Abstract
Background
Preserving optimal growth has long been a significant concern for children with chronic kidney disease (CKD). We aimed to examine the incidence of and risk factors for short stature in Asian pediatric patients with CKD.
Methods
We analyzed growth status by height, weight, and body mass index (BMI) standard deviation scores (SDSs) for 432 participants in the KoreaN cohort study for Outcome in patients With Pediatric Chronic Kidney Disease.
Results
The median height, weight, and BMI SDSs were − 0.94 (interquartile range (IQR) − 1.95 to 0.05), − 0.58 (IQR − 1.46 to 0.48), and − 0.26 (IQR − 1.13 to 0.61), respectively. A high prevalence of short stature (101 of 432 patients, 23.4%) and underweight (61 of 432 patients, 14.1%) was observed. In multivariable logistic regression analysis, CKD stages 4 and 5 (adjusted odds ratio (aOR) 2.700, p = 0.001), onset before age 2 (aOR 2.928, p < 0.0001), underweight (aOR 2.353, p = 0.013), premature birth (aOR 3.484, p < 0.0001), LBW (aOR 3.496, p = 0.001), and low household income (aOR 1.935, p = 0.030) were independent risk factors associated with short stature in children with CKD.
Conclusions
Children with CKD in Korea were shorter and had lower body weight and BMI than the general population. Short stature in children with CKD was most independently associated with low birth weight, followed by premature birth, onset before age 2, CKD stages 4 and 5, underweight, and low household income. Among these, underweight is the only modifiable factor. Therefore, we suggest children with CKD should be carefully monitored for weight, nutritional status, and body composition to achieve optimal growth.
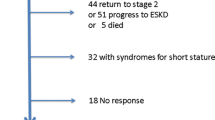
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maintaining optimal growth is a primary concern in children with chronic kidney disease (CKD). Previous studies have shown that factors affecting the growth of children with CKD include genetic factors, hormonal factors, nutritional disorders, metabolic derangements, and inflammatory disorders [1,2,3]. Although the clinical management of CKD has improved over the years, growth restriction remains a prevalent complication in children with CKD [4,5,6].
There is a significant link between the height of children with CKD and their quality of life and psychosocial health. In a previous study, the KoreaN cohort study for Outcome in patients With Pediatric Chronic Kidney Disease (KNOW-Ped CKD), short stature showed an inverse association with quality of life scores and a negative correlation with mental health and psychosocial adjustment problems [7, 8]. Height impairment is also an excellent clinical indicator that reflects the overall quality of care in children with CKD. Previous studies have also shown that pediatric CKD patients with short stature have higher morbidity and mortality [9, 10].
Most studies on the growth of children with CKD target patients on dialysis or those who have undergone transplantation, and very limited epidemiological data exist for Asian children [11,12,13]. We therefore aimed to examine the incidence of and risk factors for short stature in children with CKD in an Asian population using the baseline data from the KNOW-Ped CKD.
Methods
Study design and definitions
The nationwide observational study, the KNOW-Ped CKD, is a 10-year prospective cohort study launched in 2011 and funded by the Korea Centers for Disease Control and Prevention [14]. We enrolled 432 CKD children who had not received kidney replacement therapy and were younger than 18 years from seven major pediatric nephrology centers in Korea from April 2011 to February 2016.
We calculated the estimated glomerular filtration rate (eGFR) using the creatinine-cystatin C–based CKiD equation derived from the Chronic Kidney Disease in Children (CKiD) study [15]. CKD was defined and staged according to the Kidney Disease Improving Global Outcomes criteria [16]. Standard deviation scores (SDSs) of age-sex-specific height, age-sex-specific weight, and BMI expressed relative to height-age were calculated using the 2017 Korean National Pediatric and Adolescent Standard Growth Chart (KNGC2017) and WHO Child Growth Standards [17, 18]. Body mass index (BMI) SDS was calculated relative to height-age, at which a child would be of average height (50th percentile) for age [19]. Growth abnormalities were defined according to the screening criteria in the KNGC2017 as follows: short stature, height SDS < − 1.88 (3rd percentile); underweight, BMI SDS < − 1.65 (5th percentile); overweight, 1.04 (85th percentile) ≤ BMI SDS < 1.65 (95th percentile); obesity, BMI SDS ≥ 1.65 (95th percentile) [18]. Puberty onset was defined as the volume of the testes at Tanner stage 2 in boys and breast development at Tanner stage 2 in girls. The duration of CKD refers to the time from when the patient was diagnosed with CKD to the time of the baseline visit. Data including primary diseases leading to CKD, medication, parental heights, Tanner stage, birth history, and household income status (high, $4500 per month or more; middle, between $1500 and $4500 per month; and low, $1500 per month or less) were collected. Premature birth was defined as birth before the gestational age of 37 weeks, while low birth weight (LBW) was defined as birth weight < 2500 g. Finally, small for gestational age (SGA) was defined as the 10th percentile of birth weight according to gestational age using Korean references [20, 21].
Statistical analyses
We used the median and interquartile range (IQR) to summarize continuous variables and percentages to summarize categorical variables. The Mann-Whitney test was used to evaluate differences in continuous variables between groups and an independent t test was used to evaluate the overall association between categorical variables. Logistic regression analysis was performed to identify the factors associated with short stature to generate odds ratios (ORs) and 95% confidence intervals (CIs). Based on a literature review of previous reports, we examined the following variables as potential risk factors for short stature in children with CKD: CKD stages 4 and 5, onset before age 2, underweight, CKD due to congenital anomalies of the kidney and urinary tract (CAKUT), premature birth, LBW, SGA, low household income, duration of CKD, and steroid therapy [1,2,3,4,5,6]. In the multivariable logistic regression analysis, each variable was adjusted for mid-parental height, and potential confounders were selected a priori using directed acyclic graphs (Supplementary Figures S1–6) [22]. For the association between CKD stages 4 and 5 and short stature, age, sex, CKD due to CAKUT, onset before age 2, low household income, duration of CKD, and premature birth were adjusted for. CKD due to CAKUT was adjusted for the association between onset before age 2 and short stature. For the association between underweight and short stature, CKD stages 4 and 5, low birth weight, and low household income were adjusted for. CKD due to CAKUT was adjusted for the association between premature birth and short stature. For the association between low birth weight and short stature, premature birth was adjusted for. We used SPSS software version 26.0 for Windows (SPSS, Chicago, IL, USA) for all analyses. A p value < 0.05 was considered significant.
Results
Baseline characteristics of the cohort
Table 1 presents the demographic and clinical characteristics of the 432 children. Our cohort had a median age of 10.9 years (IQR, 5.2 to 14.6) and 68.1% were boys. The median baseline eGFR was 53.9 mL/min/1.73 m2 (IQR 32.16 to 80.87), CKD was due to CAKUT in 248 (57.4%) children, and CKD was due to glomerular problems in 109 (25.2%) children. CKD stages 1 and 2 were present in 45.6% of patients (197 of 432), 33.1% (143 of 432) of children were in CKD stage 3, and 21.3% (92 of 432) of children were in CKD stages 4 and 5. Compared with normative data from Korean children, participants in the KNOW-Ped CKD were shorter (median height SDS − 0.94; IQR − 1.95 to 0.05), had lower body weight (median weight SDS − 0.58; IQR − 1.46 to 0.48), and had lower BMI (median BMI SDS − 0.26; IQR − 1.21 to 0.62). Short stature was observed in 101 children (23.4%), and 61 children (14.1%) were underweight. On the other hand, 28 children (6.5%) were overweight, and 38 children (8.8%) were obese. A total of 83 children (48.2%) reached puberty. Premature birth, LBW, and SGA were observed in 83 children (19.5%), 74 children (17.5%), and 113 children (26.7%), respectively. Of the cohorts, 33 children (7.6%) were treated with recombinant human growth hormone (rhGH) and 31 children (7.2%) were treated with steroids.
Baseline characteristics of children with short stature
The median height, weight, and BMI SDS of children with short stature were − 2.80 (IQR − 4.11 to − 2.39), − 1.44 (IQR − 2.61 to − 0.08), and − 0.74 (IQR − 1.73 to 0.32), respectively. Children with short stature had a higher proportion of patients with onset before age 2, underweight, CKD stages 4 and 5, premature birth, and LBW than children without short stature (p < 0.0001). The proportion of patients with low household income, CKD due to CAKUT, prepuberty, SGA, and rhGH therapy were also higher in children with short stature than in children without short stature (Table 1). In addition, children with short stature had higher blood urea nitrogen (BUN) and cystatin C levels (p < 0.0001), lower hemoglobin levels (p = 0.018), lower carbon dioxide levels (p = 0.003), higher parathyroid hormone levels (p = 0.014), and higher urinary protein-creatinine ratios than children without short stature (p = 0.003) (Fig. 1).
Baseline laboratory findings of 432 study participants from the KNOW-Ped CKD stratified by height status. a BUN level. b Cystatin C level. c Hemoglobin level. d Calcium level. e Parathyroid hormone level. f 25-Hydroxyvitamin D level. g Carbon dioxide level. h Urinary protein-creatinine ratio. BUN, blood urea nitrogen; Hb, hemoglobin; Ca, calcium; PTH, parathyroid hormone; VitD, 25-hydroxy vitamin D; TCO2, carbon dioxide; PCR, urinary protein-creatinine ratio
Factors associated with short stature in children with CKD
Table 2 demonstrates the univariable and multivariable logistic regression analyses performed to examine the factors associated with short stature in children with CKD. Short stature was strongly associated with CKD stages 4 and 5 (OR 2.549, p < 0.0001), onset before age 2 (OR 2.502, p < 0.0001), underweight (OR 3.187, p < 0.0001), premature birth (OR 3.494, p < 0.0001), LBW (OR 4.453, p < 0.0001), and low household income (OR 1.883, p = 0.025) in a univariable analysis. The variables that were statistically significant by univariable analysis were included in a multivariable analysis. In a multivariable logistic regression analysis, CKD stages 4 and 5 (adjusted odds ratio (aOR) 2.700, p = 0.001), onset before age 2 (aOR 2.928, p < 0.0001), underweight (aOR 2.353, p = 0.013), premature birth (aOR 3.484, p < 0.0001), LBW (aOR 3.496, p = 0.001), and low household income (aOR 1.935, p = 0.030) were independent risk factors associated with short stature in children with CKD after adjustments for mid-parental height and potential confounders (Supplementary Figures S1–6). Among the potential risk factors, CKD due to CAKUT, SGA, duration of CKD, and steroid therapy were not shown in the table because they had no statistically significant association with short stature in the analysis.
Discussion
In this cross-sectional study using the baseline data from the KNOW-Ped CKD, we demonstrate that underweight is significantly associated with short stature in children with CKD, independent of other known risk factors for short stature. Underweight is a well-known risk factor for short stature in the general population, and this study confirmed that underweight also acts as a significant independent risk factor for short stature in children with CKD [23, 24]. Currently, data on the prevalence of underweight and the effect of underweight on the height of children with CKD are limited. This is the first large-scale study that comprehensively confirms underweight as a significant independent risk factor for short stature in a pediatric CKD cohort.
In our study, children with CKD were shorter and had a higher prevalence of short stature than the general population, as previously reported in Western studies [3, 6, 11, 12]. However, our cohort had a difference in the proportion of underweight, overweight, and obese children compared to other reports [11, 25]. A CKiD study reported that the median BMI SDS for the cohort was 0.44 (IQR − 0.33 to 1.23), with 13% being overweight and 16% being obese, but the study did not comment on underweight. According to a European study of the Cardiovascular Comorbidity in Children with Chronic Kidney Disease (4C study) cohort, the mean BMI SDS for the cohort was 0.08 ± 1.32, the proportion of underweight individuals in the cohort was 8.7%, and the combined proportion of overweight and obese individuals was 22.0%. On the other hand, our cohort had a median BMI SDS of − 0.26 (IQR − 1.21 to 0.62), with 14.1%, 6.5%, and 8.8% being underweight, overweight, and obese, respectively. Because of the difference in the proportion of underweight, overweight, and obesity among cohorts, being underweight may be a significant contributing factor to the short stature in our cohort. We cannot clearly explain the differences in these proportions; however, the cohort’s baseline characteristics, including region, ethnicity, and CKD severity, may have played a role [11, 26].
Underweight and low weight for height are the recommended indicators of malnutrition in both the general population and children with illness [24, 27], and there is a body of evidence showing an association between height impairment and underweight [28]. In children with CKD, not only is the proper intake and absorption of nutrients reduced, but protein-energy wasting (PEW) may also occur, leading to underweight, which can worsen linear growth in these populations [29]. The International Society of Renal Nutrition and Metabolism has defined PEW as the loss of body protein mass and fuel reserves [30]. In children with CKD, metabolic acidosis, chronic inflammation, and endocrine perturbation are considered the leading causes of PEW [29, 31]. A recent study of CKiD confirmed this trend. Children with advanced CKD stages had lower protein intake and reduced muscle mass; thus, they had a below-average BMI at the baseline visit [32]. While protein intake and muscle mass were not evaluated in our study, we assume that the high incidence of being underweight (14.1%) in our cohort seems to be related to CKD because the incidence of underweight in the Korean general population is only 2.2% before 2 years of age and 2.8% between 2 and 18 years of age [17]. Underweight is of great importance for clinical practice compared to other factors contributing to short stature found in previous cohort studies in that there is room for improvement through early and intensive dietary intervention and nutritional support [19]. Otherwise, rhGH is the only proven effective treatment for growth failure in children with CKD [33, 34].
Our findings confirmed that advanced CKD stages are a significant independent risk factor related to height deficits in children with CKD. This result is generally consistent with prior reports from Western and Asian countries [3, 13, 35], revealing that advanced CKD stages are risk factors for short stature. Although it is not clear how linear growth is affected as CKD progresses, decreased eGFR acts on a variety of growth-related factors, ultimately disrupting the normal physiology of long bones at the epiphyseal growth plate [1]. We also confirmed that abnormal birth histories, LBW, and premature birth were significant independent risk factors for short stature in children with CKD. In the general population, premature birth is well known to disrupt endocrine regulation, which affects linear growth and adiposity. Previous reports of pediatric CKD cohorts have also reported an association between LBW and short stature in children with CKD [36,37,38,39]. There are few studies on the link between linear growth and onset age and income level in children with CKD. Rees et al. reported impaired growth and final height in infants with severe CKD who received a kidney diagnosis within the first 6 months of life [40]. In a report from the CKiD cohort, children with low household income (under $30,000 per year) were unable to overcome height deficits over time and had a higher risk of growth impairment [41]. This is in line with our results showing that low household income was associated with a higher risk of short stature in children with CKD. However, further analysis of longitudinal data is required to confirm these results in our cohort.
Among potentially modifiable factors associated with growth, such as rhGH and steroid therapy, steroid therapy was not found to be significantly associated with short stature in this study, probably because of the small number of cases (Table 1). The administration of rhGH in patients with CKD is known to accelerate growth and improve final adult height [33]. In our study, rhGH therapy was administered in only 14.3% of children with short stature and 7.6% of the entire cohort. Considering the effect of rhGH therapy, physicians should pay more attention to the growth status of children with CKD and prescribe rhGH when indicated.
While this study has the strength of including a large group of pediatric CKD patients in the Asian population, there are some limitations. First, this is a cross-sectional analysis using baseline data from the KNOW-Ped CKD; further longitudinal data analysis is required in future studies. Second, data on nutritional status, body composition change, dietary intake, and physical activity were not collected in this cohort. Therefore, we were not able to determine whether underweight was associated with malnutrition or PEW. Third, the influence of possible comorbidities on growth, such as chromosomal anomalies or syndromic diseases, was not considered for evaluation in the study.
In summary, this study using baseline data from the KNOW-Ped CKD showed that children with CKD were shorter and had lower body weight and BMI than the general population. Short stature in children with CKD was most associated with low birth weight, followed by premature birth, onset before age 2, CKD stages 4 and 5, underweight, and low household income. Our study highlights the need for underweight to receive considerably more attention in children with CKD. For these patients, we should carefully monitor the nutritional status and body composition changes and consider early intensive dietary intervention and nutritional support along with rhGH treatment.
References
Fernández-Iglesias Á, López JM, Santos F (2020) Growth plate alterations in chronic kidney disease. Pediatr Nephrol 35:367–374. https://doi.org/10.1007/s00467-018-4160-7
Rees L, Jones H (2013) Nutritional management and growth in children with chronic kidney disease. Pediatr Nephrol 28:527–536. https://doi.org/10.1007/s00467-012-2258-x
Seikaly MG, Salhab N, Gipson D, Yiu V, Stablein D (2006) Stature in children with chronic kidney disease: analysis of NAPRTCS database. Pediatr Nephrol 21:793–799. https://doi.org/10.1007/s00467-006-0040-7
Franke D, Winkel S, Gellermann J, Querfeld U, Pape L, Ehrich JH, Haffner D, Pavičić L, Zivičnjak M (2013) Growth and maturation improvement in children on renal replacement therapy over the past 20 years. Pediatr Nephrol 28:2043–2051. https://doi.org/10.1007/s00467-013-2502-z
Harambat J, Bonthuis M, van Stralen KJ, Ariceta G, Battelino N, Bjerre A, Jahnukainen T, Leroy V, Reusz G, Sandes AR, Sinha MD, Groothoff JW, Combe C, Jager KJ, Verrina E, Schaefer F (2014) Adult height in patients with advanced CKD requiring renal replacement therapy during childhood. Clin J Am Soc Nephrol 9:92–99. https://doi.org/10.2215/cjn.00890113
Rodig NM, McDermott KC, Schneider MF, Hotchkiss HM, Yadin O, Seikaly MG, Furth SL, Warady BA (2014) Growth in children with chronic kidney disease: a report from the Chronic Kidney Disease in Children study. Pediatr Nephrol 29:1987–1995. https://doi.org/10.1007/s00467-014-2812-9
Kang NR, Ahn YH, Park E, Choi HJ, Kim SH, Cho H, Cho MH, Shin JI, Lee JH, Park YS, Cheong HI, Kang HG, Ha IS, Kwack YS, Han KH (2019) Mental health and psychosocial adjustment in pediatric chronic kidney disease derived from the KNOW-Ped CKD study. Pediatr Nephrol 34:1753–1764. https://doi.org/10.1007/s00467-019-04292-w
Baek HS, Kang HG, Choi HJ, Cheong HI, Ha IS, Han KH, Kim SH, Cho HY, Shin JI, Park YS, Lee JH, Lee J, Ahn C, Cho MH (2017) Health-related quality of life of children with pre-dialysis chronic kidney disease. Pediatr Nephrol 32:2097–2105. https://doi.org/10.1007/s00467-017-3721-5
Furth SL, Stablein D, Fine RN, Powe NR, Fivush BA (2002) Adverse clinical outcomes associated with short stature at dialysis initiation: a report of the North American Pediatric Renal Transplant Cooperative Study. Pediatrics 109:909–913. https://doi.org/10.1542/peds.109.5.909
Gerson AC, Wentz A, Abraham AG, Mendley SR, Hooper SR, Butler RW, Gipson DS, Lande MB, Shinnar S, Moxey-Mims MM, Warady BA, Furth SL (2010) Health-related quality of life of children with mild to moderate chronic kidney disease. Pediatrics 125:e349–e357. https://doi.org/10.1542/peds.2009-0085
Behnisch R, Kirchner M, Anarat A, Bacchetta J, Shroff R, Bilginer Y, Mir S, Caliskan S, Paripovic D, Harambat J, Mencarelli F, Büscher R, Arbeiter K, Soylemezoglu O, Zaloszyc A, Zurowska A, Melk A, Querfeld U, Schaefer F (2019) Determinants of statural growth in European children with chronic kidney disease: findings from the Cardiovascular Comorbidity in Children With Chronic Kidney Disease (4C) Study. Front Pediatr 7:278. https://doi.org/10.3389/fped.2019.00278
Salević P, Radović P, Milić N, Bogdanović R, Paripović D, Paripović A, Golubović E, Milosević B, Mulić B, Peco-Antić A (2014) Growth in children with chronic kidney disease: 13 years follow up study. J Nephrol 27:537–544. https://doi.org/10.1007/s40620-014-0094-8
Hamasaki Y, Ishikura K, Uemura O, Ito S, Wada N, Hattori M, Ohashi Y, Tanaka R, Nakanishi K, Kaneko T, Honda M (2015) Growth impairment in children with pre-dialysis chronic kidney disease in Japan. Clin Exp Nephrol 19:1142–1148. https://doi.org/10.1007/s10157-015-1098-y
Kang HG, Choi HJ, Han KH, Kim SH, Cho HY, Cho MH, Shin JI, Lee JH, Lee J, Oh KH, Park YS, Cheong HI, Ahn C, Ha IS (2016) KNOW-Ped CKD (KoreaN cohort study for outcomes in patients with pediatric CKD): design and methods. BMC Nephrol 17:35. https://doi.org/10.1186/s12882-016-0248-0
Fadrowski JJ, Neu AM, Schwartz GJ, Furth SL (2011) Pediatric GFR estimating equations applied to adolescents in the general population. Clin J Am Soc Nephrol 6:1427–1435. https://doi.org/10.2215/cjn.06460710
Kliger AS, Foley RN, Goldfarb DS, Goldstein SL, Johansen K, Singh A, Szczech L (2013) KDOQI US commentary on the 2012 KDIGO Clinical Practice Guideline for Anemia in CKD. Am J Kidney Dis 62:849–859. https://doi.org/10.1053/j.ajkd.2013.06.008
Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, Lee JH, Kim SC, Lim D, Yang SW, Oh K, Moon JS (2018) The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr 61:135–149. https://doi.org/10.3345/kjp.2018.61.5.135
WHO Multicentre Growth Reference Study Group (2006) WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl 450:76–85. https://doi.org/10.1111/j.1651-2227.2006.tb02378.x
KDOQI Work Group (2009) KDOQI Clinical Practice Guideline for Nutrition in Children with CKD: 2008 update. Executive summary. Am J Kidney Dis 53(3 Suppl 2):S11–S104. https://doi.org/10.1053/j.ajkd.2008.11.017
Lim JS, Lim SW, Ahn JH, Song BS, Shim KS, Hwang IT (2014) New Korean reference for birth weight by gestational age and sex: data from the Korean Statistical Information Service (2008-2012). Ann Pediatr Endocrinol Metab 19:146–153. https://doi.org/10.6065/apem.2014.19.3.146
Clayton PE, Cianfarani S, Czernichow P, Johannsson G, Rapaport R, Rogol A (2007) Management of the child born small for gestational age through to adulthood: a consensus statement of the International Societies of Pediatric Endocrinology and the Growth Hormone Research Society. J Clin Endocrinol Metab 92:804–810. https://doi.org/10.1210/jc.2006-2017
Textor J, van der Zander B, Gilthorpe MS, Liskiewicz M, Ellison GTH (2016) Robust causal inference using directed acyclic graphs: the R package ‘dagitty’. Int J Epidemiol 45:1887–1894. https://doi.org/10.1093/ije/dyw341
Lifshitz F (2009) Nutrition and growth. J Clin Res Pediatr Endocrinol 1:157–163. https://doi.org/10.4274/jcrpe.v1i4.39
Becker PJ, Nieman Carney L, Corkins MR, Monczka J, Smith E, Smith SE, Spear BA, White JV (2014) Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: indicators recommended for the identification and documentation of pediatric malnutrition (undernutrition). J Acad Nutr Diet 114:1988–2000. https://doi.org/10.1016/j.jand.2014.08.026
Brady TM, Roem J, Cox C, Schneider MF, Wilson AC, Furth SL, Warady BA, Mitsnefes M (2020) Adiposity, sex, and cardiovascular disease risk in children with CKD: a longitudinal study of youth enrolled in the Chronic Kidney Disease in Children (CKiD) study. Am J Kidney Dis 76:166–173. https://doi.org/10.1053/j.ajkd.2020.01.011
Schaefer F, Benner L, Borzych-Dużałka D, Zaritsky J, Xu H, Rees L, Antonio ZL, Serdaroglu E, Hooman N, Patel H, Sever L, Vondrak K, Flynn J, Rébori A, Wong W, Hölttä T, Yildirim ZY, Ranchin B, Grenda R, Testa S, Drożdz D, Szabo AJ, Eid L, Basu B, Vitkevic R, Wong C, Pottoore SJ, Müller D, Dusunsel R, Celedon CG, Fila M, Sartz L, Sander A, Warady BA (2019) Global variation of nutritional status in children undergoing chronic peritoneal dialysis: a longitudinal study of the International Pediatric Peritoneal Dialysis Network. Sci Rep 9:4886. https://doi.org/10.1038/s41598-018-36975-z
Larson-Nath C, Goday P (2019) Malnutrition in children with chronic disease. Nutr Clin Pract 34:349–358. https://doi.org/10.1002/ncp.10274
de Onis M, Branca F (2016) Childhood stunting: a global perspective. Matern Child Nutr 12(Suppl 1):12–26. https://doi.org/10.1111/mcn.12231
Abraham AG, Mak RH, Mitsnefes M, White C, Moxey-Mims M, Warady B, Furth SL (2014) Protein energy wasting in children with chronic kidney disease. Pediatr Nephrol 29:1231–1238. https://doi.org/10.1007/s00467-014-2768-9
Fouque D, Kalantar-Zadeh K, Kopple J, Cano N, Chauveau P, Cuppari L, Franch H, Guarnieri G, Ikizler TA, Kaysen G, Lindholm B, Massy Z, Mitch W, Pineda E, Stenvinkel P, Treviño-Becerra A, Wanner C (2008) A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int 73:391–398. https://doi.org/10.1038/sj.ki.5002585
Mak RH, Cheung WW, Zhan JY, Shen Q, Foster BJ (2012) Cachexia and protein-energy wasting in children with chronic kidney disease. Pediatr Nephrol 27:173–181. https://doi.org/10.1007/s00467-011-1765-5
Ku E, Kopple JD, McCulloch CE, Warady BA, Furth SL, Mak RH, Grimes BA, Mitsnefes M (2018) Associations between weight loss, kidney function decline, and risk of ESRD in the Chronic Kidney Disease in Children (CKiD) cohort study. Am J Kidney Dis 71:648–656. https://doi.org/10.1053/j.ajkd.2017.08.013
Mahan JD, Warady BA (2006) Assessment and treatment of short stature in pediatric patients with chronic kidney disease: a consensus statement. Pediatr Nephrol 21:917–930. https://doi.org/10.1007/s00467-006-0020-y
Haffner D, Schaefer F, Nissel R, Wühl E, Tönshoff B, Mehls O (2000) Effect of growth hormone treatment on the adult height of children with chronic renal failure. German Study Group for Growth Hormone Treatment in Chronic Renal Failure. N Engl J Med 343:923–930. https://doi.org/10.1056/nejm200009283431304
Chou HH, Lin CY, Chiou YH, Tain YL, Wang YF, Wang HH, Chiou YY (2016) Clinical characteristics and prevalence of complications of chronic kidney disease in children: the Taiwan Pediatric Renal Collaborative study. Pediatr Nephrol 31:1113–1120. https://doi.org/10.1007/s00467-016-3325-5
Rowe DL, Derraik JG, Robinson E, Cutfield WS, Hofman PL (2011) Preterm birth and the endocrine regulation of growth in childhood and adolescence. Clin Endocrinol 75:661–665. https://doi.org/10.1111/j.1365-2265.2011.04116.x
Bocca-Tjeertes IF, Reijneveld SA, Kerstjens JM, de Winter AF, Bos AF (2013) Growth in small-for-gestational-age preterm-born children from 0 to 4 years: the role of both prematurity and SGA status. Neonatology 103:293–299. https://doi.org/10.1159/000347094
Greenbaum LA, Muñoz A, Schneider MF, Kaskel FJ, Askenazi DJ, Jenkins R, Hotchkiss H, Moxey-Mims M, Furth SL, Warady BA (2011) The association between abnormal birth history and growth in children with CKD. Clin J Am Soc Nephrol 6:14–21. https://doi.org/10.2215/cjn.08481109
Franke D, Alakan H, Pavičić L, Gellermann J, Müller D, Querfeld U, Haffner D, Živičnjak M (2013) Birth parameters and parental height predict growth outcome in children with chronic kidney disease. Pediatr Nephrol 28:2335–2341. https://doi.org/10.1007/s00467-013-2604-7
Mekahli D, Shaw V, Ledermann SE, Rees L (2010) Long-term outcome of infants with severe chronic kidney disease. Clin J Am Soc Nephrol 5:10–17. https://doi.org/10.2215/CJN.05600809
Hidalgo G, Ng DK, Moxey-Mims M, Minnick ML, Blydt-Hansen T, Warady BA, Furth SL (2013) Association of income level with kidney disease severity and progression among children and adolescents with CKD: a report from the Chronic Kidney Disease in Children (CKiD) Study. Am J Kidney Dis 62:1087–1094. https://doi.org/10.1053/j.ajkd.2013.06.013
Availability of data, code, and material
Requests for access to data from the study should be addressed to the corresponding author at kanghg@snu.ac.kr. All proposals requesting data access will need to specify how they plan to use the data, and all proposals will need approval of the trial co-investigator team before data release.
Funding
This study was supported by the Research Program funded by the Korea Centers for Disease Control and Prevention (fund codes 2011E3300300, 2012E3301100, 2013E3301600, 2013E3301601, 2013E3301602, 2016E3300200, 2016E3300201, 2016E3300202, 2019E320100, 2019E320101, and 2019E320102).
Author information
Authors and Affiliations
Contributions
E.P. contributed to the study conception and drafted the article; H.J.L. contributed to the study design and revised the article; I.H., Y.S.P., J.H.L., J.I.S., H.C., K.H.H., S.H.K., and M.H.C. contributed to data acquisition; H.J.C. and Y.H.A. contributed to the analysis and interpretation of data; H.G.K. provided intellectual content of critical importance to the work described and approved the final version of the article to be published. All authors provided review and final approval of the manuscript to be published.
Corresponding authors
Ethics declarations
Ethics approval
This study was approved by the institutional review boards of the participating centers, namely Jeju National University Hospital (Jeju, South Korea), Pusan National University Children’s Hospital (Yangsan, South Korea), Severance Children’s Hospital (Seoul, South Korea), Kyungpook National University Children’s Hospital (Daegu, South Korea), Seoul National University Children’s Hospital (Seoul, South Korea), Samsung Medical Center (Seoul, South Korea), Asan Medical Center (Seoul, South Korea), and Hallym University Kangnam Sacred Heart Hospital (Seoul, South Korea).
Consent to participate
Informed consent was obtained from the parents of all individual participants according to local requirements.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, E., Lee, H.J., Choi, H.J. et al. Incidence of and risk factors for short stature in children with chronic kidney disease: results from the KNOW-Ped CKD. Pediatr Nephrol 36, 2857–2864 (2021). https://doi.org/10.1007/s00467-021-05054-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05054-3