Abstract
Impairment of pubertal growth and sexual maturation resulting in reduced adult height is an significant complication in children suffering from chronic kidney disease (CKD). Delayed puberty and reduced pubertal growth are most pronounced in children with pre-existing severe stunting before puberty, requiring long-term dialysis treatment, and in transplanted children with poor graft function and high glucocorticoid exposure. In pre-dialysis patients, therapeutic measures to improve pubertal growth are limited and mainly based on the preservation of renal function and the use of growth hormone treatment. In patients with end-stage CKD, early kidney transplantation with steroid withdrawal within 6 months of renal transplantation allows for normal pubertal development in the majority of patients. This review focuses on the underlying pathophysiology and strategies for improving height and development in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maintaining optimal pubertal growth and normal sexual maturation are challenging problems in the management of children with chronic kidney disease (CKD): approximately 50 % of children requiring renal replacement therapy (RRT) before their 13th birthday show delayed puberty and have a final height below the normal range [1–4]. A short stature is a marker for increased mortality and hampers the psychosocial integration of pediatric CKD patients [5]. However, there is evidence that, owing to advancements in the medical and technical management of CKD and RRT, height prognosis has substantially improved over the last few decades [1, 2, 4, 6]. Yet, this is not the case in all parts of the world, particularly in those with inadequate local resources, where height prognosis remains dismally low [2]. There is no single cause of impairment of growth and development during adolescence in CKD patients (Table 1). The three most important influences are the degree of pre-existing stunting already acquired during childhood, the severity of CKD, and steroid exposure in transplanted patients. This review summarizes the current knowledge of the phenotype, pathophysiology, and therapeutic options for adolescents with growth failure and delayed puberty resulting from CKD.
Normal pubertal growth and development
Adolescence begins and progresses across a wide age range and differs between the sexes. Careful monitoring of linear growth (height and annual height velocity) and stages of sexual maturity (Tanner stages, testicular volume [boys], and menarche [girls]) are mandatory in detecting abnormal growth and development in children with CKD. Approximately 80 % of growth has already been achieved before puberty. Unfortunately, this growth period is very sensitive to disturbances related to deterioration in renal function or glucocorticoid treatment. This may result in significant growth failure or even growth arrest. Catch-up growth during puberty using any therapeutic measures is often incomplete in CKD patients and it is essential to avoid stunting before puberty.
The earliest stage of puberty is initiated by sleep-augmented pulsatile secretion of pituitary gonadotropins and growth hormone (GH), resulting in the stimulation of ovarian estrogens and testosterone in testes and clinical signs of puberty (girls, Tanner breast stage 2; boys, testicular volume >3 ml). The gonadotropic hormone axis stimulates growth via increased proliferation of growth plate chondrocytes and modulation of GH secretion from the pituitary gland, resulting in the pubertal growth spurt [7].
Effect of CKD on pubertal growth and development
As with any chronic disease, height velocity is most affected during periods of rapid growth (i.e., the first 2 years of life and the pubertal age). In the pre-pubertal years, the appearance of secondary sexual characteristics is delayed and the growth rate is disproportionately decreased [8, 9]. The pubertal growth spurt is later than normal and its degree impaired, resulting in loss of growth potential and reduced final height [7]. Over the last 20 years, although these basic principles remain, new concepts for improving pubertal development have been established.
Pubertal development
Delayed onset and progression of pubertal development was a common feature when RRT programs for children began [8]. Studies of the timing of pubertal onset have been hampered by the fact that bone age is only a crude marker in the assessment of CKD. Indeed, the distribution of bone age at onset of puberty varies at least as much as the distribution of chronological age in these patients. However, data from the late 1980s demonstrated a delay in pubertal onset of 2 to 2.5 years [8]. Although the onset of puberty is usually delayed in CKD patients, the progression through the pubertal stages appears to be normal or only slightly delayed. Studies in the 1980s reported that menarche occurs after the upper limit of the normal age range (i.e., 15 years) in almost half of the girls treated by dialysis or transplantation [10]. Moreover, despite the achievement of pubertal stage IV or V, a substantial proportion of dialysis patients presented with a permanently impaired reproductive function [11]. Fortunately, over the last 20 years, most children requiring RRT before puberty presented with normal or only slightly delayed pubertal onset. In three recent studies, mean age at pubertal onset and at menarche did not differ in children on RRT and healthy children, and the serum levels of pubertal reproductive hormones were normal in the great majority of patients [12, 13]. Bone maturation continues to be delayed by approximately 1.4 years compared with healthy children, although this does not have a negative impact on pubertal development [1]. Therefore, delayed puberty in a patient with CKD should nowadays not be assumed to be “normal.” but should lead to a thorough clinical work-up for other causes of pubertal delay, e.g., Ullrich Turner syndrome, and other gonadal disorders. It has to be kept in mind that certain underlying kidney disease are frequently associated with gonadal insufficiency/dysgenesia, e.g., syndromes related to mutations in the Wilms tumor gene, WT1 (Denys–Drash syndrome, Frasier syndrome), and nephropathic cystinosis. In addition, pubertal delay could also be caused by treatment with glucocorticoids or other drugs that can potentially interfere with sex hormone production. Finally, the age at onset of puberty correlates positively with the age at transplantation. Thus, early renal transplantation (KTx) is a prerequisite for the prevention of pubertal delay in children with stage 5 CKD [9, 12].
Pubertal growth
In general, the severity of the relative growth retardation at the time of puberty correlates positively with the delay in skeletal maturation [7]. In puberty, there is such an acceleration in skeletal maturation that the bone age deficit is reduced [9]. However, bone ageing and growth during puberty are disassociated in CKD patients, resulting in an irreversible loss of growth potential. Consequently, assessment of bone age in pubertal CKD patients is not helpful in clinical practice, except to exclude epiphyseal closure before and after initiation of GH treatment [7].
During the last two decades, in parallel with the improvement in sexual maturation, there has been an improvement in pubertal height gain [1, 2, 4, 9, 12]. Longitudinal growth in 384 German children on RRT who were followed up between 1998 and 2009 was compared with that in 732 children enrolled in the European Dialysis and Transplant Association (EDTA) Registry between 1985 and 1988 (Fig. 1) [1]. In line with previous studies, the pubertal growth spurt in the EDTA patients was delayed by approximately 2.5 years. In many patients no clear pubertal growth spurt was present, and consequently standardized height was decreased during puberty (Fig. 1a). In contrast, a clear pubertal growth spurt was present and the onset of the pubertal growth spurt was within the normal range in the majority of those patients followed up more recently. Consequently, standardized height even improved during puberty and until adult height (Fig. 1b). A strong negative correlation between total pubertal height gain and age at transplantation was reported in two studies [9, 12]. Thus, whereas 20 years ago a loss of about 1.0 SD was expected during puberty, nowadays a normal or only slightly reduced pubertal growth spurt can be expected if long-term dialysis is avoided.
a Mean height velocity of European children with renal replacement therapy in the European Dialysis and Transplant Association (EDTA) study 1985–1988 (blue lines) versus the Hannover/Berlin (HB) pediatric population cohort 1998–2009 (red lines) in different age cohorts. Reproduced from Franke et al. [1], used with permission. b Age-dependent height standard deviation score (SDS) of European children on renal replacement therapy 1985–1988 (EDTA study, n = 732, blue error bars) and in the HB group (n = 384, red error bars). Reproduced from Franke et al. [1], used with permission. CI confidence interval
Segmental growth
It has been postulated that during malnutrition there is preferential preservation of growth of vital organs at the expense of less vital tissues such as the limbs, so that malnutrition during childhood results in disproportionate stunting with impairment of leg growth, and preserved trunk and head growth [14]. In the CKD Growth and Development Study, pediatric CKD patients have been prospectively followed-up by detailed standardized evaluation of body morphology at two pediatric nephrology centers in Northern Germany since 1998. Analysis of linear growth in a mixed cohort of 190 boys with a long-term history of CKD and RRT demonstrated an age related disproportionate growth pattern [15]. Sitting height was mostly preserved, whereas leg and arm growth was most severely affected. This resulted in a markedly elevated sitting height index (ratio of sitting height to total body height). Leg lengths were more affected in prepubertal compared to pubertal children. Consequently, body disproportion was less pronounced in pubertal patients. Similar results were recently obtained in a cohort of 398 prepubertal and pubertal KTx patients [16].
Final height and height prediction
When interpreting the final height of patients treated for CKD in childhood, it has to be noted that the data obtained will reflect treatment practices spanning the previous two decades. Furthermore, most reports of final height do not, or incompletely, discriminate according to patient characteristics (e.g., diagnoses, ages at onset of CKD, types and durations of RRT), and, in particular, registries do not separate out children with comorbidities that affect growth in their own right. With that in mind, reduced adult height has been reported in up to 50 % of CKD patients, although there has been a trend toward improvement over the past decade (Fig. 2) [1–4, 8, 9]. Mean final height varies from 148 to 158 cm for women and 162–168 cm for men (second centiles 151 and 163 cm respectively).
Changes in final height SDS over time according to the age and period of start of RRT (n = 981). Reproduced from Harambat et al. [2], used with permission. The horizontal line in the middle of the box represents the median, the bottom and top of the box represent the lower and upper quartiles respectively, and the ends of the whiskers represent the 10th and the 90th percentiles. RRT renal replacement therapy
There is evidence that over the years, final height post-transplantation is improving [3]. This is likely to be due to a combination of factors, such as better growth attained pre-transplant, adequate nutrition and GH therapy, and pre-emptive transplantation, thus avoiding dialysis, and to the development of protocols that minimize the use of corticosteroids [3, 16]. European data show an improvement in final height from −2.06 SDS in children who reached adulthood in 1990–1995 to −1.33 SDS in 2006–2011 [2]. Older age at start of RRT, beginning RRT more recently, cumulative time with a transplant, and greater height SDS at initiation of RRT were independently associated with a higher final height SDS. Most impressively, recent results of the avoidance of post-transplant steroids altogether are excellent, with mean final heights of 177 and 175 cm in men transplanted prepuberty and postpuberty respectively, with similar figures of 165 and 162 cm for women (Fig. 3) [4].
Mean standardized height at the time of renal transplantation compared with adult height and comparison of adult height with genetic target height in patients with steroid withdrawal during months 4–6 after transplantation. Reproduced from Klare et al. [4], used with permission. a Mean standardized height at the time of transplantation and final height in prepubertal (n = 36) and pubertal (n = 24) patients. b Mean adult height (open bars) and genetic target height (hatched bars) in boys (n = 25) and girls (n = 17). Data in a and b are given as mean ± standard error of the mean (SEM)
A recent analysis from the ESPN/EDTA registry has shown that, after adjustment for age and period of initiation of RRT, final height increased significantly from −1.93 SDS in children who started RRT before 1990, to −1.78 in children from 1990 to 1999, and to −1.61 in those starting RRT after 1999 (p <0.001), [4]. The improvement in final height over time was independent of age at the start of RRT (Fig. 2). Poorest growth outcomes were associated with an earlier start and longer duration of dialysis or diagnosis of a metabolic disorder, such as cystinosis and hyperoxaluria, whereas those with a longer time spent with a renal transplant and those treated with GH achieved the most growth [2, 17–19].
The applicability of adult height prediction methods in children suffering from CKD is questionable. Final height was over-predicted by 3 to 10 cm in several validation studies [8, 9, 17]. Most likely this reflects the complexity and thus unpredictability of growth and development in chronic uremia, with a highly variable and dynamic impact of disease progression, medication, bone disease, RRT modalities, skeletal maturation, and pubertal timing [17].
Causes of growth failure during puberty in CKD
Growth failure in CKD is due to a complex interplay of many different factors (Table 1). Most of the factors contributing to growth failure during infancy and childhood are also at work during puberty. However, congenital CKD, malnutrition, and birth-related factors have an impact mainly on growth in early life, whereas with hormonal disturbances it is mainly during childhood and adolescence. Some of these factors are potentially correctable (e.g., hormonal abnormalities, acidosis, and anemia); the effects of others, such as birth parameters, associated syndromes, race, and parental height, are not.
Cause of renal disease
The most common cause of congenital CKD is a congenital abnormality of the kidney and urinary tract (CAKUT) resulting in renal tubular sodium and bicarbonate loss and severe growth failure and a reduced final height. Acquired glomerulopathies are a frequent cause of growth failure during puberty [2]. The nephrotic state per se and glucocorticoid treatment are known risk factors. Prolonged high corticosteroid doses lead to severe growth failure. Although partial catch-up growth can be seen after cessation of glucocorticoid treatment, this is rarely observed in pubertal patients [20].
The most severe growth failure, which can be very difficult to treat, occurs in patients suffering from complex tubular disorders, such as Fanconi syndrome [21, 22]. Systemic metabolic disorders (such as cystinosis, hyperoxaluria and mitochondrial cytopathies) resulting in complex tubular dysfunction, progressive loss of renal function, and involvement of the endocrine system or other vital organs (e.g., liver, bone, and brain), also lead to severe growth failure [2]. In children with nephropathic cystinosis, growth failure already occurs in infancy when glomerular function is typically not yet compromised. Progressive growth failure and reduced pubertal height gain is further sustained by generalized deposition of cystine crystals altering the function of the growth plate, bone marrow, hypothalamus, and pituitary and thyroid glands. Early initiation of treatment with cysteine-depleting agents (cysteamine) results in the preservation of renal function, or at least in a delay in the development of CKD, and improvement of prepubertal and pubertal growth [22]. In patients with systemic oxalosis, combined liver and kidney transplantation is a curative option; however, real catch-up growth after combined transplantation is rarely observed in pubertal oxalosis patients [19].
Stage of CKD and dialysis
Even a moderate reduction of glomerular filtration rate (GFR) has been reported to result in impaired growth. The principal registry providing data on the epidemiology of growth in conservatively managed CKD is the North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS). The 2006 report covers the 10 years between 1994 and 2004 and includes a very large cohort of over 5,000 children with GFRs of up to 75 ml/min/1.73 m2 [23]. As expected, the most severely growth-retarded were the youngest children, but mean height SDS was also reduced at pubertal age (−2.3 at 0 to 2, and −1.0 at >12 years). Although height deficit was less pronounced during the pubertal age, standardized height worsened with progression of CKD in all age groups. Short stature is even more common in children on dialysis. The United States Renal Data System (USRDS) is another registry collecting data on patients on RRT programs in the USA. Their 2007 report shows that the height and weight of approximately half of patients requiring dialysis treatment during puberty was below the 20th centile for the healthy population [24]. Within the ESPN/ERA-EDTA registry, adult height in patients with advanced CKD requiring RRT during childhood was analyzed. Mean adult height SD scores, adjusted for age at start of RRT and primary renal disease, was significantly lower in patients started on peritoneal (−1.86) or hemodialysis (−1.81) compared with those receiving a renal transplant (−1.57) [2]. Taken together, pubertal growth is best preserved in patients with mild to moderate CKD, patients on dialysis are shorter than their transplanted peers, although all groups are below the height of the normal age-matched population.
Protein calorie malnutrition
Protein calorie malnutrition plays a major role in the pathophysiology of growth failure in infants and young children, but has a rather low impact during puberty [25]. However, similar to patients presenting with anorexia nervosa, severe malnutrition may result in delayed, arrested or even absent pubertal development. Vomiting is rarely observed in adolescent patients, and may be due to gastro-esophageal reflux especially in peritoneal dialysis (PD) patients.
Protein energy wasting
Protein energy wasting (PEW) is characterized by maladaptive responses including anorexia, elevated basic metabolic rate, wasting of lean body tissue, and under-utilization of fat tissue for energy [25]. In contrast to malnutrition, PEW can only be partially reversed by increased nutrition. Chronic inflammation is the most likely cause of PEW in CKD patients, resulting in growth failure and reduced adult height. Currently, novel therapeutic strategies, such as ghrelin agonists and melanocortin antagonists, are being tested to overcome PEW in CKD patients.
Obesity
Although malnutrition is nowadays rarely seen in adolescent CKD patients, obesity is an increasing problem, as it is in the healthy population. In the ESPN/ERA-EDTA registry (N = 5,199) the prevalence of underweight in pediatric CKD patients was 4.3 %, whereas 19.6 and 11.2 % were overweight or obese respectively [26]. The prevalence of overweight/obesity is particularly high among transplanted patients [26]. In addition, patients with Bardet–Biedl syndrome are prone to obesity before and after KTx. In a study of 68 prepubertal and pubertal KTx patients, all on daily steroids, the most predictive parameter of inappropriate weight gain over 3 years was the body mass index of the mother [27]. This strongly suggests that genetic and/or environmental factors might be involved in the development of post-transplant obesity. Regular nutritional advice to patients and their families and the use of steroid-sparing regimens are suitable measures for the mitigation of post-transplant obesity in adolescent patients [26].
Metabolic acidosis
Metabolic acidosis usually begins when the GFR falls below 50 % of normal, and is associated with decreased (pubertal) growth and increased protein breakdown [7]. Metabolic acidosis induces a state of GH insensitivity [28] that is likely to contribute to impaired longitudinal growth in CKD patients.
Disturbances of water and electrolyte balance
Although the relationship between salt loss and growth failure has not been formally proven in CKD, children with isolated tubular disorders resulting in urinary salt and water losses show severe growth retardation, which can be at least partly resolved by adequate salt and water supplementation [29].
CKD mineral and bone disorder
It is widely accepted that skeletal deformities due to CKD mineral and bone disorders (CKD-MBD) contribute to uremic growth failure [30]. Pronounced secondary hyperparathyroidism can interfere with longitudinal growth by destruction of the growth plate architecture, epiphyseal displacement, and metaphyseal fractures. Severe destruction of the metaphyseal bone architecture may result in complete growth arrest. Although there is no strong evidence, older data suggest a possible role of vitamin D in improving pubertal growth [31, 32].
Anemia
Long-standing anemia in CKD patients has profound systemic consequences, including anorexia and catabolism due to altered energy turnover, and multiple dysfunction of organ systems. Although the short-term stimulatory effects of erythropoietin treatment on longitudinal growth have been reported anecdotally, no persistent catch-up growth could be demonstrated in several multicenter clinical trials [33].
Endocrine changes
Uremia interferes with the metabolism and regulation of various peptide hormones. This leads to inappropriate concentrations of circulating hormones and/or altered hormone action on target tissues. Distinct alterations of the somatotropic and gonadotropic hormone axes have been identified, which are believed to play an important role in uremic growth failure [7].
Gonadotropic hormone axis
Gonadal hormones
Low or low to normal, total, and free testosterone (T) and dihydrotestosterone (DHT) plasma concentrations due to decreased synthesis and/or increased metabolic clearance have been reported in adolescents and adults with long-standing uremia. The reduced conversion of T to DHT secondary to diminished 5α-reductase activity may contribute to the delayed pubertal development seen in some boys on dialysis. Similarly, plasma estradiol levels in women tend to decrease in parallel with GFR reduction, and some adolescent girls show low to normal or decreased estradiol levels in relation to pubertal age [7]. However, these observations were all made more than 20 years ago. Nowadays, at least in transplanted children, this issue seems to be resolved. In two recent studies, the majority of transplanted children without previous long-term dialysis had normal estradiol and testosterone levels [12, 13]. This may at least partly explain the improvement in pubertal development in patients on RRT over the last few decades [1].
Gonadotropins
Increased plasma concentrations of luteinizing hormone (LH) and follicle-stimulating hormone (FSH), in combination with decreased or low to normal gonadal hormones, suggest a state of compensated hypergonadotropic hypogonadism in patients with stage 5 CKD [34]. However, in patients on dialysis, gonadotrophin secretion may be inadequate relative to the degree of hypogonadism. This is compatible with an additional pituitary gonadotropin release defect, and the analysis of spontaneous pulsatile LH secretion has provided insights into the underlying pathophysiology [35, 36]. In dialyzed patients mean LH plasma levels are elevated despite significantly reduced pituitary LH secretion, owing to the markedly impaired renal metabolic clearance of LH. When renal function is restored by kidney transplantation, pulsatile LH secretion normalizes and hypergonadotropic FSH and/or LH levels are only rarely observed [12, 13]. Animal studies suggest that a primary hypothalamic defect may contribute to the delayed onset of puberty in patients with uremia. The observed reduced release of hypothalamic gonadotropin-releasing hormone (GnRH) is due to uremia-related inhibitory factors and/or an increase in the inhibitory neurotransmitter gamma-aminobutyric acid [37, 38]. Beyond the quantitative alterations of gonadotropin release, uremia also affects the biological quality of circulating gonadotropins. In pubertal and adult dialysis patients the proportion of bioactive LH in relation to the total immunochemically measurable amount of LH is reduced. This may be due to altered glycosylation and/or accumulation of less active isoforms [39].
Taken together, insufficient activation of the hypothalamic GnRH pulse generator, likely mediated via circulating inhibitors, appears to be the key abnormality underlying delayed puberty and altered sexual function in patients with stage 5 CKD. This statement was also thought to be true for KTx patients some 20 years ago. However, those patients often had a history of long-standing dialysis and high-dose glucocorticoid treatment. Recently, Förster et al. evaluated gonadotropic hormones in 33 KTx patients (19 boys) aged 16.0–16.9 years. LH, FSH, androstenedione, dehydroepiandrosterone sulfate, or testosterone/estradiol levels were within normal ranges for the local age-matched population in almost all patients [13]. Thus, renal transplantation is able to completely normalize all these alterations in the majority of patients if long periods on dialysis treatment are avoided.
Growth hormone: insulin-like growth factor-1 axis
Chronic kidney disease is a state of GH resistance, as there is poor growth in association with normal or high GH levels and decreased IGF-1 bioactivity [40]. Fasting GH concentrations are normal or even increased, owing to reduced renal metabolic clearance, resulting in a prolonged plasma half-life of GH [41]. Pituitary GH secretion is unaltered in prepubertal patients, but decreased in adolescents with CKD, suggesting insufficient stimulation by gonadal steroids during puberty [42, 43]. In addition, malnutrition, metabolic acidosis, and glucocorticoid treatment have a negative impact on GH secretion rates in CKD patients, resulting in reduced pubertal height gain [44].
Experimental studies demonstrated that the GH-induced hepatic, and the growth plate cartilage IGF-1 synthesis, is diminished, due either to decreased expression of the GH receptor (GH-R) and/or a post-receptor signaling defect, impairment of Janus kinase 2/signal transducer and activator of transcription (JAK-STAT) signaling [45]. Recent studies suggest that the chronic inflammatory state associated with CKD contributes to GH resistance, probably by enhancement of suppressors of cytokine signaling (SOCS) [46]. Apart from GH resistance, insensitivity to IGF-1 is also found in patients with advanced CKD [47]. All these findings strongly support the concept of the multilevel homeostatic failure of the GH–IGF-1 system in CKD [45].
Corticosteroid treatment
Long-term glucocorticoid treatment in patients after transplantation leads to diminished longitudinal growth by impairment of the somatotropic hormone axis. High-dose glucocorticoid treatment suppresses pulsatile GH release from the pituitary gland [48]. The physiological increase in GH secretion during puberty is reduced in allograft recipients receiving glucocorticoid treatment and the association between sex-steroid plasma concentrations and GH release observed in healthy adolescents is blunted [48]. These changes are mainly due to increased hypothalamic somatostatin release. In addition to reduced GH release, corticosteroids suppress GH-R mRNA and protein in animals and most likely also in humans [49]. Consequently, hepatic IGF-1 mRNA levels are reduced in animals receiving glucocorticoids. Local effects of glucocorticoids at the growth plate include reduction of IGF-1 production, inducing IGF-1 resistance, which results in a reduction of chondrocyte proliferation, matrix synthesis, and hypertrophy [49].
Strategies to attain normal pubertal growth and development in CKD patients
General measures
Maintenance of adequate nutrition with regard to energy and protein intake is mandatory in adolescent CKD patients [7]. However, the growth-depressing effects of malnutrition are less pronounced compared with that in younger ages. In general, the targeted caloric intake should be between 80 and 100 % of the recommended daily allowance (RDA) for healthy adolescents. Protein intake should be 100 % of RDA. In patients on peritoneal dialysis, a higher intake (+0.2 g/kg/day) is recommended to compensate for dialytic protein losses. The aim is to maintain a normal serum albumin and urea below 20 mmol/l as far as possible. Metabolic acidosis should be vigorously treated by alkali supplementation, aiming at bicarbonate levels of at least 22 mmol/l. In addition, supplementation of water and electrolytes is essential in patients presenting with polyuria and/or salt-losing nephropathies. However, none of the above therapeutic procedures has been demonstrated to induce catch-up growth in short pubertal children with CKD.
Dialysis and intensified dialysis
Although dialysis reduces uremia, longitudinal growth is not usually improved and long-term PD or hemodialysis (HD) is associated with a gradual loss of standardized height in adolescents [50]. Patients on dialysis who maintain some residual renal function have the best growth. It has been suggested that intensified dialysis, achieved by either extended thrice-weekly sessions, daily nocturnal or short daily sessions, may be able to induce catch-up growth [51]. According to a recent study, catch-up growth can be maximized when intensified hemodiafiltration (3 h, 6 times a week) and GH therapy are combined [52]. Using this approach in 15 mainly prepubertal children for an average observation time of 21 months, mean standardized height increased by 1.7 SDS, representing complete catch-up growth according to the attainment of the target height SDS. It remains to be seen whether the growth-promoting effects of intensified dialysis are sustained during puberty.
Intermittent nocturnal hemodialysis allows for free dietary intake and improves protein catabolic rate and appetite in adolescent patients [53]. This results in significant weight gain and increased serum albumin levels compared with conventional HD treatment. It is tempting to speculate that this might also improve pubertal development. However, this must be proved in adequately designed studies.
Transplantation
Although many of the metabolic and endocrine disorders contributing to uremic growth failure are resolved by renal transplantation, post-transplant catch-up growth is rarely seen during adolescence [3, 9]. In addition to transplant function, age, severity of stunting at the time of transplantation and glucocorticoid dosage are inversely associated with longitudinal growth. One retrospective study found that while standardized height was comparable at the time of transplantation, growth rates during puberty were significantly higher among living-related donors (LRD) than deceased donor transplant (DDT) during puberty [54]. This benefit of LRD grafts was independent of GFR, thus arguing in favor of preferential LRD in children with regard to post-transplant growth. However, this beneficial effect of LRD on pubertal growth was not observed in registry studies [3].
An analysis using data from the NAPRTCS was recently reported by Fine et al. [3]. The authors assessed the growth spurt of each of 132 recipients with Tanner stages 2 to 5. The mean increment in height from Tanner stage 2 to stage 5 was 18.8 cm (21.7 cm in 4.7 years for boys and 14.3 cm in 4.5 years for girls). This indicates a reduction of the cumulative pubertal height gain by approximately 30 and 40 % in boys and girls respectively.
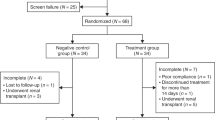
Nissel et al. evaluated pubertal growth in 37 KTx recipients [9]. Although peak height velocity during puberty was significantly increased compared with healthy children, total pubertal height gain was reduced by 20 % because of its shortened duration (Fig. 4). Mean standardized height significantly increased from the time of KTx until final height by 1.3 SD and 0.7 SD in children transplanted before and after the start of puberty respectively. Total pubertal height gain was associated with age at start of puberty, GFR, and age at KTx.
Synchronized mean height velocity curves (left panels) and synchronized mean growth curves (right panels) of boys (upper panels) and girls (lower panels) transplanted before the onset of puberty, compared with normal children. Reproduced from Nissel et al. [9], used with permission. RTx renal transplantation, MHV minimal prespurt height velocity, PHV peak height velocity, EHV end-point height velocity
It is important to note that the vast majority of patients included in the reports by Fine et al. [3] and Nissel et al. [9] were on daily glucocorticoid treatment. It must be stressed that even low-dose glucocorticoid treatment (<4 mg/m2/day) results in growth suppression in children after KTx. In a recent randomized trial of late steroid withdrawal in patients on treatment with cyclosporine A, mycophenolate mofetil steroid-free patients showed improved growth compared with controls (i.e., change in height SDS; 0.6 ± 0.1 vs −0.2 ± 0.1) within 27 months [55]. However, catch-up growth in pubertal patients (0.3 SDS) was rather limited compared with that in prepubertal patients (0.7 SDS). It seems logical that if steroids are withdrawn at an early stage, or even completely avoided, a better growth outcome will be observed. However, an absence of significant catch-up growth among pubertal children (n = 50) was observed in the 2-year follow-up of the Twist study where corticosteroids were withdrawn at day 4 after KTx [56]. Likewise, in the National Institutes of Health-sponsored trial, complete steroid avoidance did not result in a significant increase in standardized height in pubertal patients within 3 years post-transplant compared with controls [57].
Klare et al. evaluated the effect of steroid withdrawal on final adult height in prepubertal and pubertal children (n = 74). In this uncontrolled single-center study patients were weaned off steroids within 6 months of transplantation [4]. Mean adult height was −0.5 ± 1.1 SDS and −1.0 ± 1.3 SDS in prepubertal and pubertal patients and was within the normal range (> −2 SD) in 94 and 80 % respectively (Fig. 3). Unfortunately, final height data from randomized controlled trials on steroid withdrawal/avoidance are lacking.
Although experimental data indicate that mTOR inhibitors may interfere with chondrocyte proliferation and/or gonadal hormone synthesis, recent case–control studies in transplanted children revealed similar growth rates and pubertal development in patients with and without mTOR inhibitor treatment [13, 58].
Recently, the effect of KTx on segmental growth was assessed in a cohort of 398 prepubertal and pubertal pediatric transplant recipients [16]. As expected, KTx patients revealed disproportionate growth failure. Leg length was most impaired, whereas sitting height was best preserved. After early childhood a sustained increase in standardized leg length and total body height was observed from preschool throughout puberty until adulthood, resulting in restoration of body proportions in most patients (Fig. 5). Time after transplantation, congenital renal disease, bone maturation, steroid exposure, degree of metabolic acidosis and anemia, intrauterine growth restriction, and parental height were significant predictors of linear body dimensions and body proportions during childhood and adolescence. Thus, KTx seems to be an effective measure not only in improving stature but also in normalizing body proportions in patients with end-stage CKD. In summary, efforts to avoid a height deficit before transplantation, preemptive transplantation, and the use of efficacious immunosuppressive strategies for optimized graft function and early withdrawal, or even complete avoidance, of steroids are suitable measures for improving pubertal growth and final height [7, 9, 16].
Mean sitting height index (ratio between trunk length and total body height) as a function of age in 389 renal transplant recipients. Reproduced from Franke et al. [16], used with permission. *P < 0.05 for age cohorts of 3 years versus 5 years; **P < 0.05 for age cohorts of 2–5 years vs 8–12 years; ***P < 0.05 for age cohorts of 8–12 years versus 14–18 years. Data are given as mean and 95 % CI. Horizontal lines refer to the normal mean (0 SDS) and upper normal range (2.0 SDS)
Endocrine therapies
Sex hormones
There are few reports on the use of sex hormones in children with CKD; these children suffer growth retardation and extremely delayed puberty. Kassmann et al. showed a short-term growth response to low-dose testosterone administration in prepubertal hemodialysis boys with poor pretreatment growth, whereas short-term height velocity did not change in boys with “normal” pretreatment growth rates [59]. Low-testosterone treatment in 4 male end-stage CKD patients aged 19–21 years with extreme growth delay in puberty resulted in a rapid increase in growth velocity and development of secondary sexual characteristics; however, bone maturation accelerated disproportionately, at rates of 2 to 4 years of bone age per year of chronological age, resulting in a dramatic loss of predicted height [60]. Currently, treatment of growth failure in CKD patients with sex steroids must be viewed with caution. Particularly in cases of extreme pubertal delay, the growth plate of patients with CKD may be hypersensitive to stimulation by sex steroids [7].
However, treatment of hypogonadism by the substitution of sex steroids in adolescent CKD patients seems to be justified, to induce development of secondary sexual characteristics and to help to match the patients with their peers [59]. However, nowadays hypogonadism is rarely observed in adolescent CKD patients, even in those with long-standing dialysis treatment. Therefore, causes of hypogonadism other than CKD should be excluded before starting treatment.
Calcitriol
Although calcitriol supplementation reverses the biochemical, radiographic, and histological signs of CKD-MBD, consistent improvement in pubertal growth has been lacking in clinical studies [61]. These conflicting results may be due to differences in the mode of administration and the pleiotropic calcitriol-specific effects on growth plate chondrocytes. Current pediatric consensus guidelines differ markedly with regard to the optimal parathyroid hormone (PTH) range [61]. European guidelines (EPDWG) recommend that PTH be maintained within the normal range in children with GFR <30 ml/min/1.73 m2, and within 2–3 times the upper limit of normal (ULN) in stage 5 CKD, irrespective of age. By contrast, the USA-based k/DOQI guidelines recommend a target range of 3–5 times the ULN in stage 5 CKD. The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines recommend a PTH target range of 2–9 times the ULN in stage 5. However, none of these recommendations has been validated in a large pediatric stage 5 cohort. Recent data from large registries suggest an optimal PTH target range of 1.7–3 times the ULN in pediatric PD patients to avoid CKD-MBD-associated complications, such as growth failure [61].
Calcimimetics
Pilot studies have provided preliminary evidence that calcimimetics are an effective therapy for secondary hyperparathyroidism in pediatric dialysis patients [62]. Calcimimetics (cinacalcet) have been shown to improve food efficiency and body weight gain in uremic rats, but no effects on growth plate morphology and/or longitudinal growth were seen [63]. However, there is no evidence that calcimimetics affect pubertal growth in CKD patients.
Growth hormone
The unraveling of the pathomechanisms by which CKD impairs the action of endogenous GH paved the way for pharmacological treatment with recombinant human GH [64]. Administration of GH markedly stimulates IGF-1 synthesis, with only a modest effect on IGF binding proteins, thereby normalizing somatomedin bioactivity and promoting longitudinal growth [65]. The efficacy and safety of GH therapy in children with CKD during prepuberty and puberty has been shown extensively, although there has never been a randomized, controlled trial on its effects on final adult height [66].
Effects of GH on pubertal growth and final height
The analysis of pubertal growth in CKD patients is complicated by the fact that the pubertal growth spurt is usually delayed and shortened compared with that in healthy children. Moreover, during the physiological deceleration of height velocity before the onset of the pubertal growth spurt, the growth response during long-term GH treatment may appear disappointing, frequently causing physicians to curtail treatment. However, a marked pubertal growth spurt can still be expected in these patients (Fig. 6), [67].
Individual growth chart of a girl treated with growth hormone therapy for many years, showing a dip in height velocity during the period before the start of puberty. Reproduced from Hokken-Koelega et al. [67], used with permission. TH target height
In a study following up patients with CKD from late prepuberty to final height, the average height increment in GH-treated patients was twice that seen in a retrospective control group. The main benefit for total growth and final height was achieved before the onset of the pubertal growth spurt, whereas no overall effect on the pubertal height gain was observed [17]. The apparent inefficacy of GH administration during puberty in this analysis may in part be explained by the fact that GH treatment was stopped during puberty (mainly because of KTx) in 50 % of patients. Indeed, the pubertal height gain was positively correlated with the duration of GH treatment during this growth period. GH therapy did not accelerate bone maturation or induce an earlier onset of puberty. Unfortunately, there has never been a randomized controlled trial on the impact of GH treatment during the pubertal growth period in CKD patients. Such a randomized controlled trial could address whether a short-term course of GH during the period of pubertal growth would enhance growth and have a positive impact on final adult height.
The median change in standardized height until attainment of adult height in 11 studies, comprising a total of 313 CKD patients on various modes of RRT, amounted to 0.9 SDS (range 0.3–1.4 SDS) [7]. Recently, the determinants of final height were analyzed in 240 GH-treated children on conservative treatment, dialysis or after transplantation, reported to the Pfizer International Growth Study (KIGS) registry (Fig. 7) [18]. In children with normal pubertal timing the mean increase in standardized height from prepuberty to final height was 1.3 SDS. Patients with delayed onset of puberty achieved a significantly smaller increase in standardized height (+0.9 SDS). However, the mean age at initiation of GH treatment in these patients was 14.5 years and the mean duration of GH therapy was only 2.0 years. The average cumulative increase in height SDS was significantly greater in CKD patients who remained on conservative treatment throughout puberty (+1.5 SDS) than in those on dialysis and in renal allograft recipients (both +1.1 SDS). Adult height was independently positively predicted by the height attained at the start and duration of GH treatment, and inversely, by the time spent on dialysis, the age at onset of puberty, and the age at the start of GH. Hence, evidence suggests that GH might improve final height in prepubertal and pubertal patients, but growth response is diminished in patients with delayed onset of puberty and those on long-term dialysis [18].
a Mean height SDS of growth hormone (GH)-treated boys (full circles; n = 193; aged 4.7–19.7 years) and girls (open circles; n = 47; aged 8.1–18.0 years) with chronic kidney disease (CKD) in the year before the start of therapy until attainment of near-final height. Reproduced from Nissel et al. [18], used with permission. Data are given as mean ± SEM; #P < 0.01 boys vs girls; * P < 0.01 vs previous time point. b Mean height SDS of prepubertal CKD patients with normal (open circles, n = 68; aged 4.7–13.0 years) or delayed (open squares, n = 25; aged 10.1–17.1 years) onset of puberty and patients in early (closed triangles, n = 112; aged 10.1–19.7 years) and late (closed diamonds, n = 35; aged 13.8–19.5 years) puberty in the year before the start of GH therapy until attainment of near-final height (data are given as mean ± SEM; *P < 0.003 vs previous time point)
GH treatment strategies during puberty
The optimal dose of GH in prepubertal and pubertal CKD patients is 0.33 mg/kg/week [66]. The growth response to GH treatment is positively associated with residual renal function, target height, initial target height deficit, and duration of GH treatment, and inversely with age at the start of treatment [17, 18, 68]. GH treatment should be started as soon as growth retardation has failed to respond to optimization of conservative measures, e.g., nutritional, metabolic, and hematological intervention [66]. However, GH treatment may induce significant catch-up growth even in late puberty. Exclusion of epiphyseal closure before and during GH treatment is mandatory in this setting. The primary treatment target should be to achieve a height according to the patient’s individual genetic percentile chart. Treatment may be suspended once this target is reached, but growth should be monitored closely. Otherwise, GH should be continued throughout puberty until adult height has been achieved (Fig. 6). After renal transplantation GH should be stopped. If growth remains subnormal, weaning of glucocorticoids should be the first therapeutic consideration, and reinstitution of GH restricted to those patients with insufficient catch-up growth after steroid withdrawal or with a permanent need for maintenance glucocorticoid medication [7, 66].
Future perspectives
Despite attention to preservation of growth potential during prepuberty and the availability of GH therapy, the maintenance of normal pubertal height gain remains a great challenge in CKD patients. If early renal transplantation is not possible, intensified hemodialysis is a promising option. Other avenues currently at the research stage include recombinant IGF-1, administered as a monotherapy or in combination with GH, and targeting of the SOCS2 signaling pathway [69]. The latter is a theoretical possibility because the chronic inflammatory state associated with CKD contributes to GH resistance—an important pathway in metabolism [46].
Pharmacological inhibition of epiphyseal closure may allow an extended duration of the remaining growth period. Since the closure of the epiphyseal growth plate is induced by local estrogen action, inhibition of estrogen synthesis is a principal therapeutic option. Gonadotropin-releasing hormone analogs arrest pubertal progress, but the potential growth benefit would come at the psychological cost of delayed sexual maturation. In boys, aromatase inhibitors, which suppress the local conversion of testosterone to estradiol, may extend the growth phase without affecting pubertal development and thereby increase the window for GH therapy. Initial proof of this concept has recently been provided in short adolescent boys treated with GH combined with the aromatase inhibitor anastrozole [70]. Although some case reports on this treatment option look promising, carefully designed studies proving efficacy and safety in CKD patients must be undertaken before this treatment modality can be recommended [71].
Conclusions
Pubertal growth and sexual maturation in children with CKD has markedly improved during the last two decades. Adequate treatment, e.g., nutrition, metabolic control, and GH therapy, must be undertaken to prevent stunting in childhood growth, as catch-up growth by any measure is limited in puberty. If long-term dialysis treatment can be avoided the majority of CKD patients show normal or slightly diminished pubertal growth. At this stage, successful, early (pre-emptive) renal transplantation with minimized steroid exposure is ultimately the best current measure for improving pubertal growth and sexual maturation in children with stage 5 CKD.
Key summary points
-
In the last 20 years most children requiring RRT before puberty presented with normal or only slightly delayed pubertal onset.
-
Pubertal growth is substantially more impaired in dialysis patients compared with patients with CKD stages 3–5.
-
In parallel with the improvement in sexual maturation there has been an improvement in pubertal height gain in CKD patients over the last two decades.
-
Growth hormone treatment increases final adult height in pediatric CKD patients. This is mainly achieved by an increase in prepubertal height gain, whereas pubertal timing and total pubertal height gain are not affected.
-
Efforts to avoid a height deficit before transplantation, preemptive transplantation, and the use of efficacious immunosuppressive strategies for optimized graft function and early withdrawal, or even complete avoidance, of steroids are suitable measures for improving pubertal growth and final height.
Key research points
-
The impact of intensified dialysis on pubertal growth is unknown and should be evaluated in prospective trials.
-
There has never been a randomized controlled trial of the impact of GH treatment during the pubertal growth period in CKD patients. Such a randomized controlled trial could address whether a short-term course of GH during the period of pubertal growth would enhance growth and have a positive impact on final adult height.
-
Pharmacological inhibition of epiphyseal closure (e.g., by aromatase inhibitors in boys) may allow an extended duration of the remaining growth period in pubertal CKD patients. The efficacy and safety of this concept should be evaluated in prospective trials.
Multiple choice questions (answers after reference list)
-
1.
Which is NOT true? Impairment of pubertal height gain in children with CKD is associated with:
-
a.
Exposure to glucocorticoids
-
b.
An earlier era for the start of renal replacement therapy
-
c.
Age at renal transplantation
-
d.
Growth hormone treatment
-
e.
Duration of dialysis
-
a.
-
2.
Which of the following statements regarding skeletal maturation in CKD patients is NOT true?
-
a.
The severity of the relative growth retardation at the time of puberty correlates positively with the delay in bone maturation
-
b.
Linear growth and bone maturation are dissociated during puberty
-
c.
Final height prediction models are reliable
-
d.
GH treatment does not accelerate bone maturation
-
e.
Treatment with sex steroids is associated with accelerated bone maturation
-
a.
-
3.
Which of the following does NOT occur in adolescents with end-stage CKD?
-
a.
LH and FSH levels may be increased
-
b.
Gonadal hormone levels may be decreased
-
c.
Pituitary GH secretion may be decreased
-
d.
IGF binding capacity is usually normal
-
e.
A state of hypergonadotropic hypogonadism is frequently observed in patients with long-standing dialysis
-
a.
-
4.
Which is NOT true?
-
a.
Pubertal delay is rarely seen nowadays in patients with end-stage CKD
-
b.
GH treatment may result in precocious puberty in CKD patients
-
c.
GH treatment does not increase total pubertal height gain
-
d.
GH treatment results in catch-up growth during the prepubertal age
-
e.
Withdrawal of glucocorticoids within the first 6 months after transplantation results in normal pubertal growth and adult height in the majority of patients
-
a.
-
5.
Which is NOT true? Renal transplantation with use of daily steroids:
-
a.
Is associated with obesity
-
b.
Has been shown to increase total pubertal height gain compared with healthy children
-
c.
May require GH treatment in the case of persistent growth failure
-
d.
Is associated with reduced pituitary GH secretion
-
e.
Is associated with low plasma IGF-1 levels
-
a.
References
Franke D, Winkel S, Gellermann J, Querfeld U, Pape L, Ehrich JH, Haffner D, Pavičić L, Zivičnjak M (2013) Growth and maturation improvement in children on renal replacement therapy over the past 20 years. Pediatr Nephrol 28:2043–2051
Harambat J, Bonthuis M, van Stralen KJ, Ariceta G, Battelino N, Bjerre A, Jahnukainen T, Leroy V, Reusz G, Sandes AR, Sinha MD, Groothoff JW, Combe C, Jager KJ, Verrina E, Schaefer F (2014) Adult height in patients with advanced CKD requiring renal replacement therapy during childhood. Clin J Am Soc Nephrol 9:92–99
Fine RN, Martz K, Stablein D (2010) What have 20 years of data from the North American Pediatric Renal Transplant Cooperative Study taught us about growth following renal transplantation in infants, children, and adolescents with end-stage renal disease? Pediatr Nephrol 25:739–746
Klare B, Montoya CR, Fischer DC, Stangl MJ, Haffner D (2012) Normal adult height after steroid-withdrawal within 6 months of pediatric kidney transplantation: a 20 years single center experience. Transpl Int 25:276–282
Furth SL, Stablein D, Fine RN, Powe NR, Fivush BA (2002) Adverse clinical outcomes associated with short stature at dialysis initiation: a report of the North American Pediatric Renal Transplant Cooperative Study . Pediatrics 109:909–913
Hartung EA, Furth SL (2013) Growth in children on renal replacement therapy: a shrinking problem? Pediatr Nephrol 28:1905–1908
Haffner D, Fischer DC (2012) Growth and pubertal development in dialyzed children and adolescents. In: Warady BA, Schaefer F, Alexander SR (eds) Pediatric dialysis, 2nd edn. Springer, New York, pp 453–481
Schaefer F, Seidel C, Binding A, Gasser T, Largo RH, Prader A, Schärer K (1990) Pubertal growth in chronic renal failure. Pediatr Res 28:5–10
Nissel R, Brázda I, Feneberg R, Wigger M, Greiner C, Querfeld U, Haffner D (2004) Effect of renal transplantation in childhood on longitudinal growth and adult height. Kidney Int 66:792–800
Rizzoni G, Broyer M, Brunner FP, Brynger H, Challah S, Kramer P, Oulès R, Selwood NH, Wing AJ, Balás EA (1985) Combined report on regular dialysis and transplantation of children in Europe, XIII, 1983. Proc Eur Dial Transplant Assoc Eur Ren Assoc 21:66–95
Burke BA, Lindgren B, Wick M, Holley K, Manivel C (1989) Testicular germ cell loss in children with renal failure. Pediatr Pathol 9:433–444
Tainio J, Qvist E, Vehmas R, Jahnukainen K, Hölttä T, Valta H, Jahnukainen T, Jalanko H (2011) Pubertal development is normal in adolescents after renal transplantation in childhood. Transplantation 92:404–409
Förster J, Ahlenstiel-Grunow T, Zapf A, Mynarek M, Pape L (2016) Pubertal development in pediatric kidney transplant patients receiving mammalian target of rapamycin inhibitors or conventional immunosuppression. Transplantation. doi:10.1097/TP.0000000000001037
Zivicnjak M, Franke D, Ehrich JH, Filler G (2000) Does growth hormone therapy harmonize distorted morphology and body composition in chronic renal failure? Pediatr Nephrol 15:229–235
Zivicnjak M, Franke D, Filler G, Haffner D, Froede K, Nissel R, Haase S, Offner G, Ehrich JH, Querfeld U (2007) Growth impairment shows an age-dependent pattern in boys with chronic kidney disease. Pediatr Nephrol 22:420–429
Franke D, Thomas L, Steffens R, Pavičić L, Gellermann J, Froede K, Querfeld U, Haffner D, Živičnjak M (2015) Patterns of growth after kidney transplantation among children with ESRD. Clin J Am Soc Nephrol 10:127–134
Haffner D, Schaefer F, Nissel R, Wuhl E, Tonshoff B, Mehls O (2000) Effect of growth hormone treatment on the adult height of children with chronic renal failure. German study group for growth hormone treatment in chronic renal failure. N Engl J Med 343:923–930
Nissel R, Lindberg A, Mehls O, Haffner D, Pfizer International Growth Database (KIGS) International Board (2008) Factors predicting the near-final height in growth hormone-treated children and adolescents with chronic kidney disease. J Clin Endocrinol Metab 93:1359–1365
Nissel R, Latta K, Gagnadoux MF, Kelly D, Hulton S, Kemper MJ, Ruder H, Söderdahl G, Otte JB, Cochat P, Roquet O, Jamieson NV, Haffner D (2006) Body growth after combined liver-kidney transplantation in children with primary hyperoxaluria type 1. Transplantation 82:48–54
Rees L, Greene SA, Adlard P, Jones J, Haycock GB, Rigden SP, Preece M, Chantler C (1988) Growth and endocrine function in steroid sensitive nephrotic syndrome. Arch Dis Child 63:484–490
Haffner D, Weinfurth A, Manz F, Schmidt H, Bremer HJ, Mehls O, Schärer K (1999) Long-term outcome of paediatric patients with hereditary tubular disorders. Nephron 83:250–260
Greco M, Brugnara M, Zaffanello M, Taranta A, Pastore A, Emma F (2010) Long-term outcome of nephropathic cystinosis: a 20-year single-center experience. Pediatr Nephrol 25:2459–2467
Seikaly MG, Salhab N, Gipson D, Yiu V, Stablein D (2006) Stature in children with chronic kidney disease: analysis of NAPRTCS database. Pediatr Nephrol 21:793–799
United States Renal Data System (USRDS) 2008 report. USRDS Coordinating Center, Minneapolis, pp 296–297. http://www.usrds.org/adr.aspx
Mak RH, Cheung WW, Zhan JY, Shen Q, Foster BJ (2012) Cachexia and protein-energy wasting in children with chronic kidney disease. Pediatr Nephrol 27:173–181
Bonthuis M, van Stralen KJ, Verrina E, Groothoff JW, Alonso Melgar Á, Edefonti A, Fischbach M, Mendes P, Molchanova EA, Paripović D, Peco-Antic A, Printza N, Rees L, Rubik J, Stefanidis CJ, Sinha MD, Zagożdżon I, Jager KJ, Schaefer F (2013) Underweight, overweight and obesity in paediatric dialysis and renal transplant patients. Nephrol Dial Transplant 28 [Suppl 4]:v195–iv204
Vester U, Schaefer A, Kranz B, Wingen AM, Nadalin S, Paul A, Malagò M, Broelsch CE, Hoyer PF (2005) Development of growth and body mass index after pediatric renal transplantation. Pediatr Transplant 9:445–449
Brungger M, Hulter HN, Krapf R (1997) Effect of chronic metabolic acidosis on the growth hormone/IGF-1 endocrine axis: new cause of growth hormone insensitivity in humans. Kidney Int 51:216–221
Parekh RS, Flynn JT, Smoyer WE, Milne JL, Kershaw DB, Bunchman TE, Sedman AB (2001) Improved growth in young children with severe chronic renal insufficiency who use specified nutritional therapy. J Am Soc Nephrol 12:2418–2426
Haffner D, Fischer DC (2010) Bone cell biology and pediatric renal osteodystrophy. Minerva Pediatr 62:273–284
Chesney RW, Moorthy AV, Eisman JA, Jax DK, Mazess RB, DeLuca HF (1978) Increased growth after long-term oral 1,25-vitamin D3 in childhood renal osteodystrophy. N Engl J Med 298:238–242
Chan JC, Kodroff MB, Landwehr DM (1981) Effects of 1,25-dihydroxyvitamin-D3 on renal function, mineral balance, and growth in children with severe chronic renal failure. Pediatrics 68:559–571
Jabs K (1996) The effects of recombinant human erythropoietin on growth and nutritional status. Pediatr Nephrol 10:324–327
Schaefer F, Seidel C, Mitchell R, Scharer K, Robertson WR (1991) Pulsatile immunoreactive and bioactive luteinizing hormone secretion in adolescents with chronic renal failure. the cooperative study group on pubertal development in chronic renal failure (CSPCRF). Pediatr Nephrol 5:566–571
Schaefer F, Veldhuis JD, Robertson WR, Dunger D, Scharer K (1994) Immunoreactive and bioactive luteinizing hormone in pubertal patients with chronic renal failure. cooperative study group on pubertal development in chronic renal failure. Kidney Int 45:1465–1476
Schaefer F, Daschner M, Veldhuis JD, Oh J, Qadri F, Scharer K (1994) In vivo alterations in the gonadotropin-releasing hormone pulse generator and the secretion and clearance of luteinizing hormone in the uremic castrate rat. Neuroendocrinology 59:285–296
Daschner M, Philippin B, Nguyen T, Wiesner RJ, Walz C, Oh J, Sandow J, Mehls O, Schaefer F (2002) Circulating inhibitor of gonadotropin releasing hormone secretion by hypothalamic neurons in uremia. Kidney Int 62:1582–1590
Schaefer F, Vogel M, Kerkhoff G, Woitzik J, Daschner M, Mehls O (2001) Experimental uremia affects hypothalamic amino acid neurotransmitter milieu. J Am Soc Nephrol 12:1218–1227
Mitchell R, Bauerfeld C, Schaefer F, Scharer K, Robertson WR (1994) Less acidic forms of luteinizing hormone are associated with lower testosterone secretion in men on haemodialysis treatment. Clin Endocrinol 41:65–73
Blum WF, Ranke MB, Kietzmann K, Tonshoff B, Mehls O (1991) Growth hormone resistance and inhibition of somatomedin activity by excess of insulin-like growth factor binding protein in uraemia. Pediatr Nephrol 5:539–544
Haffner D, Schaefer F, Girard J, Ritz E, Mehls O (1994) Metabolic clearance of recombinant human growth hormone in health and chronic renal failure. J Clin Invest 93:1163–1171
Tonshoff B, Veldhuis JD, Heinrich U, Mehls O (1995) Deconvolution analysis of spontaneous nocturnal growth hormone secretion in prepubertal children with preterminal chronic renal failure and with end-stage renal disease. Pediatr Res 37:86–93
Schaefer F, Veldhuis JD, Stanhope R, Jones J, Scharer K (1994) Alterations in growth hormone secretion and clearance in peripubertal boys with chronic renal failure and after renal transplantation. Cooperative study group of pubertal development in chronic renal failure. J Clin Endocrinol Metab 78:1298–1306
Challa A, Chan W, Krieg RJ Jr, Thabet MA, Liu F, Hintz RL, Chan JC (1993) Effect of metabolic acidosis on the expression of insulin-like growth factor and growth hormone receptor. Kidney Int 44:1224–1227
Rabkin R, Sun DF, Chen Y, Tan J, Schaefer F (2005) Growth hormone resistance in uremia, a role for impaired JAK/STAT signaling. Pediatr Nephrol 20:313–318
Farquharson C, Ahmed SF (2013) Inflammation and linear bone growth: the inhibitory role of SOCS2 on GH/IGF-1 signaling. Pediatr Nephrol 28:547–556
Tonshoff B, Kiepe D, Ciarmatori S (2005) Growth hormone/insulin-like growth factor system in children with chronic renal failure. Pediatr Nephrol 20:279–289
Schaefer F, Hamill G, Stanhope R, Preece MA, Scharer K (1991) Pulsatile growth hormone secretion in peripubertal patients with chronic renal failure. Cooperative study group on pubertal development in chronic renal failure. J Pediatr 119:568–577
Olney RC (2009) Mechanisms of impaired growth: effect of steroids on bone and cartilage. Horm Res 72 [Suppl 1]:30–35
Neu AM, Bedinger M, Fivush BA, Warady BA, Watkins SL, Friedman AL, Brem AS, Goldstein SL, Frankenfield DL (2005) Growth in adolescent hemodialysis patients: data from the Centers for Medicare & Medicaid Services ESRD Clinical Performance Measures Project. Pediatr Nephrol 20:1156–1160
Katz A, Bock GH, Mauer M (2000) Improved growth velocity with intensive dialysis. Consequence or coincidence? Pediatr Nephrol 14:710–712
Fischbach M, Terzic J, Menouer S, Dheu C, Seuge L, Zalosczic A (2010) Daily on line haemodiafiltration promotes catch-up growth in children on chronic dialysis. Nephrol Dial Transplant 25:867–873
Hoppe A, von Puttkamer C, Linke U, Kahler C, Booss M, Braunauer-Kolberg R, Hofmann K, Joachimsky P, Hirte I, Schley S, Utsch B, Thumfart J, Briese S, Gellermann J, Zimmering M, Querfeld U, Müller D (2011) A hospital-based intermittent nocturnal hemodialysis program for children and adolescents. J Pediatr 158:95–99
Pape L, Ehrich JH, Zivicnjak M, Offner G (2005) Growth in children after kidney transplantation with living related donor graft or cadaveric graft. Lancet 366:151–153
Höcker B, Weber LT, Feneberg R, Drube J, John U, Fehrenbach H, Pohl M, Zimmering M, Fründ S, Klaus G, Wühl E, Tönshoff B (2010) Improved growth and cardiovascular risk after late steroid withdrawal: 2-year results of a prospective, randomised trial in paediatric renal transplantation. Nephrol Dial Transplant 25:617–624
Webb NJ, Douglas SE, Rajai A, Roberts SA, Grenda R, Marks SD, Watson AR, Fitzpatrick M, Vondrak K, Maxwell H, Jaray J, Van Damme-Lombaerts R, Milford DV, Godefroid N, Cochat P, Ognjanovic M, Murer L, McCulloch M, Tönshoff B (2015) Corticosteroid-free kidney transplantation improves growth: 2-year follow-up of the TWIST randomized controlled trial. Transplantation 99:1178–1185
Sarwal MM, Ettenger RB, Dharnidharka V, Benfield M, Mathias R, Portale A, McDonald R, Harmon W, Kershaw D, Vehaskari VM, Kamil E, Baluarte HJ, Warady B, Tang L, Liu J, Li L, Naesens M, Sigdel T, Waskerwitz J, Salvatierra O (2012) Complete steroid avoidance is effective and safe in children with renal transplants: a multicenter randomized trial with three-year follow-up. Am J Transplant 12:2719–2729
Billing H, Burmeister G, Plotnicki L, Ahlenstiel T, Fichtner A, Sander A, Höcker B, Tönshoff B, Pape L (2013) Longitudinal growth on an everolimus- versus an MMF-based steroid-free immunosuppressive regimen in paediatric renal transplant recipients. Transpl Int 26:903–909
Kassmann K, Rappaport R, Broyer M (1992) The short-term effect of testosterone on growth in boys with hemodialysis. Clin Nephrol 37:148–154
Van Steenbergen MW, Wit JM, Donckerwolcke RAMG (1991) Testosterone esters advance skeletal maturation more than growth in short boys with chronic renal failure and delayed puberty. Eur J Pediatr 150:676–780
Haffner D, Schaefer F (2013) Searching the optimal PTH target range in children undergoing peritoneal dialysis: new insights from international cohort studies. Pediatr Nephrol 28:537–545
Muscheites J, Wigger M, Drueckler E, Fischer DC, Kundt G, Haffner D (2008) Cinacalcet for secondary hyperparathyroidism in children with end-stage renal disease. Pediatr Nephrol 23:1823–1829
Nakagawa K, Pérez EC, Oh J, Santos F, Geldyyev A, Gross ML, Schaefer F, Schmitt CP (2008) Cinacalcet does not affect longitudinal growth but increases body weight gain in experimental uraemia. Nephrol Dial Transplant 23:2761–2767
Mehls O, Ritz E, Hunziker EB, Eggli P, Heinrich U, Zapf J (1988) Improvement of growth and food utilization by human recombinant growth hormone in uremia. Kidney Int 33:45–52
Powell DR, Durham SK, Liu F, Baker BK, Lee PD, Watkins SL, Campbell PG, Brewer ED, Hintz RL, Hogg RJ (1998) The insulin-like growth factor axis and growth in children with chronic renal failure: a report of the southwest pediatric nephrology study group. J Clin Endocrinol Metab 83:1654–1661
Rees L (2015) Growth hormone therapy in children with CKD after more than two decades of practice. Pediatr Nephrol. doi:10.1007/s00467-015-3179-2
Hokken-Koelega A, Mulder P, De Jong R, Lilien M, Donckerwolcke R, Groothof J (2000) Long-term effects of growth hormone treatment on growth and puberty in patients with chronic renal insufficiency. Pediatr Nephrol 14:701–706
Haffner D, Wühl E, Schaefer F, Nissel R, Tonshoff B, Mehls O (1998) Factors predictive of the short- and long-term efficacy of growth hormone treatment in prepubertal children with chronic renal failure. The German Study Group for Growth Hormone Treatment in Chronic Renal Failure. J Am Soc Nephrol 9:1899–1907
Kovács GT, Oh J, Kovács J, Tönshoff B, Hunziker EB, Zapf J, Mehls O (1996) Growth promoting effects of growth hormone and IGF-I are additive in experimental uremia. Kidney Int 49:1413–1421
Mauras N, Gonzalez de Pijem L, Hsiang HY, Desrosiers P, Rapaport R, Schwartz ID, Klein KO, Singh RJ, Miyamoto A, Bishop K (2008) Anastrozole increases predicted adult height of short adolescent males treated with growth hormone: a randomized, placebo-controlled, multicenter trial for one to three years. J Clin Endocrinol Metab 93:823–831
Mendly SR, Spyropoulos F, Counts DR (2015) Short stature in chronic kidney disease treated with growth hormone and an aromatase inhibitor. Case Rep Pediatr 2015:738571
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None declared.
Additional information
Answers
1. d
2. c
3. d
4. b
5. b
Rights and permissions
About this article
Cite this article
Haffner, D., Zivicnjak, M. Pubertal development in children with chronic kidney disease. Pediatr Nephrol 32, 949–964 (2017). https://doi.org/10.1007/s00467-016-3432-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3432-3