Abstract
Background
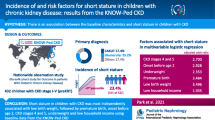
Children with chronic kidney disease (CKD) have delays in normal growth and pubertal development. We describe factors associated with delayed menarche and the association of delayed menarche with short stature in girls with CKD.
Methods
Two hundred eighty-seven girls with CKD onset prior to menarche within the Chronic Kidney Disease in Children (CKiD) cohort were studied. Delayed menarche was defined as menarche at age 15 years or older; short stature was defined as last available height 2 standard deviations below projected adult height. Kaplan-Meier cumulative incidence function was used to estimate median age at menarche. Chi-squared and Wilcoxon rank-sum tests were used to assess factors associated with delayed menarche. Chi-squared test was used to evaluate the association between delayed menarche and short stature.
Results
Among 287 girls, 68 enrolled with prevalent menarche, 131 were observed to have incident menarche, and 88 were pre-menarchal at their last study visit. Median age at menarche was 12 years. Ten percent had delayed menarche. African American race, lower estimated glomerular filtration rate, ever corticosteroid use, and longer CKD duration were associated with delayed menarche (p < 0.05). Girls with delayed menarche had lower height and weight percentiles at the time of menarche (p < 0.05). Sixty-one percent of girls with delayed menarche had short stature compared with only 35% of girls without delayed menarche (p = 0.03).
Conclusion
Median age at menarche is similar among girls with CKD and healthy girls. Ten percent of girls with CKD had delayed menarche and may be at risk for short stature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children with chronic kidney disease (CKD) have delays in normal growth and pubertal development [1,2,3]. Puberty is considered a high-risk period for decline in kidney function among children with CKD. Studies have shown accelerated decline in kidney function after the onset of the pubertal growth spurt [4]. Pubertal delay has also been associated with a range of complications including neurocognitive impairment, increased fracture risk, and cardiovascular disease in the general population [4,5,6,7].
Pubertal onset can be defined based on hormonal levels (e.g., concentration of luteinizing hormone) and clinical markers (e.g., Tanner stage, growth spurt). However, hormonal levels are not typically assessed clinically without indication, and clinical makers of puberty onset such as transition from Tanner stage 1 to stage 2 (i.e., thelarche) can be difficult to reliably assess [8]. In contrast, for girls, age at menarche is a reliable and well-defined indicator of pubertal development based on patient report and requires no physical exam.
Puberty usually begins between age 8 and 13 years among girls in the general population, although there is variability by race and ethnicity. [9] The median age at menarche in the general population is 12.4 years, with earlier menarche among non-Hispanic blacks (12.1 years) versus non-Hispanic white girls (12.6 years). [10] Data from the National Health and Nutrition Examination Survey (NHANES) has shown a trend toward earlier menarche with younger generations. [11] Delayed puberty is defined as lack of signs of pubertal development at an age 2 to 2.5 standard deviations above the mean for children of the same sex. For girls, lack of pubertal development by age 13 is considered delayed puberty [8]. Delayed menarche is defined as the absence of menses by age 15 [8].
Prior studies of pubertal development in children with CKD have shown that children on renal replacement therapy (RRT) have delayed pubertal onset by 2–2.5 years, and menarche occurred at the upper limit of normal (around 15 years of age) in about half of girls on RRT [2, 3]. However, to our knowledge, there are no large studies evaluating age at menarche among girls with CKD prior to RRT. We aimed to describe the age at menarche among a large cohort of girls with CKD and identify factors associated with delayed menarche. In addition, we aimed to evaluate the association between delayed menarche and short stature as a marker of physical development among girls with CKD.
Methods
Study design
This analysis utilized data from the Chronic Kidney Disease in Children (CKiD) prospective cohort study. Initial CKiD study design and methods have been published previously [12]. Inclusion criteria included age 1–16 years and estimated glomerular filtration rate (eGFR) of 30–90 ml/min per 1.73 m2, calculated using the bedside CKiD equation [13, 14]. The cohort was further restricted to female subjects who reported onset of menarche after CKD diagnosis.
Variables
Baseline clinical and demographic data were obtained at study entry including race, glomerular versus non-glomerular diagnosis, age of onset of CKD, birth history (including prematurity, small for gestational age, or low birth weight), and mid-parental height. Menarchal status (self-reported), Tanner stage, height, weight, medications (self-reported), and eGFR were collected at annual study visits [15].
Delayed menarche was defined as menarche at age 15 years or older or pre-menarche at age 15 years or older at last study follow-up. Projected adult height for girls was calculated as: (father’s height + mother’s height − 13 cm)/2, where height was measured in centimeters [16]. Short stature was defined as a last observed height less than 2 standard deviations below projected mid-parental height [16].
Statistical methods
The cumulative incidence of age at menarche was estimated using the Kaplan-Meier method. This allowed a comparison of ages at menarche among girls with CKD to healthy girls based on previously published data from NHANES [11]. This method appropriately accounted for girls who had not yet reached menarche as being “at-risk,” but menarche-free. Time origin was set at age 5 years, with a time metric of age in years, and outcome of menarche. Chi-squared and Wilcoxon rank-sum tests were used to assess factors associated with delayed menarche including race, abnormal birth history, need for food assistance, age of CKD onset, duration of CKD, glomerular versus non-glomerular diagnosis, eGFR, ever growth hormone use, ever corticosteroid use, BMI, weight percentile, and height percentile. A Chi-squared test was also used to evaluate the association between delayed menarche and short stature. Analyses were conducted using Stata, version 15.1 [17]. A p value of less than 0.05 was the threshold for statistical significance.
Results
The cohort included 287 girls. Forty eight girls with menarche prior to CKD onset were excluded. Of the 287 girls included, 68 had prevalent menarche, 131 had incident menarche, and 88 were pre-menarchal at last study follow-up. All girls with prevalent menarche reported menarche prior to age 15. Of the 131 girls with incident menarche, 124 had menarche prior to age 15 and 7 had delayed menarche. Of the 88 girls who were pre-menarchal at last study follow-up, 14 demonstrated delayed menarche as they were pre-menarchal at age 15 or older. The estimated median age of menarche was 12.0 years (interquartile range (IQR), 12.0–14.0 years) (Fig. 1). The observed median age of menarche among girls with prevalent and incident menarche was 14.0 (IQR, 12.9–15.1 years). The majority of girls in the CKiD study population had menarche at similar age to girls in the NHANES population. However, 10% of girls in CKiD had delayed menarche as opposed to less than 5% of girls in NHANES (Fig. 1).
Table 1 shows demographic and clinical characteristics of 124 girls without delayed menarche compared with 21 girls with delayed menarche. This table excludes girls with prevalent menarche, as we were unable to assess time-varying clinical variables at the time of menarche. The median age at menarche for those without delayed menarche was 12.0 (IQR, 12.0–13.0 years). The median age at menarche for post-menarchal girls with delayed menarche was 15.0 years (IQR, 15.0–16.0 years). The median age for pre-menarchal girls who were defined as having delayed menarche due to pre-menarchal status at age 15 or older was 16.1 years (IQR, 15.2–17.9 years). Girls with delayed menarche were more likely to be of African American race, have been prescribed corticosteroids, have longer duration of kidney disease, and have lower eGFR at the time of menarche compared with girls with normal onset of menarche (p < 0.05). There was no significant difference by menarche status for abnormal birth history (premature, small for gestational age, or low birth weight), BMI, need for food assistance, age at CKD diagnosis, underlying cause of CKD, or ever growth hormone use. Height and weight percentiles at the time of menarche were lower for girls with delayed menarche compared with those with normal menarche (p < 0.05). Thirty-eight percent of post-menarchal girls were defined as having short stature based on last height during study follow-up. Sixty-one percent of girls with delayed menarche had short stature compared with only 35% of girls without delayed menarche (p = 0.03), with median age at last height available of 17.4 years (IQR, 15.3–19.2 years).
Discussion
In this cohort of girls with CKD in which onset of menarche was reported, we found that the median age of menarche was similar to that reported in healthy girls. However, 10% of girls in this cohort had delayed menarche. Factors associated with delayed menarche included African American race, corticosteroid use, lower eGFR at the time of menarche, and longer duration of CKD. Girls with delayed menarche also had lower height and weight percentiles at the time of menarche and were more likely to have short stature. This study highlights the prevalence of delayed menarche in girls with CKD and the potential impact on final adult height.
Pubertal delay has been described among children with CKD. A study of girls with end-stage kidney disease (ESKD) requiring RRT showed that about half of girls had menarche at the upper age limit of normal [3]. Our study is unique in that we evaluated pubertal development in girls with earlier stages of CKD. Although we found that the majority of girls with CKD had menarche at a similar age as healthy girls, 10% had delayed menarche. Given the potential impact of pubertal delay on growth, neurocognitive function, cardiovascular disease risk, and fracture risk, it is important for clinicians to be aware of the risk of pubertal delay in girls with CKD [5,6,7,8]. The mechanism of pubertal delay among children with CKD is not fully understood. Changes in normal pubertal hormones may play a part. Prior studies have shown that children on dialysis have elevated LH levels compared with the general population, but there are no studies on estrogen and testosterone levels on children in CKD [18, 19]. In addition, delayed puberty has also been reported in other chronic diseases such as cystic fibrosis and inflammatory bowel disease as a result of secondary hypogonadism [8]. Therefore, delayed puberty in CKD may be a result of chronic illness.
We found that African American race was associated with delayed menarche among girls with CKD. This is in contrast to trends in the general population in which African American race is associated with earlier puberty in girls [20]. It is possible that the association between African American race and delayed menarche in girls with CKD is a result of confounding by underlying CKD diagnosis or severity, as African Americans have a higher prevalence of glomerular disease as well as faster progression of CKD [21, 22].
We also found that girls with delayed menarche were more likely to have corticosteroid exposure. There may be a relationship between glomerular disease diagnosis, corticosteroid exposure, and African American race. The mechanism by which corticosteroids affect puberty is unclear. It has been postulated that glucocorticoids impair pubertal onset through inhibition at the level of the hypothalamus and pituitary, reduced secretion of sex steroids from the gonads, or impaired end-organ sensitivity to sex steroids. LH has been showed to be suppressed in women with rheumatic diseases as well as in children with steroid-sensitive nephrotic syndrome on glucocorticoids [23].
Another important finding from this analysis was that delayed menarche in girls with CKD was associated with short stature. The association between pubertal delay and growth is variable based on the underlying cause for pubertal delay. For example, children with constitutional delay of puberty are expected to reach full growth potential despite delay in onset of puberty [8]. Children with isolated primary hypogonadism from hypogonadotropic hypogonadism typically have a modest increase in final adult height, likely as a result of delayed epiphyseal closure due to hypogonadism [24]. However, children with delayed puberty secondary to chronic illnesses have been reported to have stunted growth and reduced final height with variable catch-up growth depending on length and type of illness [8]. Our findings suggest that similar to delayed puberty secondary to other chronic illnesses like cystic fibrosis, inflammatory bowel disease, and eating disorders, delayed puberty among girls with CKD is associated with stunted growth and short stature [8]. Of note, corticosteroids are also associated with decreased bone strength and growth via apoptosis of osteocytes, decreased maturation of cells into osteoblasts, and a negative calcium balance via decreased intestinal calcium absorption [23]. As girls with delayed menarche were more likely to be prescribed corticosteroids, this may be another risk factor for short stature. Clinicians may falsely believe that a delay in puberty confers time for additional catch-up growth, as seen among children with isolated primary hypogonadism. Our data suggest that pubertal delay among girls with CKD is actually associated with short stature at the time of menarche.
This study has several limitations. First, there was relatively short follow-up time. The age at menarche was collected as an integer at yearly follow-up visits, limiting the ability to more granularly define age at menarche. The average age at last available height was at 17.4 years, so it is possible that participants continued to grow after the last study visit. In the healthy population, about 7 cm of growth is expected on average after menarche [25]. However, to the authors’ knowledge, there are no estimates of expected growth post-menarche in the CKD population. In addition, we were only able to assess factors associated with pubertal delay among girls with incident menarche, as variables such as eGFR were not available at the time of menarche among girls with prevalent menarche before study entry. Finally, we used self-reported menarche as the marker of pubertal delay in this study. This limited the cohort to only girls, and these results are not applicable to boys with CKD. Furthermore, the age range in the original CKiD study was 1.1–21.8 years, whereas the NHANES population included a birth cohort from the 1920s for whom self-reported age at menarche may have more recall bias than for those within the younger CKiD population. Other variables such as hormonal markers may be a more sensitive marker of pubertal delay.
Conclusion
Median age at menarche was similar among girls with CKD compared with healthy girls. However, there was a proportion of girls with CKD with delayed menarche, and this may be a risk factor for short stature. Further research is needed to assess whether delayed menarche is also associated with other long-term CKD complications such as cardiovascular disease and neurocognitive function. Clinicians should be aware of the risk of pubertal delay and short stature among girls with CKD.
References
Rodig NM et al (2014) Growth in children with chronic kidney disease: a report from the Chronic Kidney Disease in Children Study. Pediatr Nephrol 29(10):1987–1995
Schaefer F et al (1990) Pubertal growth in chronic renal failure. Pediatr Res 28(1):5–10
Haffner D, Zivicnjak M (2017) Pubertal development in children with chronic kidney disease. Pediatr Nephrol 32(6):949–964
Ardissino G et al (2012) Puberty is associated with increased deterioration of renal function in patients with CKD: data from the ItalKid Project. Arch Dis Child 97(10):885–888
Blakemore SJ, Burnett S, Dahl RE (2010) The role of puberty in the developing adolescent brain. Hum Brain Mapp 31(6):926–933
Bonjour JP, Chevalley T (2014) Pubertal timing, bone acquisition, and risk of fracture throughout life. Endocr Rev 35(5):820–847
Canoy D et al (2015) Age at menarche and risks of coronary heart and other vascular diseases in a large UK cohort. Circulation 131(3):237–244
Wolf RM, Long D (2016) Pubertal development. Pediatr Rev 37(7):292–300
Bordini B, Rosenfield RL (2011) Normal pubertal development: part II: clinical aspects of puberty. Pediatr Rev 32(7):281–292
Chumlea WC et al (2003) Age at menarche and racial comparisons in US girls. Pediatrics 111(1):110–113
McDowell MA, Brody DJ, Hughes JP (2007) Has age at menarche changed? Results from the National Health and Nutrition Examination Survey (NHANES) 1999-2004. J Adolesc Health 40(3):227–231
Furth SL et al (2006) Design and methods of the Chronic Kidney Disease in Children (CKiD) prospective cohort study. Clin J Am Soc Nephrol 1(5):1006–1015
Schwartz GJ et al (2009) New equations to estimate GFR in children with CKD. Journal of the American Society of Nephrology, 20(3), 629-637
Schwartz GJ et al (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58(2):259–263
Schwartz GJ et al (2012) Improved equations estimating GFR in children with chronic kidney disease using an immunonephelometric determination of cystatin C. Kidney Int 82(4):445–453
Rose SR, Vogiatzi MG, Copeland KC (2005) A general pediatric approach to evaluating a short child. Pediatr Rev 26(11):410–420
StataCorp (2017) Stata Statistical Software: Release 15. StataCorp LLC: College Station
Distiller LA et al (1975) Pituitary-gonadal function in chronic renal failure: the effect of luteinizing hormone--releasing hormone and the influence of dialysis. Metabolism 24(6):711–720
Rathi M, Ramachandran R (2012) Sexual and gonadal dysfunction in chronic kidney disease: pathophysiology. Indian journal of endocrinology and metabolism, 16(2), 214.
Kaplowitz PB et al (2001) Earlier onset of puberty in girls: relation to increased body mass index and race. Pediatrics 108(2):347–353
Minnick ML et al (2010) Sex, race, and socioeconomic disparities in kidney disease in children. Semin Nephrol 30(1):26–32
Moxey-Mims M (2018) Kidney disease in African American children: biological and nonbiological disparities. Am J Kidney Dis 72(5s1):S17–s21
Kao KT et al (2019) Pubertal abnormalities in adolescents with chronic disease. Best Pract Res Clin Endocrinol Metab 33(3):101275
Uriarte MM et al (1992) The effect of pubertal delay on adult height in men with isolated hypogonadotropic hypogonadism. J Clin Endocrinol Metab 74(2):436–440
Nakamoto JM (2000) Topics in Review: Myths and variations in normal pubertal development. Western Journal of Medicine, 172(3), 182
Funding
This work was supported by T32DK007732.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, H.S., Ng, D.K., Matheson, M.B. et al. Delayed menarche in girls with chronic kidney disease and the association with short stature. Pediatr Nephrol 35, 1471–1475 (2020). https://doi.org/10.1007/s00467-020-04559-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04559-7