS between studies that challenges the homogeneity of the HS operation for comparative purposes. Although, the exact indications and surgical detail for each HS performed in each study is beyond the scope of this study, every effort was made to clarify the components involved. The extent to which including various HS components from study to study affects the validity of the outcomes is difficult to ascertain at this moment, due to the aforementioned limitations. Nonetheless, these findings indicate that the concept of HS is a comparable concept in mCDD treatment and future investigations into the impact of its makeup are warranted. This particular consideration serves as an important reminder that the term ‘hybrid surgery’ remains more of a theoretical concept rather than that a single, exact practice.
Conclusion
Based on the currently available literature, HS appears to be a safe and feasible alternative surgical option in the treatment of mCDD in select patients. Future large, prospective, long-term randomised controlled trials are needed to fully elucidate the effectiveness of this surgery in treating mCDD compared to the current gold standard of ACDF.
References
Matsumoto M, Yoshikazu F, Suzuki N et al (1998) MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br 80(1):19–24
Siivola SM, Levoska S, Tervonen O, Ilkko E, Vanharanta H, Keinanen-Kiukaanniemi S (2002) MRI changes of cervical spine in asymptomatic and symptomatic young adults. Eur Spine J 11(4):358–363
Rao RD, Gourab K, David KS (2006) Operative treatment of cervical spondylotic myelopathy. J Bone Joint Surg Am 88(7):1619–1640
Bohlman H, Emery S, Goodfellow D, Jones P (1993) Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 75(9):1298–1307
Hilibrand A, Carlson G, Palumbo M, Jones P, Bohlman HH (1999) radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81(4):519–528
Song KJ, Lee KB, Song JH (2012) Efficacy of multilevel anterior cervical discectomy and fusion versus corpectomy and fusion for multilevel cervical spondylotic myelopathy: a minimum 5-year follow-up study. Eur Spine J 21(8):1551–1557
Mummaneni PV, Kaiser MG, Matz PG et al (2009) Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. J Neurosurg Spine 11(2):130–141
Chen J, Xu L, Jia YS et al (2016) Cervical anterior hybrid technique with bi-level Bryan artificial disc replacement and adjacent segment fusion for cervical myelopathy over three consecutive segments. J Clin Neurosci 27:59–62
Barbagallo GM, Assietti R, Corbino L et al (2009) Early results and review of the literature of a novel hybrid surgical technique combining cervical arthrodesis and disc arthroplasty for treating multilevel degenerative disc disease: opposite or complementary techniques? Eur Spine J 18(Suppl 1):29–39
Cardoso MJ, Rosner MK (2010) Multilevel cervical arthroplasty with artificial disc replacement. Neurosurg Focus 28(5):E19
Huppert J, Beaurain J, Steib JP et al (2011) Comparison between single- and multi-level patients: clinical and radiological outcomes 2 years after cervical disc replacement. Eur Spine J 20(9):1417–1426
Ashkenazi E, Smorgick Y, Rand N, Millgram M, Mirovsky Y, Floman Y (2005) Anterior decompression combined with corpectomies and discectomies in the management of multilevel cervical myelopathy: a hybrid decompression and fixation technique. J Neurosug Spine 3(3):205–209
Auerbach JD, Jones KJ, Fras CI, Balderston JR, Rushton SA, Chin KR (2008) The prevalence of indications and contraindications to cervical total disc replacement. Spine J 8(5):711–716
Moher D, Liberati A, Tetzlaff J, Althman D (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PloS Med 6(7):e1000097
Phan K, Mobbs RJ (2015) Systematic reviews and meta-analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg. doi:10.3978/jss.2015.06.01
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283(15):2008–2012
Murrey D, Janssen M, Delamarter R et al (2009) Results of the prospective, randomized, controlled multicenter food and drug administration investigational device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine J. 9(4):275–286
Ding F, Jia Z, Wu Y, Li C, He Q, Ruan D (2014) Fusion-nonfusion hybrid construct versus anterior cervical hybrid decompression and fusion: a comparative study for 3-level cervical degenerative disc diseases. Spine (Phila Pa 1976) 39(23):1934–1942
Mao N, Wu J, Zhang Y et al (2015) A Comparison of Anterior Cervical Corpectomy and Fusion Combined With Artificial Disc Replacement and Cage Fusion in Patients With Multilevel Cervical Spondylotic Myelopathy. Spine (Phila Pa 1976) 40(16):1277–1283
Bose B (2001) Anterior cervical instrumentation enhances fusion rates in multilevel reconstruction in smokers. J Spinal Disord 14(1):3–9
Choi MK, Kim SB, Park CK, Kim SM (2016) Comparison of the clinical and radiologic outcomes obtained with single- versus two-level anterior cervical decompression and fusion using stand-alone PEEK cages filled with allograft. Acta Neurochir (Wien) 158(3):481–487
Lau D, Chou D, Mummaneni PV (2015) Two-level corpectomy versus three-level discectomy for cervical spondylotic myelopathy: a comparison of perioperative, radiographic, and clinical outcomes. J Neurosurg Spine 23(3):280–289
Phillips F, Carlson G, Emery S, Bohlman HH (1997) Anterior cervical pseudarthrosis. Natural history and treatment. Spine (Phila Pa 1976) 22(14):1585–1589
Shen H, Buchowski J, Yeom JS, Liu G, Lin N, Riew KD (2010) Pseudarthrosis in multilevel anterior cervical fusion with rhBMP-2 and allograft. Spine 35(7):747–753
Kan L, Kang J, Gao R, Chen X, Jia L (2014) Clinical and radiological results of two hybrid reconstructive techniques in noncontiguous 3-level cervical spondylosis. J Neurosurg Spine 21(6):944–950
Kang L, Lin D, Ding Z, Liang B, Lian K (2013) Artificial disk replacement combined with midlevel ACDF versus multilevel fusion for cervical disk disease involving 3 levels. Orthopedics 36(1):e88–e94
Grasso G (2015) Clinical and radiological features of hybrid surgery in multilevel cervical degenerative disc disease. Eur Spine J 24(Suppl 7):842–848
Hey HW, Hong CC, Long AS, Hee HT (2013) Is hybrid surgery of the cervical spine a good balance between fusion and arthroplasty? Pilot results from a single surgeon series. Eur Spine J 22(1):116–122
Ji GY, Oh CH, Shin DA, et al. (2015) Artificial disk replacement combined with fusion versus 2-level fusion in cervical 2-level disk disease with a 5-year follow-up. J Spinal Disord Tech, [Epub ahead of print]
Mende K, Kahl N, Detzner M, Lefering R, Franke J, Weber F (2015) Comparison of dual level fusion and hybrid treatment in the cervical spine based on patient outcome. J Spine 4(2):1–5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest of funding sources to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lu, V.M., Zhang, L., Scherman, D.B. et al. Treating multi-level cervical disc disease with hybrid surgery compared to anterior cervical discectomy and fusion: a systematic review and meta-analysis. Eur Spine J 26, 546–557 (2017). https://doi.org/10.1007/s00586-016-4791-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4791-y