Abstract
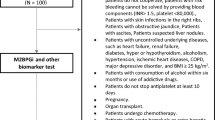
Assessing liver fibrosis is important for predicting the efficacy of antiviral therapy and patient prognosis. Liver biopsy is the gold standard for diagnosing liver fibrosis, despite its invasiveness and problematic diagnostic accuracy. Although noninvasive techniques to assess liver fibrosis are becoming important, reliable serum surrogate markers are not available. A glycoproteomics study aimed at identifying such markers discovered Mac 2-Binding Protein Gylcan Isomer (M2BPGi), which is a reliable marker for assessing liver fibrosis in patients with viral hepatitis and other fibrotic liver diseases such as primary biliary cholangitis, biliary atresia, autoimmune hepatitis, and nonalcoholic fatty liver disease. M2BPGi predicts the development of hepatocellular carcinoma (HCC) in patients infected with hepatitis B and C as well as the prognosis of liver cirrhosis in those with HCC after therapy. The unique features of M2BPGi are as follows: (1) cut-off values differ for the same stages of fibrosis according to the cause of fibrosis; and (2) M2BPGi levels rapidly decrease after patients achieve a sustained antiviral response to hepatitis C virus. These observations cannot be explained if M2BPGi levels reflect the amount of fibrotic tissue. Hepatic stellate cells (HSCs) secrete M2BPGi, which may serve as a messenger between HSCs and Kupffer cells via Mac-2 (galectin 3) that is expressed in Kupffer cells during fibrosis progression. Here we show that M2BPGi is a surrogate marker for assessing HSC activation. These findings may reveal the roles of HSCs in extrahepatic fibrotic disease progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic liver disease (CLD) is a serious health concern worldwide, and infections associated with hepatitis B virus (HBV) and hepatitis C virus (HCV), alcohol abuse, primary biliary cholangitis, and nonalcoholic fatty liver disease (NAFLD) are the common predisposing conditions for developing liver fibrosis and cirrhosis [1]. Without proper management, CLD progresses to liver fibrosis and consequently leads to liver cirrhosis, which increases morbidity and mortality caused by portal hypertension, hepatic insufficiency, and the development of hepatocellular carcinoma (HCC) [2, 3]. The prognosis and treatment of patients with CLD varies depending on the stage of fibrosis, and therefore the diagnosis of the stage of fibrosis, is clinically important [4,5,6]. However, the diagnosis of liver cirrhosis is challenging [1].
Although liver biopsy is considered the gold standard for stratifying hepatic fibrosis [7, 8], it is invasive, its diagnostic value is limited by sampling error, and histologic interpretations can vary [1, 9,10,11,12]. Furthermore, repeated liver biopsies to monitor liver fibrosis are not feasible in a routine clinical setting [1, 13]. Therefore, noninvasive tests to assess liver fibrosis have emerged, which include elastographic techniques [14,15,16,17], serum biomarkers such as hyaluronic acids, type IV collagen, and type III procollagen-N-peptide [18] as well as surrogate markers (e.g., the AST-to-platelet ratio index (APRI) [19], and the FIB-4 index [20]). Among elastographic techniques, transient elastography (TE) and magnetic resonance elastography (MRE) are widely accepted. Several major manufacturers of ultrasound instrumentation recently have developed ultrasound systems that perform elastographic imaging. Furthermore, a novel marker for assessing liver fibrosis, M2BPGi (called WFA+-M2BP), was recently introduced. In this review, we summarize the biological profiles and clinical applications of M2BPGi.
Mac-2 binding protein
The 90K/Mac-2 binding protein (M2BP) is a secreted glycoprotein that is present in the extracellular matrix of several tissues [21], and elevated levels are present in certain tumors and in people with viral infections [21]. In vitro, human M2BP induces the production of interleukin (IL)-1, IL-6, and other cytokines by blood monocytes [22]. A prominent feature of human M2BP is its oligomerization to form large ring structures, which resemble a “powdered sugar doughnut” covered with 70–112 N-glycans [23]. M2BP is extensively glycosylated and interacts with galectin-3 (former name, Mac-2), and it interacts with other extracellular proteins such as collagens IV, V, and VI, fibronectin, and nidogen [23]. M2BP binds galectin-3 on the cell surface and induces homotypic cell aggregation [23].
Sources and the role of M2BPGi in liver fibrosis
Bekki et al. [24] found that hepatic stellate cells (HSCs) are the source of M2BPGi in subpopulations of liver-derived cells such as HSCs, Kupffer cells, endothelial cells, biliary epithelial cells, and hepatocytes. An in vitro study found that the addition of exogenous M2BPGi enhances Mac-2 (galectin 3) expression by Kupffer cells. Furthermore, in cocultures of HSCs and Kupffer cells, alpha-SMA expression by HSCs is increased, which is reduced by Mac-2 depletion from Kupffer cells. These findings suggest that M2BPGi is a juxtacrine-acting messenger sent by HSCs to Kupffer cells during liver fibrosis and that it plays an important role in the progression of fibrosis (Fig. 1). Thus, M2BPGi levels reflect the activation of HSCs during the progression of liver fibrosis, in contrast to the amount of collagen. This may explain the rapid decrease of M2BPGi levels after patients with hepatitis C achieve a sustained virus response (SVR).
An immunohistochemical analysis of cirrhotic human liver found that Mac-2 (galectin 3) and M2BPGi are expressed by CD68-positive cells, which are likely Kupffer cells. Therefore, M2BPGi may interact with Mac-2-positive cells to induce biological activity. Mac-2 is involved in diverse functions such as cell adhesion, growth regulation, cytokine production, T cell apoptosis, and immune responses. For example, Kianoush et al. [25] suggest that Mac-2 induces M2 polarization of macrophages, and other studies indicate that Mac-2 may stimulate cancer progression [26]. Thus, the biological activities of M2BPGi mediated by Mac-2 may explain the high incidence of the development of HCC development in patients with high M2BPGi levels.
Discovery of a new marker for diagnosing liver fibrosis
Kuno et al. [27, 28] and Narimatsu [29] used glycoproteomics techniques to identify biomarkers of liver fibrosis. Glycoproteomics uses comprehensive high-throughput methods to analyze glycosylation sites, glycan structures, and peptide sequences. The investigators cited above focused on the glyco-alteration of α1-acid glycoprotein (AGP), an acute-phase protein that is secreted mainly by the liver. Glyco-alteration of AGP occurs during cirrhosis and acute and chronic inflammation. Thus, the signal patterns of 12 selected lectins reflect fibrosis-associated glyco-alterations of AGP [27]. Furthermore, a fully automated glycan-based immunoassay, called FastLec-Hepa, was developed to search for serum biomarkers for liver fibrosis using a single glycoprotein rather than sets of glycoproteins [28]. FastLec-Hepa automatically detects unique fibrosis-related glycol-alterations of hyperglycosylated Mac-2 binding protein present in serum. Six candidate lectins were selected that bind M2BP [28]. After analyzing sera from patients with different stages of fibrosis, Wisteria floribunda agglutinin (WFA) was found to be superior to the other five lectins for diagnosing liver fibrosis. This glycoprotein (WFA+-Mac2 binding protein) is named Mac-2 binding protein glycosylation isomer (M2BPGi).
Measurement of M2BPGi
M2BPGi is measured using a sandwich immunoassay with anti-WFA and anti-M2BP antibodies. M2BP enriched from serum is added to WFA-coated agarose in a microtube, immunoprecipitated, and analyzed using 5–20% gradient SDS–polyacrylamide electrophoresis under reducing conditions [28]. Alternatively, M2BPGi is measured using a fully automated HSCL-2000i Immunoanalyzer (Sysmecs Co., Hyogo, Japan) [29]. The values of M2BPGi conjugated to WFA are indexed to the values calculated as follows:
where [M2BPGi]sample represents the M2BPGi count of the serum sample (PC, positive control; NC, negative control). The positive control is supplied as a calibration solution that is preliminarily standardized to yield COI = 1.0.
Clinical significance of M2BPGi for the assessment of liver fibrosis
Kuno et al. [28] found that M2BPGi is the most precise predictor of severe fibrosis or liver cirrhosis compared with markers such as the FIB-4 index and hyaluronic acid. Moreover, Toshima et al. [30] found the following: 1. Only histologically diagnosed fibrosis stage correlates with M2BPGi levels. 2. The area under the curve (AUC) of fibrosis (F ≥ 3) using M2BPGi is similar to that determined using ultrasound-based virtual touch tissue quantification. 3. The AUC values of M2BPGi are superior to those of serum surrogate markers such as APRI, hyaluronic acids, and type 4 collagen. These findings suggest that M2BPGi may serve as the most reliable serum biomarker. Moreover, the usefulness of M2BPGi as a marker for assessing liver fibrosis is shown in a study that enrolled patients infected with chronic hepatitis C [28, 31, 32] or B virus [33,34,35,36,37]. Recent studies show that M2BPGi is a useful marker for monitoring the improvement of patients with liver fibrosis after achieving an SVR following antiviral therapy [38, 39].
M2BPGi is useful for assessing liver fibrosis in patients with primary biliary cirrhosis [40, 41], biliary atresia [42], autoimmune hepatitis [43], nonalcoholic fatty liver disease [44,45,46,47,48], and hepatitis B or C infection. A meta-analysis confirms that M2BPGi is a reliable predictor for staging liver fibrosis [49]. Although M2BPGi is a novel marker for assessing liver fibrosis, M2BPGi COI values may differ among patients stratified according to the cause of liver fibrosis, even for those with the same stage of fibrosis (Table 1). Nishikawa et al. [50] found that M2BPGi levels in patients with chronic hepatitis C are higher compared with those of patients with chronic hepatitis B infection, even for those with the same degree of liver fibrosis. Patients with nonalcoholic steatohepatitis (NASH) have the lowest M2BPGi levels compared with those of patients with chronic hepatitis C or B infection. The histological criteria used to diagnose liver fibrosis in patients with NASH differ from those with chronic hepatitis B or C infection. However, in patients with advanced cirrhosis with NASH [51], the M2BPGi levels are much lower compared with those of patients with chronic hepatitis B or C infection.
Another unique aspect of M2BPGi is its rapid decrease after treatment of hepatitis C. For example, Nagata et al. [52] found that the M2BPGi values of 64 patients who achieved SVR significantly decreased after completing treatment. However, in 12 patients without SVR, there were no significant differences between serum M2BPGi values before and after treatment. Because rapid improvement of liver fibrosis beyond 24-week post-treatment is unlikely, even in SVR patients, these studies suggest that M2BPGi values may not reflect the amount of fibrous tissue.
M2BPGi reflects liver function, the effects of antiviral therapy, and liver failure
Yamasaki et al. [31] studied patients with chronic hepatitis C and found that M2BPGi correlates with the stage of fibrosis, alpha-fetoprotein (AFP), albumin, AST, platelets, sex, HCV core antigen, total bilirubin, and age. Other studies show that M2BPGi levels significantly correlate with the Child–Pugh class and the MELD score, and serve as a marker of fibrosis [53, 54]. Moreover, M2BPGi is a useful marker for predicting the efficacy of direct-acting agent-based therapy, including regimens with or without interferon for treating chronic hepatitis C infection [55, 56]. In patients with hepatitis B infection, M2BPGi levels that are > 1.55 COI are poor significant predictors that are linked to the loss of HBeAg or seroconversion of patients positive for hepatitis B e-antigen [57]. Furthermore, Hanai et al. [53] and Hasegawa et al. [58] found that M2BPGi is a useful predictor of the prognosis of patients with liver cirrhosis (Table 2).
Okuda et al. [59] found that preoperative M2BPGi predicts posthepatectomy liver failure, and Morio et al. [60] found that M2BPGi increases in patients with acute liver injury and decreased after recovery. They suggested that M2BPGi might reflect liver fibrosis and other factors such as liver inflammation, liver damage, and hepatocyte regeneration.
Predicting the development of HCC
Several studies show that elevated serum M2BPGi levels predict the development of HCC (Table 3). For example, Yamasaki et al. [31] found that in patients with chronic hepatitis C infection with M2BPGi ≥ 4, the cumulative 5-year incidence of HCC is 77%, although for those with COI = 1–4 or those with COI < 1, the cumulative 5-year incidence is 31.6% and 3.1%, respectively.
There is a high incidence of HCC in patients with chronic hepatitis C infection and elevated serum M2BPGi levels [61]. In patients with chronic hepatitis C infection who reach an SVR and who receive antiviral therapy, a high M2BP value is a significant risk factor for the development of HCC [28, 31, 62, 63]. Furthermore, there is a high incidence of HCC in patients with chronic hepatitis B infection and elevated serum M2BPGi levels [64,65,66,67]. A meta-analysis supports the hypothesis that an elevated M2BPGi level is a risk factor for developing HCC [49].
Elevated AFP levels correlate with a high incidence of the development of HCC [68]. However, Yamasaki et al. [31] found that the M2BPGi assay is superior to other assays that assess AFP levels for predicting the development of HCC. Furthermore, the progression of liver fibrosis increases the risk of developing HCC [69]. Therefore, predicting the development of HCC using M2BPGi may reflect liver fibrosis. Yamasaki et al. [31] found that elevated M2BPGi levels are a significant risk factor, even after stratification of patients according to histologically confirmed liver fibrosis. Thus, in each fibrosis stage (F0/1, F2/3, and F4), elevated M2BPGi levels indicate a significant risk for developing HCC. Therefore, elevated M2BPGi levels may serve as a risk factor for developing HCC, independent of the stage of fibrosis.
M2BPGi as a prognostic factor after therapy for HCC
M2BPGi levels are a prognostic factor for patients with HCC (Table 1). For example, Fujiyoshi et al. [70] found that an elevated M2BPGi level is a significant risk factor for tumor recurrence and shorter overall survival in patients with HCC who undergo hepatectomy. Moreover, M2BPGi levels are not affected by tumor-related factors such as AFP, AFP L3, PIVKA II, tumor number, tumor size, lymph node metastasis, vascular invasion, and tumor differentiation. Toyoda et al. [71] found that an elevated M2BPGi level is a risk factor for tumor recurrence and shorter overall survival of patients with early-stage HCC who underwent curative resection. These investigators were unable to demonstrate a correlation between tumor-related factors and M2BPGi levels, and they suggested that M2BPGi represents the liver’s background degree of oncogenic potential.
M2BPGi in other diseases
M2BPGi levels are elevated in organ fibrosis, such as idiopathic pulmonary fibrosis [72] and chronic pancreatitis [73], and correlate with the severity of disease. Moreover, M2BPGi levels are increased in pancreatic ductal adenocarcinoma [74], and elevated M2BPGi levels are associated with metastatic lesions. Pancreatic ductal adenocarcinoma is a cancer typical of those with dense fibrosis, and activation of stellate cells plays an important role in its progression [75]. Therefore, elevated M2BPGi levels in pancreatic ductal adenocarcinoma may reflect activation of cancer-associated stellate cells.
In conclusion, M2BPGi is a new, reliable surrogate marker of liver fibrosis and liver function. M2BPGi predicts the development of HCC, the prognosis of patients with liver cirrhosis, and patient prognosis after curative treatment for HCC. Moreover, elevated M2BPGi levels may reflect the activation of HSCs. Further clinical studies of HSC activation will likely contribute to a better understanding of disease.
References
Mokdad AA, Lopez AD, Shahraz S, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med. 2014;12:145. https://doi.org/10.1186/s12916-014-0145-y (PMID 25242656).
Schuppan D, Afdahal NH. Liver cirrhosis. Lancet. 2008;371:838–51.
Perz JF, Armstrong GL, Farrington LA, et al. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2003;38(Suppl 1):S38–53.
Karanjia RN, Crossey MM, Cox IJ, et al. Hepatic steatosis and fibrosis: non-invasive assessment. World J Gastroenterol. 2016;22:9880–97.
Majumdar A, Kitson MT, Roberts SK. Treatment of hepatitis C in patients with cirrhosis: remaining challenges for direct-acting antiviral therapy. Drugs. 2015;75:823–34.
Cammà C, Di Bona D, Schepis F, et al. Effect of peginterferon alfa-2a on liver histology in chronic hepatitis C: a meta-analysis of individual patient data. Hepatology. 2004;39:333–42.
Rockey DC, Caldwell SH, Goodman ZD, et al. American Association for the study of liver diseases. Liver biopsy. Hepatology. 2009;49(3):1017–44.
Goodman ZD. Grading and staging systems for inflammation and fibrosis in chronic liver diseases. J Hepatol. 2007;47:598–607.
Cholongitas E, Senzolo M, Standish R, et al. A systematic review of the quality of liver biopsy specimens. Am J Clin Pathol. 2006;125:710–21.
Colloredo G, Guido M, Sonzogni A, et al. Impact of liver biopsy size on histological evaluation of chronic viral hepatitis: the smaller the sample, the milder the disease. J Hepatol. 2003;39(2):239–44.
Garcia-Tsao G, Friedman S, Iredale J. Now there are many (stages) where before there was one: in search of a pathophysiological classification of cirrhosis. Hepatology. 2010;51:1445–9.
Germani G, Hytiroglou P, Fotiadu A, et al. Assessment of fibrosis and cirrhosis in liver biopsies: an update. Semin Liver Dis. 2011;31(1):82–90.
Lurie Y, Webb M, Cytter-Kuint R, et al. Non-invasive diagnosis of liver fibrosis and cirrhosis. World J Gastroenterol. 2015;21:11567–83.
Toshima T, Shirabe K, Takeishi K, et al. New method for assessing liver fibrosis based on acoustic radiation force impulse: a special reference to the difference between right and left liver. J Gastroenterol. 2011;46:705–11.
Sandrin L, Fourquet B, Hasquenoph JM, et al. Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol. 2003;29(12):1705–13.
Cui J, Heba E, Hernandez C, et al. Magnetic resonance elastography is superior to acoustic radiation force impulse for the diagnosis of fibrosis in patients with biopsy-proven nonalcoholic fatty liver disease: a prospective study. Hepatology. 2016;63:453–61.
Şirli R, Sporea I, Popescu A, et al. Ultrasound-based elastography for the diagnosis of portal hypertension in cirrhotics. World J Gastroenterol. 2015;21(41):11542–51.
Tatsumi C, Kudo M, Ueshima K, et al. Noninvasive evaluation of hepatic fibrosis using serum fibrotic marker, transient elastography (FibroScan) and real-time tissue elastography. Intervirology. 2008;51(1):27–33.
Wai CT, Greenson JK, Fontana RJ, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38:518–26.
Vallet-Pichard A, Mallet V, Nalpas B, et al. FIB-4: an inexpensive and accurate marker of fibrosis in HCV infection. Comparison with liver biopsy and fibrotest. Hepatology. 2007;46:32–6.
Rosenberg I, Cherayil BJ, Isselbacher KJ, et al. Mac-2-binding glycoproteins. Putative ligands for a cytosolic β-galactoside lectin. J Biol Chem. 1991;266:18731–6.
Hellstern S, Sasaki T, Fauser C, et al. Functional studies on recombinant domains Mac-2-binding protein. J Biol Chem. 2002;277:15690–6.
Sasaki T, Brakebusch C, Engel J, et al. Mac-2 binging protein is a cell-adhesive protein of the extracellular matrix which self-assembles into ring-like structures and binds beta 1 integrins, collagens and fibronectin. EMBO J. 1998;17:1606–13.
Bekki Y, Yoshizumi T, Shimoda S, et al. Hepatic stellate cells secrete WFA+-M2BP. Its role in biological interactions with Kupffer cells. J Gastroenterol Hepatol. 2016. https://doi.org/10.1111/jgh.13706 (Epub ahead of print).
Kianoush A, Nematollahi M, Waterfield JD, et al. Regulation of RAW 264.7 macrophage polarization on smooth and rough surface topographies by galectin-3. J Biomed Mater Res A. 2017. https://doi.org/10.1002/jpm.a.36107 (epubahead of print).
Wang L, Guo XL. Molecular regulation of galectin 3 expression and therapeutic implication in cancer progression. Biomed Pharmacother. 2016;78:165–71.
Kuno A, Sato T, Shimazaki H, et al. Reconstruction of a robust glycodiagnostic agent supported by multiple lectin-assisted glycan profiling. Proteom Clin Appl. 2013;7:642–7.
Kuno A, Ikehara Y, Tanaka Y, et al. A serum “sweet-doughnut” protein facilitates fibrosis evaluation and therapy assessment in patients with viral hepatitis. Sci Rep. 2013;3:1065.
Narimatsu H. Development of M2BPGi: a novel fibrosis serum glyco-biomarker for chronic hepatitis/cirrhosis diagnostics. Expert Rev Proteom. 2015;12(6):683–93.
Toshima T, Shirabe K, Ikegami T, et al. A novel serum marker, glycosylated Wisteria floribunda agglutinin-positive Mac-2 binding protein (WFA(+)-M2BP), for assessing liver fibrosis. J Gastroenterol. 2015;50:76–84.
Yamasaki K, Tateyama M, Abiru S, et al. Elevated serum levels of Wisteria floribunda agglutinin-positive Mac-2 binding protein predict the development of hepatocellular carcinoma in hepatitis C patients. Hepatology. 2014;60:1563–70.
Xu H, Kong W, Liu L, et al. Accuracy of M2BPGi, compared with Fibro Scan®, in analysis of liver fibrosis in patients with hepatitis C. BMC Gastroenterol. 2017;17(1):62. https://doi.org/10.1186/s12876-017-0618-5.
Zou X, Zhu MY, Li W, et al. Serum WFA+-M2BP levels for evaluation of early stage of liver fibrosis in patients with chronic hepatitis B virus infection. Liver Int. 2017;37:35–44.
Nishikawa H, Hasegawa K, Ishii A, et al. A proposed predictive model for advanced fibrosis in patients with chronic hepatitis B and its validation. Medicine. 2016;95(35):e4679.
Ishii A, Nishikawa H, Enomoto H, et al. Clinical implication of serum Wisteria floribunda agglutinin positive Mac-2 binding protein in treatment-naïve chronic hepatitis B. Hepatol Res. 2017;47:204–15.
Nakamura M, Kanda T, Jiang X, et al. Serum microRNA-122 and Wisteria floribunda agglutinin positive Mac-2-binding protein are useful tools for liquid biopsy of the patients with hepatitis B virus and advanced liver fibrosis. PLoS One. 2017;12:e177302. https://doi.org/10.1371/journal.pone.0177302.
Wei B, Feng S, Chen E, Li D, et al. M2BPGi as a potential diagnostic tool of cirrhosis in Chinese patients with Hepatitis B virus infection. J Clin Lab Anal. 2017. https://doi.org/10.1002/jcla.22261 (Epub ahead of print).
Miyaki E, Imamura M, Hiraga N, et al. Daclatasvir and asunaprevir treatment improves liver function parameters and reduces liver fibrosis markers in chronic hepatitis C patients. Hepatol Res. 2016;46(8):758–64.
Suda T, Okawa O, Masaoka R, et al. Shear wave elastography in hepatitis C patients before and after antiviral therapy. World J Hepatol. 2017;9(1):64–8.
Umemura T, Joshita S, Sekiguchi T, et al. Serum Wisteria floribunda agglutinin positive Mac-2-binding protein level predicts liver fibrosis and prognosis in primary biliary cirrhosis. Am J Gastroenterol. 2015;110:857–64.
Nishikawa H, Enomoto H, Iwata Y, et al. Impact of serum Wisteria floribunda agglutinin positive Mac-2-binding protein and serum interferon-γ-inducible protein-10 in primary biliary cirrhosis. Hepatol Res. 2016;46:575–83.
Yamada N, Sanada Y, Tashiro M, et al. Serum Mac-2 binding protein glycosylation isomer predicts grade F4 liver fibrosis in patients with biliary atresia. J Gastroenterol. 2017;52:245–52.
Nishikawa H, Enomoto H, Iwata Y, et al. Clinical significance of serum Wisteria floribunda agglutinin positive Mac-2-binding protein level and high-sensitivity C-reactive protein concentration in autoimmune hepatitis. Hepatol Res. 2016;46:613–21.
Abe M, Miyake T, Kuno A, et al. Association between Wisteria floribunda agglutinin positive Mac-2-binding protein and the fibrosis stage of non-alcoholic fatty liver disease. J Gastroetenrol. 2015;50:776–84.
Mizuno M, Shima T, Oya H, et al. Classification of patients with non-alcoholic fatty liver disease using rapid immunoassay of serum type IV collagen compared with liver histology and other fibrosis markers. Hepatol Res. 2017;47:216–25.
Shigefuku R, Takahashi H, Nakano H, et al. Correlations of hepatic hemodynamics, liver function, and fibrosis markers in nonalcoholic fatty liver disease: comparison with chronic hepatitis related to hepatitis C virus. Int J Mol Sci. 2016;17:1545. https://doi.org/10.3390/jims17091545.
Nishikawa H, Enomoto H, Iwata Y, et al. Clinical significance of serum Wisteria floribunda agglutinin positive Mac-2-binding protein level in non-alcoholic steatohepatitis. Hepatol Res. 2016;46:1194–202.
Lai LL, Chan WK, Sthaneshwar P, et al. Serum Wisteria floribunda agglutinin positive Mac-2-binding protein in non-alcoholic fatty liver disease. PLoS One. 2017;12:e174982.
Ito K, Murotani K, Nakade Y, et al. Serum WFA+-M2BP levels predict liver fibrosis, development of hepatocellular carcinoma, and overall survival: A meta-analysis. J Gastroenterol Hepatol. 2017. https://doi.org/10.1111/jgh.13802 (Epub ahead of print).
Nishikawa H, Enomoto H, Iwata Y, et al. Serum Wisteria floribunda agglutinin positive Mac-2-binding protein for patients with chronic hepatitis B and C: a comparative study. J Viral Hepat. 2016;23:977–84.
Kleiner DF, Brunt EM, Natta MV, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Nagata H, Nakagawa M, Nishimura-Sakurai Y, et al. Serum measurement of Wisteria floribunda agglutinin positive Mac-2-binding protein is useful for predicting liver fibrosis and the development of hepatocellular carcinoma in chronic hepatitis C patients treated with IFN-based and IFN-free therapy. Hepatol Int. 2016;10:956–64.
Hanai T, Shiraki M, Ohnishi S, et al. Impact of serum glycosylated Wisteria floribunda agglutinin positive Mac-2 binding protein levels on liver functional reserves and mortality in patients with liver cirrhosis. Hepatol Res. 2015;45:1083–90.
Nishikawa H, Takata R, Enomoto H, et al. Proposal of a predictive model for advanced fibrosis containing Wisteria floribunda agglutinin-positive Mac-2 binding protein in chronic hepatitis C. Hepatol Res. 2017;47:E47–84.
Ura K, Furusho N, Ogawa E, et al. Serum WFA(+)-M2BP is a non-invasive liver fibrosis marker that can predict the efficacy of direct acting anti-viral-based triple therapy for chronic hepatitis C. Aliment Phamacol Ther. 2016;43:114–24.
Watanabe T, Tokumoto Y, Joko K, et al. Predictors of treatment efficacy and ALT non-normalization with sofosbuvir/ribavirin therapy for patients with hepatitis C virus genotype 2. J Med Virol. 2017. https://doi.org/10.1002/jmv.24776 (Epub ahead of print).
Nishikawa H, Enomoto H, Iwata Y, et al. Clinical implication of serum Wisteria floribunda agglutinin positive Mac-2-binding protein level on hepatitis B e-antigen loss or seroconversion in hepatitis B e-antigen positive patients. Hepatol Res. 2016;46:1065–73.
Hasegawa K, Takata R, Nishikawa H, et al. Impact of Wisteria floribunda agglutinin positive Mac-2-binding protein in patients with hepatitis C virus related compensated liver cirrhosis. Int J Mol Sci. 2016;17:1500. https://doi.org/10.3390/ijms17091500.
Okuda Y, Taura K, Yoshino K, et al. Usefulness of Mac-2 binding protein glycosylation isomer for prediction of posthepatectomy liver failure in patients with hepatocellular carcinoma. Ann Surg. 2017;265:1201–8.
Morio K, Imamura M, Daijo K, et al. Wisteria floribunda agglutinin positive Mac-2-binding protein level increases in patients with acute liver injury. J Gastroenterol. 2017. https://doi.org/10.1007/s00535-017-1345-y.
Tamaki N, Kurosaki M, Kuno A, et al. Wisteria floribunda agglutinin positive Mac-2-binding protein as a predictor of hepatocellular carcinoma development in chronic hepatitis C patients. Hepatol Res. 2015;45:E82–8.
Sato S, Genda T, Ichida T, et al. Prediction of hepatocellular carcinoma development after hepatitis C virus eradication using serum Wisteria floribunda agglutinin positive Mac-2-binding protein. Int J Mol Sci. 2016;17:2143. https://doi.org/10.3390/ijms17122143.
Sasaki R, Yamasaki K, Abiru S, et al. Serum Wisteria floribunda agglutinin positive Mac-2-binding protein values predict the development of hepatocellular carcinoma among patients with chronic hepatitis C after sustained virological response. PLoS One. 2015;50:1134–44.
Heo JY, Kim SU, Kim BK, et al. Use of Wisteria floribunda agglutinin positive Mac-2-binding protein in assessing risk of hepatocellular carcinoma due to hepatitis B. Medicine. 2016;95:e3328.
Kim SU, Heo JY, Kim BK, et al. Wisteria floribunda agglutinin positive Mac-2-binding protein predicts the risk of HBV-related liver cancer development. Liver Int. 2016. https://doi.org/10.1111/liv.13341 (Epub ahead of print).
Ichikawa Y, Joshita S, Umemura T, et al. Serum Wisteria floribunda agglutinin positive Mac-2-binding protein may predict liver fibrosis and progression to hepatocellular carcinoma in patients with chronic hepatitis B virus infection. Hepatol Res. 2017;47:226–33.
Cheung KS, Seto WK, Wong DK, et al. Wisteria floribunda agglutinin-positive human Mac-2 binding protein predicts liver cancer development in chronic hepatitis B patients under antiviral treatment. Oncotarget. 2017. https://doi.org/10.18632/oncotarget.17670 (Epub ahead of print).
Tateyama M, Yatsuhashi H, Taura N, et al. Alpha-fetoprotein above normal levels as a risk factor for the development of hepatocellular carcinoma in patients infected with hepatitis C virus. J Gastroenterol. 2011;46:92–100.
Westbrook RH, Dusheiko G. Natural history of hepatitis C. J Hepatol. 2014;61:S58–68.
Fujiyoshi M, Kuno A, Gotoh M, et al. Clinicopathological characteristics and diagnostic performance of Wisteria floribunda agglutinin positive Mac-2-binding protein as a preoperative serum marker of liver fibrosis in hepatocellular carcinoma. J Gastroenterol. 2015;50:1134–44.
Toyoda H, Kumada T, Tada T, et al. Serum WFA+-M2BP levels as a prognostic factor in patients with early hepatocellular carcinoma undergoing curative resection. Liver Int. 2016;36:293–301.
Kono M, Nakamura Y, Oyama Y, et al. Increased levels of serum Wisteria floribunda agglutinin positive Mac-2-binding protein in idiopathic pulmonary fibrosis. Respir Med. 2016;115:46–52.
Fujiyama T, Ito T, Ueda K, et al. Srume levels of Wisteria floribunda agglutinin positive Mac-2-binding protein reflect the severity of chronic pancreatitis. J Dig Dis. 2017. https://doi.org/10.1111/1751-2980.12475 (Epub ahead of print).
Waragai Y, Suzuki R, Takagi T, et al. Clinical significance of serum Wisteria floribunda agglutinin positive Mac-2-binding protein in pancreatic ductal adenocarcinoma. Pancreatology. 2016;16:1044–50.
Apte MV, Wilson JS, Lugaea A, et al. A starring role for stellate cells in the pancreatic cancer microenvironment. Gastroenterology. 2013;144:1210–9.
Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. The METAIR Cooperative Study Group. Hepatology. 1996;24:289–93.
Acknowledgements
This work was supported by JSPS KAKENHI Grants JP1504932 and 16K15606.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shirabe, K., Bekki, Y., Gantumur, D. et al. Mac-2 binding protein glycan isomer (M2BPGi) is a new serum biomarker for assessing liver fibrosis: more than a biomarker of liver fibrosis. J Gastroenterol 53, 819–826 (2018). https://doi.org/10.1007/s00535-017-1425-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-017-1425-z